Factors Involved in the Perception of Enamel Dyschromic Lesions—A Questionnaire-Based Study
Abstract
:1. Introduction
2. Materials and Methods
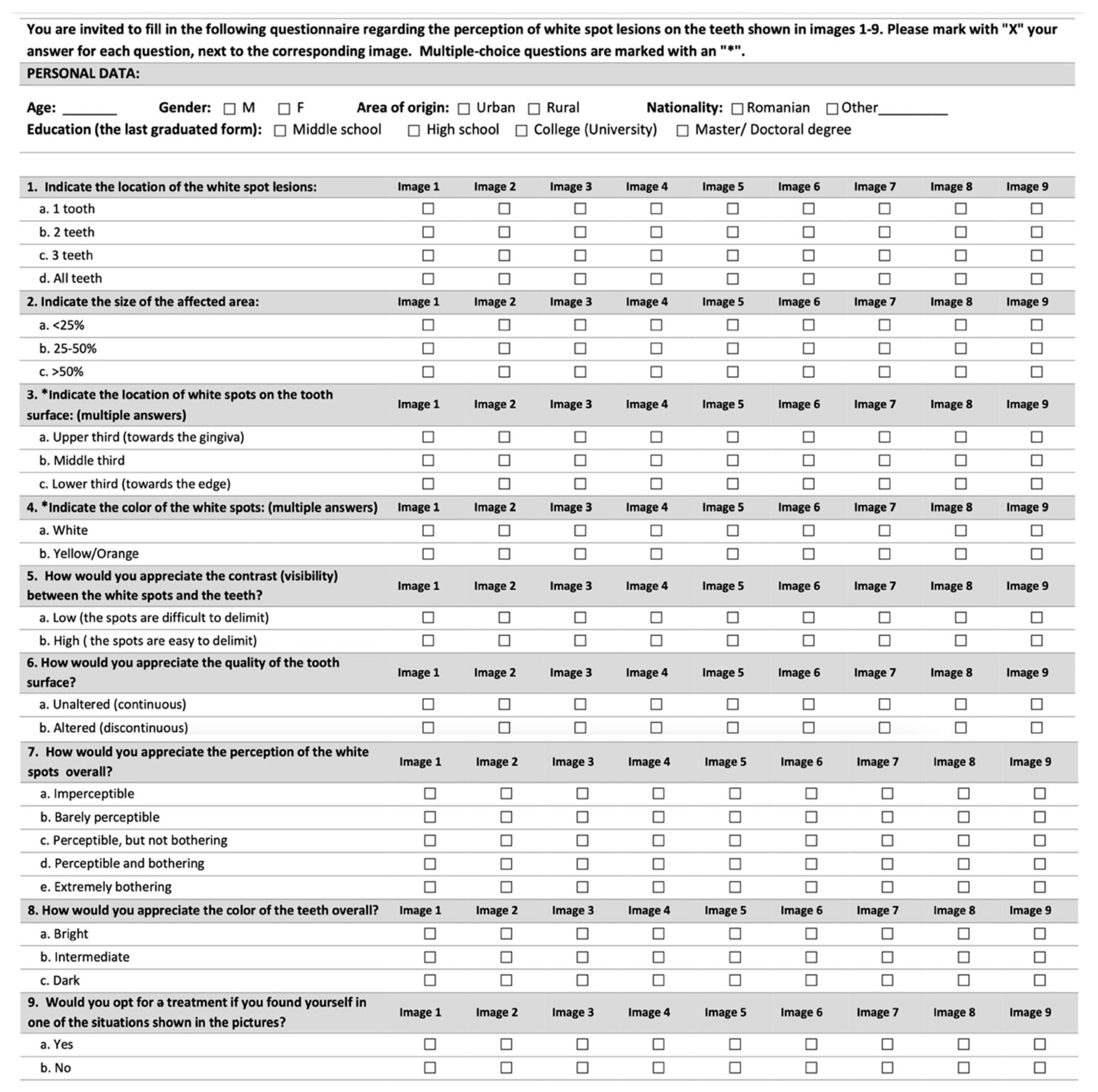
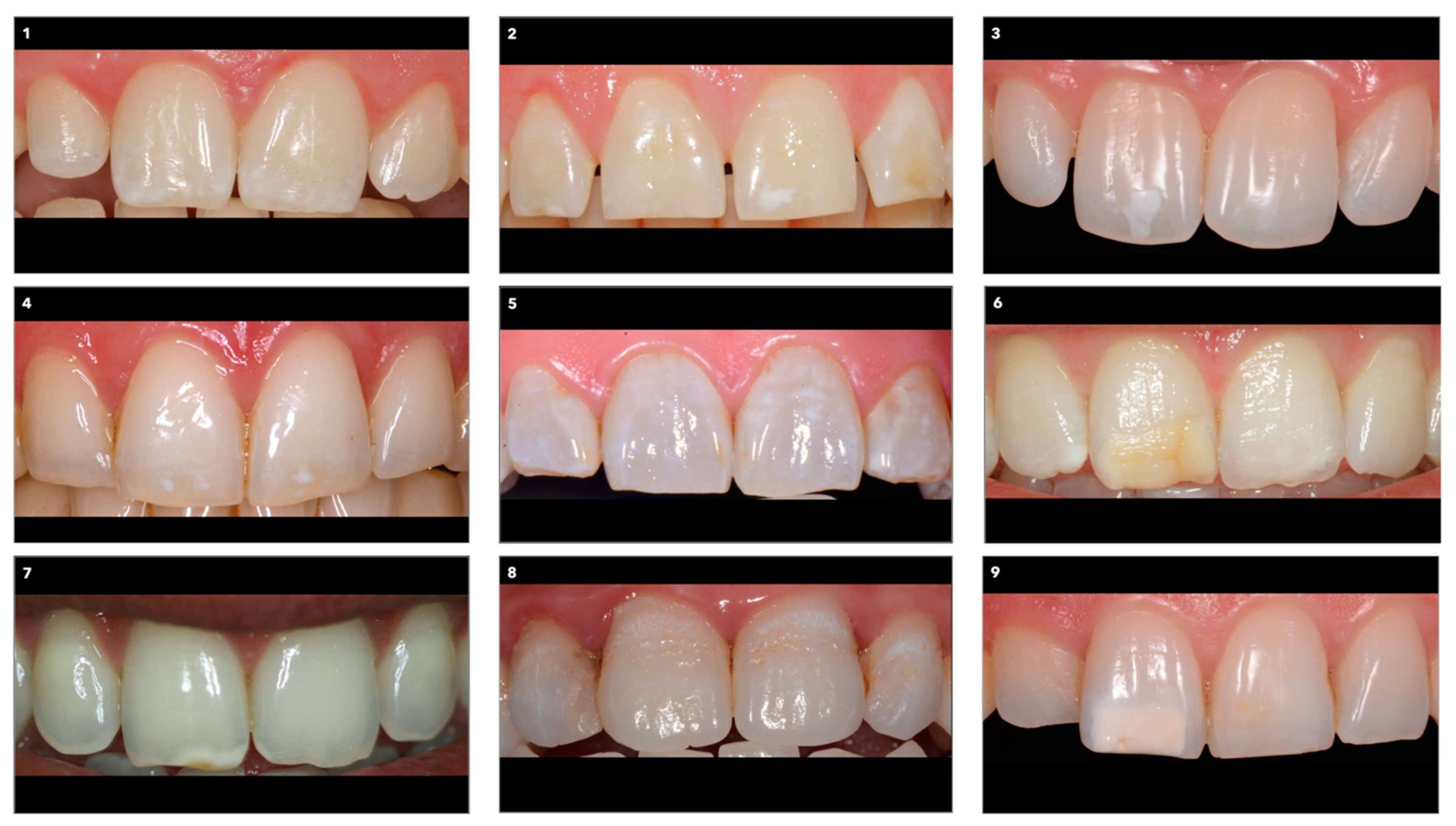
2.1. The Questionnaire
2.2. The Participants
2.3. Statistical Analyses
3. Results
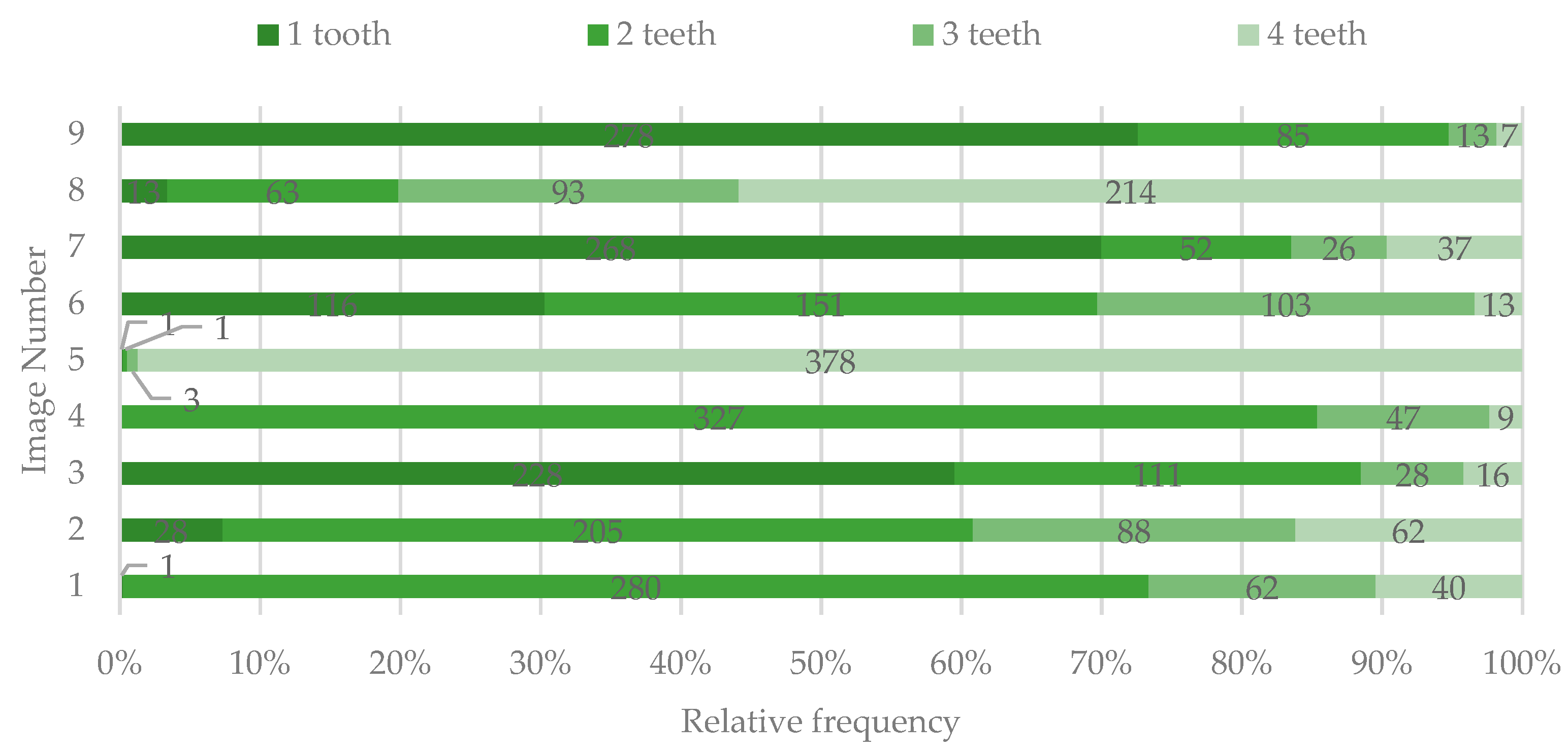
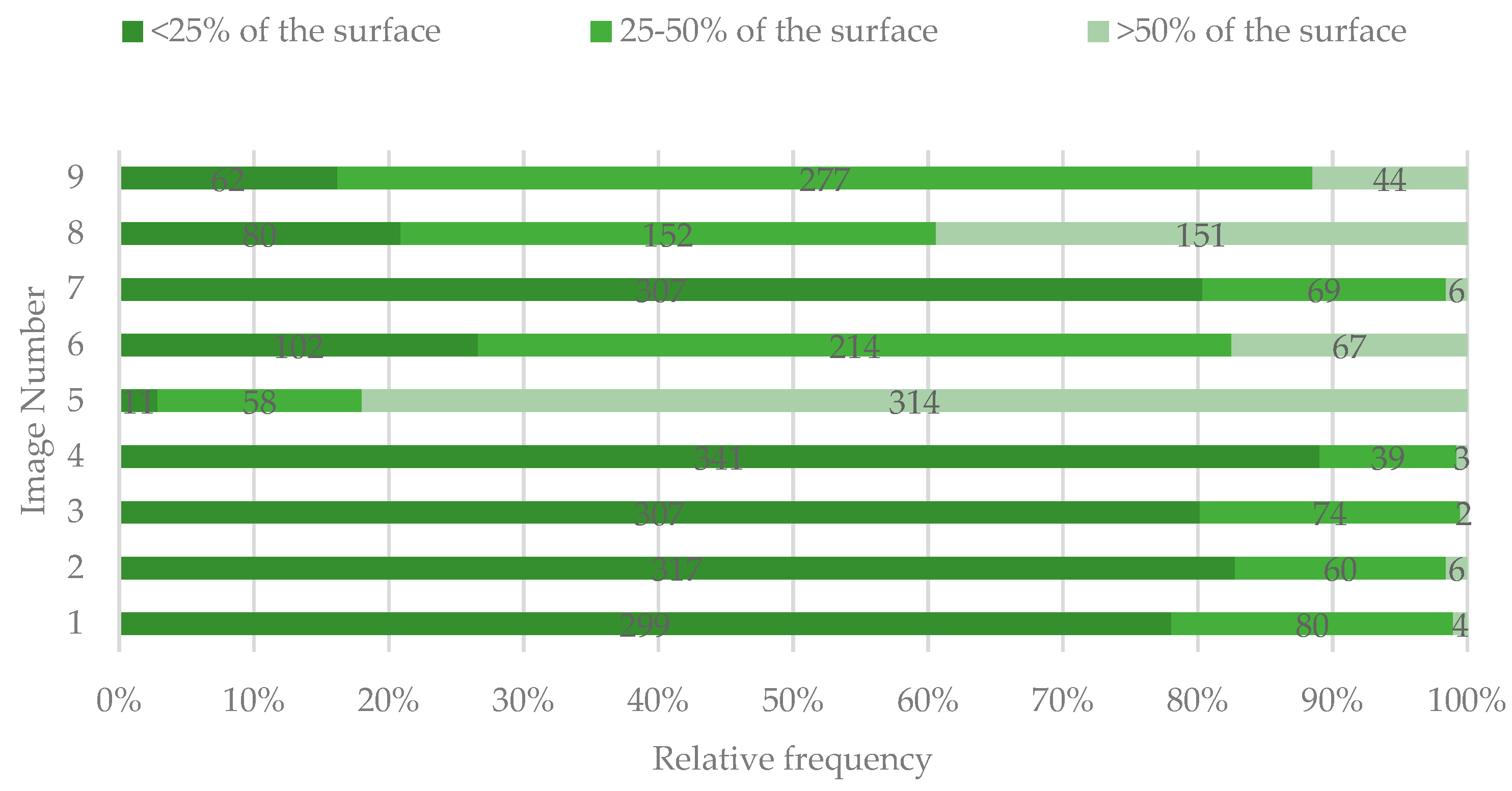
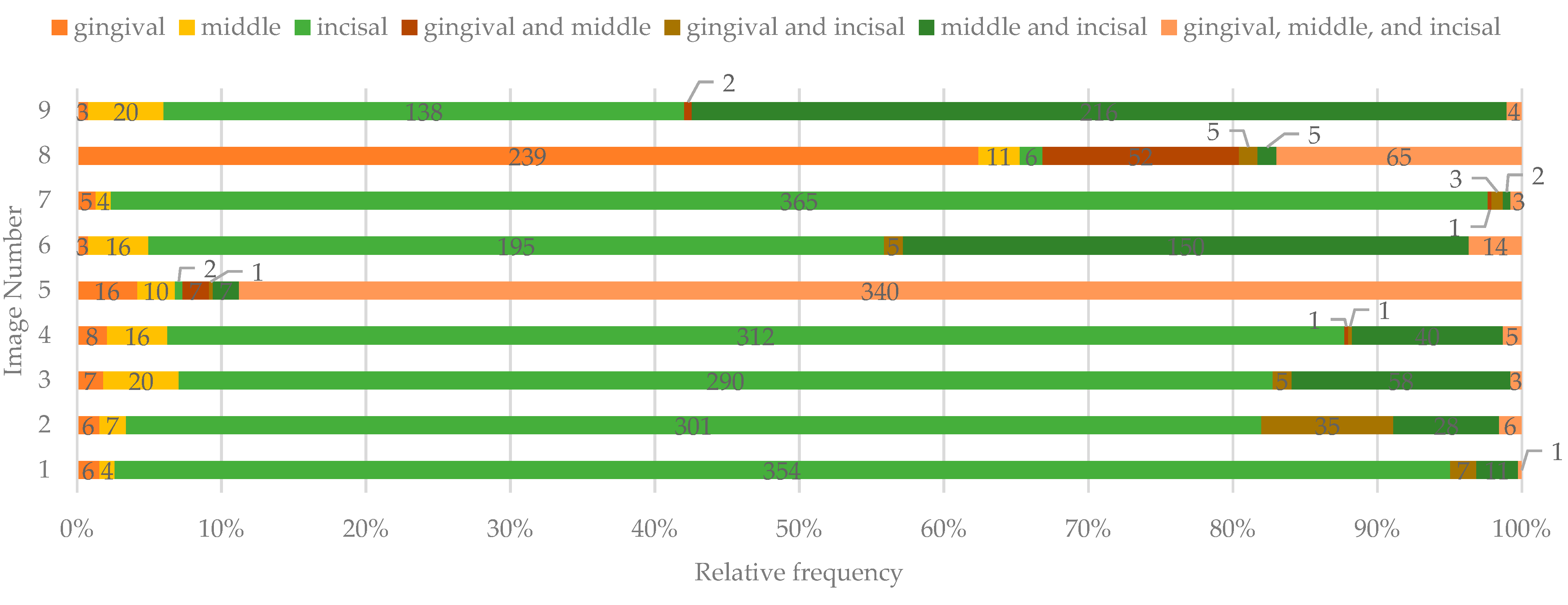
3.1. Location of the DLs (WSLs and Color-Affected Areas) of the Teeth
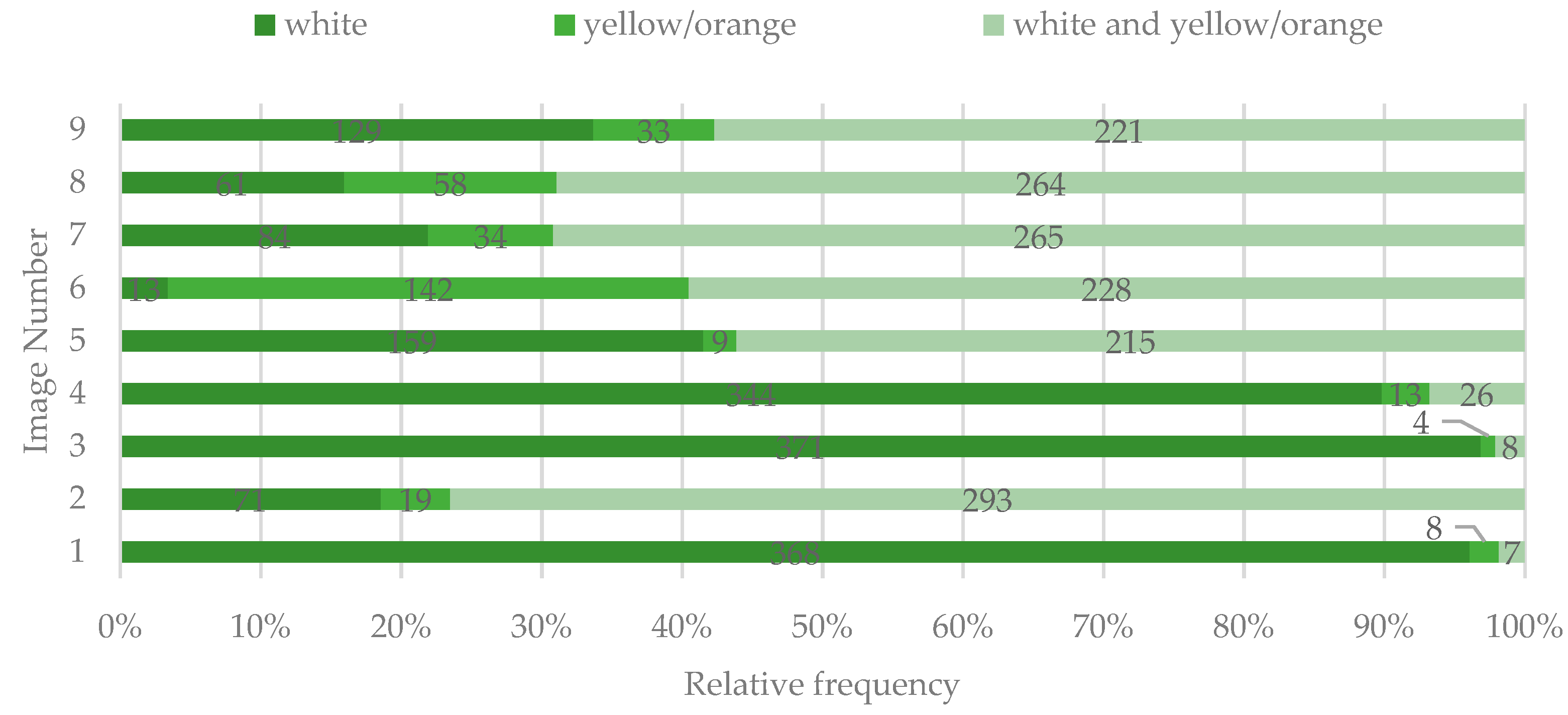
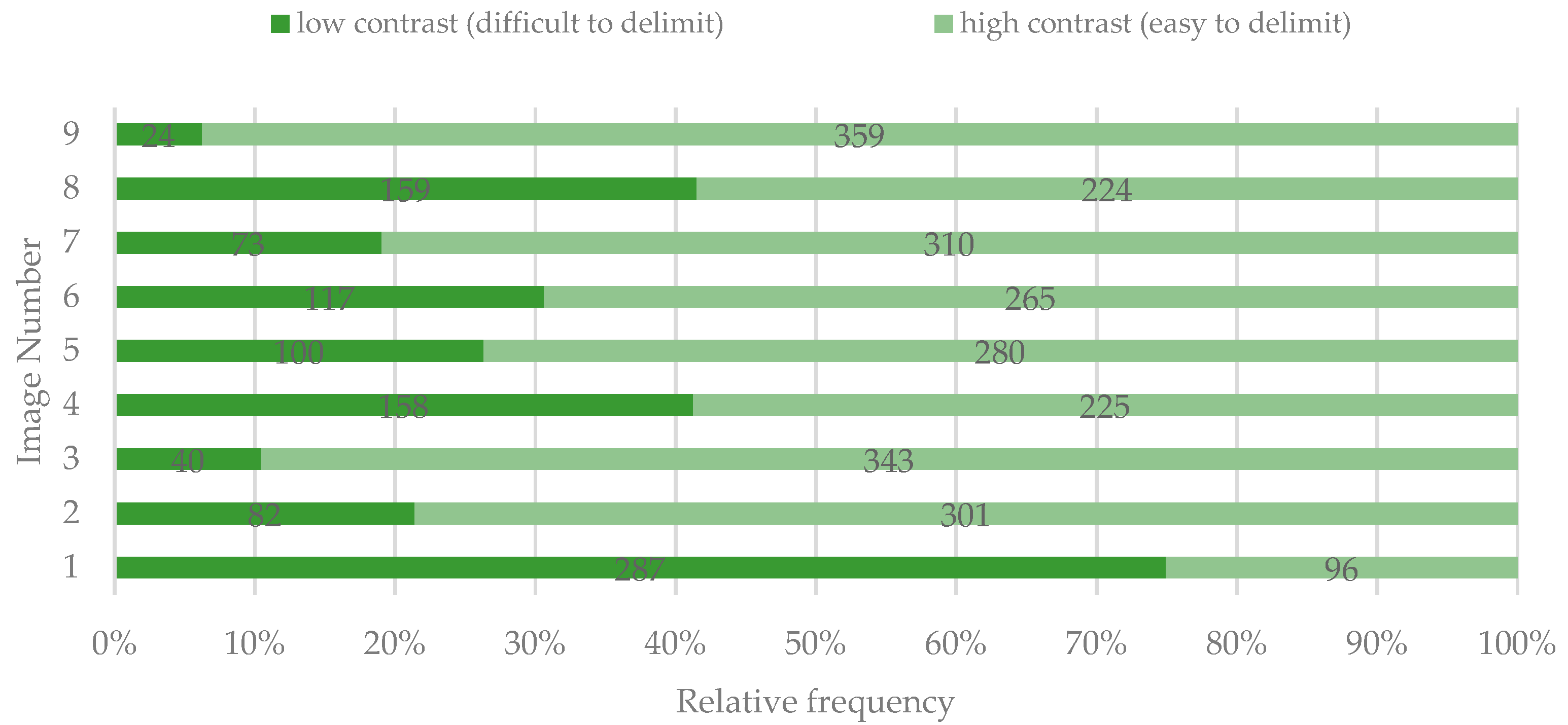
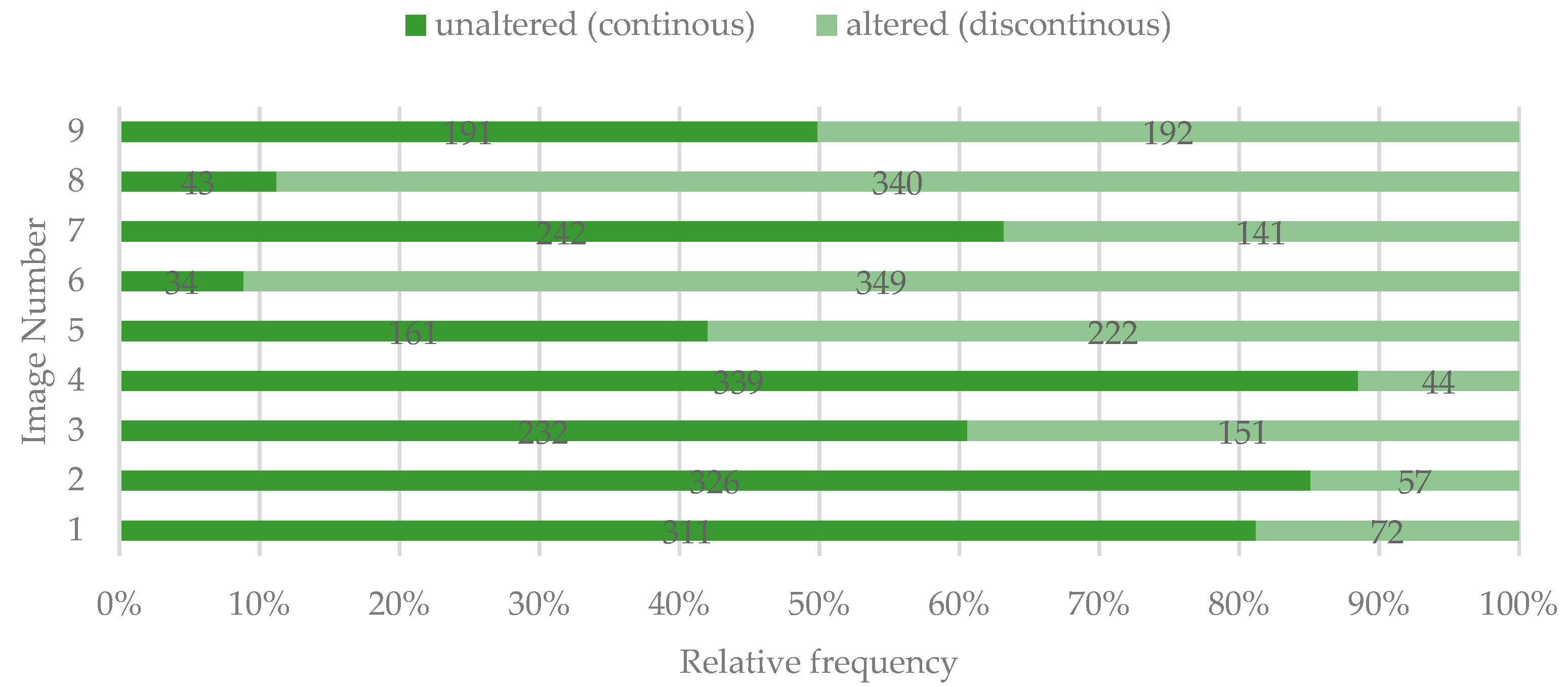
3.2. Color, Contrast, and Surface Texture of the DLs
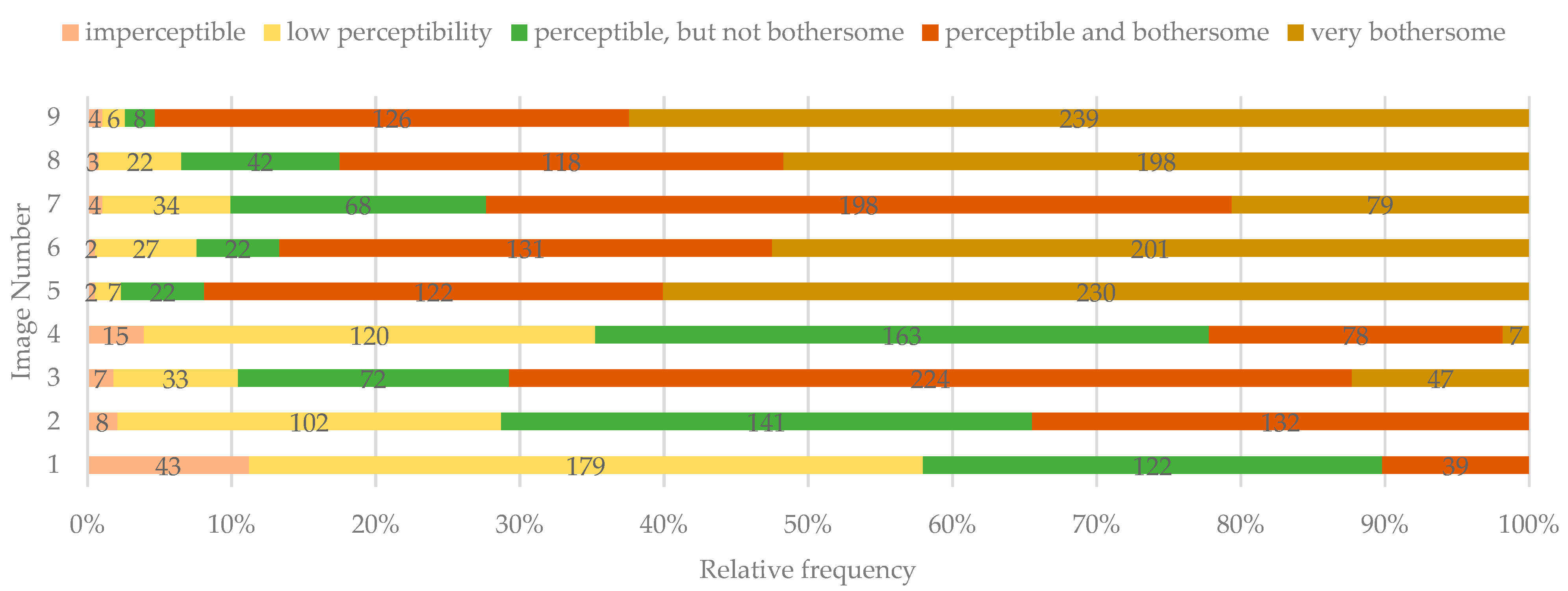
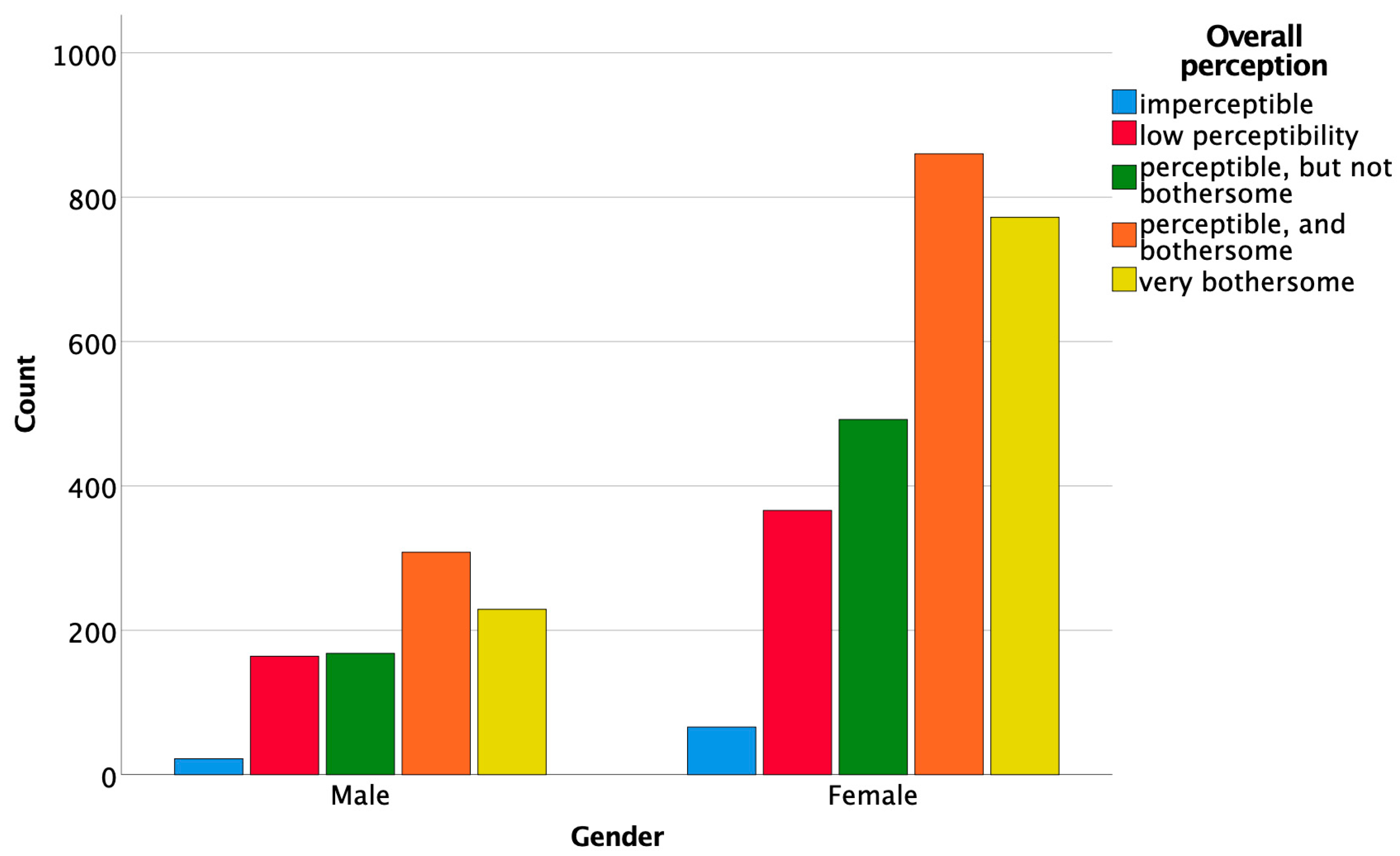
3.3. The Overall Perception of the DLs
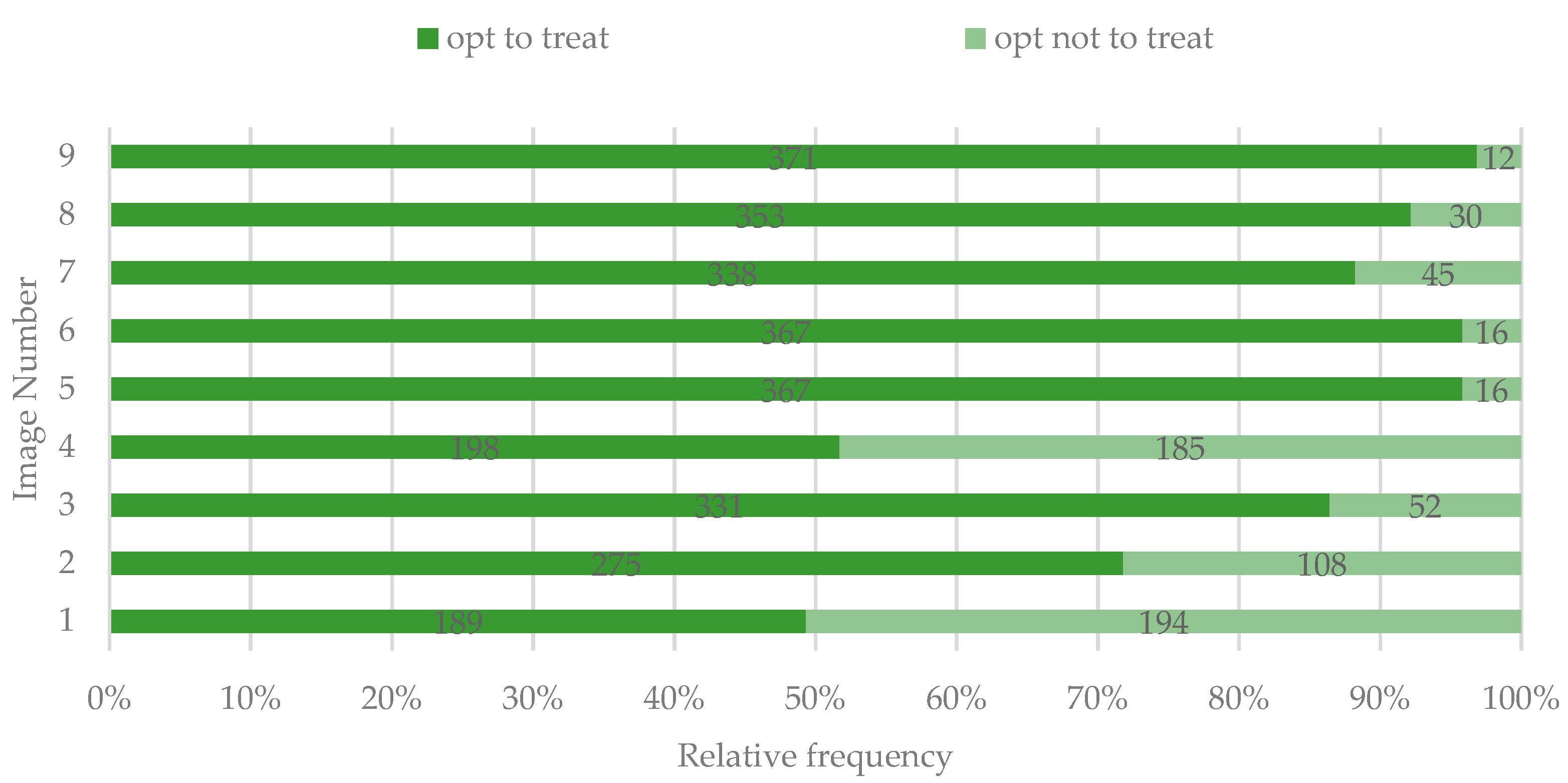
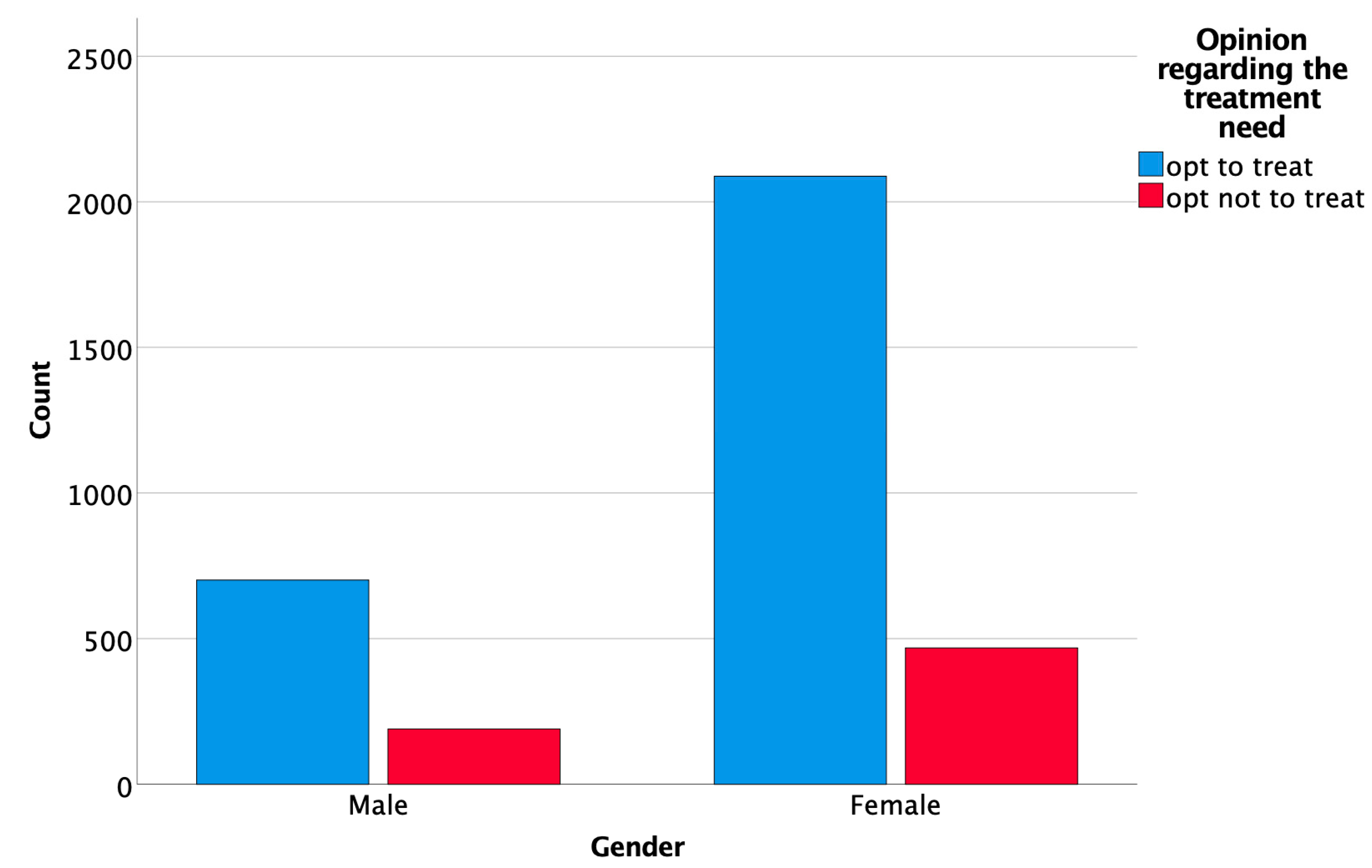
3.4. Opinion Regarding the Treatment Need for the Dyschromic Areas
4. Discussion
5. Conclusions
- Perception of DLs is influenced by the number of affected teeth, the severity of the lesion, and their contrast with the surrounding dental surface; however, the color of the lesions did not seem to play a significant role in the esthetic perception.
- The opinion regarding the need for treatment of DLs correlated significantly with the overall perception of the DLs.
- Gender and medical background significantly influenced the overall perception of DLs.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Browne, D.; Whelton, H.; O’Mullane, D.; Tavener, J.; Flannery, E. The aesthetic impact of enamel fluorosis on Irish adolescents. Community Dent. Oral Epidemiol. 2011, 39, 127–136. [Google Scholar] [CrossRef]
- Muth, J.; Cash, T. Body images attitudes: What difference does gender make? J. Appl. Soc. Psychol. 1997, 27, 1438–1452. [Google Scholar] [CrossRef]
- Goldstein, R.E.; Chu, S.J.; Lee, E.A.; Stappert, C.F.J.; Ronald, E. Goldstein’s Esthetics in Dentistry, 3rd ed.; Wiley-Blackwell: Hoboken, NJ, USA, 2018; p. 1576. [Google Scholar]
- Dudea, D.; Lasserre, J.F.; Alb, C.; Culic, B.; Pop Ciutrila, I.S.; Colosi, H. Patients’ perspective on dental aesthetics in a South-Eastern European community. J. Dent. 2012, 40, e72–e81. [Google Scholar] [CrossRef] [PubMed]
- Greta, D.C.; Colosi, H.A.; Gasparik, C.; Dudea, D. Perceptions of Dental Dyschromia by Patients and Dentist. Int. J. Prosthodont. 2021, 34, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Daneshvar, M.; Devji, T.F.; Davis, A.B.; White, M.A. Oral health related quality of life: A novel metric targeted to young adults. J. Public Health Dent. 2015, 75, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Samorodnitzky-Naveh, G.R.; Geiger, S.B.; Levin, L. Patients’ satisfaction with dental esthetics. J. Am. Dent. Assoc. 2007, 138, 805–808. [Google Scholar] [CrossRef]
- Machiulskiene, V.; Campus, G.; Carvalho, J.C.; Dige, I.; Ekstrand, K.R.; Jablonski-Momeni, A.; Maltz, M.; Manton, D.J.; Martignon, S.; Martinez-Mier, E.A.; et al. Terminology of Dental Caries and Dental Caries Management: Consensus Report of a Workshop Organized by ORCA and Cariology Research Group of IADR. Caries Res. 2020, 54, 7–14. [Google Scholar] [CrossRef]
- Sampson, V.; Sampson, A. Diagnosis and treatment options for anterior white spot lesions. Br. Dent. J. 2020, 229, 348–352. [Google Scholar] [CrossRef]
- Ellwood, R.P.; O’Mullane, D. Enamel opacities and dental esthetics. J. Public Health Dent. 1995, 55, 171–176. [Google Scholar] [CrossRef]
- McKnight, C.B.; Levy, S.M.; Cooper, S.E.; Jakobsen, J.R.; Warren, J.J. A pilot study of dental students’ esthetic perceptions of computer-generated mild dental fluorosis compared to other conditions. J. Public Health Dent. 1999, 59, 18–23. [Google Scholar] [CrossRef]
- Wondwossen, F.; Astrøm, A.N.; Bårdsen, A.; Bjorvatn, K. Perception of dental fluorosis amongst Ethiopian children and their mothers. Acta Odontol. Scand. 2003, 61, 81–86. [Google Scholar] [CrossRef]
- Chankanka, O.; Levy, S.M.; Warren, J.J.; Chalmers, J.M. A literature review of aesthetic perceptions of dental fluorosis and relationships with psychosocial aspects/oral health-related quality of life. Community Dent. Oral Epidemiol. 2010, 38, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.G.; Nalweyiso, N.; Busingye, J.; Whitworth, J. Subjective impacts of dental caries and fluorosis in rural Ugandan children. Community Dent. Health 2005, 22, 231–236. [Google Scholar] [PubMed]
- de Amorim Lde, F.; Estrela, C.; da Costa, L.R. Effects of traumatic dental injuries to primary teeth on permanent teeth--a clinical follow-up study. Dent. Traumatol. 2011, 27, 117–121. [Google Scholar] [CrossRef]
- Freitas Fernandes, L.H.; Laureano, I.C.C.; Farias, L.; Andrade, N.M.; Soares Forte, F.D.; Barros Alencar, C.R.; Cavalcanti, A.L. Incisor Molar Hypomineralization and Quality of Life: A Population-Based Study with Brazilian Schoolchildren. Int. J. Dent. 2021, 2021, 6655771. [Google Scholar] [CrossRef] [PubMed]
- Hasmun, N.; Lawson, J.; Vettore, M.V.; Elcock, C.; Zaitoun, H.; Rodd, H. Change in Oral Health-Related Quality of Life Following Minimally Invasive Aesthetic Treatment for Children with Molar Incisor Hypomineralisation: A Prospective Study. Dent. J. 2018, 6, 61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Julien, K.C.; Buschang, P.H.; Campbell, P.M. Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod. 2013, 83, 641–647. [Google Scholar] [CrossRef] [PubMed]
- Sundararaj, D.; Venkatachalapathy, S.; Tandon, A.; Pereira, A. Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: A meta-analysis. J. Int. Soc. Prev. Community Dent. 2015, 5, 433–439. [Google Scholar] [CrossRef] [Green Version]
- McGrady, M.G.; Ellwood, R.P.; Goodwin, M.; Boothman, N.; Pretty, I.A. Adolescents’ perceptions of the aesthetic impact of dental fluorosis vs. other dental conditions in areas with and without water fluoridation. BMC Oral Health 2012, 12, 4. [Google Scholar] [CrossRef] [PubMed]
- Sigurjóns, H.; Cochran, J.A.; Ketley, C.E.; Holbrook, W.P.; Lennon, M.A.; O’Mullane, D.M. Parental perception of fluorosis among 8-year-old children living in three communities in Iceland, Ireland and England. Community Dent. Oral Epidemiol. 2004, 32, 34–38. [Google Scholar] [CrossRef]
- Kavand, G.; Broffitt, B.; Levy, S.M.; Warren, J.J. Comparison of dental esthetic perceptions of young adolescents and their parents. J. Public Health Dent. 2012, 72, 164–171. [Google Scholar] [CrossRef] [Green Version]
- Silva, F.; Magno, M.B.; Neves, A.B.; Coqueiro, R.D.S.; Costa, M.C.; Maia, L.C.; Pithon, M.M. Aesthetic perceptions and social judgments about different enamel opacities. Braz. Oral Res. 2020, 34, e049. [Google Scholar] [CrossRef]
- Hawley, G.M.; Ellwood, R.P.; Davies, R.M. Dental caries, fluorosis and the cosmetic implications of different TF scores in 14-year-old adolescents. Community Dent. Health 1996, 13, 189–192. [Google Scholar] [PubMed]
- Edwards, M.; Macpherson, L.M.; Simmons, D.R.; Harper Gilmour, W.; Stephen, K.W. An assessment of teenagers’ perceptions of dental fluorosis using digital simulation and web-based testing. Community Dent. Oral Epidemiol. 2005, 33, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.M.; Chestnutt, I.G.; Bennett, P.D.; Hood, K.; Lowe, R. Characteristics attributed to individuals with dental fluorosis. Community Dent. Health 2006, 23, 209–216. [Google Scholar]
- Cochrane, S.M.; Cunningham, S.J.; Hunt, N.P. A comparison of the perception of facial profile by the general public and 3 groups of clinicians. Int. J. Adult Orthod. Orthognath. Surg. 1999, 14, 291–295. [Google Scholar]
- Wong, H.M.; McGrath, C.; King, N.M. Dental practitioners’ views on the need to treat developmental defects of enamel. Community Dent. Oral Epidemiol. 2007, 35, 130–139. [Google Scholar] [CrossRef]
- Haddad, H.J.; Jakstat, H.A.; Arnetzl, G.; Borbely, J.; Vichi, A.; Dumfahrt, H.; Renault, P.; Corcodel, N.; Pohlen, B.; Marada, G.; et al. Does gender and experience influence shade matching quality? J. Dent. 2009, 37, e40–e44. [Google Scholar] [CrossRef]
- Gasparik, C.; Grecu, A.G.; Culic, B.; Badea, M.E.; Dudea, D. Shade-matching performance using a new light-correcting device. J. Esthet. Restor. Dent. 2015, 27, 285–292. [Google Scholar] [CrossRef]
- Pecho, O.E.; Ghinea, R.; Perez, M.M.; Della Bona, A. Influence of Gender on Visual Shade Matching in Dentistry. J. Esthet. Restor. Dent. 2017, 29, e15–e23. [Google Scholar] [CrossRef] [PubMed]
| Age | |||||||
|---|---|---|---|---|---|---|---|
| <20y | 20–29y | 30–39 | 40–49y | 50–59y | >60y | ||
| 20.37% (n = 78) | 63.19% (n = 242) | 7.83% (n = 30) | 6.79% (n = 26) | 1.04% (n = 4) | 0.78% (n = 3) | ||
| Gender | Area of origin | Nationality | |||||
| Males | Females | Urban | Rural | Romanian | Other | ||
| 25.85% (n = 99) | 74.15% (n = 284) | 78.59% (n = 301) | 21.41% (n = 82) | 79.63% (n = 305) | 20.36% (n = 78) | ||
| Education | |||||||
| Middle school | High school | College/University | Doctoral/Masters’ degree | ||||
| 1.57% (n = 6) | 66.58% (n = 255) | 25.33% (n = 97) | 6.52% (n = 25) | ||||
| Profession | |||||||
| Non-professionals | Dentists | ||||||
| 77.55% (n = 297) | 22.45% (n = 86) | ||||||
| Dental students | Patients | General dentists | Prostho-dontists | Ortho-dontists | Endo-dontists | Oral surgeons | Perio-dontists |
| 36.81% (n = 141) | 40.74% (n = 156) | 11.63% (n = 10) | 47.67% (n = 41) | 20.93% (n = 18) | 11.63% (n = 10) | 4.65% (n = 4) | 3.49% (n = 3) |
| Imperceptible | Low Perceptibility | Perceptible But Not Bothersome | Perceptible and Bothersome | Very Bothersome | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Low Contrast | High Contrast | Low Contrast | High Contrast | Low Contrast | High Contrast | Low Contrast | High Contrast | Low Contrast | High Contrast | Sign. | |
| Image 1 | 35 | 8 | 157 | 22 | 81 | 41 | 14 | 25 | 0 | 0 | χ2(3, N = 383) = 52.889, p = 0.000; τb = 0.296, p = 0.000 |
| Image 2 | 5 | 3 | 33 | 69 | 28 | 113 | 16 | 116 | 0 | 0 | χ2(3, N = 383) = 22.257, p = 0.000; τb = 0.207, p = 0.000 |
| Image 3 | 4 | 3 | 12 | 21 | 14 | 58 | 7 | 217 | 3 | 44 | χ2(4, N = 383) = 59.919, p = 0.000; τb = 0.297, p = 0.000 |
| Image 4 | 10 | 5 | 64 | 56 | 65 | 98 | 15 | 63 | 4 | 3 | χ2(4, N = 383) = 27.689, p = 0.000; τb = 0.225, p = 0.000 |
| Image 5 | 0 | 2 | 3 | 4 | 14 | 8 | 37 | 85 | 46 | 184 | χ2(4, N = 383) = 23.359, p = 0.000; τb = 0.187, p = 0.000 |
| Image 6 | 1 | 1 | 13 | 14 | 12 | 10 | 45 | 86 | 46 | 155 | χ2(4, N = 383) = 16.726, p = 0.002; τb = 0.188, p = 0.000 |
| Image 7 | 2 | 2 | 19 | 15 | 17 | 51 | 24 | 174 | 11 | 68 | χ2(4, N = 383) = 41.450, p = 0.000; τb = 0.222, p = 0.000 |
| Image 8 | 2 | 1 | 15 | 7 | 25 | 17 | 51 | 67 | 66 | 132 | χ2(4, N = 383) = 18.435, p = 0.001; τb = 0.194, p = 0.000 |
| Image 9 | 2 | 2 | 0 | 6 | 1 | 7 | 11 | 115 | 10 | 229 | χ2(4, N = 383) = 17.022, p = 0.002; τb = 0.118, p = 0.040 |
| Imperceptible | Low Perceptibility | Perceptible But Not Bothersome | Perceptible and Bothersome | Very Bothersome | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| To Treat | Not to Treat | To Treat | Not to Treat | To Treat | Not to Treat | To Treat | Not to Treat | To Treat | Not to Treat | Sign. | |
| Image 1 | 12 | 31 | 78 | 101 | 65 | 57 | 34 | 5 | 0 | 0 | χ2(3, N = 383) = 33.380, p = 0.000; τb = −0.245, p = 0.000 |
| Image 2 | 4 | 4 | 63 | 39 | 94 | 47 | 114 | 18 | 0 | 0 | χ2(3, N = 383) = 22.614, p = 0.000; τb = −0.218, p = 0.000 |
| Image 3 | 4 | 3 | 22 | 11 | 54 | 18 | 206 | 18 | 45 | 2 | χ2(4, N = 383) = 33.441, p = 0.000; τb = −0.259, p = 0.000 |
| Image 4 | 7 | 8 | 41 | 79 | 83 | 80 | 61 | 17 | 6 | 2 | χ2(4, N = 383) = 40.152, p = 0.000; τb = −0.282, p = 0.000 |
| Image 5 | 1 | 1 | 6 | 1 | 16 | 6 | 118 | 4 | 226 | 4 | χ2(4, N = 383) = 42.254, p = 0.000; τb = −0.1987, p = 0.005 |
| Image 6 | 1 | 1 | 23 | 4 | 18 | 4 | 127 | 4 | 198 | 3 | χ2(4, N = 383) = 32.934, p = 0.000; τb = −0.190, p = 0.003 |
| Image 7 | 1 | 3 | 25 | 9 | 50 | 18 | 186 | 12 | 76 | 3 | χ2(4, N = 383) = 7.749, p = 0.000; τb = −0.270, p = 0.000 |
| Image 8 | 3 | 0 | 14 | 8 | 31 | 11 | 111 | 7 | 194 | 4 | χ2(4, N = 383) = 54.523, p = 0.000; τb = −0.283, p = 0.000 |
| Image 9 | 4 | 0 | 5 | 1 | 7 | 1 | 121 | 5 | 234 | 5 | χ2(4, N = 383) = 7.206, p = 0.125; τb = −0.0878, p = 0.146 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasparik, C.; Colosi, H.A.; Varvara, B.E.; Grecu, A.G.; Aghiorghiesei, A.I.; Mesaroș, A.Ș.; Mazilu, A.; Dudea, D. Factors Involved in the Perception of Enamel Dyschromic Lesions—A Questionnaire-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 900. https://doi.org/10.3390/ijerph19020900
Gasparik C, Colosi HA, Varvara BE, Grecu AG, Aghiorghiesei AI, Mesaroș AȘ, Mazilu A, Dudea D. Factors Involved in the Perception of Enamel Dyschromic Lesions—A Questionnaire-Based Study. International Journal of Environmental Research and Public Health. 2022; 19(2):900. https://doi.org/10.3390/ijerph19020900
Chicago/Turabian StyleGasparik, Cristina, Horațiu Alexandru Colosi, Bianca Elena Varvara, Alexandru Grațian Grecu, Alexandra Iulia Aghiorghiesei, Anca Ștefania Mesaroș, Amalia Mazilu (Moldovan), and Diana Dudea. 2022. "Factors Involved in the Perception of Enamel Dyschromic Lesions—A Questionnaire-Based Study" International Journal of Environmental Research and Public Health 19, no. 2: 900. https://doi.org/10.3390/ijerph19020900
APA StyleGasparik, C., Colosi, H. A., Varvara, B. E., Grecu, A. G., Aghiorghiesei, A. I., Mesaroș, A. Ș., Mazilu, A., & Dudea, D. (2022). Factors Involved in the Perception of Enamel Dyschromic Lesions—A Questionnaire-Based Study. International Journal of Environmental Research and Public Health, 19(2), 900. https://doi.org/10.3390/ijerph19020900









