Abstract
This study focuses on caregivers who work in residential facilities (RFs) for the elderly, and specifically on their organizational citizenship behaviors (OCBs) in relation to their interaction respectively with the overall context (workplace attachment dimension), the spatial-physical environment (perceived environmental comfort), and the social environment (relationship with patients). A sample of health care workers (medical or health care specialists, nurses, and office employees, n = 129) compiled a self-report paper-pencil questionnaire, which included scales measuring the study variables. The research hypotheses included secure workplace attachment style as independent variable, OCBs as the dependent variable, and perceived comfort and relations with patients as moderators. Results showed that both secure workplace attachment and perceived comfort promote OCBs, but the latter counts especially as a compensation of an insecure workplace attachment. As expected, difficult relationships with patients hinder the relationship between secure workplace attachment style and OCBs. In sum, our study highlights the importance of the joint consideration of the psychological, social, and environmental dimensions for fostering positive behaviors in caregivers employed in elderly care settings.
1. Introduction
The topic of Active and Healthy Aging (HAA) from a psychological perspective [1,2,3,4] is particularly critical for the Italian population, which ranks first in Europe in terms of number of elderly people [5]. A response to this demographic configuration of Italian society and to the resulting demand for health is provided by Residential Facilities (RFs; “Residenze Sanitarie Assistenziali” (RSA) in Italian). These facilities may be public or private, are decentralized with respect to the National Health System (NHS) and play a complementary role in continuity with hospital facilities. In fact, their mission and objectives are related to the improvement of both health and socio-psychological conditions. In this regard, RFs are framed in a perspective not only of care and rehabilitation (i.e., loss reduction), but rather of health and well-being (i.e., gain achievement) in a general sense. This explains why in the last decade the RFs have spread in all the Italian territories [6,7].
RFs approach the issue of HAA from two complementary perspectives. The first concerns the structuring of therapy and rehabilitation pathways (mainly, but not exclusively) post hospitalization and post inpatient. These are aimed at restoring the dimensions of health or maintaining and enhancing the residual ones, in a bio-psycho-social perspective [8]. These are generally short, intensive, multidimensional, integrated, and personalized pathways, which aim to restore the health conditions of the elderly person and end with the reintegration into their social and territorial context [7,9]. The second perspective concerns the elderly with severe and/or chronic disabilities, who are often carriers of multiple and/or degenerative diseases and are therefore particularly fragile. Again, the goal is the maintenance and enhancement of residual health dimensions, but the elderly’s stay is significantly prolonged, and may become indefinite or definitive [10,11].
In the pursuit of HAA, particularly with the most frail elderly and those destined to long-term inpatient stays, RFs are supposed to be oriented toward achieving and maintaining high standards of response quality and healthcare humanization [12,13]. This perspective focuses on multiple dimensions, i.e., the physical health of the elderly (including monitoring and administration of care [9,14]), their emotions, and their culture, traditions, and habits [10]. In addition, the care of greenery (outside and inside the facilities [15]), aesthetics, comfort, and possibility of socialization [16] are of considerable importance. A further key facet of this orientation is represented by the occupational, organizational, and environmental health of staff working in RFs. In fact, it is necessary that operators are capable of caring work in their area of expertise, but also of cooperating within a multidisciplinary team that is open to discussion and improvement [17,18]. In addition, they should be able both to relate to the patient and his or her caregivers (often family members) with empathy, listening skills, emotional closeness, and affective exchange [19,20], and to know how to cope with critical relational situations, which can be marked by fear, suffering, anger, conflict, and misunderstanding [21], and not infrequently by despair and grief [22,23]. To promote job satisfaction in RFs staff, that is supposed to positively impact on the quality of care, again the characteristics of the spatial-physical environment are supposed to play an important role, in terms of functionality, welcoming appearance [24], and design humanization [16].
The importance that RFs have assumed in recent years, as a positive NHS response to the need for care and pursuit of HAA, is evidenced by the recent COVID-19 pandemic due to the SARS-CoV-2 virus [25]. In Italy the pandemic has highlighted the fragility of regional health systems and the importance of RFs. In fact, these facilities have vicariously served as hospital presidia, and their staff have cared for older and frail patients with a dedication and self-sacrifice that, in some cases, have put their health and safety at risk [26].
The psychological literature on HAA has primarily focused on the elderly people, whereas less attention has been devoted to caregivers as key resources for the promotion of elderly health in institutionalized settings [27,28]. The focus on RFs workers is motivated by their active role in providing support not only to the elderly residents, but also to their families [16]. In fact, a proper communication between the staff of healthcare environments and the older adults’ family can facilitate the involvement of family members in residents’ care, thus providing social support and reducing the level of anxiety [29]. Hence, the attention should be put on the quality of RFs caregivers’ experiences, since it can influence the residents’ health and well-being [30]. In this regard, there has been a lack of exploration about the connection between the relationship of RFs workers with their physical-spatial milieu and their behavioral responses. Following this line, our study focuses on organizational citizenship behaviors (OCB, [31,32]) of RFs caregivers, in relation to features covering different socio-psychological interfaces: (a) people-overall context interface-where the overall context includes both the spatial-physical and the social environment-represented by the workplace attachment style; (b) people-physical environment interface, represented by the perceived environmental comfort; (c) and finally, people-people interface, represented by the relationship between staff and patients. The following paragraphs report the literature ground which provides support to our choice to focus on such features.
1.1. Organizational Citizenship Behaviors in Healthcare Settings
According to Organ [31], organizational citizenship consists of the set of behaviors enacted by members of an organization, and that promote its efficiency and effectiveness. They are discretionary, not imposed by a contract, and do not involve formal rewards [32]. These behaviors are spontaneous and pro-social acts that go beyond the formally defined role and tasks. Thus, they are intra- and extra-role behaviors of fundamental importance for the effectiveness and efficiency of organizational processes and their improvement [33,34]. Organ [31] and other authors [35], have identified five dimensions of OCBs. The first is Conscientiousness, which refers to the special care a worker takes in performing his or her duties (e.g., strictly adhering to the job description). The second dimension is Civic Virtue, which refers to a strong sense of responsibility to the organization (for example, a willingness to offer advice to colleagues or to try to solve problems that arise at work). The third dimension, Sportsmanship, implies a sense of loyalty to one’s organization, which is manifested by emphasizing its best aspects and avoiding paying attention to the less positive ones. The fourth dimension, Altruism, expresses a willingness to help one’s co-workers (e.g., by helping new members or those with a higher workload). Finally, the fifth dimension, Courtesy, includes taking special care in establishing kind and cooperative relationships (e.g., trying to avoid relational conflicts between co-workers) [36]. In recent decades, literature on OCBs has highly expanded, with a focus both on OCBs’ nature and intensity, and on their antecedents and consequences [32,34,37,38]. A further issue concerns OCBs’ categorization, for which different criteria have been proposed. For example, Podsakoff et al. [39] distinguished OCBs with respect to two different worker orientations, i.e., OCBAs (behaviors oriented toward Affiliation to others, such as Altruism, Courtesy, and Interpersonal Help; or to the organization, such as Sportsmanship, Loyalty, and Compliance) and OCBCs (oriented to Challenge and Initiative, such as Civic Virtue and Making Constructive Suggestions).
Regarding healthcare organizations, several studies show the importance of the role played by OCBs. For example, Jahani et al. [40] showed that OCBs have a positive influence on organizational communication, promote organizational planning, improve interpersonal cooperation, develop a better organizational climate, and affect staff satisfaction, work life quality, service provision, job commitment, and financial output. Regarding the relationship between OCBs and human resources management practices in health care settings, Ranjhan and Mallick [41] showed the impact of OCBs on workers’ productivity, competitive advantage, and job performance in a study conducted with different job profiles of health care facilities (hospitals, nursing homes, and diagnostic centers). Another study, carried out by Saleh et al. [42], highlighted the influence of psychological capital and work engagement, on OCBs and organizational commitment.
In contrast, there are very few studies regarding OCBs of caregivers who work in RFs with the elderly. For instance, a study was led on caregivers of long term and community care facilities for the elderly by Ginsburg et al. [43], who highlighted the importance of work engagement and psychological empowerment on OCBs and turnover intention of caregivers, and how important these are for the quality of care provided by caregivers to the elderly people. In another study focusing on the same target population (i.e., long term care and community care operators), Perreira and colleagues [44] found that organizationally oriented OCBs are related to psychological empowerment, job satisfaction, and intention to remain in the same work setting.
1.2. Workplace Attachment Styles
The development of positive job-related responses in workers can be also promoted by a positive workplace attachment, which is a specific pattern included in the broader construct of place attachment, defined as an individual’s bond (mainly of affective nature) to a meaningful place [45]. Place attachment is conceived as composed of two dimensions, i.e., place dependence [46], that is a form of functional attachment to a specific place, and place identity [47], that refers to a substructure of the self-including cognitions, emotions, and behavioral tendencies toward the physical environment [48]. The interest for the place attachment topic is witnessed by the noteworthy number of studies that have addressed this pattern as implied in various outcomes, such as individual well-being [49], social well-being [50], customer behavior [51], environmentally responsible behavior [52] or satisfaction [53], coping behaviors in environmental disasters [54]. A recent theoretical proposal conceives place attachment in the light of Bowlby’s classical theory of attachment [55]. In fact, according to Scannell [56], places can also act as a “safe haven” for individuals. In that case the specific places will have the role of protecting the individual, solving problems and emotional relief. According to Morgan [57], children develop internal operational models (IWMs) in relation to their experiences with places. Such IWMs would therefore be formed during childhood as a function of the relationships between the child and their home [58] and the characteristics of these IWMs will influence future relationships between individuals and other specific places [59] such as the city [60], the neighborhood [61], or the workplace [62]. For example, Scrima, et al. [63] found that it is possible to identify attachment styles to the workplace. Taking up the model of Bartholomew and Horovitz [64], Scrima et al. [63] argue that place attachment styles are a function of the thoughts of Self and thoughts of Place. Positive thoughts of Self and Place refer to a secure attachment style, positive thoughts of Self and negative thoughts of Place are associated with an avoidant attachment style, negative thoughts of Self and positive thoughts of Place are associated with a preoccupied attachment style, and negative thoughts of Self and Place characterize the disorganized attachment style. In particular, secure attachment style develops when a specific place satisfies the needs of its user [65].
Thus, a workplace that meets the employee’s needs should allow the employee to develop a secure attachment style with the workplace. The development of a secure attachment style to the workplace seems to have numerous beneficial aspects. For example, a secure style promotes exploration, since this allows individuals to walk away without feeling discomfort [66]. According to Stancu et al. [67], a secure place attachment is a buffer against psychological distress and improves constructive and adaptive strategies in risk coping. To the best of our knowledge, there have been no studies so far focusing on workplace attachment styles in health care and RFs settings.
1.3. The Physical-Spatial Comfort of Caregivers in Healthcare Settings
The literature on the effect of the workplace spatial-physical features on office employees’ well-being and behaviors has evidenced that design-related dimensions such as noise, lighting, temperature, and indoor air quality conditions can play a role in employees’ satisfaction, attitudes, behaviors, and performance (e.g., [68]). The lack of quality of the workplace design can in fact elicit a low level of work satisfaction and job productivity, poor health, and high mental fatigue [69]. About the healthcare settings, the influence of spatial-physical features of the workplace in caregivers’ outcomes has been evidenced by the extended literature review by Ulrich and colleagues [70], who showed that different aspects of the built environment can affect the degree of staff injuries, stress, work effectiveness, and satisfaction. The importance of considering the impact of healthcare workers’ perceived comfort on their well-being and behaviors is explicitly remarked in the architectural humanization approach to the healthcare environments [71,72,73]. According to this approach, more humanized healthcare settings elicit a higher perceived quality of design attributes that should be provided in order to satisfy users’ needs, including sense of welcome, orientation, and comfort, both spatial (i.e., office furniture, layout, and spatial characteristics) and sensorial (in visual terms, i.e., adequate lighting and panoramic views; auditory terms, i.e., avoidance of annoying noises; and climatic terms, i.e., adequacy of temperature and humidity [74]).
1.4. The Relationships between Patients and Caregivers in Healthcare Settings
In the perspective of the humanization of care settings, a patient-centered approach, takes on particular importance. This orientation is focused on the involvement of the patient as an active and autonomous subject (with physical, relational, and emotional needs [75]), and on an adequate relationship between the patient and the caregiver [76]. Regarding this last aspect, several authors highlight how empathy is a supportive factor in the process of care, since it promotes patient’s compliance and treatment positive outcomes, and facilitates the well-being of health care providers themselves (e.g., [77,78]). Other important antecedents of an adequate caregiver-patient relationship are the caregiver professionals’ ability to actively listen [79] and communication skills in terms of assertiveness [80,81]. With regard to RFs, some scholars have emphasized the importance of the relationship between health care providers and the residents (e.g., [82]), whilst another study highlighted the operators’ professional skills involved in the care of the elderly, such as bonding and connection, tenderness and closeness, non-infantilization and respect [83]. Such skills can be considered as positive extra-role behaviors, which are necessary for the achievement and maintenance of an adequate level of relational humanization in these health care settings.
1.5. Objective and Hypotheses
The aim of this research is to verify the role of secure workplace attachment style (tapping people-overall context interface), perceived comfort (concerning people-physical environment interface) and relationship staff-patients (regarding people-people interface) in the RFs workers’ OCBs.
The relationship between workplace attachment and OCBs (or similar organizational behaviors), is still substantially unexplored, with a few exceptions. For instance, Desivilya [84] showed that the secure attachment style is an antecedent of pro-social and positive behaviors in organizations, and among them OCBs. Harms et al. [85] found that employees’ avoidant attachment style toward their bosses negatively affects their OCBs directed at other individuals. Finally, Reizer [86] showed that Self-compassion mediates the negative influence of avoidant and anxious attachment styles on OCBs. It is to remark that none of these studies were carried out in health care settings or RFs. Thus, we hypothesized that:
Hypothesis 1 (H1).
Secure workplace attachment is positively related to OCBs, both in terms of overall factors and concerning the distinct OCBs components (i.e., Altruism, Conscientiousness, and Civic Virtue).
Studies on the influence of physical-spatial comfort and organizational behaviors such as OCBs are generally lacking. Even though it has been shown that office physical features such as noise, lighting conditions, temperature, and indoor air quality impact the attitudes, behaviors, productivity, and satisfaction of employees [68], and that the low quality of workplace design can elicit lower work satisfaction, lower job productivity, poorer health, and higher mental fatigue [69], less attention has been placed on perceived design quality in relation to workers’ behaviors and well-being. Among those addressing these concerns, Zoghbi-Manrique-de-Lara et al. [87], evidenced the negative influence of crowded physical workspaces with low privacy on organizational citizenship behaviors in favor of others (OCB-I) in a study with workers in open-space facilities. Carter and colleagues [88] found that satisfaction with physical workspace and perceived quality of the physical workplace are drivers of OCBs. Scrima et al. [89] detected a significant impact of satisfaction toward the workplace design on exhaustion, i.e., a subdimension of burnout.
We expected both a main effect of perceived spatial-physical comfort on OCBs and an amplification effect of the relationship between secure workplace attachment and OCBs:
Hypothesis 2 (H2).
Perceived spatial-physical comfort is positively related to OCBs, both in terms of overall factors and concerning the distinct OCBs components.
Hypothesis 3 (H3).
Perceived spatial-physical comfort moderates the relationship between secure workplace attachment and OCBs, both in terms of overall factors and concerning the distinct OCBs components.
Regarding the bond of staff-patient relationships with OCBs or similar behaviors, Jarfarpanah et al. [90], found a connection between patient safety culture and OCBs Altruism, Civic Virtue, and Courtesy in nurses. Wibowo and colleagues [91], showed that OCBs in hospital settings facilitate better performance in caring work with patients. Perreira et al. [92] showed that caregivers’ affective commitment to patients positively influences their OCBs, Finally, Lavee and Pindek [93] found that commitment to care work can lead caregivers to exhaustion (i.e., an outcome that is opposite to OCBs) under conditions of high job demand in health, education, and welfare service providers.
As well as in the case of perceived spatial-physical comfort, we hypothesized both a main negative effect of difficult staff-patient relationships on OCBs and a buffer effect of the link between secure workplace attachment and OCBs. Thus, we expected that:
Hypothesis 4 (H4).
Difficult staff-patient relationships are negatively related to OCBs, both in terms of overall factors and concerning the distinct OCBs components.
Hypothesis 5 (H5).
Difficult staff-patient relationships moderate the relationship between secure workplace attachment and OCBs, both in terms of overall factors and concerning the distinct OCBs components.
2. Materials and Methods
2.1. Research Protocol
Data were collected between October 2019 and February 2020 through a self-report paper-pencil questionnaire administered to operators of three RFs in the Autonomous Region of Sardinia (Italy). The sample was of convenience and those who participated in the research volunteered (without receiving any compensation). Although the sample is not representative of the population of RFs caregivers, we respected the structure of job roles found in RFs. A total of 164 research questionnaires were distributed, of which 129 were returned (response rate = 78.65%).
2.2. Participants
The final sample of 129 practitioners consists mostly of females (77.51%, n = 100), whereas males are about one quarter (22.49%, n = 29). Approximately half of the participants (53.48%, n = 69) are health care workers (in Italian “Operatore Socio Sanitario, (OSS)”); 22.48% (n = 29) are medical or health care specialists; 13.95% (n = 18) are nurses; and about the remaining 10% are office employees (n = 13). Most are either graduates (37.98%, n = 49) or high school graduates (44.96%, n = 58) and have an average length of service of 11.18 years (SD = 6.95). Finally, about half are between the ages of 31 and 45 (51.93%, n = 67) and about one-third are between the ages of 46 and 60 (31.08%, n = 40).
2.3. Instruments
The questionnaire contains the following measurement scales.
Organizational Citizenship Behavior (OCB): We used the brief version (15 items) of the Organizational Citizenship Behavior Scale [35] in its Italian validation [94]. The Principal Component Analysis performed on the scale confirmed its 3-component factorial structure, including Altruism (5 items, Alpha = 0.89, e.g., “I help others who have a heavy workload”), Conscientiousness (3 items, Alpha = 0.73, e.g., “I do my job without constant requests from my boss”) and Civic Virtue (4 items, Alpha = 0.82, e.g., “I keep abreast of changes in the organization”). We used both these three specific components and the overall OCB (15 items, Alpha = 0.89) for the inferential analyses.
Secure workplace attachment style: from the Workplace Attachment Scale (Echelle d’Attachement au lieu de travail–EALT, [62]), recently validated in Italian by Scrima [95], the five items included in the secure workplace attachment style (Alpha = 0.84, e.g., “I am attached to my workplace”) were used;
Perceived physical-spatial comfort: A 16-item scale adapted from the short version of the Perceived Healthcare Environment Quality Indicators (IUOP, [73,96]) was used to assess the perceived physical-spatial comfort (Alpha = 0.87, e.g., “In this in-patient/waiting area furnishings are in good condition”);
Difficult relationship with patients: for the assessment of the relationship between RFs workers and patients, the five items of the component “ambiguous customer expectations” of the Customer-Related Social Stressors scale by Dormann and Zapf [97] were used (Alpha = 0.88, e.g., “Customers’ wishes are often contradictory”).
For all these measures, the response scales consisted of a 7-step Likert-type scale (from 1 = “completely disagree” to 7 = “fully agree”).
Socio-demographic data (sex, age, and length of service expressed in range, occupational role, and level of education) were also collected.
2.4. Data Analysis
The mono-factorial structure of the scales measuring secure workplace attachment style, perceived spatial-physical comfort, and difficult relationship with patients was verified through a Principal Component Analysis (on IBM SPSS 26). As concerns the factorial structure of the OCBs scale (see Supplementary Materials, Figure S1, Table S1), which has been conceived and then tested as multi-factorial in previous literature (e.g., [31]), a confirmatory factor analysis (CFA) was run (on JASP 0.14). The model including the 3-factor structure and the second-order overall factor was confirmed, showing acceptable fit indices (CFI = 0.96; TLI = 0.95; RMSA = 0.07 [90% CI = 0.04, 0.10]; SRNR = 0.04; χ2/df = 1.6).
To test the research hypotheses, model 2 (Figure 1a; Figure 1b) of the process macro (on IBM SPSS 26) was used [98], including a secure workplace attachment style as the independent variable (IV), overall OCB and the three specific OCB subdimensions (Altruism, Conscientiousness, and Civic Virtue) as dependent variables (DVs), and perceived comfort and difficult relationship with patients as moderators.
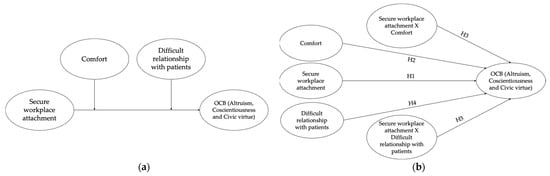
Figure 1.
(a) Conceptual model of the tested model. (b) Diagram of the tested model.
The simple slope analysis allowed us to interpret the moderation effects of perceived comfort and difficult relationship with patients. Sex, age, education level, and marital status were inserted as covariates.
2.5. Ethical Issues
The research was authorized by the Ethics Committee of the University of Cagliari (approval number 73624 dated 30 March 2021). It was conducted in full compliance with the Ethical Principles of Psychologists and Code of Conduct of the American Psychological Association (APA), integrated into the Associazione Italiana Psicologia (AIP) code of ethics. Furthermore, the study did not address any sensitive topics and was carried out via procedures for informed and consenting adults. Lastly, in accordance with the Italian privacy law, the research ensured the anonymity and privacy of all participants.
3. Results
3.1. Preliminary Analyses
The results of the factor analysis on the multidimensional scales suggested the use of a single-factor measure for the scales of perceived comfort, secure workplace attachment style, and problematic relationships with patients; and a 3-factorial structure for the OCB scale (Altruism, Conscientiousness, and Civic Virtue).
Table 1 shows the descriptive and correlational analyses performed on the aggregate variables computed after the verification of factorial solution and reliability.

Table 1.
Means, SDs and bivariate correlations of the study variables, and alpha in diagonal.
Regarding the correlations between socio-demographic variables and the variables under study, age (r = −0.26, p < 0.01) and marital status (r = −0.21, p < 0.01) are negatively associated with Altruism, while education level is positively correlated with perceived comfort (r = 0.19, p < 0.05). As expected, overall OCB correlates positively with secure workplace attachment style (r = 0.34, p < 0.00001). Specifically, secure workplace attachment correlates with Altruism (r = 0.30, p < 0.0001) and with Civic Virtue (r = 0.36, p < 0.0001), but not with Conscientiousness (r = 0.17, p = n.s.). Furthermore, overall OCB correlates positively with perceived comfort (r = 0.42, p < 0.0001). The three dimensions of OCB, Altruism, Conscientiousness and Civic Virtue, are positively associated (p < 0.0001) with perceived comfort, showing coefficients of 0.35, 0.33, and 0.30 respectively. It is also interesting to note that no OCB dimension is associated with difficult relationship with patient. Finally, secure workplace attachment correlates positively with perceived comfort (r = 0.39, p < 0.0001)
3.2. Hypotheses Testing
Four independent models were tested to verify the five hypotheses: one for the overall OCB and the other three for its components (Altruism, Conscientiousness, and Civic Virtue). As expected (H1), secure workplace attachment style is positively related with overall OCB (B = 0.13, p < 0.05) (Table 2), Altruism (B = 0.13, p < 0.05) (Table 3) and Civic Virtue (B = 0.26, p < 0.01) (Table 4).

Table 2.
Moderation model with overall OCB as DV.

Table 3.
Moderation model with secure WA as IV and Altruism as DV.

Table 4.
Moderation model with secure WA as IV and Civic Virtue as DV.
Contrary to what has been hypothesized, secure workplace attachment style is not positively related with Conscientiousness in the workplace (B = 0.04, p = n.s.) (Table 5).

Table 5.
Moderation model with secure WA as IV and Conscientiousness as DV.
A statistically significant relationship emerged from the test of the direct effect of perceived comfort on the OCB (H2): the perceived comfort was positively related with overall OCB (B = 0.26, p < 0.01) (Table 2), Altruism (B = 0.27, p < 0.01) (Table 3) and Conscientiousness (B = 0.28, p < 0.01) (Table 5) but not with Civic Virtue (B = 0.20, p = n.s.) (Table 4).
Unlike what was expected (H3) only the interaction between secure WA and perceived comfort on overall OCB was statistically significant (B = −0.10, p < 0.05) (Table 2; Figure 2, Simple slope a).
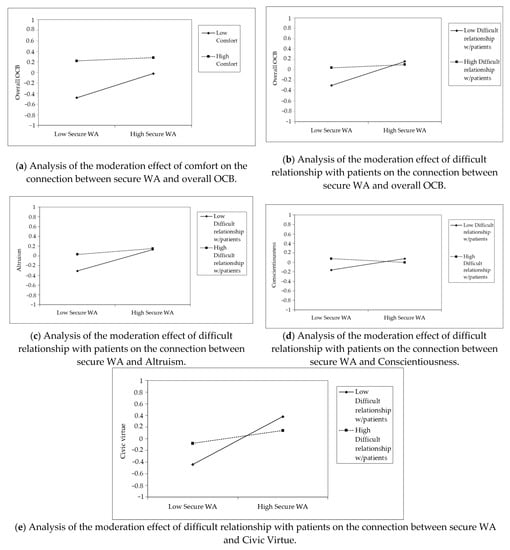
Figure 2.
Simple slope analysis of the moderation effect of perceived comfort and difficult relationship with patients, on the connection between secure WA and OCBs (Overall, Altruism, Conscientiousness, and Civic Virtue).
No statistically significant interaction between secure WA and perceived comfort emerged on the other dependent variables, Altruism (B = −0.08, p = n.s.) (Table 3), Conscientiousness (B = −0.11, p = n.s.) (Table 4) and Civic Virtue (B = −0.10, p = n.s.) (Table 5).
Likewise, the results relating to H4 do not highlight any direct effect of difficult relationship with patient with overall OCB (B = 0.07, p = n.s.) (Table 2), nor with the components of Altruism (B = 0.09, p = n.s.) (Table 3), Civic Virtue (B = 0.03, p = n.s.) (Table 4) and Conscientiousness (B = 0.04, p = n.s.) (Table 5).
The results referring to the interaction between secure WA and difficult relationship with patients fully support the hypotheses (H5): as emerged from the simple slope analysis, the interaction is negatively associated with overall OCB (B = −0.10, p < 0.01) (Table 2; Figure 2, Simple slope b), Altruism (B = −0.08, p < 0.05) (Table 3; Figure 2, Simple slope c), Conscientiousness (B = −0.08, p < 0.01) (Table 5; Figure 2, Simple slope d), and Civic Virtue (B = −0.15, p < 0.01) (Table 4; Figure 2, Simple slope e).
4. Discussion
Regarding H1, the emergence of the expected positive relationship between secure attachment to the workplace and organizational citizenship behaviors substantially confirmed what has been shown in other studies (e.g., [84]), especially with reference to altruistic and virtuous behavior towards the organization. However, previous evidence concerns indeed a different source of the secure attachment, that is the job itself rather than the workplace. Having said that, our results provide further proof about the importance of developing a secure attachment at work to promote positive behaviors.
About H2, it is substantially confirmed. In fact, in line with Carter et al. [88], caregivers’ perceived spatial-physical comfort in the work environment increases the likelihood of performing OCBs. In particular, the relationships emerged between perceived comfort and altruistic behaviors, this is in line with the negative effects of low comfort on workers’ altruism found in the study by Zoghbi-Manrique-de-Lara et al. [87].
Concerning H3, a pattern opposite to the one expected was found. In fact, perceived comfort played a buffering rather than an amplifying role in the moderation of the relationship between secure workplace attachment style and OCBs. It is to note that this was found only for the overall OCBs and not for the specific components. This counterintuitive finding, which requires further investigation, can be explained in terms of compensation provided by a comfortable environment for those caregivers with an insecure attachment to the workplace, whereas this environmental perception counts less in case of secure workplace attachment. In other words, the fact that operators perceive a condition of physical-spatial comfort overshadows (and depowers) the need for them to “draw on” their secure workplace attachment style as a motivational dimension capable of promoting their OCBs.
Regarding H4, contrary to what was expected, the difficulties faced by staff in their relationships with patients do not negatively affect their implementation of OCBs. A possible explanation for this lack of negative incidence can lie in the awareness that RFs operators have of the particular conditions, non-self-sufficiency, and often mental pathology of their patients (often suffering from senile dementia or similar disabling mental pathologies related to aging). This awareness can lead practitioners to a high level of tolerance and compassionate forbearance of the relational difficulties that may arise with these type of patients (see e.g., [79]), without negatively affecting their propensity to implement OCBs.
Finally, H5 is confirmed, since the difficulties in the relationships with patients adversely affect the relationship between caregivers’ secure workplace attachment and their OCBs (both general OCBs and the specific components, i.e., Altruism, Civic Virtue, and Conscientiousness). This result suggests that it is also important to consider the relational dimension of the secure workplace attachment style, both towards the social work environment (as found by Afshar et al. [50]) and towards users (consistently with findings of Alexandris et al. [51]). In this sense, it is therefore plausible that problematic relationships with users may depower the ability of the secure workplace attachment style to foster organizational citizenship behaviors.
This study has some limitations. The first one concerns the limited number of participants, due to the specific target population (i.e., staff of residential facilities who work with the elderly), that is not easy to reach and investigate for its special characteristics (including the difficulty to obtain access to elderly facilities for survey aims). In addition, participants were identified based on their availability, without a sampling method that would allow us representativeness of these workers and generalizability of our results. However, the sample number is good enough for ensuring the reliability of our results, given the low number of variables that we included in the tested moderation model. A second limitation is given by the lack of objective parameters of the design features, since we relied only on the staff assessment of their spatial-physical environment. Thus, future research should fill this gap by considering also objective indicators of the workplace environment, such as spatial configuration, lighting conditions, indoor and outdoor views, furniture, etc., to compare with users’ perceived comfort. Finally, it would be interesting to confirm our speculations about why the independent or moderating variables in our study did not affect OCBs (as for H4) or affected them in an unexpected way (i.e., the counterintuitive results related to H3) through the realization of a qualitative exploration (e.g., focus groups of semi-structured interviews) of practitioners’ views.
Despite these limitations, the outcomes of our study emphasize the importance of the joint consideration, for the implementation of OCBs in the RFs, and more generally in residential care settings, of dimensions tapping aspects concerning different socio-psychological interfaces, i.e., covering the overall context (including both the spatial-physical and the social environment), mirrored by the workplace attachment style; the spatial-physical environment, represented by the perceived environmental comfort; and finally the people facet, reflected by the relationships between staff and patients. In other words, this study highlights that, in order to promote positive caregiver behaviors (OCBs) towards older adults and the healthcare organization, it is crucial to jointly consider place-based dimensions, such as the workplace attachment style and the perceived environmental comfort, as well as the socio-relational dimension represented by the helping relationship towards patients.
5. Conclusions
Our study lies within the theoretical framework of positive organizational behaviors (POBs) enacted by individuals, teams, organizations, and the health network as a whole [8,99], in the light of the promotion of healthcare humanization for the older adults [82,83], consistently with a healthy and active aging perspective [1,2]. In this view, caregivers’ OCBs can be considered as desirable outcomes promoting HAA. From a practical point of view, the development of a secure attachment to the workplace can be fostered through listening to, engaging with, and meeting the needs of caregivers in care settings [65]. This should encourage them to be proactive in exploring innovative ways to benefit the organization and the patients (and thus enact organizational citizenship behaviors) and promote their work well-being [67]. Furthermore, the achievement or maintenance of a high level of physical-spatial comfort, according to an architectural humanization approach to the healthcare environments [72], requires the participation of the actors involved in the monitoring, evaluation, and improvement of the healthcare environments [74]. In addition, the quality of the staff-patients relationship in these settings from a patient-centered perspective [75] is particularly important for the elderly population. Therefore, it is appropriate that caregivers carry out periodically and systematically learning update activities for improving their listening skills [79], empathy [77,78], and assertiveness [81]. It is also important that caregivers benefit from supervision for avoiding the risks of exhaustion [89] or compassion fatigue [23] resulting from a poor helping relationship with patients that, for its emotional charge, can jeopardize their work well-being and hinder their commitment to active and healthy aging of the elderly.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph19020963/s1, Figure S1: Scree Plot of Exploratory Factor Analysis of the Organizational Citizenship Behavior Scale, Table S1: Results of Exploratory Factor Analysis (EFA) of the Organizational Citizenship Behavior Scale.
Author Contributions
Conceptualization, M.N., F.S. and F.F.; methodology, A.L.M. and F.F.; formal analysis, A.L.M. and F.F.; investigation, M.N. and S.C.; data curation, S.C. and A.L.M.; writing—original draft preparation, M.N., F.S. and F.F.; writing—review and editing, F.F.; visualization, A.L.M.; supervision, F.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the University of Cagliari (approval number 73624 dated 30 March 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Upon reasonable request, data used and analyzed during the current study are available from the corresponding author.
Acknowledgments
We thank the participants, without whom this study would never have been possible.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Stephens, C.; Breheny, M.; Mansvelt, J. Healthy ageing from the perspective of older people: A capability approach to resilience. Psychol. Health 2015, 30, 715–731. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Kubzansky, L.D.; Soo, J.; Boehm, J.K. Maintaining Healthy Behavior: A Prospective Study of Psychological Well-Being and Physical Activity. Ann. Behav. Med. 2017, 51, 337–347. [Google Scholar] [CrossRef] [PubMed]
- North, M.S.; Fiske, S.T. Modern Attitudes Toward Older Adults in the Aging World: A Cross-Cultural Meta-Analysis. Psychol. Bull. 2015, 141, 993–1021. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitama, S.; Berg, M.K.; Chopik, W.J. Culture and Well-Being in Late Adulthood: Theory and Evidence. Am. Psychol. 2020, 75, 567–576. [Google Scholar] [CrossRef] [PubMed]
- WHO. Age-Friendly Environments in Europe: Indicators, Monitoring and Assessments. 2018. Available online: https://www.euro.who.int/en/health-topics/Life-stages/healthy-ageing/publications (accessed on 24 October 2021).
- AUSER. Le Case di Riposo in Italia. Prima Ricerca Nazionale Auser Sulle Case di Riposo. 2011. Available online: https://www.auser.it/cosa-facciamo/aiuto-alla-persona/indagine-auser-case-di-riposo (accessed on 27 September 2021).
- Rapporto OASI. Osservatorio sulle Aziende e sul Sistema Sanitario Italiano; Cergas, Università Bocconi: Milan, Italy, 2020; Available online: https://cergas.unibocconi.eu/sites/default/files/files/1_OASI2020.pdf (accessed on 2 November 2021).
- Braithwaite, J.; Herkes, J.; Ludlow, K.; Testa, L.; Lamprell, G. Association between organizational and workplace cultures, and patient outcomes: Systematic review. BMJ Open 2017, 7, e017708. [Google Scholar] [CrossRef] [Green Version]
- Ministero della Salute. Prestazioni Residenziali e Semiresidenziali. 2021. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_646_allegato.pdf (accessed on 28 October 2021).
- Sun, C.; Ding, Y.; Cui, Y.; Zhu, S.; Li, X.; Chen, S.; Zhou, R.; Yu, Y. The adaptation of older adults’ transition to residential care facilities and cultural factors: A meta-synthesis. BMC Geriatr. 2021, 21, 64. [Google Scholar] [CrossRef]
- van Loon, J.; Luijkx, K.; Janssen, M.; de Rooij, I.; Janssen, B. Facilitators and barriers to autonomy: A systematic literature review for older adults with physical impairments, living in residential care facilities. Ageing Soc. 2021, 41, 1021–1050. [Google Scholar] [CrossRef] [Green Version]
- Borbasi, S.; Galvin, K.T.; Adams, T.; Todres, L.; Farrelly, B. Demonstration of the usefulness of a theoretical framework for humanising care with reference to a residential aged care service in Australia: Humanising Residential Dementia Care. J. Clin. Nurs. 2012, 22, 881–889. [Google Scholar] [CrossRef]
- Pascuci, L.; Meyer, V.; Nogueira, E.E.; Forte, L.T. Humanization in a Hospital: A Change Process Integrating Individual, Organizational and Social Dimensions. J. Health Manag. 2017, 192, 224–243. [Google Scholar] [CrossRef]
- Gharaveis, A. A systematic framework for understanding environmental design influences on physical activity in the elderly population: A review of literature. Facilities 2020, 38, 625–6493. [Google Scholar] [CrossRef]
- Gagliardi, C.; Piccinini, F. The use of nature—Based activities for the well-being of older people: An integrative literature review. Arch. Gerontol. Geriatr. 2019, 83, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Fornara, F.; Manca, S. Healthy residential environments for the elderly. In Handbook of Environmental Psychology and Quality of Life Research; Fleury-Bahi, G., Pol, E., Navarro, O., Eds.; Springer: Berlin, Germany, 2017; pp. 441–465. [Google Scholar] [CrossRef]
- Devi, R.; Martin, G.; Banerjee, J.; Butler, L.; Pattison, T.; Cruickshank, L.; Maries-Tillott, C.; Wilson, T.; Damery, S.; Meyer, J.; et al. Improving the Quality of Care in Care Homes Using the Quality Improvement Collaborative Approach: Lessons Learnt from Six Projects Conducted in the UK and The Netherlands. Int. J. Environ. Res. Public Health 2020, 17, 7601. [Google Scholar] [CrossRef] [PubMed]
- Venturato, L.; Horner, B.; Etherton-Beer, C. Development and evaluation of an organisational culture change intervention in residential aged care facilities. Australas J. Ageing 2019, 39, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Delgado, C.; Upton, D.; Ranse, K.; Furness, T.; Foster, K. Nurses’ resilience and the emotional labour of nursing work: An integrative review of empirical literature. Int. J. Nurs. Stud. 2017, 70, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Duarte, J.; Pinto-Gouveia, J. Empathy and feelings of guilt experienced by nurses: A cross-sectional study of their role in burnout and compassion fatigue symptoms. Appl. Nurs. Res. 2017, 35, 42–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campana, K.L.; Hammoud, S. Incivility from patients and their families: Can organisational justice protect nurses from burnout? J. Nurs. Manag. 2015, 23, 716–725. [Google Scholar] [CrossRef]
- Hasson, H.; Arnetz, J.E. Nursing staff competence, work strain, stress and satisfaction in elderly care: A comparison of home-based care and nursing homes. J. Clin. Nurs. 2008, 174, 468–481. [Google Scholar] [CrossRef]
- Giesbrecht, M.; Stajduhar, K.I.; Cloutier, D. “We are to be like machines...fill the bed before it gets cold”: Exploring the emotional geographies of healthcare providers caring for dying residents in long-term care facilities. Soc. Sci. Med. 2021, 272, 113749. [Google Scholar] [CrossRef]
- Annear, M.; Keeling, S.; Wilkinson, T.; Cushman, G.; Gidlow, B.; Hopkins, H. Environmental influences on healthy and active ageing: A systematic review. Ageing Soc. 2014, 34, 590–622. [Google Scholar] [CrossRef]
- Gardner, W.; States, D.; Bagley, N. The Coronavirus and the Risks to the Elderly in Long-Term Care. J. Aging Soc. Policy 2020, 32, 310–315. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Istituto Superiore di Sanità. Survey Nazionale sul Contagio COVID-19 Nelle Strutture Residenziali e Sociosanitarie. Report Finale. 2020. Available online: https://www.epicentro.iss.it/coronavirus/pdf/sars-cov-2-survey-rsa-rapporto-finale.pdf (accessed on 10 October 2021).
- Foà, C.; Guarnieri, M.C.; Bastoni, G.; Benini, B.; Giunti, O.M.; Mazzotti, M.; Rossi, C.; Savoia, A.; Sarli, L.; Artioli, G. Job satisfaction, work engagement and stress/burnout of elderly care staff: A qualitative research. Acta Biomed. Health Prof. 2020, 91, 2020014. [Google Scholar] [CrossRef]
- Aloisio, L.D.; Baumbusch, J.; Estabrooks, C.A.; Bostrom, A.-M.; Chamberlain, S.; Cummings, G.C.; Thompson, G.; Squires, J.E. Factors affecting job satisfaction in long-term care unit managers, directors of care and facility administrators: A secondary analysis. J. Nurs. Manag. 2019, 27, 1764–1772. [Google Scholar] [CrossRef]
- Laitinen, P.; Isola, A. Promoting participation of informal caregivers in the hospital care of the elderly patient: Informal caregivers’ perceptions. J. Adv. Nurs. 1996, 23, 942–947. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.; Ream, E.; Richardson, A.; Thomas, H.; Andrews, P.; Campbell, P.; Dawson, T.; Edwards, J.; Goldie, T.; Hammick, M.; et al. Cancer related fatigue—A difference of opinion ? Results of a multicentre survey of healthcare professionals, patients and caregivers. Eur. J. Cancer Care 2003, 12, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Organ, D.W. Organizational Citizenship Behavior: The Good Soldier Syndrome; Lexington Books: Lexington, MA, USA, 1988. [Google Scholar]
- Organ, D.W.; Ryan, K. A meta-analitic review of attitudinal and dispositional predictors of organizational citizenship behavior. Pers. Psychol. 1995, 48, 775–802. [Google Scholar] [CrossRef]
- Singh, U.; Srivastava, K.B.L. Organizational trust and Organizational citizenship behaviour. Glob. Bus. Rev. 2016, 173, 594–609. [Google Scholar] [CrossRef]
- Ocampo, L.; Acedillo, V.; Bacunador, A.M.; Balo, C.C.; Lagdameo, Y.J.; Tupa, N.S. A historical review of the development of Organizational citizenship behavior (OCB) and its implications for the twenty-first century. Pers. Rev. 2018, 47, 821–862. [Google Scholar] [CrossRef]
- Podsakoff, P.M.; Mackenzie, S.B.; Moorman, R.H.; Fetter, R. Transformational leader behaviors and their effects on followers’ trust in leader, satisfaction and Organizational citizenship behavior. Leadersh. Q. 1990, 1, 107–142. [Google Scholar] [CrossRef]
- Shanker, M. Organizational Citizenship Behavior Dimensions in Indian Companies. IJRSI 2014, 1, 25–28. [Google Scholar]
- Organ, D.W.; Podsakoff, P.M.; MacKenzie, S.B. Organizational Citizenship Behavior: Its Nature, Antecedents, and Consequences; Sage Publications: Thousand Oaks, CA, USA, 2006. [Google Scholar]
- Organ, D.W. Organizational Citizenship Behavior: Recent Trends and Developments. Annu. Rev. Organ. Psych. 2018, 5, 295–306. [Google Scholar] [CrossRef]
- Podsakoff, N.P.; Podsakoff, P.M.; Mackenzie, S.B.; Maynes, T.D.; Spoelma, T.M. Consequences of unit-level organizational citizenship behaviors: A review and recommendations for future research. J. Organ. Behav. 2014, 35, S87–S119. [Google Scholar] [CrossRef]
- Jahani, M.A.; Mahmoudjanloo, S.; Rostami, F.H.; Nikbakht, H.A.; Mahmoudi, G. Datasets on Organizational citizenship behavior in the selected hospitals with different ownership. Data Brief 2018, 19, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Ranjhan, S.; Mallick, E. Organizational citizenship behaviour creating competitive advantage in Indian health care industry: The moderating role of HR practices. Glob. Bus. Rev. 2018, 19, 1275–1289. [Google Scholar] [CrossRef]
- Saleh, A.; Wirawan, H.; Tamar, M. Improving Health Care Service through Healthy Psychological Capital and Positive Attitudes. Int. J. Adv. Sci. Eng. Inf. Technol. 2020, 10, 11723–11730. [Google Scholar] [CrossRef]
- Ginsburg, L.; Berta, W.; Baumbusch, J.; Rohit Dass, A.; Laporte, A.; Reid, C.; Squires, J.; Taylor, D. Measuring Work Engagement, Psychological Empowerment, and Organizational Citizenship Behavior among Health Care Aides. Gerontologist 2016, 56, e1–e11. [Google Scholar] [CrossRef] [Green Version]
- Perreira, T.A.; Berta, W.; Laporte, A.; Ginsburg, L.; Deber, R.; Elliott, G.; Lum, J. Shining a Light: Examining Similarities and Differences in the Work Psychology of Health Support Workers Employed in Long-Term Care and Home and Community Care Settings. J. Appl. Gerontol. 2019, 38, 1595–1614. [Google Scholar] [CrossRef]
- Low, S.M.; Altman, I. Place Attachment; Springer: Boston, MA, USA, 1992; pp. 1–12. [Google Scholar] [CrossRef]
- Stokols, D.; Shumaker, S.A. People in places: A transactional view of settings. In Cognition, Social Behavior, and the Environment; Harvey, J., Ed.; Erlbaum: Hillsdale, NJ, USA, 1981; pp. 441–488. [Google Scholar]
- Williams, D.R.; Patterson, M.E. Environmental psychology: Mapping landscape meanings for ecosystem management. In Integrating Social Sciences and Ecosystem Management: Human Dimensions in Assessment, Policy and Management; Cordell, H.K., Bergstrom, J.C., Eds.; Sagamore Press: Champaign, IL, USA, 1999; pp. 141–160. [Google Scholar]
- Proshansky, H.M.; Fabian, A.K.; Kaminoff, R. Place-identity: Physical world socialization of the self. J. Environ. Psychol. 1983, 3, 57–83. [Google Scholar] [CrossRef]
- Maricchiolo, F.; Mosca, O.; Paolini, D.; Fornara, F. The mediating role of Place Attachment dimensions in the relationship between local community identity and well-being. Front. Psychol. 2021, 12, 2643. [Google Scholar] [CrossRef]
- Afshar, P.F.; Foroughan, M.; Vedadhir, A.; Tabatabaei, M.G. The effects of place attachment on social well-being in older adults. Educ. Gerontol. 2017, 43, 45–51. [Google Scholar] [CrossRef]
- Alexandris, K.; Kouthouris, C.; Meligdis, A. Increasing customers’ loyalty in a skiing resort: The contribution of place attachment and service quality. Int. J. Contemp. Hosp. Manag. 2006, 18, 414–425. [Google Scholar] [CrossRef]
- Vaske, J.J.; Kobrin, K.C. Place attachment and environmentally responsible behavior. J. Environ. Educ. 2001, 32, 16–21. [Google Scholar] [CrossRef]
- Ríos, M.L.; Moreno-Jiménez, M.P. Place identity and residential satisfaction: Differences between native and immigrant populations. Psyecology 2012, 3, 75–86. [Google Scholar] [CrossRef]
- De Dominicis, S.; Fornara, F.; Cancellieri, U.G.; Twigger-Ross, C.; Bonaiuto, M. We are at risk, and so what? Place attachment, environmental risk perceptions and preventive coping behaviours. J. Environ. Psychol. 2015, 43, 66–78. [Google Scholar] [CrossRef]
- Bowlby, J. Attachment and Loss; Basic Books: New York, NY, USA, 1969; Volume 1. [Google Scholar]
- Scannell, L. The Bases of Bonding: The Psychological Functions of Place Attachment in Comparison to Interpersonal Attachment. Ph.D. Thesis, Philosophy, Department of Psychology, University of Victoria, Victoria, Canada, 2013. Unpublished. [Google Scholar]
- Morgan, P. Towards a developmental theory of place attachment. J. Environ. Psychol. 2010, 30, 11–22. [Google Scholar] [CrossRef]
- Little, S.; Derr, V. The Influence of Nature on a Child’s Development: Connecting the Outcomes of Human Attachment and Place Attachment. In Research Handbook on Childhoodnature; Springer International Handbooks of Education; Cutter-Mackenzie-Knowles, A., Malone, K., Barratt Hacking, E., Eds.; Springer: Cham, Switzerland, 2020; pp. 151–178. [Google Scholar] [CrossRef]
- Little, S. Wild Boys of the Creek: Autonomous Exploration of a Leftover Space in Raleigh. Ph.D. Thesis, North Carolina State University, Raleigh, NC, USA, 2016. Unpublished. [Google Scholar]
- Belanche, D.; Casaló, L.V.; Orús, C. City attachment and use of urban services: Benefits for smart cities. Cities 2016, 50, 75–81. [Google Scholar] [CrossRef]
- Lewicka, M. What makes neighborhood different from home and city? Effects of place scale on place attachment. J. Environ. Psychol. 2010, 30, 35–51. [Google Scholar] [CrossRef]
- Rioux, L. Construction d’une échelle d’attachement au lieu de travail: Une démarche exploratoire. Can. J. Behav. Sci.-Rev. Can. Sci. Comport. 2006, 38, 325–336. [Google Scholar] [CrossRef]
- Scrima, F.; Rioux, L.; Di Stefano, G. I hate my workplace but I am very attached to it: Workplace attachment style: An exploratory approach. Pers. Rev. 2017, 46, 936–949. [Google Scholar] [CrossRef]
- Bartholomew, K.; Horowitz, L.M. Attachment styles among young adults: A test of a four-category model. J. Pers. Soc. Psychol. 1991, 61, 226–244. [Google Scholar] [CrossRef]
- Scannell, L.; Gifford, R. The experienced psychological benefits of place attachment. J. Environ. Psychol. 2017, 51, 256–269. [Google Scholar] [CrossRef]
- Fried, M. Continuities and discontinuities of place. J. Environ. Psychol. 2000, 20, 193–205. [Google Scholar] [CrossRef]
- Stancu, A.; Ariccio, S.; De Dominicis, S.; Cancellieri, U.G.; Petruccelli, I.; Ilin, C.; Bonaiuto, M. The better the bond, the better we cope. The effects of place attachment intensity and place attachment styles on the link between perception of risk and emotional and behavioral coping. Int. J. Disaster Risk Reduct. 2020, 51, 101771. [Google Scholar] [CrossRef]
- Rashid, M.; Zimring, C. A review of the empirical literature on the relationship between indoor environment and stress in health care and office settings. Environ. Behav. 2008, 40, 151–190. [Google Scholar] [CrossRef]
- Bellini, D.; Fornara, F.; Bonaiuto, M. Positive environment in the workplace: The case of the mediating role of work engagement between restorativeness and job satisfaction. Psyecology 2015, 6, 252–286. [Google Scholar] [CrossRef]
- Ulrich, R.S.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.B.; Choi, Y.S.; Xiaobo, Q.; Joseph, A. A review of the research literature on evidence-based healthcare design. Herd-Health Env. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Evans, G.; McCoy, J. When buildings don’t work: The role of architecture in human health. J. Environ. Psychol. 1998, 18, 85–94. [Google Scholar] [CrossRef] [Green Version]
- Nagasawa, Y. The geography of hospitals. In Theoretical Perspectives in Environment-Behavior Research; Wapner, S., Demick, J., Yamamoto, T., Minani, H., Eds.; Kluwer: New York, NY, USA, 2000; pp. 217–227. [Google Scholar] [CrossRef]
- Andrade, C.; Lima, L.; Fornara, F.; Bonaiuto, M. Users’ views of hospital environmental quality: Validation of the Perceived Hospital Environment Quality Indicators (PHEQIs). J. Environ. Psychol. 2012, 32, 97–111. [Google Scholar] [CrossRef]
- Fornara, F.; Andrade, C. Healthcare environments. In The Oxford Handbook of Environmental and Conservation Psychology; Clayton, S., Ed.; Oxford University Press: New York, NY, USA, 2012; pp. 295–315. [Google Scholar] [CrossRef]
- Kitson, A.; Marshall, A.; Bassett, K.; Zeitz, K. What are the core elements of patient centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J. Adv. Nurs. 2012, 69, 4–15. [Google Scholar] [CrossRef]
- Davis, J.; Foley, A.; Crigger, N.; Brannigan, M.C. Healthcare and listening: A relationship for caring. Int. J. Listening 2008, 22, 168–175. [Google Scholar] [CrossRef]
- Hojat, M.; Louis, D.Z.; Markham, F.W.; Wender, R.; Rabinowitz, C.; Gonnella, J.S. Physicians’ empathy and clinical outcomes for diabetic patients. Acad. Med. 2011, 86, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Mealem, Y.; Siniver, E.; Yaniv, G. Patient compliance, physician empathy and financial incentives within a principal-agent framework. J. Socio-Econ. 2012, 41, 827–830. [Google Scholar] [CrossRef]
- Jagosh, J.; Boudreau, D.J.; Steinert, Y.; MacDonald, M.; Ingram, L. The importance of physician listening from the patients’ perspective: Enhancing diagnosis, healing, and the doctor–patient relationship. Patient Educ. Couns. 2011, 85, 369–374. [Google Scholar] [CrossRef] [PubMed]
- Salazar, I.C.; Roldán, G.M.; Garriddo, L.; Parejo, J.M.R. La asertividad y su relación con los problemas emocionales y el desgaste en profesionales sanitarios. Psicol. Conductual 2014, 22, 523–549. [Google Scholar]
- Cuccu, S.; Nonnis, M.; Cortese, C.G.; Massidda, D.; Altoè, G. The physician-patient relationship: A study of the psychometric properties of an interdependence scale. BPA Appl. Psychol. Bull. 2015, 272, 33–41. [Google Scholar]
- Melo, R.C.C.P.; Costa, P.J.; Henriques, L.V.L.; Tanaka, L.H.; Queirós, P.J.P.; Araújo, J.P. Humanitude in the humanization of elderly care: Experience reports in a health service. Rev. Bras. Enferm. 2019, 72, 825–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López, J.; Pérez-Rojo, G.; Noriega, C.; Velasco, C. Personal and work-related factors associated with good care for institutionalized older adults. Int. J. Environ. Res. Public Health 2021, 18, 820. [Google Scholar] [CrossRef] [PubMed]
- Desivilya, H. Prosocial tendencies in organizations: The role of attachment styles and organizational justice in shaping organizational citizenship behavior. Int. J. Organ. Anal. 2006, 14, 22–42. [Google Scholar] [CrossRef]
- Harms, P.D.; Bai, Y.; Han, G.H. How leader and follower attachment styles are mediated by trust. Hum. Relat. 2016, 69, 1853–1876. [Google Scholar] [CrossRef]
- Reizer, A. Bringing self-kindness into the workplace: Exploring the mediating role of self-compassion in the associations between attachment and organizational outcomes. Front. Psychol. 2019, 10, 1148. [Google Scholar] [CrossRef]
- Zoghbi-Manrique-de-Lara, P.; Sharifiatashgah, M. An Affective Events Model of the Influence of the Physical Work Environment on Interpersonal Citizenship Behavior. J. Work Organ. Psychol. 2020, 36, 27–37. [Google Scholar] [CrossRef] [Green Version]
- Carter, K.M.; Harman, D.M.; Walter, S.L.; Gruca, T.S. Relationship of immediate workspace and environmental workplace with organizational citizenship behaviors. J. Manag. Psychol. 2020, 36, 310–326. [Google Scholar] [CrossRef]
- Scrima, F.; Mura, A.L.; Nonnis, M.; Fornara, F. The relation between workplace attachment style, design satisfaction, privacy and exhaustion in office employees: A moderated mediation model. J. Environ. Psychol. 2021, 78, 101693. [Google Scholar] [CrossRef]
- Jafarpanah, M.; Behrooz Rezaei, B. Association between organizational citizenship behavior and patient safety culture from nurses’ perspectives: A descriptive correlational study. BMC Nurs. 2020, 19, 24. [Google Scholar] [CrossRef] [Green Version]
- Wibowo, T.S.; Mochklas, M. Urgency of organizational citizenship behavior towards performance of nurses of Type-C hospitals in Surabaya. Int. J. Sci. Technol. Res. 2020, 9, 4534–4538. [Google Scholar]
- Perreira, T.; Berta, W.; Ginsburg, L.; Barnsley, J.; Herbert, M. Insights into nurses’ work: Exploring relationships among work attitudes and work-related behaviors. Health Care Manag. Rev. 2018, 43, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Lavee, E.; Pindek, S. The Costs of Customer Service Citizenship Behaviors: A Qualitative Study. Front. Psychol. 2020, 11, 460. [Google Scholar] [CrossRef]
- Argentero, P.; Cortese, C.G.; Ferretti, M.S. An evaluation of Organizational citizenship behavior: Psychometric characteristics of the Italian version of Podsakoff et al.’s scale. TPM—Test. Psichometrics Methodol. Appl. Psychol. 2008, 15, 61–75. [Google Scholar] [CrossRef]
- Scrima, F. The psychometric properties of the workplace attachment style questionnaire. Curr. Psychol. 2020, 39, 2285–2292. [Google Scholar] [CrossRef]
- Fornara, F.; Bonaiuto, M.; Bonnes, M. Perceived hospital environment quality indicators: A study of orthopaedic units. J. Environ. Psychol. 2006, 26, 321–334. [Google Scholar] [CrossRef]
- Dormann, C.; Zapf, D. Customer-Related Social Stressors and Burnout. J. Occup. Health Psychol. 2004, 9, 61–82. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. An index and test of linear moderated mediation. Multivariate Behav. Res. 2015, 50, 1–22. [Google Scholar] [CrossRef]
- Pavithra, A. Towards developing a comprehensive conceptual understanding of positive hospital culture and approaches to healthcare organizational culture change in Australia. J. Health Organ. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).