A Randomized Clinical Trial to Assess the Efficacy of Online-Treatment with Trial-Based Cognitive Therapy, Mindfulness-Based Health Promotion and Positive Psychotherapy for Post-Traumatic Stress Disorder during the COVID-19 Pandemic: A Study Protocol
Abstract
1. Introduction
2. Materials and Methods
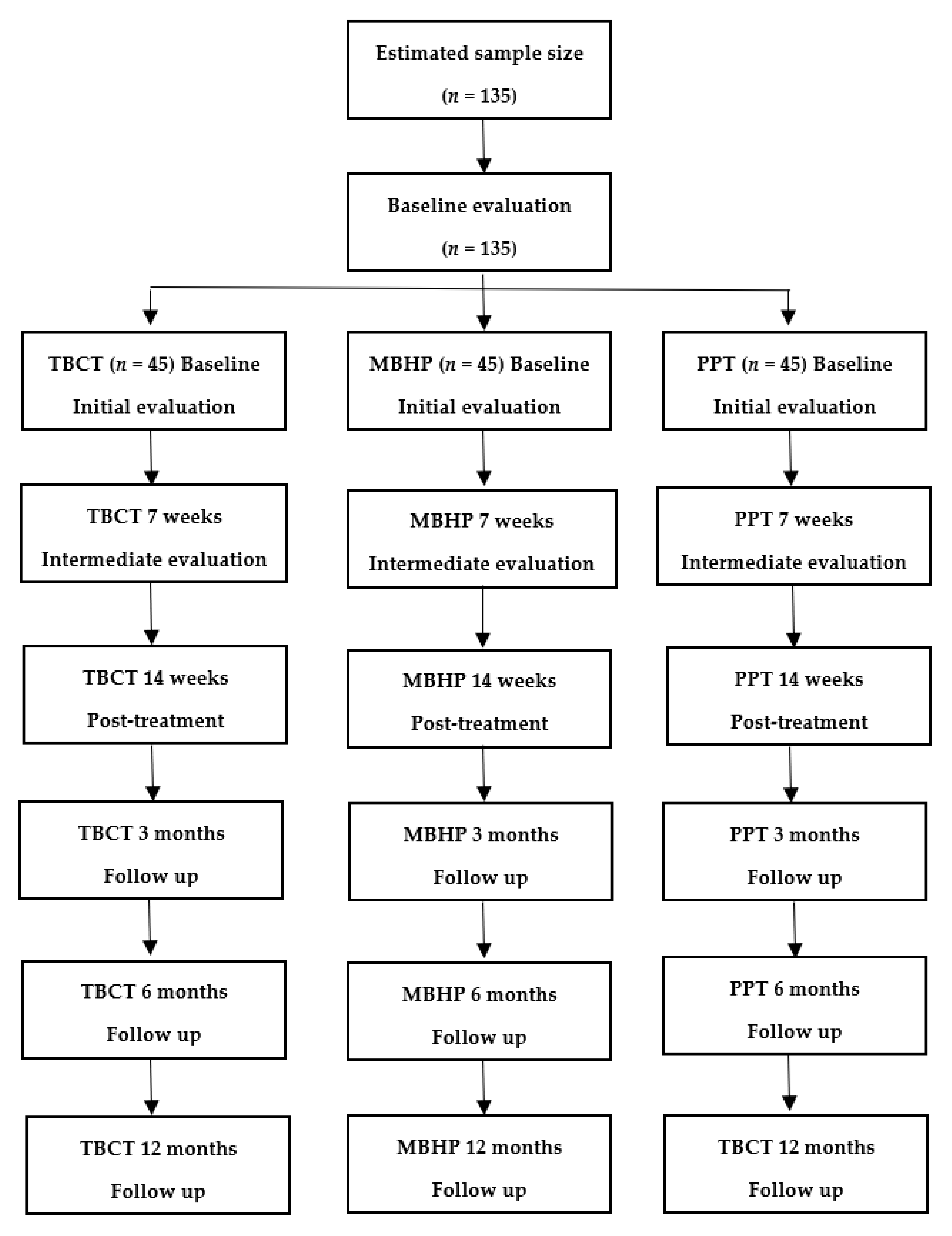
2.1. Study Design
2.2. Hypotheses
2.3. Participants
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Study Settings
2.7. Interventions
- Trial-based cognitive therapy
- Mindfulness-based health promotion
- Positive psychotherapy
2.8. Outcomes
2.9. Instruments
- Diagnostic assessment
- Primary outcome
- Secondary outcome
- Mediator variables
2.10. Sample Size
2.11. Randomization and Sequence Generation
2.12. Implementation
2.13. Randomization and Concealment
2.14. Interventions Similarities and Differences
2.15. Statistical Methods
2.16. Ethical Aspects
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Registration Number for Clinical Research
References
- American Psychiatric Association. DSM-5: Manual Diagnóstico e Estatístico DE Transtornos Mentais; American Psychiatric Association: Porto Alegre, Brazil, 2014. [Google Scholar]
- Kessler, R.C.; Aguilar-Gaxiola, S.; Alonso, J.; Benjet, C.; Bromet, E.J.; Cardoso, G.; Degenhardt, L.; de Girolamo, G.; Dinolova, R.V.; Ferry, F. Trauma and PTSD in the WHO world mental health surveys. Eur. J. Psychotraumatol. 2017, 8, 1353383. [Google Scholar] [CrossRef]
- Zohar, J.; Juven-Wetzler, A.; Sonnino, R.; Cwikel-Hamzany, S.; Balaban, E.; Cohen, H. New insights into secondary prevention in post-traumatic stress disorder. Dialogues Clin. Neurosci. 2011, 13, 301. [Google Scholar]
- Smith, S.M.; Goldstein, R.B.; Grant, B.F. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J. Psychiatr. Res. 2016, 82, 16–22. [Google Scholar] [CrossRef]
- Mealer, M.; Burnham, E.L.; Goode, C.J.; Rothbaum, B.; Moss, M. The prevalence and impact of post traumatic stress disorder and burnout syndrome in nurses. Depress. Anxiety 2009, 26, 1118–1126. [Google Scholar] [CrossRef] [PubMed]
- DeLucia, J.A.; Bitter, C.; Fitzgerald, J.; Greenberg, M.; Dalwari, P.; Buchanan, P. Prevalence of post-traumatic stress disorder in emergency physicians in the United States. West. J. Emerg. Med. 2019, 20, 740. [Google Scholar] [CrossRef]
- Hosseininejad, S.M.; Jahanian, F.; Elyasi, F.; Mokhtari, H.; Koulaei, M.E.; Pashaei, S.M. The prevalence of post-traumatic stress disorder among emergency nurses: A cross sectional study in northern Iran. BioMedicine 2019, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Chen, J.-H.; Xu, Y.-F. Rethinking online mental health services in China during the COVID-19 epidemic. Asian J. Psychiatr. 2020, 50, 102015. [Google Scholar] [CrossRef] [PubMed]
- Ćosić, K.; Popović, S.; Šarlija, M.; Kesedžić, I. Impact of human disasters and COVID-19 pandemic on mental health: Potential of digital psychiatry. Psychiatr. Danub. 2020, 32, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Iyanda, A.E.; Adeleke, R.; Lu, Y.; Osayomi, T.; Adaralegbe, A.; Lasode, M.; Chima-Adaralegbe, N.J.; Osundina, A.M. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: A multiscale geographically weighted regression analysis (11 January–28 June 2020). J. Infect. Public Health 2020, 13, 1438–1445. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Kar, N. Cognitive behavioral therapy for the treatment of post-traumatic stress disorder: A review. Neuropsychiatr. Dis. Treat. 2011, 7, 167–181. [Google Scholar] [CrossRef]
- Resick, P.A.; Galovski, T.E.; Uhlmansiek, M.O.; Scher, C.D.; Clum, G.A.; Young-Xu, Y. A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. J. Consult. Clin. Psychol. 2008, 76, 243. [Google Scholar] [CrossRef] [PubMed]
- Rizvi, S.L.; Vogt, D.S.; Resick, P.A. Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behav. Res. Ther. 2009, 47, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Resick, P.A.; Monson, C.M.; Chard, K.M. Cognitive Processing Therapy for PTSD: A Comprehensive Manual; Guilford Publications: New York, NY, USA, 2016; ISBN 1462528643. [Google Scholar]
- Powers, M.B.; Halpern, J.M.; Ferenschak, M.P.; Gillihan, S.J.; Foa, E.B. A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clin. Psychol. Rev. 2010, 30, 635–641. [Google Scholar] [CrossRef]
- Zhou, Y.; Sun, L.; Wang, Y.; Wu, L.; Sun, Z.; Zhang, F.; Liu, W. Developments of prolonged exposure in treatment effect of post-traumatic stress disorder and controlling dropout rate: A meta-analytic review. Clin. Psychol. Psychother. 2020, 27, 449–462. [Google Scholar] [CrossRef]
- Foa, E.B.; Chrestman, K.R.; Gilboa-Schechtman, E. Prolonged Exposure Therapy for Adolescents with PTSD Emotional Processing of Traumatic Experiences, Therapist Guide; Oxford University Press: Oxford, UK, 2008; ISBN 0195331745. [Google Scholar]
- Duran, É.P.; Menezes, C.H.; Neto, F.L.; Savóia, M.G.; de Oliveira, I.R. Perfil de pacientes com diagnóstico de transtorno de estresse pós-traumático atendidos em um ambulatório de ansiedade e trauma. Rev. Ciênc. Méd. Biol. 2020, 19, 597–601. [Google Scholar] [CrossRef]
- Schottenbauer, M.A.; Glass, C.R.; Arnkoff, D.B.; Tendick, V.; Gray, S.H. Nonresponse and dropout rates in outcome studies on PTSD: Review and methodological considerations. Psychiatry Interpers. Biol. Process. 2008, 71, 134–168. [Google Scholar] [CrossRef] [PubMed]
- Goetter, E.M.; Bui, E.; Ojserkis, R.A.; Zakarian, R.J.; Brendel, R.W.; Simon, N.M. A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. J. Trauma. Stress 2015, 28, 401–409. [Google Scholar] [CrossRef] [PubMed]
- Berke, D.S.; Yeterian, J.; Presseau, C.; Rusowicz-Orazem, L.; Kline, N.K.; Nash, W.P.; Litz, B.T. Dynamic changes in marines’ reports of PTSD symptoms and problem alcohol use across the deployment cycle. Psychol. Addict. Behav. 2019, 33, 162. [Google Scholar] [CrossRef]
- Schnyder, U. Why new psychotherapies for posttraumatic stress disorder? Psychother. Psychosom. 2005, 74, 199–201. [Google Scholar] [CrossRef]
- Butollo, W.; Karl, R.; König, J.; Rosner, R. A randomized controlled clinical trial of dialogical exposure therapy versus cognitive processing therapy for adult outpatients suffering from PTSD after type I trauma in adulthood. Psychother. Psychosom. 2016, 85, 16–26. [Google Scholar] [CrossRef] [PubMed]
- Duran, É.P.; Corchs, F.; Vianna, A.; Araújo, Á.C.; Del Real, N.; Silva, C.; Ferreira, A.P.; De Vitto Francez, P.; Godói, C.; Silveira, H.; et al. A randomized clinical trial to assess the efficacy of trial-based cognitive therapy (TBCT) compared to prolonged exposure for post-traumatic stress disorder: Preliminary findings. CNS Spectr. 2021, 26, 427–434. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, I.R. de Trial-Based Thought Record (TBTR): Preliminary data on a strategy to deal with core beliefs by combining sentence reversion and the use of analogy with a judicial process. Rev. Bras. Psiquiatr. 2008, 30, 12–18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De Oliveira, I.R. Trial-Based Cognitive Therapy: A Manual for Clinicians; Routledge: Londond, UK, 2014; ISBN 1317625544. [Google Scholar]
- De Oliveira, I.R. Trial-Based Cognitive Therapy: Distinctive Features; Routledge: London, UK, 2016; ISBN 1317532651. [Google Scholar]
- Wenzel, A. Innovations in Cognitive Behavioral Therapy: Strategic Interventions for Creative Practice; Routledge: London, UK, 2017; ISBN 1317674154. [Google Scholar]
- Hemanny, C.; Carvalho, C.; Maia, N.; Reis, D.; Botelho, A.C.; Bonavides, D.; Seixas, C.; De Oliveira, I.R. Efficacy of trial-based cognitive therapy, behavioral activation and treatment as usual in the treatment of major depressive disorder: Preliminary findings from a randomized clinical trial. CNS Spectr. 2020, 25, 535–544. [Google Scholar] [CrossRef]
- Powell, V.B.; de Oliveira, O.H.; Seixas, C.; Almeida, C.; Grangeon, M.C.; Caldas, M.; Bonfim, T.D.; Castro, M.; Galvao-de Almeida, A.; de Moraes, R.O.; et al. Changing core beliefs with trial-based cognitive therapy may improve quality of life in social phobia: A randomized study. Rev. Bras. Psiquiatr. 2013, 35, 243–247. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Neufeld, C.B.; Palma, P.C.; Caetano, K.A.S.; Brust-Renck, P.G.; Curtiss, J.; Hofmann, S.G. A randomized clinical trial of group and individual cognitive-behavioral therapy approaches for social anxiety disorder. Int. J. Clin. Health Psychol. 2020, 20, 29–37. [Google Scholar] [CrossRef]
- Caetano, K.A.S.; Depreeuw, B.; Papenfuss, I.; Curtiss, J.; Langwerden, R.J.; Hofmann, S.G.; Neufeld, C.B. Trial-Based Cognitive Therapy: Efficacy of a New CBT Approach for Treating Social Anxiety Disorder with Comorbid Depression. Int. J. Cogn. Ther. 2018, 11, 325–342. [Google Scholar] [CrossRef]
- De Oliveira, I.R.; Powell, V.B.; Wenzel, A.; Caldas, M.; Seixas, C.; Almeida, C.; Bonfim, T.; Grangeon, M.C.; Castro, M.; Galvao, A.; et al. Efficacy of the trial-based thought record, a new cognitive therapy strategy designed to change core beliefs, in social phobia. J. Clin. Pharm. Ther. 2012, 37, 328–334. [Google Scholar] [CrossRef]
- Delavechia, T.R.; Velasquez, M.L.; Duran, É.P.; Matsumoto, L.S.; Oliveira, I.R. de Changing negative core beliefs with trial-based thought record. Arch. Clin. Psychiatry 2016, 43, 31–33. [Google Scholar] [CrossRef]
- Trombka, M.; Demarzo, M.; Bacas, D.C.; Antonio, S.B.; Cicuto, K.; Salvo, V.; Claudino, F.C.A.; Ribeiro, L.; Christopher, M.; Garcia-Campayo, J. Study protocol of a multicenter randomized controlled trial of mindfulness training to reduce burnout and promote quality of life in police officers: The POLICE study. BMC Psychiatry 2018, 18, 151. [Google Scholar] [CrossRef]
- Lopes, S.A.; Vannucchi, B.P.; Demarzo, M.; Cunha, Â.G.J.; de Nunes, M.P.T. Effectiveness of a mindfulness-based intervention in the management of musculoskeletal pain in nursing workers. Pain Manag. Nurs. 2019, 20, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Salvo, V.; Kristeller, J.; Marin, J.M.; Sanudo, A.; Lourenço, B.H.; Schveitzer, M.C.; D’Almeida, V.; Morillo, H.; Gimeno, S.G.A.; Garcia-Campayo, J. Mindfulness as a complementary intervention in the treatment of overweight and obesity in primary health care: Study protocol for a randomised controlled trial. Trials 2018, 19, 1–14. [Google Scholar] [CrossRef]
- Seligman, M.E.P.; Steen, T.A.; Park, N.; Peterson, C. Positive psychology progress: Empirical validation of interventions. Am. Psychol. 2005, 60, 410. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M. Flourish: Positive psychology and positive interventions. In Tanner Lectures in Human Values; Cambridge University Press: Cambridge, UK, 2009; Volume 31, pp. 1–56. [Google Scholar]
- Seligman, M.; Csikszentmihalyi, M. Positive psychology: An introduction American psychologist. Am. Psychol. 2001, 56, 89–90. [Google Scholar] [CrossRef]
- Ryff, C.D. Psychological well-being revisited: Advances in the science and practice of eudaimonia. Psychother. Psychosom. 2014, 83, 10–28. [Google Scholar] [CrossRef] [PubMed]
- Mongrain, M.; Anselmo-Matthews, T. Do positive psychology exercises work? A replication of Seligman et al. (†). J. Clin. Psychol. 2012, 68, 382–389. [Google Scholar] [CrossRef]
- Rashid, T.; Seligman, M. Psicoterapia Positiva: Manual do Terapeuta; Artmed Editora: Porto Alegre, RS, Brazil, 2019; ISBN 8582715501. [Google Scholar]
- Riches, S.; Schrank, B.; Rashid, T.; Slade, M. WELLFOCUS PPT: Modifying positive psychotherapy for psychosis. Psychotherapy 2016, 53, 68. [Google Scholar] [CrossRef]
- Chan, A.-W.; Tetzlaff, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 346, e7586. [Google Scholar] [CrossRef] [PubMed]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- Osorio, F.L.; Silva, T.D.A.D.A.; Santos, R.G.D.O.S.; Chagas, M.H.N.; Chagas, N.M.S.; Sanches, R.F.; Crippa, J.A.D.E.S. Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Transcultural adaptation of the Brazilian version. Arch. Clin. Psychiatry 2017, 44, 10–19. [Google Scholar] [CrossRef][Green Version]
- Pereira-Lima, K.; Loureiro, S.R.; Bolsoni, L.M.; Apolinario da Silva, T.D.; Osório, F.L. Psychometric properties and diagnostic utility of a Brazilian version of the PCL-5 (complete and abbreviated versions). Eur. J. Psychotraumatol. 2019, 10, 1581020. [Google Scholar] [CrossRef]
- De Oliveira, I.R. Trial-Based Cognitive Therapy; Routledge: London, UK, 2016; ISBN 9781315725000. [Google Scholar]
- De Oliveira, I.R.; Seixas, C.; Osorio, F.L.; Crippa, J.A.S.; de Abreu, J.N.; Menezes, I.G.; Pidgeon, A.; Sudak, D.; Wenzel, A. Evaluation of the Psychometric Properties of the Cognitive Distortions Questionnaire (CD-Quest) in a Sample of Undergraduate Students. Innov. Clin. Neurosci. 2015, 12, 20–27. [Google Scholar]
- Osmo, F.; Duran, V.; Wenzel, A.; de Oliveira, I.R.; Nepomuceno, S.; Madeira, M.; Menezes, I. The Negative Core Beliefs Inventory: Development and Psychometric Properties. J. Cogn. Psychother. 2018, 32, 67–84. [Google Scholar] [CrossRef]
- Kafka, F. Der Process: Roman (1925); BWV Verlag: Berlin, Germany, 2006; Volume 25, ISBN 3830511779. [Google Scholar]
- De Oliveira, I.R. Kafka’s trial dilemma: Proposal of a practical solution to Joseph, K.’s unknown accusation. Med. Hypotheses 2011, 77, 5–6. [Google Scholar] [CrossRef] [PubMed]
- Perls, F. The Gestalt Approach & Eye Witness to Therapy.; Science & Behavior Books: Mountain View, CA, USA, 1973; ISBN 083140034X. [Google Scholar]
- Greenberg, L.S. Resolving splits: Use of the two chair technique. Psychother. Theory Res. Pract. 1979, 16, 316. [Google Scholar] [CrossRef]
- De Oliveira, I.R.; Hemmany, C.; Powell, V.B.; Bonfim, T.D.; Duran, E.P.; Novais, N.; Velasquez, M.; Di Sarno, E.; Alves, G.L.; Cesnik, J.A. Trial-based psychotherapy and the efficacy of trial-based thought record in changing unhelpful core beliefs and reducing self-criticism. CNS Spectr. 2012, 17, 16–23. [Google Scholar] [CrossRef] [PubMed]
- De Roos, C.; van der Oord, S.; Zijlstra, B.; Lucassen, S.; Perrin, S.; Emmelkamp, P.; De Jongh, A.D. Comparison of eye movement desensitization and reprocessing therapy, cognitive behavioral writing therapy, and wait-list in pediatric posttraumatic stress disorder following single-incident trauma: A multicenter randomized clinical trial. J. Child Psychol. Psychiatry 2017, 58, 1219–1228. [Google Scholar] [CrossRef]
- Nascimento, J.C.P.; dos Santos, K.V.G.; dos Dantas, J.K.S.; Dantas, D.V.; Dantas, R.A.N. Non-pharmacological therapies for the treatment of post-traumatic stress disorder among emergency responders: A scoping review. Rev. Esc. Enferm. USP 2021, 55, e03724. [Google Scholar] [CrossRef] [PubMed]
- Lee Duckworth, A.; Steen, T.A.; Seligman, M.E.P. Positive psychology in clinical practice. Annu. Rev. Clin. Psychol. 2005, 1, 629–651. [Google Scholar] [CrossRef] [PubMed]
- Seligman, M.E.P. Florescer: Uma Nova Compreensão Sobre a Natureza da Felicidade E do Bem-Estar; Objectiva: Rio de Janeiro, Brazil, 2012. [Google Scholar]
- Habib, A.; Stevelink, S.A.M.; Greenberg, N.; Williamson, V. Post-traumatic growth in (ex-) military personnel: Review and qualitative synthesis. Occup. Med. 2018, 68, 617–625. [Google Scholar] [CrossRef]
- First, M.B.; Williams, J.B.; Karg, R.S.; Spitzer, R.L. Entrevista Clínica Estruturada Para os Transtornos do DSM-5: SCID-5-CV Versão Clínica; Artmed Editora: Porto Alegre, RS, Brazil, 2017; ISBN 8582714270. [Google Scholar]
- Oliveira-Watanabe, T.T.; Ramos-Lima, L.F.; Santos, R.C.; Mello, M.F.; Mello, A.F. The clinician-administered PTSD Scale (CAPS-5): Adaptation to brazilian portuguese. Rev. Bras. Psiquiatr. 2019, 41, 92. [Google Scholar] [CrossRef] [PubMed]
- Djukanovic, I.; Carlsson, J.; Årestedt, K. Is the Hospital Anxiety and Depression Scale (HADS) a valid measure in a general population 65–80 years old? A psychometric evaluation study. Health Qual. Life Outcomes 2017, 15, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383. [Google Scholar] [CrossRef]
- Faro, A. Análise fatorial confirmatória e normatização da Hospital Anxiety and Depression Scale (HADS). Psicol. Teor. Pesqui. 2015, 31, 349–353. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Topp, C.W.; Østergaard, S.D.; Søndergaard, S.; Bech, P. The WHO-5 Well-Being Index: A systematic review of the literature. Psychother. Psychosom. 2015, 84, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Dadfar, M.; Momeni Safarabad, N.; Asgharnejad Farid, A.A.; Nemati Shirzy, M.; Ghazie pour Abarghouie, F. Reliability, validity, and factorial structure of the World Health Organization-5 Well-Being Index (WHO-5) in Iranian psychiatric outpatients. Trends Psychiatry Psychother. 2018, 40, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo Vicario, M.H.; Rodríguez Hernández, P.R. DSM-5. Manual Diagnóstico y Estadístico de los Trastornos Mentales. Últimas Novedades; American Psychiatric Association: Washington, DC, USA, 2013; Volume 17, ISBN 9780890425541. [Google Scholar]
- Kubany, E.S.; Haynes, S.N.; Abueg, F.R.; Manke, F.P.; Brennan, J.M.; Stahura, C. Development and validation of the trauma-related guilt inventory (TRGI). Psychol. Assess. 1996, 8, 428. [Google Scholar] [CrossRef]
- Beck, J.S.; Tompkins, M. Cognitive Therapy; Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Marmar, C.R.; Weiss, D.S.; Gaston, L. Toward the validation of the California Therapeutic Alliance Rating System. Psychol. Assess. A J. Consult. Clin. Psychol. 1989, 1, 46. [Google Scholar] [CrossRef]
- Marcolino, J.A.M.; Iacoponi, E. The early impact of therapeutic alliance in brief psychodynamic psychotherapy. Brazilian J. Psychiatry 2003, 25, 78–86. [Google Scholar] [CrossRef][Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- IBM Corp. IBM SPSS Statistics for Windows; Version 24.0. 2016; IBM Corp: New York, NY, USA, 2016. [Google Scholar]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain. Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef]
- Liu, Q.; Luo, D.; Haase, J.E.; Guo, Q.; Wang, X.Q.; Liu, S.; Xia, L.; Liu, Z.; Yang, J.; Yang, B.X. The experiences of health-care providers during the COVID-19 crisis in China: A qualitative study. Lancet Glob. Health 2020, 8, e790–e798. [Google Scholar] [CrossRef]
- Galea, S.; Merchant, R.M.; Lurie, N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Intern. Med. 2020, 180, 817–818. [Google Scholar] [CrossRef] [PubMed]
- Bo, H.-X.; Li, W.; Yang, Y.; Wang, Y.; Zhang, Q.; Cheung, T.; Wu, X.; Xiang, Y.-T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2021, 51, 1052–1053. [Google Scholar] [CrossRef]
- Boyd, J.E.; Lanius, R.A.; McKinnon, M.C. Mindfulness-based treatments for posttraumatic stress disorder: A review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 2018, 43, 7–25. [Google Scholar] [CrossRef]
- Karatzias, T.; Chouliara, Z.; Power, K.; Brown, K.; Begum, M.; McGoldrick, T.; MacLean, R. Life satisfaction in people with post-traumatic stress disorder. J. Ment. Health 2013, 22, 501–508. [Google Scholar] [CrossRef]
| Study Period | |||||||
|---|---|---|---|---|---|---|---|
| Enrolment | Allocation | Post-Allocation | Follow-Up | ||||
| Timepoint | Screening | Baseline | 7 weeks | 14 weeks | 3 months | 6 months | 12 months |
| Enrolment: | |||||||
| Eligibility screen | X | ||||||
| Informed consent | X | ||||||
| Allocation | X | ||||||
| Interventions: | |||||||
| TBCT |  | ||||||
| MBHP |  | ||||||
| PPT |  | ||||||
| Assessments: | |||||||
| PCL-5 | X | ||||||
| SCID-5 | X | ||||||
| CAPS-5 | X | X | X | X | X | X | |
| HADS | X | X | X | X | X | X | |
| TRGI | X | X | X | X | X | X | |
| NCBI | X | X | X | X | X | X | |
| WHO-5 | X | X | X | X | X | X | |
| CALPAS-P | X | X | X | ||||
| SS interview | X | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duran, É.P.; Hemanny, C.; Vieira, R.; Nascimento, O.; Machado, L.; de Oliveira, I.R.; Demarzo, M. A Randomized Clinical Trial to Assess the Efficacy of Online-Treatment with Trial-Based Cognitive Therapy, Mindfulness-Based Health Promotion and Positive Psychotherapy for Post-Traumatic Stress Disorder during the COVID-19 Pandemic: A Study Protocol. Int. J. Environ. Res. Public Health 2022, 19, 819. https://doi.org/10.3390/ijerph19020819
Duran ÉP, Hemanny C, Vieira R, Nascimento O, Machado L, de Oliveira IR, Demarzo M. A Randomized Clinical Trial to Assess the Efficacy of Online-Treatment with Trial-Based Cognitive Therapy, Mindfulness-Based Health Promotion and Positive Psychotherapy for Post-Traumatic Stress Disorder during the COVID-19 Pandemic: A Study Protocol. International Journal of Environmental Research and Public Health. 2022; 19(2):819. https://doi.org/10.3390/ijerph19020819
Chicago/Turabian StyleDuran, Érica Panzani, Curt Hemanny, Renata Vieira, Orlando Nascimento, Leonardo Machado, Irismar Reis de Oliveira, and Marcelo Demarzo. 2022. "A Randomized Clinical Trial to Assess the Efficacy of Online-Treatment with Trial-Based Cognitive Therapy, Mindfulness-Based Health Promotion and Positive Psychotherapy for Post-Traumatic Stress Disorder during the COVID-19 Pandemic: A Study Protocol" International Journal of Environmental Research and Public Health 19, no. 2: 819. https://doi.org/10.3390/ijerph19020819
APA StyleDuran, É. P., Hemanny, C., Vieira, R., Nascimento, O., Machado, L., de Oliveira, I. R., & Demarzo, M. (2022). A Randomized Clinical Trial to Assess the Efficacy of Online-Treatment with Trial-Based Cognitive Therapy, Mindfulness-Based Health Promotion and Positive Psychotherapy for Post-Traumatic Stress Disorder during the COVID-19 Pandemic: A Study Protocol. International Journal of Environmental Research and Public Health, 19(2), 819. https://doi.org/10.3390/ijerph19020819







