Efficacy of the Treatment of Plantar Warts Using 1064 nm Laser and Cooling
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Work and Ethical Aspects
2.2. Patients
2.3. Laser Instrumentation
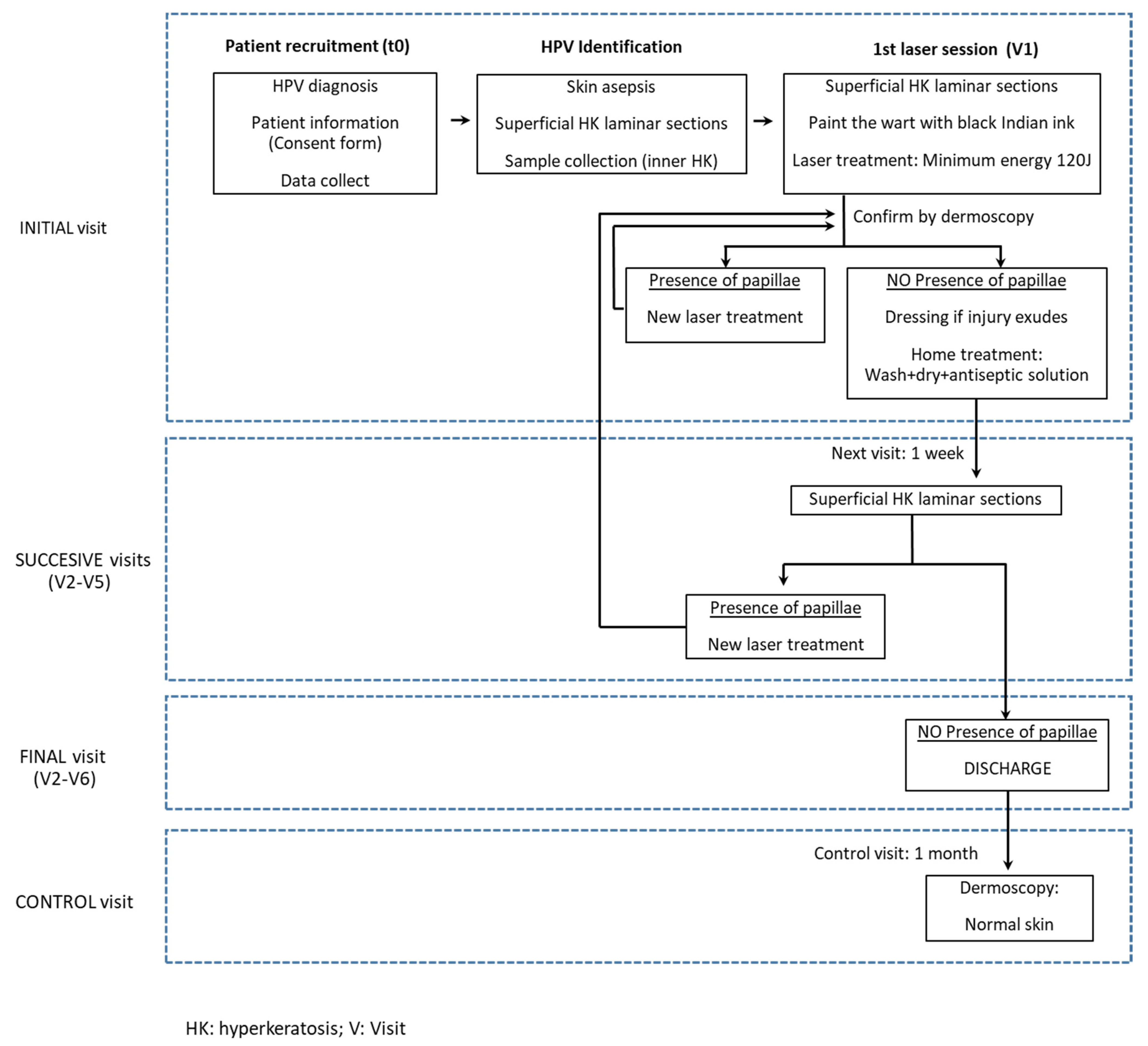
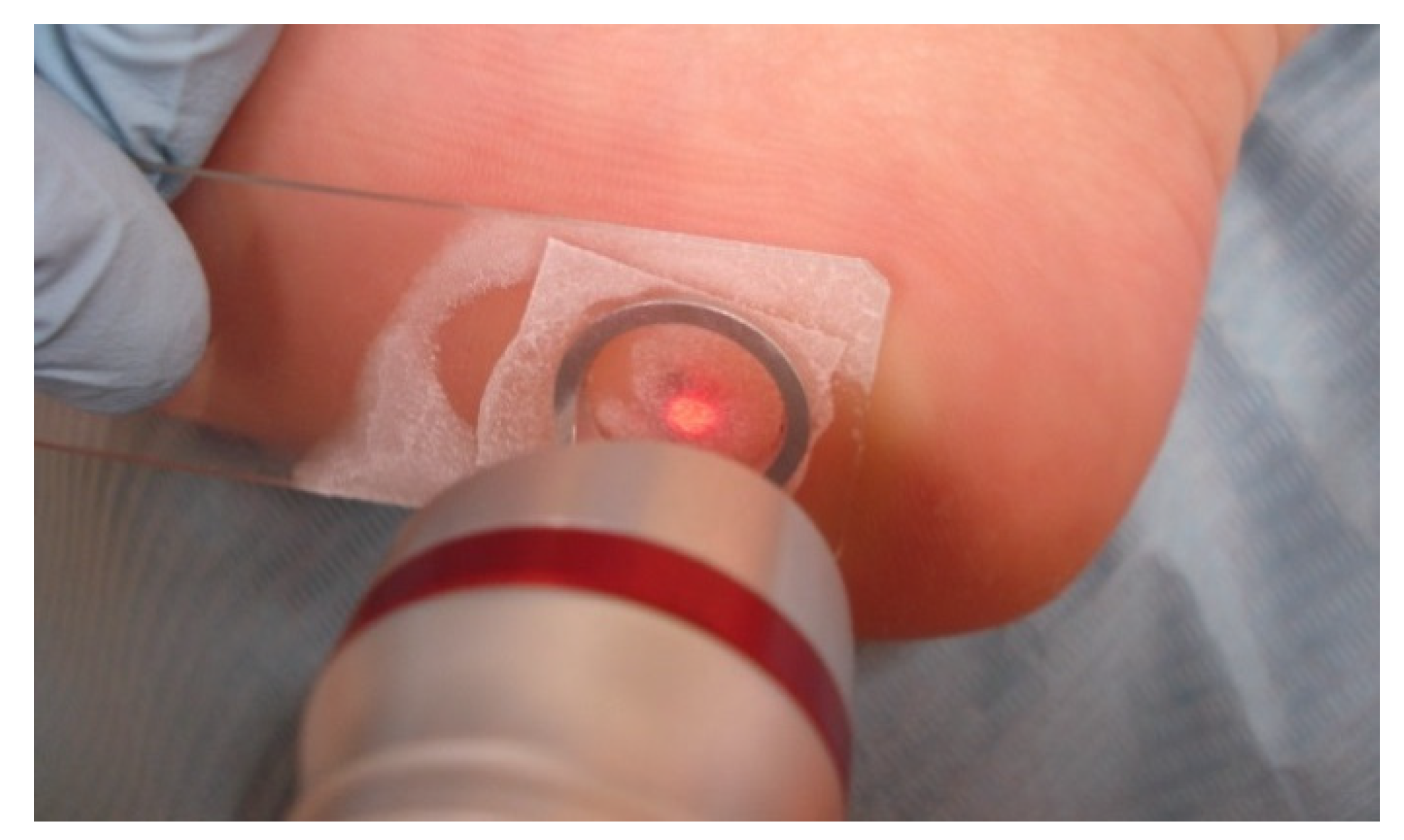
2.4. Cutaneous Warts Treatment
2.5. Viral Genotypes
2.6. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Kirnbauer, R.; Klenz, P.; Okun, M.M. Virus del papiloma humano. In Dermatologia; Bolognia, J.L., Jorizzo, J.L., Rapini, R.R., Eds.; Elsevier, Cop.: Madrid, Spain, 2004; Volume 1, pp. 1217–1225. [Google Scholar]
- Bruggink, S.C.; de Koning, M.N.; Gussekloo, J.; Egberts, P.F.; ter Schegget, J.; Feltkamp, M.; Bavinck, J.N.B.; Quint, W.G.; Assendelft, W.; Eekhof, J.A. Cutaneous wart-associated HPV types: Prevalence and relation with patient characteristics. J. Clin. Virol. 2012, 55, 250–255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yelverton, C.B. Verrugas. In Manual de Tratamiento de las Enfermedadesdermatológicas, 7th ed.; Arndt, K.A., Hsu, J.H., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; pp. 233–241. [Google Scholar]
- Androphy, E.J.; Lowy, D.R. Verrugas. In Dermatologíaenmedicina General [de] Fitzpatrick, 7th ed.; Wolff, K., Goldsmith, L.A., Katz, S.I., Gilchrest, B.A., Paller, A.S., Leffell, D.J., Eds.; MédicaPanamericana, Cop.: Madrid, Spain, 2009; pp. 1914–1923. [Google Scholar]
- Burns, D.A. ‘Warts and all’—The history and folklore of warts: A review. J. R. Soc. Med. 1992, 85, 37–40. [Google Scholar] [PubMed]
- Al Bdour, S.; Akkash, L.; Shehabi, A.A. Detection and typing of common human papillomaviruses among Jordanian patients. J. Med. Virol. 2013, 85, 1058–1062. [Google Scholar] [CrossRef] [PubMed]
- Sasagawa, T.; Mitsuishi, T. Novel polymerase chain reaction method for detecting cutaneous human papillomavirus DNA. J. Med. Virol. 2012, 84, 138–144. [Google Scholar] [CrossRef] [PubMed]
- de Planell-Mas, E.; Martínez-Garriga, B.; Zalacain, A.J.; Vinuesa, T.; Viñas, M. Human papillomaviruses genotyping in plantar warts. J. Med. Virol. 2017, 89, 902–907. [Google Scholar] [CrossRef] [PubMed]
- Jennings, M.B.; Ricketti, J.; Guadara, J.; Nach, W.; Goodwin, S. Treatment for simple plantar verrucae: Monochloroacetic acid and 10% formaldehyde versus 10% formaldehyde alone. J. Am. Podiatr. Med. Assoc. 2006, 96, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Soni, P.; Khandelwal, K.; Aara, N.; Ghiya, B.C.; Mehta, R.D.; Bumb, R.A. Efficacy of intralesional bleomycin in palmo-plantar and periungual warts. J. Cutan. Aesthetic Surg. 2011, 4, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Kimura, U.; Takeuchi, K.; Kinoshita, A.; Takamori, K.; Suga, Y. Long-pulsed 1064-nm neodymium:yttrium-aluminum-garnet laser treatment for refractory warts on hands and feet. J. Dermatol. 2014, 41, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Landthaler, M.; Bäumler, W.; Hohenleutner, U. Lasers and Flashlamps in Dermatology. In Fitzpatrick’s Dermatology in General Medicine, 8th ed.; Goldsmith, L.A., Katz, S.I., Gilchrest, B.A., Paller, A.S., Leffell, D.J., Wolff., K., Eds.; McGraw-Hill Education LLC: New York, NY, USA, 2012; pp. 1–2. [Google Scholar]
- Lloyd, A.A.; Graves, M.S.; Ross, E.V. Laser-Tissue Interactions. In Lasers in Dermatology and Medicine Dermatologic Applications, 2nd ed.; Nouri, K., Ed.; Springer International Publishing: Cham, Switzerland, 2018; ebook; pp. 17–20. [Google Scholar]
- Sakamoto, F.H.; Wall, T.; Avram, M.M.; Anderson, R.R. Lasers and Flashlamps in Dermatology. In Fitzpatrick’s Dermatology in General Medicine, 7th ed.; Wolff, K., Goldsmith, L.A., Katz, S.I., Gilchrest, B.A., Paller, A.S., Leffell, D.J., Eds.; McGraw-Hill Education LLC: New York, NY, USA, 2008; pp. 2263–2264. [Google Scholar]
- Smith, E.; Patel, S.; Whiteley, M. Evaluating the success of Nd: YAG laser ablation in the treatment of recalcitrant verruca plantaris and a cautionary note about local anaesthesia on the plantar aspect of the foot. J. Eur. Acad. Dermatol. Venereol. 2014, 29, 463–467. [Google Scholar] [CrossRef] [PubMed]
- Young, S.; Cohen, G.E. Treatment of Verruca Plantaris with a Combination of Topical Fluorouracil and Salicylic Acid. J. Am. Podiatr. Med. Assoc. 2005, 95, 366–369. [Google Scholar] [CrossRef] [PubMed]
- Bae, J.; Kang, H.; Kim, H.; Park, Y. Differential diagnosis of plantar wart from corn, callus and healed wart with the aid of dermoscopy. Br. J. Dermatol. 2008, 160, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Ley, J.; Guijo, I.; Vega, M.E. Fundamentos y Novedades Terapéuticas del Láser Vascular; Grupo Vena Estética: Madrid, Spain, 2002. [Google Scholar]
- Gutknecht, N. A Odontología e o Laser. Atuaçao do Laser na Especialidade Odontológica; Quintessence: Sao Paulo, Brazil, 2004. [Google Scholar]
- Arnabat, J. Efecto Bactericida del Láser de Er, Cr:YSGG en el Interior del Conducto Radicular. Ph.D. Thesis, University of Barcelona, Barcelona, Spain, 15 December 2005. [Google Scholar]
- Han, T.Y.; Lee, J.H.; Lee, C.K.; Ahn, J.Y.; Seo, S.J.; Hong, C.K. Long-Pulsed Nd:YAG Laser Treatment of Warts: Report on a Series of 369 Cases. J. Korean Med. Sci. 2009, 24, 889–893. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bacelieri, R.; Johnson, S.M. Cutaneous warts: An evidence-based approach to therapy. Am. Fam. Physician 2005, 72, 647–652. [Google Scholar] [PubMed]
- Tan, O.T.; Hurwitz, R.M.; Stafford, T.J. Pulsed dye laser treatment of recalcitrant verrucae: A preliminary report. Lasers Surg. Med. 1993, 13, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Taneja, G.; Hazarika, N.; Bhatia, R. Effectiveness of autoinoculation in viral warts: A single arm, open-label, and clinical trial. Dermatol. Ther. 2020, 33, e14122. [Google Scholar] [CrossRef] [PubMed]


| Variable | Total (n = 41) | HPV-1 (n = 6) | HPV-2 (n = 8) | HPV-27 (n = 7) | HPV-57 (n = 17) | HPV-65 (n = 3) | p-Value (1) | |
|---|---|---|---|---|---|---|---|---|
| Warts | Yes | 41 | 6 | 8 | 7 | 17 | 3 | |
| Total | 41 | 6 | 8 | 7 | 17 | 3 | ||
| Healed warts | Yes | 35 | 6 | 4 | 6 | 16 | 3 | |
| No | 6 | 4 | 1 | 1 | ||||
| Total | 41 | 6 | 8 | 7 | 17 | 3 | 0.0315 | |
| Healing achieved at: | Visit 2 | 7 | 1 | 2 | 1 | 3 | ||
| Visit 3 | 10 | 1 | 1 | 2 | 5 | 1 | ||
| Visit 4 | 12 | 2 | 3 | 5 | 2 | |||
| Visit 5 | 1 | 1 | ||||||
| Visit 6 | 5 | 2 | 1 | 2 | ||||
| Total | 35 | 6 | 4 | 6 | 16 | 3 | 0.8653 | |
| Change of treatment | Yes | 4 | 3 | 1 | ||||
| No | 37 | 6 | 5 | 7 | 16 | 3 | ||
| Total | 41 | 6 | 8 | 7 | 17 | 3 | 0.0608 | |
| Treatment abandonment | Yes | 2 | 1 | 1 | ||||
| No | 39 | 6 | 7 | 6 | 17 | 3 | ||
| Total | 41 | 6 | 8 | 7 | 17 | 3 | 0.4525 |
| Variable | Total (n = 41) | Forefoot (n = 13) | Midfoot (n = 4) | Toes (n = 13) | Heel (n = 11) | p-Value (1) | |
|---|---|---|---|---|---|---|---|
| Warts | Total | 41 | 13 | 4 | 13 | 11 | |
| Yes | 41 | 13 | 4 | 13 | 11 | ||
| Healed warts | Yes | 35 | 9 | 3 | 12 | 11 | |
| No | 6 | 4 | 1 | 1 | |||
| Total | 41 | 13 | 4 | 13 | 11 | 0.1422 | |
| Healing achieved at: | Visit 2 | 7 | 2 | 2 | 2 | 1 | |
| Visit 3 | 10 | 1 | 3 | 6 | |||
| Visit 4 | 12 | 5 | 1 | 4 | 2 | ||
| Visit 5 | 1 | 1 | |||||
| Visit 6 | 5 | 1 | 2 | 2 | |||
| Total | 35 | 9 | 3 | 12 | 11 | 0.3636 | |
| Change of treatment | Yes | 4 | 2 | 1 | 1 | ||
| No | 37 | 11 | 3 | 12 | 11 | ||
| Total | 41 | 13 | 4 | 13 | 11 | 0.4275 | |
| Treatment abandonment | Yes | 2 | 2 | ||||
| No | 39 | 11 | 4 | 13 | 11 | ||
| Total | 41 | 13 | 4 | 13 | 11 | 0.2098 |
| Variable | Total | ≤4 mm | >4 mm | p-Value (1) | |
|---|---|---|---|---|---|
| Warts | Yes | ||||
| Total | 41 | 18 | 23 | ||
| Healing warts | Yes | 35 | 15 | 20 | |
| No | 6 | 3 | 3 | ||
| Total | 41 | 18 | 23 | 0.7446 | |
| Healing achieved at: | Visit 2 | 7 | 4 | 3 | |
| Visit 3 | 10 | 4 | 6 | ||
| Visit 4 | 12 | 6 | 6 | ||
| Visit 5 | 1 | 1 | |||
| Visit 6 | 5 | 5 | |||
| Total | 35 | 15 | 20 | 0.2029 | |
| Change of treatment | Yes | 4 | 2 | 2 | |
| No | 37 | 16 | 21 | ||
| Total | 41 | 18 | 23 | 0.7959 | |
| Treatment abandonment | Yes | 2 | 1 | 1 | |
| No | 39 | 17 | 22 | ||
| Total | 41 | 18 | 23 | 0.8586 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Planell-Mas, E.; Martínez-Garriga, B.; Viñas, M.; Zalacain-Vicuña, A.J. Efficacy of the Treatment of Plantar Warts Using 1064 nm Laser and Cooling. Int. J. Environ. Res. Public Health 2022, 19, 801. https://doi.org/10.3390/ijerph19020801
de Planell-Mas E, Martínez-Garriga B, Viñas M, Zalacain-Vicuña AJ. Efficacy of the Treatment of Plantar Warts Using 1064 nm Laser and Cooling. International Journal of Environmental Research and Public Health. 2022; 19(2):801. https://doi.org/10.3390/ijerph19020801
Chicago/Turabian Stylede Planell-Mas, Elena, Blanca Martínez-Garriga, Miguel Viñas, and Antonio J. Zalacain-Vicuña. 2022. "Efficacy of the Treatment of Plantar Warts Using 1064 nm Laser and Cooling" International Journal of Environmental Research and Public Health 19, no. 2: 801. https://doi.org/10.3390/ijerph19020801
APA Stylede Planell-Mas, E., Martínez-Garriga, B., Viñas, M., & Zalacain-Vicuña, A. J. (2022). Efficacy of the Treatment of Plantar Warts Using 1064 nm Laser and Cooling. International Journal of Environmental Research and Public Health, 19(2), 801. https://doi.org/10.3390/ijerph19020801







