Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Institutional Approvals
2.3. Selection of Households
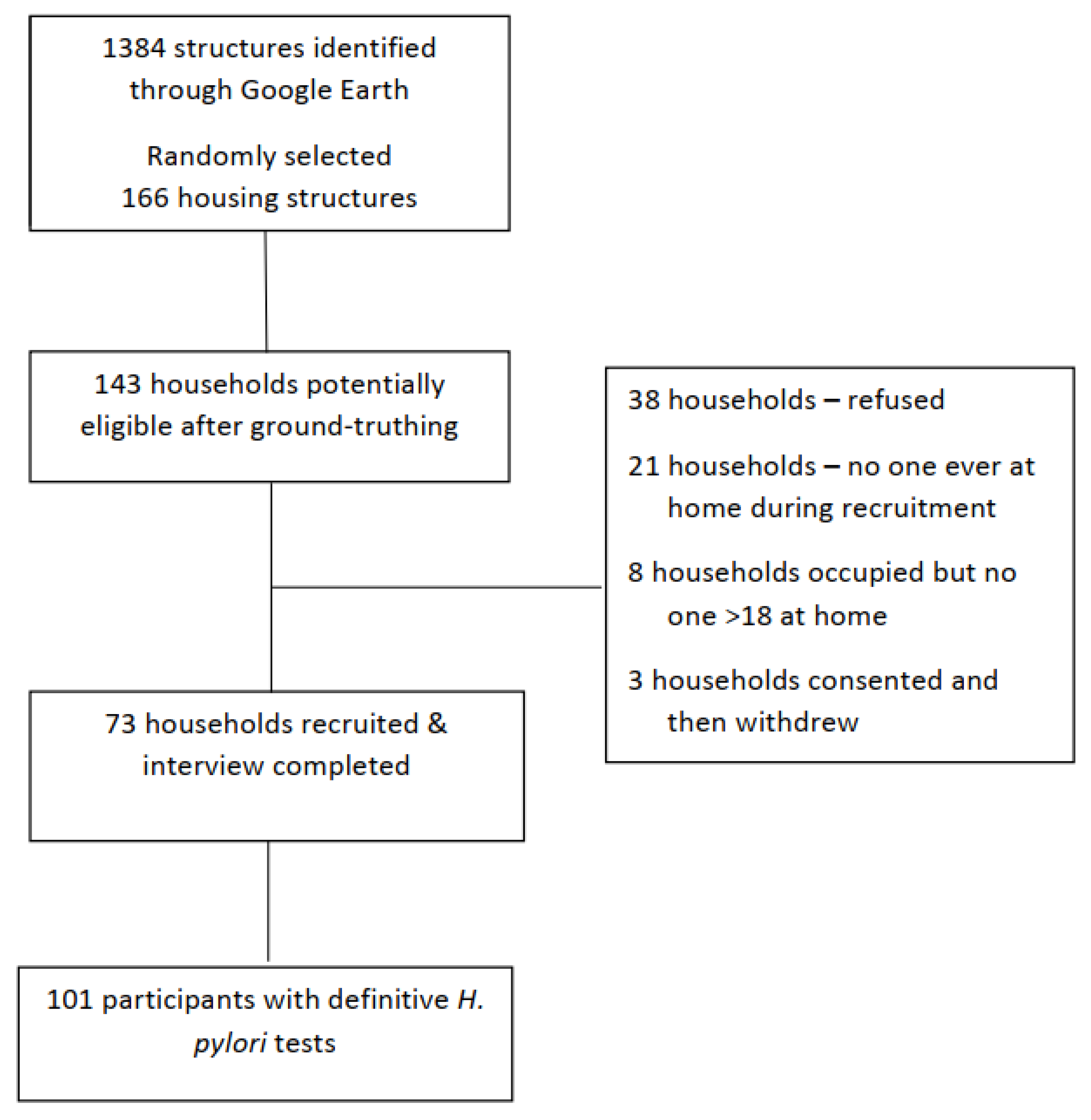
2.4. Recruitment
2.5. Training
2.6. Data Collection
2.7. Measures
2.8. Statistical Analysis
2.9. Sensitivity Analyses
3. Results
3.1. Individual and Household Characteristics
3.2. Prevalence of H. pylori Infection
3.3. Association of Risk Factors for Infection
3.4. H. pylori Awareness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Makola, D.; Peura, D.A.; Crowe, S.E. Helicobacter pylori Infection and Related Gastrointestinal Diseases. J. Clin. Gastroenterol. 2007, 41, 548–558. [Google Scholar] [CrossRef]
- De Martel, C.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncol. 2012, 13, 607–615. [Google Scholar] [CrossRef]
- Eusebi, L.H.; Zagari, R.M.; Bazzoli, F. Epidemiology of Helicobacter pylori Infection. Helicobacter 2014, 19 (Suppl. 1), 1–5. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.M. Helicobacter Pylori: Epidemiology and Routes of Transmission. Epidemiol. Rev. 2000, 22, 283–297. [Google Scholar] [CrossRef] [PubMed]
- Staat, M.A.; Kruszon-Moran, D.; McQuillan, G.M.; Kaslow, R.A. A Population-Based Serologic Survey of Helicobacter pylori Infection in Children and Adolescents in the United States. J. Infect. Dis. 1996, 174, 1120–1123. [Google Scholar] [CrossRef] [Green Version]
- Mapel, D.; Roberts, M.; Overhiser, A.; Mason, A. The Epidemiology, Diagnosis, and Cost of Dyspepsia and Helicobacter pylori Gastritis: A Case–Control Analysis in the Southwestern United States. Helicobacter 2013, 18, 54–65. [Google Scholar] [CrossRef] [Green Version]
- McColl, K.E.L. Helicobacter pylori Infection. N. Engl. J. Med. 2010, 362, 1597–1604. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, M.M.; Sharaf, R.R.; Aziz, R.K. Helicobacter pylori: A poor man’s gut pathogen? Gut Pathog. 2010, 2, 2. [Google Scholar] [CrossRef] [Green Version]
- Portal-Celhay, C.; Perez-Perez, G.I. Immune responses to Helicobacter pylori colonization: Mechanisms and clinical outcomes. Clin. Sci. 2006, 110, 305–314. [Google Scholar] [CrossRef] [Green Version]
- Ernst, P.B.; Gold, B.D. The Disease Spectrum of Helicobacter Pylori: The Immunopathogenesis of Gastroduodenal Ulcer and Gastric Cancer. Annu. Rev. Microbiol. 2000, 54, 615–640. [Google Scholar] [CrossRef]
- Peek, R.M.; Blaser, M.J. Helicobacter pylori and gastrointestinal tract adenocarcinomas. Nat. Cancer 2002, 2, 28–37. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Agency for Research on Cancer. World Cancer Report 2014, 3rd ed.; Stewart, B.W., Wild, C., Eds.; IARC: Lyon, France, 2014. [Google Scholar]
- Wild, C.P.; Weiderpass, E.; Stewart, B.W. World Cancer Report: Cancer Research for Cancer Prevention; Wild, C.P., Weiderpass, E., Stewart, B.W., Eds.; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- Ferro, A.; Peleteiro, B.; Malvezzi, M.; Bosetti, C.; Bertuccio, P.; Levi, F.; Negri, E.; La Vecchia, C.; Lunet, N. Worldwide trends in gastric cancer mortality (1980–2011), with predictions to 2015, and incidence by subtype. Eur. J. Cancer 2014, 50, 1330–1344. [Google Scholar] [CrossRef] [Green Version]
- Rawla, P.; Barsouk, A. Epidemiology of gastric cancer: Global trends, risk factors and prevention. Gastroenterol. Rev. 2019, 14, 26–38. [Google Scholar] [CrossRef]
- Melkonian, S.C.; Jim, M.A.; Haverkamp, D.; Wiggins, C.L.; Mccollum, J.; White, M.C.; Kaur, J.S.; Espey, D.K. Disparities in Cancer Incidence and Trends among American Indians and Alaska Natives in the United States, 2010–2015. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1604–1611. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, H.E.; Dennis, L.K.; Lauro, P.; Jain, P.; Pelley, E.; Oren, E. Emerging Evidence for Infectious Causes of Cancer in the United States. Epidemiol. Rev. 2019, 41, 82–96. [Google Scholar] [CrossRef]
- Navajo Cancer Workgroup. Cancer among the Navajo 2005–2013; Navajo Epidemiology Center, Navajo Department of Health, Navajo Nation: Window Rock, AZ, USA, 2018. Available online: https://www.nec.navajo-nsn.gov/Portals/0/Reports/Cancer%20Among%20Navajo%202018%20Spread.pdf (accessed on 2 January 2022).
- Kelley, J.R.; Duggan, J.M. Gastric cancer epidemiology and risk factors. J. Clin. Epidemiol. 2003, 56, 1–9. [Google Scholar] [CrossRef]
- Buiatti, E.; Palli, D.; Decarli, A.; Amadori, D.; Avellini, C.; Bianchi, S.; Biserni, R.; Cipriani, F.; Cocco, P.; Giacosa, A.; et al. A case-control study of gastric cancer and diet in Italy. Int. J. Cancer 1989, 44, 611–616. [Google Scholar] [CrossRef]
- Hansson, L.-E.; Baron, J.; Nyrén, O.; Bergström, R.; Wolk, A.; Adami, H.-O. Tobacco, alcohol and the risk of gastric cancer. A population-based case-control study in Sweden. Int. J. Cancer 1994, 57, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Santiago, P.; Moreno, Y.; Ferrus, M.A. Identification of Viable Helicobacter pylori in Drinking Water Supplies by Cultural and Molecular Techniques. Helicobacter 2015, 20, 252–259. [Google Scholar] [CrossRef]
- Bui, D.; Harris, R.B.; Oren, E.; Brown, H. Serologic Evidence for Fecal–Oral Transmission of Helicobacter pylori. Am. J. Trop. Med. Hyg. 2016, 94, 82–88. [Google Scholar] [CrossRef] [Green Version]
- Baker, K.H.; Hegarty, J.P. Presence of Helicobacter pylori in drinking water is associated with clinical infection. Scand. J. Infect. Dis. 2001, 33, 744–746. [Google Scholar] [CrossRef] [Green Version]
- Rolle-Kampczyk, U.E.; Fritz, G.J.; Diez, U.; Lehmann, I.; Richter, M.; Herbarth, O. Well water—One source of Helicobacter pylori colonization. Int. J. Hyg. Environ. Health 2004, 207, 363–368. [Google Scholar] [CrossRef]
- Sethi, A.; Chaudhuri, M.; Kelly, L.; Hopman, W. Prevalence of Helicobacter pylori in a First Nations population in northwestern Ontario. Can. Fam. Physician Med. Fam. Can. 2013, 59, e182–e187. [Google Scholar]
- Bernstein, C.N.; McKeown, I.; Embil, J.M.; Blanchard, J.F.; Dawood, M.; Kabani, A.; Kliewer, E.; Smart, G.; Coghlan, G.; Macdonald, S.; et al. Seroprevalence of Helicobacter pylori, incidence of gastric cancer, and peptic ulcer-associated hospitalizations in a Canadian Indian population. Dig. Dis. Sci. 1999, 44, 668–674. [Google Scholar] [CrossRef] [PubMed]
- Melius, E.; Sobel, J. Risk Factors for Helicobacter pylori in a Rural Community in Montana. In Proceedings of the 54th Annual Epidemic Intelligence Service (EIS) Conference, Atlanta, GA, USA, 11–15 April 2005. [Google Scholar]
- Parkinson, A.J.; Gold, B.D.; Bulkow, L.; Wainwright, R.B.; Swaminathan, B.; Khanna, B.; Petersen, K.M.; Fitzgerald, M.A. High Prevalence of Helicobacter pylori in the Alaska Native Population and Association with Low Serum Ferritin Levels in Young Adults. Clin. Diagn. Lab. Immunol. 2000, 7, 885–888. [Google Scholar] [CrossRef] [Green Version]
- Nagy, P.; Johansson, S.; Molloy-Bland, M. Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 2016, 8, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huerta-Franco, M.-R.; Banderas, J.W.; E Allsworth, J. Ethnic/racial differences in gastrointestinal symptoms and diagnosis associated with the risk of Helicobacter pylori infection in the US. Clin. Exp. Gastroenterol. 2018, 11, 39–49. [Google Scholar] [CrossRef] [Green Version]
- Navajo Nation Wind. Navajo Nation Profile. Available online: https://navajoprofile.wind.enavajo.org/ (accessed on 1 May 2020).
- Ferwana, M.; Abdulmajeed, I.; Alhajiahmed, A.; Madani, W.; Firwana, B.; Hasan, R.; Altayar, O.; Limburg, P.J.; Murad, M.H.; Knawy, B. Accuracy of urea breath test in Helicobacter pylori infection: Meta-analysis. World J. Gastroenterol. 2015, 21, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Miernyk, K.M.; Bulkow, L.R.; Gold, B.D.; Bruce, M.G.; Hurlburt, D.H.; Griffin, P.M.; Swerdlow, D.L.; Cook, K.; Hennessy, T.W.; Parkinson, A.J. Prevalence ofHelicobacter pyloriamong Alaskans: Factors associated with infection and comparison of urea breath test and anti-Helicobacter pylori IgG antibodies. Helicobacter 2018, 23, e12482. [Google Scholar] [CrossRef]
- Bruden, D.L. Diagnostic accuracy of tests for Helicobacter pylori in an Alaska Native population. World J. Gastroenterol. 2011, 17, 4682–4688. [Google Scholar] [CrossRef]
- Robinson, L.E.; Black, F.L.; Lee, F.K.; Sousa, A.O.; Owens, M.; Danielsson, D.; Nahmias, A.J.; Gold, B.D. Helicobacter pylori Prevalence among Indigenous Peoples of South America. J. Infect. Dis. 2002, 186, 1131–1137. [Google Scholar] [CrossRef] [Green Version]
- Tveit, A.H.; Bruce, M.G.; Bruden, D.L.; Morris, J.; Reasonover, A.; Hurlburt, D.A.; Hennessy, T.W.; McMahon, B. Alaska Sentinel Surveillance Study of Helicobacter pylori Isolates from Alaska Native Persons from 2000 to 2008. J. Clin. Microbiol. 2011, 49, 3638–3643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- US EPA, R. 09. Providing Safe Drinking Water in Areas with Abandoned Uranium Mines. Available online: https://www.epa.gov/navajo-nation-uranium-cleanup/providing-safe-drinking-water-areas-abandoned-uranium-mines (accessed on 19 June 2020).
- Ibrahim, A.; Morais, S.; Ferro, A.; Lunet, N.; Peleteiro, B. Sex-differences in the prevalence of Helicobacter pylori infection in pediatric and adult populations: Systematic review and meta-analysis of 244 studies. Dig. Liver Dis. 2017, 49, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Ferro, A.; Morais, S.; Pelucchi, C.; Dierssen-Sotos, T.; Martín, V.; López-Carrillo, L.; Malekzadeh, R.; Tsugane, S.; Hamada, G.S.; Hidaka, A.; et al. Sex differences in the prevalence of Helicobacter pylori infection: An individual participant data pooled analysis (StoP Project). Eur. J. Gastroenterol. Hepatol. 2019, 31, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2016. Cancer J. Clin. 2016, 66, 7–30. [Google Scholar] [CrossRef] [Green Version]
- De Martel, C.; Forman, D.; Plummer, M. Gastric Cancer. Gastroenterol. Clin. N. Am. 2013, 42, 219–240. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, L.J.; Brown, H.; Harris, R.B.; Oren, E. Population Knowledge, Attitude, and Practice Regarding Helicobacter pylori Transmission and Outcomes: A Literature Review. Front. Public Health 2017, 5, 144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, P.; Ma, M.-F.; Wang, W. Status of Helicobacter pylori infection among migrant workers in Shijiazhuang, China. Asian Pac. J. Cancer Prev. 2012, 13, 1167–1170. [Google Scholar] [CrossRef] [Green Version]
- Kinlacheeny, J.; Nez, R.A.; Foley, D.; Yazzie, D.; Francisco, S.; Lee, V.; Tracy, D. Navajo Population Profile 2010 U.S. Census; Navajo Epidemiology Center, Navajo Division of Health, Navajo Nation: Window Rock, AZ, USA, 2013. Available online: https://www.nec.navajo-nsn.gov/Portals/0/Reports/NN2010PopulationProfile.pdf (accessed on 2 January 2022).
| Overall n = 101 | UBT Positive n = 66 | UBT Negative n = 35 | ||
|---|---|---|---|---|
| Characteristics | n (%) | n (%) | n (%) | p‡ |
| Sex | 0.03 | |||
| Male | 41 (40.6) | 32 (48.5) | 9 (25.7) | |
| Female | 60 (59.4) | 34 (51.5) | 26 (74.3) | |
| Age, years | 0.46 | |||
| 18–29 | 11 (10.9) | 8 (12.1) | 3 (8.6) | |
| 30–49 | 26 (25.7) | 19 (28.8) | 7 (20.0) | |
| 50–64 | 24 (23.8) | 13 (19.7) | 11 (31.4) | |
| 65–79 | 30 (29.7) | 18 (27.3) | 12 (34.3) | |
| 80+ | 10 (9.9) | 9 (12.1) | 2 (5.7) | |
| Age, years, dichotomized | 0.22 | |||
| <50 | 37 (36.6) | 27 (40.9) | 10 (28.6) | |
| ≥50 | 64 (63.4) | 39 (59.1) | 25 (71.4) | |
| Education | 0.78 | |||
| <High School | 35 (34.7) | 22 (33.3) | 13 (37.7) | |
| ≥High School/GED | 64 (63.4) | 42 (63.6) | 22 (62.9) | |
| Missing | 2 (2.0) | 2 (3.0) | - | |
| Clinical History | ||||
| Ulcers | 4 (4.0) | 2 (3.0) | 2 (5.7) | 0.51 |
| Gallstones | 25 (23.8) | 14 (21.2) | 10 (28.6) | 0.41 |
| Gastroscopy/Endoscopy (ever) | 24 (24.0) | 12 (18.18) | 12 (34.29) | 0.08 |
| Water Sources | 0.02 | |||
| Regulated (piped, bottled) | 75 (74.3) | 43 (65.2) | 32 (91.4) | |
| Unregulated (spring, well) | 18 (17.8) | 16 (24.2) | 2 (5.7) | |
| Mixed | 8 (7.9) | 7 (10.6) | 1 (2.9) | |
| Have refrigerator in home | 94 (93.1) | 60 (90.9) | 34 (97.1) | 0.33 |
| Travel > 1 h for groceries | 86 (85.1) | 56 (84.8) | 30 (85.7) | 0.80 |
| Characteristics | UBT Positive Pos/Total (%) | Univariate | Model 1 ‡ | Model 2 § |
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | AOR (95% CI) | ||
| Overall | 66/101 (65.3) | |||
| Sex | ||||
| Female | 34/60 (56.7) | Ref | Ref | Ref |
| Male | 32/41 (78.0) | 2.72 (1.11–6.68) | 3.10 (1.10–8.72) | 3.26 (1.05–10.07) |
| Age years, dichotomized | ||||
| <50 | 27/37 (73.0) | Ref | Ref | Ref |
| ≥50 | 39/64 (60.9) | 0.58 (0.24–1.40) | 0.37 (0.13–1.10) | 0.36 (0.11–1.15) |
| Education | ||||
| <High School | 22/35 (62.9) | Ref | Ref | Ref |
| ≥High School/GED | 42/64 (65.6) | 1.13 (0.48–2.66) | 1.20 (0.40–3.61) | 1.20 (0.38–3.75) |
| Clinical History | ||||
| Ulcers | 2/4 (50.0) | 0.53 (0.07–3.83) | 0.29 (0.03–3.03) | 0.28 (0.02–3.23) |
| Gallstones | 14/24 (58.3) | 0.67 (0.26–1.73) | 1.44 (0.47–4.38) | 1.45 (0.46–4.61) |
| Water Sources | ||||
| Regulated | 43/75 (57.3) | Ref | Ref | Ref |
| Unregulated | 16/18 (88.9) | 5.95 (1.28–27.76) | 8.61 (1.45–51.05) | 9.32 (1.35–64.51) |
| Mixed | 7/8 (87.5) | 5.21 (0.61–44.48) | 5.97 (0.64–55.36) | 6.38 (0.60–67.70) |
| Overall n = 101 | UBT Positive n = 66 | UBT Negative n = 35 | ||
|---|---|---|---|---|
| n (%) | n (%) | n (%) | p | |
| Ever heard of H. pylori | 24 (23.8) | 12 (18.18) | 12 (34.29) | 0.07 |
| Any family told they have H. pylori | 11 (10.9) | 6 (9.09) | 5 (14.29) | 0.43 |
| Ever been tested for H. pylori | 13 (12.9) | 3 (4.54) | 10 (28.57) | <0.01 |
| Ever had a gastroscopy/endoscopy | 24 (24.0) | 12 (18.18) | 12 (34.29) | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harris, R.B.; Brown, H.E.; Begay, R.L.; Sanderson, P.R.; Chief, C.; Monroy, F.P.; Oren, E. Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona. Int. J. Environ. Res. Public Health 2022, 19, 797. https://doi.org/10.3390/ijerph19020797
Harris RB, Brown HE, Begay RL, Sanderson PR, Chief C, Monroy FP, Oren E. Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona. International Journal of Environmental Research and Public Health. 2022; 19(2):797. https://doi.org/10.3390/ijerph19020797
Chicago/Turabian StyleHarris, Robin B., Heidi E. Brown, Rachelle L. Begay, Priscilla R. Sanderson, Carmenlita Chief, Fernando P. Monroy, and Eyal Oren. 2022. "Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona" International Journal of Environmental Research and Public Health 19, no. 2: 797. https://doi.org/10.3390/ijerph19020797
APA StyleHarris, R. B., Brown, H. E., Begay, R. L., Sanderson, P. R., Chief, C., Monroy, F. P., & Oren, E. (2022). Helicobacter pylori Prevalence and Risk Factors in Three Rural Indigenous Communities of Northern Arizona. International Journal of Environmental Research and Public Health, 19(2), 797. https://doi.org/10.3390/ijerph19020797







