Understanding the Experience of Service Users in an Integrated Care Programme for Obesity and Mental Health: A Qualitative Investigation of Total Wellbeing Luton
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Sample
2.3. Data Collection
2.4. Data Analysis
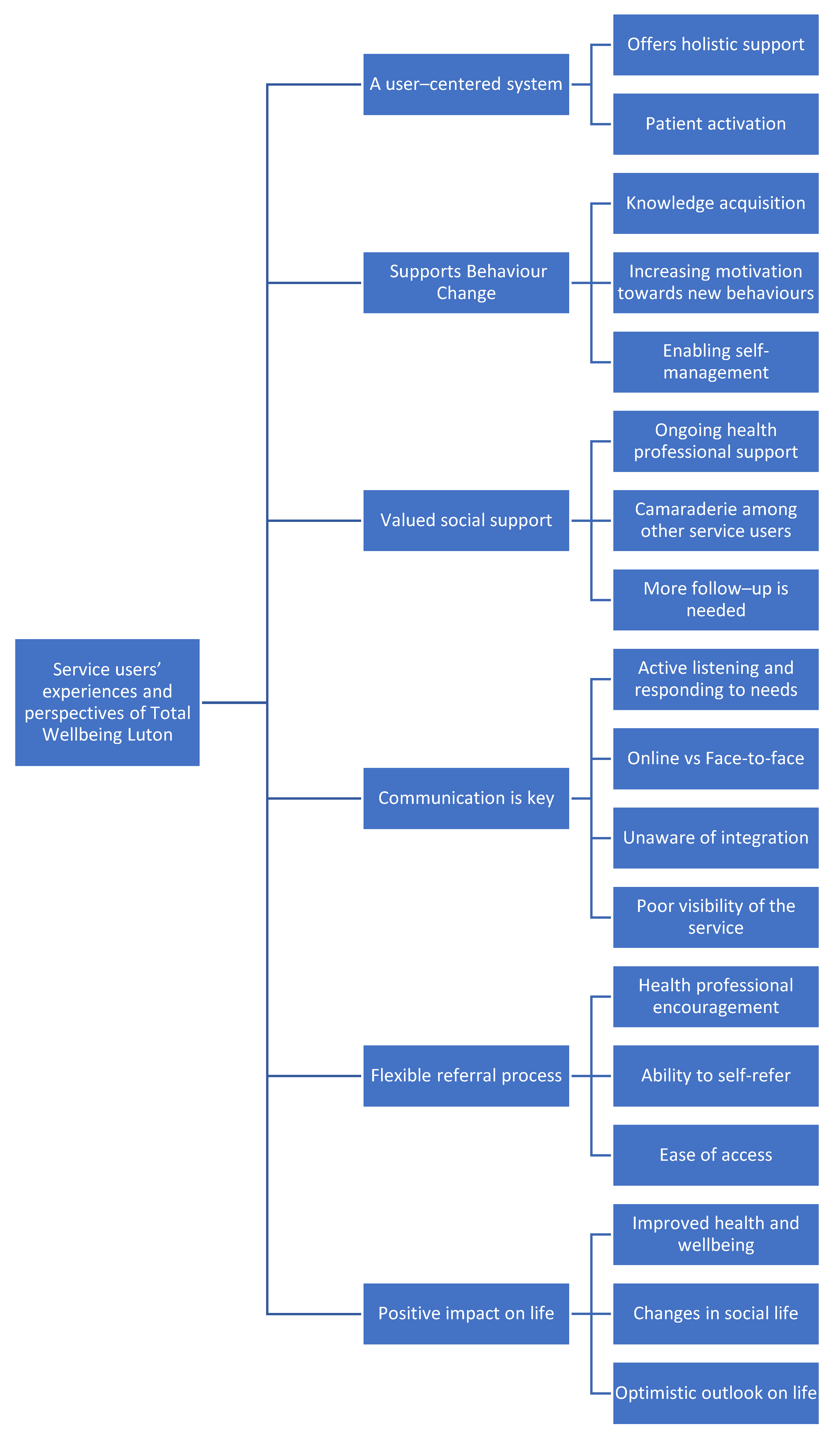
3. Results
3.1. Theme 1: A User-Centered System
3.1.1. Offers Holistic Support
“They are there for everybody, and a wide range of help and services are available. Particularly now when you know things, over the last year or so with COVID-19, uncertainties and mental health problems, either to make you feel as though you’re not alone”. (Service user 1)
“The GP referred me to weight management programme, and then they referred me to social prescription”. (Service user 6)
3.1.2. Patient Activation
“They gave us an opportunity to discuss and share ideas, back and forth with each other. And that was quite good really. They didn’t dominate the class and gave us an opportunity”. (Service user 5)
3.2. Theme 2: Supports Behaviour Change
3.2.1. Knowledge Acquisition
“I was really interested in reading food labels, I had health problems, I had to go into FOD map diet. They really help with that. I learned how to read the food labels” (Service user 14)
“And the handouts that I was given, I still use today”. (Service user 2)
3.2.2. Increasing Motivation towards New Behaviours
“If you’re doing it on your own, you have to have the motivation to do it. If you’ve got a class to go to, then, it’s in your schedule, and you will go. […] The physical benefit, but it’s also the social benefit as well, because there’s a good group of people there. […] I think because doing it in a group makes you go there. […] Monday morning, I go to a gym it’s a regular habit”. (Service user 13)
“I am more motivated. I wish, I could go to the gym because while I’m not doing that…. […] Last night was nine o’clock, I played some music and I was dancing like crazy and sweaty, because I go to work out, and there’s nowhere to go… I did some exercise. You know, I think it made me feel more… to want to move on”. (Service user 5)
3.2.3. Enabling Self-Management
“The therapist showed me different techniques, things like a journal. It’s called a worries diary, I read it every day, and if I ever have a stressful day I still go back to that. And so I still go back to all those still now”. (Service user 3)
“I am extremely happy with that service. […] I don’t feel I’m cured of it, but I certainly do feel more able to say, so much more, and know where to look for guidance if things are not heading in the right direction”. (Service user 5)
3.3. Theme 3; Valued Social Support
3.3.1. Ongoing Health Professional Support
“It’s been lockdown and I’ve kind of gone off track. And, you know, he was always able to see and not just like a couple of minutes and say… “Do this, do this, do this”, it wasn’t like that, he gave me a lot of time, even on the phone”. (Service user 6)
3.3.2. Camaraderie among Other Service Users
“It was nice because I’m at home a lot. It is the first time that I’ve got to do something like this. Got to go in and work with like a group of people and get to meet new people, got to see some new faces and staff”. (Service user 6)
“The camaraderie. When I first came, we barely had coffee once every few weeks. And then we start coming down here to get a coffee, which is lovely. They lift you emotionally”. (Service user 12)
“I think not only with the service you get from the staff, it is the people you’ve never known before. I have illnesses similar to yours. They’re making you to discuss, when you talk to people. That’s the most important part of everything. […] You could do the workouts at home, which we did with Joe Wicks, but wasn’t quite the same. […] So again, I go back to coming back to people, not only the staff, but the people you meet. It’s all about that. It’s a mixture of human connection. […] And I think they’ve got a great group of people here to try it the right way. […] I value the support from the people. They are here to advise, to look after”. (Service user14)
3.3.3. More Follow-Up Is Needed
“And then there should be a report of your progress. Is it working or is it not working? To have measurements, is it working or is it not working? […] After the program, after six months down the line, they should ask “how are you getting on?” It is a tester. What happened after the tester? And you’ll always find some people. If you have 20, you might end up with five, who just want to keep going. Yes, it makes a difference to these five and should be worth it.” (Service user 5)
“At the end of the therapy, maybe someone to get like check-up on the people that are having therapy to make sure they’re okay or if like they need anything else. It would be a good idea.” (Service user 2)
3.4. Theme 4: Communication Is Key
3.4.1. Active Listening and Responding to Needs
“They listened to everything I said and they made me feel very comfortable to open up because it’s not something that I’ve been able to do before.” (Service user 2)
“I’ve told him that I wobble a lot, I don’t have good balance and he does help me and he does put things around to help me to do.” (Service user 12)
“I think I receive support based on my individual needs, but on others as well. […] I believe, they all know our needs.” (Service user 14)
3.4.2. Online vs. Face-to-Face
“I think the online courses, it’s all right, and they give you information base. The online course doesn’t answer some of your questions. I mean you can talk to someone face-to-face and say, well, I’ve got this. And that can give you a direct answer rather than you’re thinking, well, is that right, is that wrong.” (Service user 8)
3.4.3. Unaware of Integration
“I didn’t know it was a holist program. I think it would be nice that they explained what they were in the beginning. Saying, we could do this. Nobody ever said that to me. We do this, this, this, and this, you gradually find out for yourself really, just asking questions. I wasn’t aware of what they did until you graduate. It would be nice if you were sat down and someone spoke to you and told you: “We can help you completely.” No one ever said that; that would be nice and useful.” (Service user 11)
3.4.4. Poor Visibility of the Service
“I would say I’d highly recommend it. But it’s a lot of hard work in my heart to get the information. And because I am a person like that. I know how to get information. I am quite proactive in doing things. I could access it, but for a lot of people that would have been very difficult to do. […] I think when you get into it, it works. That’s just how you know it’s there…. for me the information of what they can do for you is not obvious.” (Service user 11)
“I am speaking to a friend of mine, a couple of friends of mine and they were like saying you’re very lucky because they will also have health issues and their GP is very reluctant to refer them to this type of service. They’re not even aware of this kind of service, they don’t even know about it. They need to advertise a bit more.” (Service user 6)
3.5. Theme 5: Flexible Referral Process
3.5.1. Health Professional Encouragement
“Because my doctor had concerns over my BMI. So, and he kept on saying to me, like you’ve got to do something, and then earlier this year I went to see. And he said to me, you’ve got to accept some help. So I said, All right, fair enough. So that’s what I came and I applied for the course, I got recommended for the course.” (Service user 8)
3.5.2. Ability to Self-Refer
“And then, after all that lockdown. I contacted the gym again. I’m a member there and I said, “Look, I really want to get back into exercise again and I need some help.” And so they gave me [name of member of staff], and she was brilliant. We met twice in the gym and we went to a program and then lockdown again. So, it has been wonderful. Really, really good.” (Service user 11)
3.5.3. Ease of Access
“They had leaflets up on the wall. I just took one of those and phoned that number. No problems at all.” (Service user 11)
“They’ve got some nurses at the surgery that I use, and they put me forward to the nurse who then rang me and said, they’ve got someone to do with people losing weight and stuff like that. And they then recommended me and someone contacted me about it.” (Service user 8)
3.6. Theme 6: Positive Impact on Life
3.6.1. Improved Health and Wellbeing
“I have. I managed to lose two stone, my blood pressure in normal now, the nurse said she was really shocked, that is beautiful, whatever you’re doing, keep it up. So, she was really good, I saw a lot of changes within myself.” (Service user 6)
“It made you think about what you want to eat, or what is helping you. I’m conscious of what I did, but it made me more aware of certain foods that I thought was ok. And in doing this, I lost weight over a week.” (Service user 9)
3.6.2. Changes in Social Life
“I definitely go out and socialize more, and how I was feeling before, I think before I went out and it was make not to want to go. But now, I like what I’ve learned in my mind and make sure that I don’t avoid situations just because of how I’m feeling because I’m never going to overcome it if I keep avoiding them. Definitely, like, I’m more willing to go and socialize.” (Service user 2)
3.6.3. Optimistic Outlook on Life
“They helped me physically, mentally and emotionally. So I will say they changed my life. I was suffering from a lot of health problems and rapidly a lot of it improved.” (Service user 6)
“I’m literally like a holy person. I said what my main goal is to get back myself again. What happened is to find myself again.” (Service user 3)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Lorenzo, A.; Gratteri, S.; Gualtieri, P.; Cammarano, A.; Bertucci, P.; Di Renzo, L. Why primary obesity is a disease? J. Transl. Med. 2019, 17, 169. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Obesity and Overweight: Fact Sheet [Internet]. 2018. Available online: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 9 June 2021).
- Baker, C. Obesity Statistics. Available online: https://commonslibrary.parliament.uk/research-briefings/sn03336/ (accessed on 22 December 2021).
- Kopelman, P. Health risks associated with overweight and obesity. Obes. Rev. 2007, 8, 13–17. [Google Scholar] [CrossRef]
- Wilson, P.W.; D’Agostino, R.B.; Sullivan, L.; Parise, H.; Kannel, W.B. Overweight and obesity as determinants of cardiovascular risk: The Framingham experience. Arch Intern. Med. 2002, 162, 1867–1872. [Google Scholar] [CrossRef] [Green Version]
- Calle, E.E.; Kaaks, R. Overweight, obesity and cancer: Epidemiological evidence and proposed mechanisms. Nat. Cancer 2004, 4, 579–591. [Google Scholar] [CrossRef]
- Chen, L.; Magliano, D.; Zimmet, P. The worldwide epidemiology of type 2 diabetes mellitus—Present and future perspectives. Nat. Rev. Endocrinol. 2011, 8, 228–236. [Google Scholar] [CrossRef] [PubMed]
- De Wit, L.; Luppino, F.; van Straten, A.; Penninx, B.; Zitman, F.; Cuijpers, P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res. 2010, 178, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.E.; Deleger, S.; Strawbridge, W.J.; Kaplan, G.A. Prospective association between obesity and depression: Evidence from the Alameda County Study. Int. J. Obes. 2003, 27, 514–521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gariepy, G.; Nitka, D.; Schmitz, N. The association between obesity and anxiety disorders in the population: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 407–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amiri, S.; Behnezhad, S. Obesity and anxiety symptoms: A systematic review and meta-analysis. Neuropsychiatrie 2019, 33, 72–89. [Google Scholar] [CrossRef]
- Moussa, O.; Ardissino, M.; Kulatilake, P.; Faraj, A.; Muttoni, E.; Darzi, A.; Ziprin, P.; Scholtz, S.; Purkayastha, S. Effect of body mass index on depression in a UK cohort of 363 037 obese patients: A longitudinal analysis of transition. Clin. Obes. 2019, 9, e12305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira-Miranda, E.; Costa, P.R.; Queiroz, V.A.; Pereira-Santos, M.; Santana, M.L.P. Overweight and Obesity Associated with Higher Depression Prevalence in Adults: A Systematic Review and Meta-Analysis. J. Am. Coll. Nutr. 2017, 36, 223–233. [Google Scholar] [CrossRef]
- Holmes, J. Tackling Obesity: The Role of the NHS in a Whole-System Approach; The King’s Fund: London, UK, 2021. [Google Scholar]
- Nichols, M.; Newman, S.; Nemeth, L.S.; Magwood, G. The influence of parental participation on obesity interventions in african american adolescent females: An integrative review. J. Pediatr. Nurs. 2015, 30, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. PHE Strategy 2020-25. 2019. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/831562/PHE_Strategy_2020-25.pdf (accessed on 20 October 2021).
- Cameron, A.; Bostock, L.; Lart, R. Service user and carers perspectives of joint and integrated working between health and social care. J. Integr. Care 2014, 22, 62–70. [Google Scholar] [CrossRef] [Green Version]
- Spoorenberg, S.L.W.; Wynia, K.; Fokkens, A.S.; Slotman, K.; Kremer, H.P.H.; Reijneveld, S. Experiences of Community-Living Older Adults Receiving Integrated Care Based on the Chronic Care Model: A Qualitative Study. PLoS ONE 2015, 10, e0137803. [Google Scholar] [CrossRef] [PubMed]
- Anand, K.; Karade, S.; Sen, S.; Gupta, R.M. SARS-CoV-2: Camazotz’s Curse. Med. J. Armed Forces India 2020, 76, 136–141. [Google Scholar] [CrossRef]
- Greenfield, G.; Ignatowicz, A.M.; Belsi, A.; Pappas, Y.; Car, J.; Majeed, A.; Harris, M. Wake up, Wake up! It’s Me! It’s My Life! BMC Health Serv. Res. 2014, 14, 619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ralston, J.D.; Revere, D.; Robins, L.S.; Goldberg, H.I. An Interactive Electronic Medical Record: Qualitative Study. Bmj 2004, 328, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Glaser, B.G.; Strauss, A.L. Discovery of Grounded Theory: Strategies for Qualitative Research; Routledge: Oxford, UK, 2017. [Google Scholar]
- Peat, G.; Rodriguez, A.; Smith, J. Interpretive phenomenological analysis applied to healthcare research. Evid. Based Nurs. 2019, 22, 7–9. [Google Scholar] [CrossRef]
- Neubauer, B.E.; Witkop, C.T.; Varpio, L. How phenomenology can help us learn from the experiences of others. Perspect. Med. Educ. 2019, 8, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Sutcliffe, K.; Melendez-Torres, G.J.; Burchett, H.; Richardson, M.; Rees, R.; Thomas, J. The importance of service-users’ perspectives: A systematic review of qualitative evidence reveals overlooked critical features of weight management programmes. Health Expect. 2018, 21, 563–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allan, K.; Hoddinott, P.; Avenell, A. A qualitative study comparing commercial and health service weight loss groups, classes and clubs. J. Hum. Nutr. Diet. 2011, 24, 23–31. [Google Scholar] [CrossRef] [Green Version]
- Brown, I.; Thompson, J.; Tod, A.; Jones, G. Primary care support for tackling obesity: A qualitative study of the perceptions of obese patients. Br. J. Gen. Pract. 2006, 56, 666–672. [Google Scholar]
- Webb, R.; Davies, I.; Johnson, B.R.; Abayomi, J. A qualitative evaluation of an NHS Weight Management Programme for obese patients in Liverpool. Nutr. Food Sci. 2014, 44, 144–155. [Google Scholar] [CrossRef]
- Ahern, A.L.; Boyland, E.J.; Jebb, S.A.; Cohn, S.R. Participants’ explanatory model of being overweight and their experiences of 2 weight loss interventions. Ann. Fam. Med. 2013, 11, 251–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bidgood, J.; Buckroyd, J. An exploration of obese adults’ experience of attempting to lose weight and to maintain a reduced weight. Couns. Psychother. Res. 2005, 5, 221–229. [Google Scholar] [CrossRef]
- Nossum, R.; Rise, M.B.; Steinsbekk, A. Patient education—Which parts of the content predict impact on coping skills? Scand. J. Public Health 2013, 41, 429–435. [Google Scholar] [CrossRef]
- Solberg, H.S.; Steinsbekk, A.; Solbjør, M.; Granbo, R.; Garåsen, H. Characteristics of a self-management support programme applicable in primary health care: A qualitative study of users’ and health professionals’ perceptions. BMC Health Serv. Res. 2014, 14, 562. [Google Scholar] [CrossRef]
- Wormald, H.; Waters, H.; Sleap, M.; Ingle, L. Participants’ perceptions of a lifestyle approach to promoting physical activity: Targeting deprived communities in Kingston-Upon-Hull. BMC Public Health 2006, 6, 202. [Google Scholar] [CrossRef] [Green Version]
- Morrison, Z.; Douglas, A.; Bhopal, R.; Sheikh, A.; Forbes, J.F.; Gill, J.M.R.; Lean, M.; McKnight, J.; Murray, G.; Sattar, N.; et al. Understanding experiences of participating in a weight loss lifestyle intervention trial: A qualitative evaluation of South Asians at high risk of diabetes. BMJ Open 2014, 4, e004736. [Google Scholar] [CrossRef] [Green Version]
- Ross Middleton, K.M.; Patidar, S.M.; Perri, M.G. The impact of extended care on the long-term maintenance of weight loss: A systematic review and meta-analysis. Obes Rev. 2012, 13, 509–517. [Google Scholar] [CrossRef] [PubMed]
- Howlett, N.; Trivedi, D.; A Troop, N.A.; Chater, A.M. Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Transl. Behav. Med. 2019, 9, 147–157. [Google Scholar] [CrossRef]
- Perri, M.G.; Ariel-Donges, A.H. Maintenance of weight lost in behavioral treatment of obesity. In Handbook of Obesity Treatment; Wadden, T., Bray, G., Eds.; The Gilford Press: New York, NY, USA, 2018; 393p. [Google Scholar]
- Coulter, A.; Oldham, S.J. Person-centred care: What is it and how do we get there? Futur. Hosp. J. 2016, 3, 114–116. [Google Scholar] [CrossRef]
- Wodskou, P.M.; Høst, D.; Godtfredsen, N.S.; Frølich, A. A qualitative study of integrated care from the perspectives of patients with chronic obstructive pulmonary disease and their relatives. BMC Health Serv. Res. 2014, 14, 471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef]
- Berendsen, A.J.; De Jong, G.M.; Jong, B.M.-D.; Dekker, J.; Schuling, J. Transition of care: Experiences and preferences of patients across the primary/secondary interface a qualitative study. BMC Health Serv. Res. 2009, 9, 62–68. [Google Scholar] [CrossRef] [Green Version]
- Jones, N.; Furlanetto, D.L.C.; Jackson, J.A.; Kinn, S. An investigation of obese adults’ views of the outcomes of dietary treatment. J. Hum. Nutr. Diet. 2007, 20, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Garip, G.; Yardley, L. A synthesis of qualitative research on overweight and obese people’s views and experiences of weight management. Clin. Obes. 2011, 1, 110–126. [Google Scholar] [CrossRef]
- Müller, A.M.; Khoo, S. Non-Face-to-face physical activity interventions in older adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 35. [Google Scholar] [CrossRef] [Green Version]
- Opdenacker, J.; Boen, F. Effectiveness of face-to-face versus telephone support in increasing physical activity and mental health among university employees. J. Phys. Act. Health 2008, 5, 830–843. [Google Scholar] [CrossRef] [Green Version]
- Steele, R.M.; Mummery, W.K.; Dwyer, T. A comparison of face-to-face or internet-delivered physical activity intervention on targeted determinants. Health Educ. Behav. 2009, 36, 1051–1064. [Google Scholar] [CrossRef] [PubMed]
- Van Genugten, L.; Van Empelen, P.; Boon, B.; Borsboom, G.; Visscher, T.; Oenema, A. Results from an online computer-tailored weight management intervention for overweight adults: Randomized controlled trial. J. Med. Internet Res. 2012, 14, 100–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, P.T.; Hart-Johnson, T.; Santen, S.A.; Zaidi, N.L.B. Considerations for using race and ethnicity as quantitative variables in medical education research. Perspect. Med. Educ. 2020, 9, 318–323. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Cencus 2011 [Internet]. 2021. Available online: https://www.ons.gov.uk/ (accessed on 22 October 2021).
| Service User ID | Gender | Age | Ethnicity | Type of Referred Services | Status in the Programme (at the Stage of the Interview) |
|---|---|---|---|---|---|
| Service user 1 | Female | 59 | White—British | IAPT/smoking cessation/WM | Finished |
| Service user 2 | Female | 24 | White—British | IAPT | Finished |
| Service user 3 | Female | 33 | White—British | IAPT | Finished |
| Service user 4 | Male | 43 | White—Irish | IAPT | In process |
| Service user 5 | Female | 59 | N/A | WM | Finished |
| Service user 6 | Female | 35 | Asian/Asian British—Bangladeshi | WM/IAPT/SP | In process |
| Service user 7 | Female | 59 | White—British | WM/IAPT | Finished |
| Service user 8 | Male | 56 | White—British | WM | Finished |
| Service user 9 | Male | 66 | White—British | WM | Finished |
| Service user 10 | Female | 41 | N/A | WM | Finished |
| Service user 11 | Female | 66 | White—British | WM | Finished |
| Service user 12 | Female | 72 | White—British | WM | In process |
| Service user 13 | Male | 65 | White—British | WM | In process |
| Service user 14 | Male | 65 | White—British | WM | In process |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liapi, F.; Chater, A.M.; Pescheny, J.V.; Randhawa, G.; Pappas, Y. Understanding the Experience of Service Users in an Integrated Care Programme for Obesity and Mental Health: A Qualitative Investigation of Total Wellbeing Luton. Int. J. Environ. Res. Public Health 2022, 19, 817. https://doi.org/10.3390/ijerph19020817
Liapi F, Chater AM, Pescheny JV, Randhawa G, Pappas Y. Understanding the Experience of Service Users in an Integrated Care Programme for Obesity and Mental Health: A Qualitative Investigation of Total Wellbeing Luton. International Journal of Environmental Research and Public Health. 2022; 19(2):817. https://doi.org/10.3390/ijerph19020817
Chicago/Turabian StyleLiapi, Fani, Angel Marie Chater, Julia Vera Pescheny, Gurch Randhawa, and Yannis Pappas. 2022. "Understanding the Experience of Service Users in an Integrated Care Programme for Obesity and Mental Health: A Qualitative Investigation of Total Wellbeing Luton" International Journal of Environmental Research and Public Health 19, no. 2: 817. https://doi.org/10.3390/ijerph19020817
APA StyleLiapi, F., Chater, A. M., Pescheny, J. V., Randhawa, G., & Pappas, Y. (2022). Understanding the Experience of Service Users in an Integrated Care Programme for Obesity and Mental Health: A Qualitative Investigation of Total Wellbeing Luton. International Journal of Environmental Research and Public Health, 19(2), 817. https://doi.org/10.3390/ijerph19020817






