Trends in Smoking Prevalence and Intensity between 2010 and 2018: Implications for Tobacco Control in China
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Study Population
2.2. Indicators
2.3. Statistical Analysis
3. Results
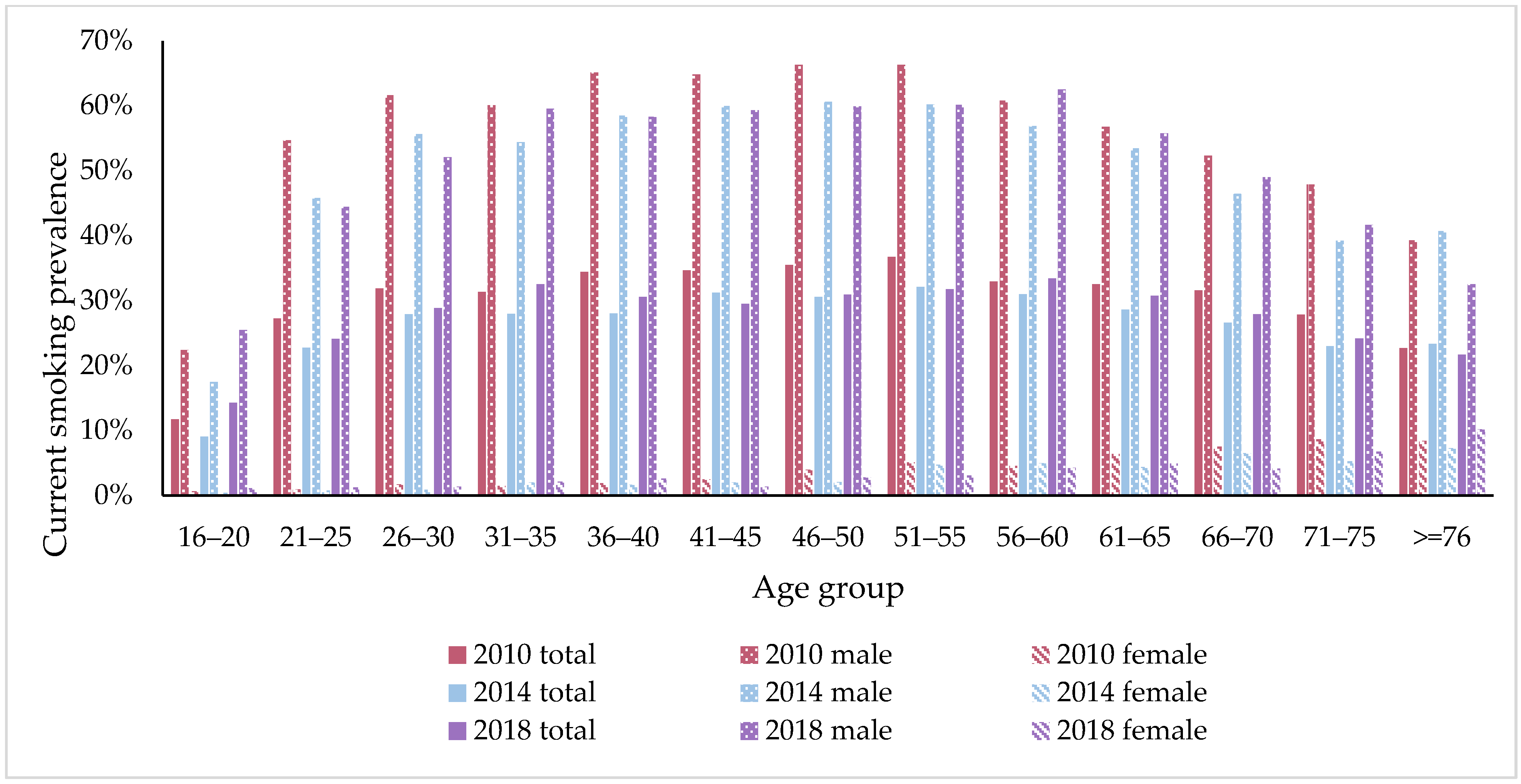
3.1. Smoking Prevalence
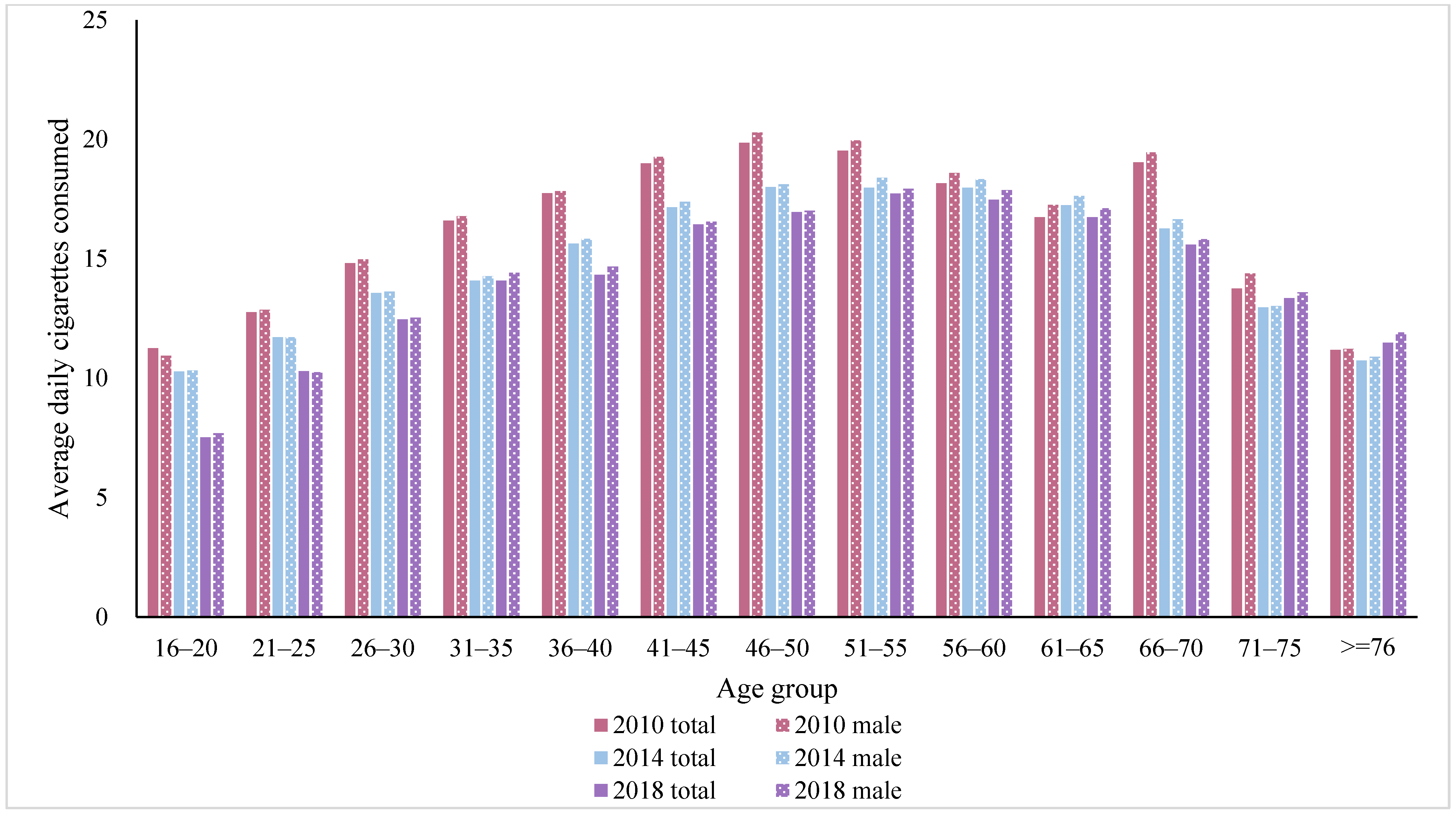
3.2. Smoking Intensity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CFPS | China Family Panel Studies |
| WHO | World Health Organization |
| FCTC | Framework Convention on Tobacco Control |
| NHS | National Health Service |
| ORs | Odds Ratios |
| RRs | Risk Ratios |
| CIs | Confidence Intervals |
| pp | percentage points |
Appendix A
| 2010 N (%) | 2012 N (%) | 2014 N (%) | 2016 N (%) | 2018 N (%) | |
|---|---|---|---|---|---|
| Individuals | 33,487 | 30,688 | 29,067 | 29,070 | 26,945 |
| Region | |||||
| East | 14,413 (43%) | 12,937 (42%) | 12,388 (43%) | 12,097 (42%) | 11,163 (42%) |
| Central | 9882 (30%) | 9124 (30%) | 8681 (30%) | 8457 (29%) | 7625 (28%) |
| West | 9192 (27%) | 8627 (28%) | 7998 (27%) | 8516 (29%) | 8157 (30%) |
| Residence | |||||
| Rural | 17,946 (54%) | 16,923 (55%) | 15,174 (52%) | 14,904 (51%) | 13,468 (50%) |
| Urban | 15,541 (46%) | 13,765 (45%) | 13,893 (48%) | 14,166 (49%) | 13,477 (50%) |
| Gender | |||||
| Female | 17,256 (51%) | 15,618 (51%) | 14,671 (50%) | 14,369 (49%) | 13,332 (49%) |
| Male | 16,231 (49%) | 15,070 (49%) | 14,396 (50%) | 14,701 (51%) | 13,613 (51%) |
| Education | |||||
| primary | 16,818 (50%) | 15,857 (52%) | 14,603 (50%) | 13,781 (47%) | 11,846 (44%) |
| middle | 14,373 (43%) | 12,613 (41%) | 12,275 (42%) | 12,449 (43%) | 12,196 (45%) |
| high | 2296 (7%) | 2218 (7%) | 2189 (8%) | 2840 (10%) | 2903 (11%) |
| Age, years | |||||
| 16–29 | 6535 (20%) | 6138 (20%) | 5539 (19%) | 5856 (20%) | 4713 (17%) |
| 30–39 | 5774 (17%) | 4787 (16%) | 4159 (14%) | 4271 (15%) | 4040 (15%) |
| 40–49 | 7739 (23%) | 7170 (23%) | 6492 (22%) | 5848 (20%) | 5045 (19%) |
| 50–59 | 6428 (19%) | 5675 (18%) | 5613 (19%) | 5593 (19%) | 5684 (21%) |
| 60–69 | 4274 (13%) | 4361 (14%) | 4719 (16%) | 4861 (17%) | 4827 (18%) |
| ≥70 | 2737 (8%) | 2557 (8%) | 2545 (9%) | 2641 (9%) | 2636 (10%) |
| Total | Women | Men | |
|---|---|---|---|
| Current Smoking | Risk Ratio (90% CIs) | Risk Ratio (90% CIs) | Risk Ratio (90% CIs) |
| Marital status | |||
| Unmarried | 1(ref) | 1(ref) | 1(ref) |
| Married or cohabited | 0.843 *** | 0.612 *** | 1.219 *** |
| (0.818–0.868) | (0.474–0.791) | (1.189–1.251) | |
| Divorced or widowed | 0.809 *** | 0.794 | 1.375 *** |
| (0.777–0.841) | (0.606–1.039) | (1.331–1.420) | |
| Educational level | |||
| Primary or below | 1(ref) | 1(ref) | 1(ref) |
| Secondary or high school | 1.140 *** | 0.733 *** | 0.924 *** |
| (1.124–1.157) | (0.671–0.800) | (0.913–0.935) | |
| College or above | 0.868 *** | 0.532 *** | 0.738 *** |
| (0.842–0.896) | (0.423–0.670) | (.719–0.757) | |
| Household income | |||
| Lower than average | 1(ref) | 1(ref) | 1(ref) |
| Equal to or higher than average | 0.943 *** | 0.674 *** | 1.013 * |
| (0.930–0.956) | (0.622–0.731) | (1.001–1.025) | |
| Work type | |||
| Unemployed | 1(ref) | 1(ref) | 1(ref) |
| Self employed | 1.442 *** | 0.855 *** | 1.169 *** |
| (1.415–1.471) | (0.786–0.931) | (1.150–1.189) | |
| Employed by others | 1.826 *** | 0.759 *** | 1.262 *** |
| (1.790–1.863) | (0.672–0.857) | (1.240–1.284) | |
| Current drinker | |||
| No | 1(ref) | 1(ref) | 1(ref) |
| Yes | 2.475 *** | 3.485 *** | 1.255 *** |
| (2.445–2.507) | (3.144–3.863) | (1.241–1.268) | |
| Physical activity | |||
| No | 1(ref) | 1(ref) | 1(ref) |
| Yes | 0.951 *** | 0.955 | 0.905 *** |
| (0.938–0.965) | (0.887–1.028) | (0.895–0.916) |
References
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 338, 1659–1724. [Google Scholar] [CrossRef] [Green Version]
- Yang, G.H.; Li, Q.A.; Wang, C.X.; Hsia, J.; Yang, Y.; Xiao, L.; Yang, J.; Zhao, L.H.; Zhang, J.; Xie, L. Findings from 2010 Global Adult Tobacco Survey: Implementation of MPOWER Policy in China. Biomed. Environ. Sci. 2010, 23, 422–429. [Google Scholar] [CrossRef]
- The Political Mapping of China’s Tobacco Industry and Anti-Smoking Campaign. Available online: https://www.brookings.edu/wp-content/uploads/2016/06/25-china-tobacco-li.pdf (accessed on 28 November 2021).
- Statistical Bulletin on National Economic and Social Development in 2010. Available online: http://www.stats.gov.cn/tjsj/tjgb/ndtjgb/qgndtjgb/201102/t20110228_30025.html (accessed on 28 November 2021). (In Chinese)
- Yang, G.; Kong, L.; Zhao, W.; Wan, X.; Zhai, Y.; Chen, L.C.; Koplan, J.P. Emergence of chronic non-communicable diseases in China. Lancet 2008, 372, 1697–1705. [Google Scholar] [CrossRef]
- The Bill China Cannot Afford: Health, Economic and Social Costs of China’s Tobacco Epidemic. Available online: https://www.cn.undp.org/content/china/en/home/library/democratic_governance/the-bill-china-cannot-afford--health-economic-and-social-costs-o.html (accessed on 28 November 2021).
- CHINA: 12th Five-Year Plan (2011–2015) for National Economic and Social Development. Available online: http://www.gov.cn/2011lh/content_1825838.htm (accessed on 28 November 2021). (In Chinese)
- Hu, T.W.; Zhang, X.L.; Zheng, R. China has raised the tax on cigarettes: What’s next? Tob. Control 2016, 25, 609–611. [Google Scholar] [CrossRef]
- Healthy China 2030 Plan Outline. Available online: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (accessed on 28 November 2021).
- Wang, N.; Feng, Y.J.; Bao, H.L.; Cong, S.; Fan, J.; Wang, B.H.; Fang, L.W. Research on smoking situation among Chinese aged over 40 in 2014. Chin. J. Epidemiol. 2018, 39, 551–556. (In Chinese) [Google Scholar]
- Chen, Y.Y.; Zhu, L.P.; Yan, W.; Liu, J.; Ji, L.; Xu, Y. Research on current smoking and smoking cessation among adults in Jiangxi in 2013. Chin. J. Epidemiol. 2017, 38, 577–582. (In Chinese) [Google Scholar]
- Gao, J.N.; Zheng, P.P.; Gao, J.L.; Chapman, S.; Fu, H. Workplace smoking policies and their association with male employees’ smoking behaviours: A cross-sectional survey in one company in China. Tob. Control 2011, 20, 131–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, Y.T.; Ji, Y.; Dong, H.B.; Chang, C. The prevalence of smoking, second-hand smoke exposure, and knowledge of the health hazards of smoking among internal migrants in 12 provinces in China: A cross-sectional analysis. BMC Public Health 2018, 18, 655. [Google Scholar] [CrossRef] [PubMed]
- He, H.J.; Pan, L.; Cui, Z.; Sun, J.X.; Yu, C.D.; Cao, Y.J.; Wang, Y.; Shan, G.L. Smoking Prevalence, Patterns, and Cessation Among Adults in Hebei Province, Central China: Implications From China National Health Survey (CNHS). Front Public Health 2020, 8, 177. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Report on Trends in Prevalence of Tobacco Use 2000–2025, Fourth Edition. Available online: https://www.who.int/publications/i/item/9789240039322 (accessed on 28 November 2021).
- WHO Report on the Global Tobacco Epidemic, 2021: Addressing New and Emerging Products. Available online: https://www.who.int/publications/i/item/9789240032095 (accessed on 28 November 2021).
- Qian, J.C.; Cai, M.; Gao, J.; Tang, S.L.; Xu, L.; Critchley, J.A. Trends in smoking and quitting in China from 1993 to 2003: National Health Service Survey data. B World Health Organ. 2010, 88, 769–776. [Google Scholar] [CrossRef]
- Wang, M.H.; Luo, X.; Xu, S.B.; Liu, W.H.; Ding, F.F.; Zhang, X.X.; Wang, L.; Liu, J.; Hu, J.P.; Wang, W. Trends in smoking prevalence and implication for chronic diseases in China: Serial national cross-sectional surveys from 2003 to 2013. Lancet Resp. Med. 2019, 7, 35–45. [Google Scholar] [CrossRef]
- Li, S.S.; Meng, L.H.; Chiolero, A.; Ma, C.W.; Xi, B. Trends in smoking prevalence and attributable mortality in China, 1991–2011. Prev. Med. 2016, 93, 82–87. [Google Scholar] [CrossRef] [Green Version]
- Xie, Y.; Hu, J.W. An Introduction to the China Family Panel Studies (CFPS). Chin. Sociol. Rev. 2014, 47, 3–29. [Google Scholar]
- Lin, H.X.; Chang, C.; Liu, Z.; Tan, H.Q. The effect of the presence of children on adult smoking behaviour: Empirical evidence based on China family panel studies. BMC Public Health 2020, 20, 1448. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.D.; Dong, Y.Q.; Liu, X.H.; Zhang, L.X.; Bai, Y.L.; Hagist, S. The More Educated, the Healthier: Evidence from Rural China. Int. J. Environ. Res. Public Health 2018, 15, 2848. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.L.; Mao, Z.Z.; He, G.; Hu, Q.T. Does smoking impact trust in physicians and satisfaction with the health system in China? Tob. Induc. Dis. 2021, 19, 6. [Google Scholar] [CrossRef] [PubMed]
- Global Adult Tobacco Survey 2010. Available online: https://extranet.who.int/ncdsmicrodata/index.php/catalog/252/related-materials (accessed on 28 November 2021).
- Global Adult Tobacco Survey 2018. Available online: https://www.tobaccofreekids.org/assets/global/pdfs/en/GATS_China_2018_FactSheet.pdf (accessed on 28 November 2021).
- Adult Smoking Habits in the UK: 2015. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2015 (accessed on 28 November 2021).
- Jamal, A.; King, B.A.; Neff, L.J.; Whitmill, J.; Babb, S.D.; Graffunder, C.M. Current Cigarette Smoking Among Adults—United States, 2005–2015. Mmwr Morbid. Mortal W 2016, 65, 1205–1211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Intarut, N.; Pukdeesamai, P. The prevalence of secondhand smoke exposure and related factors among schoolchildren in Northeast Thailand. F1000 Res. 2020, 9, 1158. [Google Scholar] [CrossRef] [PubMed]
- Cruvinel, E.; Liebman, E.; Leite, I.; Hu, J.X.; Richter, K.P. Prevalence of smoking, quit attempts and access to cessation treatment among adults with mental illness in Brazil: A cross-sectional analysis of a National Health Survey. BMJ Open 2020, 10, e033959. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.Y. Research on Chinese Tobacco Control Regulations. Master’s Thesis, Northwest Normal University, Lanzhou, China, May 2021. (In Chinese). [Google Scholar]
- Cigarette Package Health Warnings: International Status Report. Available online: http://www.tobaccofreekids.org/content/press_office/2014/2014_10_14_health_labels.pdf (accessed on 28 November 2021).
- Thrasher, J.F.; Hammond, D.; Fong, G.T.; Arillo-Santillan, E. Smokers’ reactions to cigarette package warnings with graphic imagery and with only text: A comparison between Mexico and Canada. Salud Publica Mexico 2007, 49, S233–S240. [Google Scholar] [CrossRef] [Green Version]
- Azagba, S.; Sharaf, M.F. The Effect of Graphic Cigarette Warning Labels on Smoking Behavior: Evidence from the Canadian Experience. Nicotine Tob. Res. 2013, 15, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Vardavas, C.I.; Connolly, G.; Karamanolis, K.; Kafatos, A. Adolescents perceived effectiveness of the proposed European graphic tobacco warning labels. Eur. J. Public Health 2009, 19, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Marsh, L.; Cameron, C.; Quigg, R.; Hoek, J.; Doscher, C.; McGee, R.; Sullivan, T. The impact of an increase in excise tax on the retail price of tobacco in New Zealand. Tob. Control 2016, 25, 458–463. [Google Scholar] [CrossRef] [PubMed]
- Chaloupka, F.L.; Yurekli, A.; Fong, G.T. Tobacco taxes as a tobacco control strategy. Tob. Control 2012, 21, 172–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, R.; Wang, Y.; Hua, X.; Marquez, P.V. Cigarette Affordability in China, 2001–2016; OKR: Washington, DC, USA, 2016. [Google Scholar]
- Blakely, T.; Gartner, C. Tobacco taxes have mixed effects on socioeconomic disparities. Lancet Public Health 2019, 4, E595–E596. [Google Scholar] [CrossRef] [Green Version]
- Hirono, K.T.; Smith, K.E. Australia’s $40 per pack cigarette tax plans: The need to consider equity. Tob. Control 2018, 27, 229–233. [Google Scholar] [CrossRef] [Green Version]
- Verguet, S.; Tarr, G.; Gauvreau, C.L.; Mishra, S.; Jha, P.; Liu, L.R.; Xiao, Y.; Qiu, Y.P.; Zhao, K. Distributional benefits of tobacco tax and smoke-free workplaces in China: A modeling study. J. Glob. Health 2017, 7, 020701. [Google Scholar] [CrossRef]
- Bask, M.; Melkersson, M. Rationally addicted to drinking and smoking? Appl. Econ. 2004, 36, 373–381. [Google Scholar] [CrossRef]
- Pierani, P.; Tiezzi, S. Addiction and interaction between alcohol and tobacco consumption. Empir Econ. 2009, 37, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Wang, Q.; Shen, J.J.; Sotero, M.; Li, C.A.; Hou, Z.Y. Income, occupation and education: Are they related to smoking behaviors in China? PLoS ONE 2018, 13, e0192571. [Google Scholar] [CrossRef] [Green Version]
- Kvaavik, E.; Rise, J. How Do Impulsivity and Education Relate to Smoking Initiation and Cessation Among Young Adults? J. Stud. Alcohol Drugs 2012, 73, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.O.; Gao, M.J.; Ryff, C.D. Conscientiousness and Smoking: Do Cultural Context and Gender Matter? Front. Psychol. 2020, 11, 1593. [Google Scholar] [CrossRef]
- Pan, Z.F. Socioeconomic predictors of smoking and smoking frequency in urban China: Evidence of smoking as a social function. Health Promot. Int. 2004, 19, 309–315. [Google Scholar] [CrossRef]
- Ma, S.J.; Wang, J.F.; Mei, C.Z.; Xu, X.F.; Yang, G.H. Passive smoking in China: Contributing factors and areas for future interventions. Biomed. Environ. Sci. 2007, 20, 420–425. [Google Scholar] [PubMed]
- He, G.Y.; Lin, X.S.; Ju, G.D.; Chen, Y.S. Mapping Public Concerns of Electronic Cigarettes in China. J. Psychoact. Drugs 2020, 52, 13–19. [Google Scholar] [CrossRef] [PubMed]
| Current Smoker | 2010 | 2012 | 2014 | 2016 | 2018 | Difference | ||
|---|---|---|---|---|---|---|---|---|
| Weighted Proportion (90% CI) | Weighted Proportion (90% CI) | Weighted Proportion (90% CI) | Weighted Proportion (90% CI) | Weighted Proportion (90% CI) | 2010–2014 | 2014–2018 | 2010–2018 | |
| Individuals | 30.39% (29.47–31.31) | 28.21% (27.34–29.08) | 27.04% (25.94–28.14) | 26.31% (25.38–27.25) | 28.69% (27.69–29.69) | −0.033 *** | 0.016 *** | −0.017 *** |
| Gender | ||||||||
| Female | 3.21% (2.50–3.93) | 2.93% (2.34–3.52) | 2.75% (2.16–3.34) | 3.52% (2.78–4.26) | 3.02% (2.39–3.65) | −0.005 ** | 0.003 | −0.002 |
| Male | 56.76% (55.33–58.19) | 55.00% (53.52–56.47) | 51.94% (49.98–53.90) | 48.57% (47.07–50.06) | 53.12% (51.44–54.79) | −0.048 *** | 0.012 | −0.036 *** |
| Region | ||||||||
| Eastern | 28.47% (27.28–29.65) | 27.26% (26.05–28.49) | 24.80% (23.45–26.16) | 25.17% (23.75–26.59) | 26.94% (25.56–28.31) | −0.037 *** | 0.021 *** | −0.015 ** |
| Central | 30.37% (28.94–31.81) | 28.34% (26.70–29.98) | 27.09% (26.12–28.06) | 26.79% (25.24–28.34) | 28.64% (27.20–30.07) | −0.033 *** | 0.015 * | −0.017 * |
| Western | 33.14% (31.22–35.06) | 29.54% (27.77–31.32) | 30.67% (28.59–32.75) | 27.49% (25.72–29.25) | 31.43% (29.17–33.69) | −0.025 ** | 0.008 | −0.017 |
| Residence | ||||||||
| Rural | 32.28% (30.95–33.61) | 29.10% (27.81–30.38) | 28.89% (27.41–30.37) | 28.26% (26.98–29.55) | 30.05% (28.59–31.51) | −0.034 *** | 0.012 | −0.022 *** |
| Urban | 28.52% (27.40–29.64) | 27.42% (26.37–28.48) | 25.80% (24.54–27.06) | 25.04% (23.96–26.13) | 27.81% (26.75–28.87) | −0.027 *** | 0.020 *** | −0.007 |
| Education | ||||||||
| Primary or below | 30.48% (29.10–31.87) | 27.93% (26.72–29.14) | 27.44% (26.00–28.88) | 26.43% (25.15–27.71) | 27.90% (26.36–29.44) | −0.030 *** | 0.005 | −0.026 *** |
| Secondary or high school | 31.09% (30.13–32.05) | 29.62% (28.59–30.65) | 27.68% (26.54–28.82) | 27.53% (26.43–28.63) | 31.54% (30.54–32.55) | −0.034 *** | 0.039 *** | 0.005 |
| College or above | 25.67% (23.59–27.75) | 22.82% (20.72–24.93) | 22.19% (19.87–24.52) | 19.02% (16.91–21.13) | 21.44% (19.40–23.49) | −0.035 ** | −0.008 | −0.042 ** |
| Age, years | ||||||||
| 16–29 | 22.96% (21.46–24.47) | 20.05% (18.71–21.40) | 19.74% (18.30–21.19) | 17.20% (15.93–18.47) | 22.22% (20.61–23.84) | −0.032 *** | 0.025 ** | −0.007 |
| 30–39 | 32.66% (31.22–34.10) | 30.44% (28.83–32.05) | 27.91% (26.09–29.74) | 29.71% (27.99–31.43) | 31.71% (29.77–33.64) | −0.048 *** | 0.038 *** | −0.01 |
| 40–49 | 34.85% (33.48–36.22) | 32.14% (30.75–33.52) | 30.76% (29.12–32.41) | 29.70% (28.09–31.31) | 30.17% (28.50–31.84) | −0.041 *** | −0.006 | −0.047 *** |
| 50–59 | 35.65% (34.27–37.03) | 33.92% (32.49–35.35) | 31.46% (29.69–33.23) | 30.67% (28.92–32.43) | 32.15% (30.33–33.97) | −0.042 *** | 0.007 | −0.035 *** |
| 60–69 | 31.73% (30.09–33.37) | 29.70% (28.23–31.17) | 28.56% (26.86–30.26) | 29.11% (27.34–30.87) | 29.88% (28.38–31.38) | −0.032 ** | 0.013 | −0.019 |
| ≥70 | 26.00% (23.52–28.48) | 23.61% (21.15–26.07) | 23.46% (20.85–26.06) | 22.19% (19.77–24.60) | 24.21% (22.19–26.22) | −0.025 | 0.007 | −0.018 |
| Total | Women | Men | |
|---|---|---|---|
| Current Smoking | Odds Ratio (90% CI) | Odds Ratio (90% CI) | Odds Ratio (90% CI) |
| Marital status | |||
| Unmarried | 1(ref) | 1(ref) | 1(ref) |
| Married or cohabited | 0.746 *** | 0.602 *** | 1.431 *** |
| (0.714~0.779) | (0.475~0.764) | (1.360~1.505) | |
| Divorced or widowed | 0.697 *** | 0.796 | 1.943 *** |
| (0.657~0.739) | (0.618~1.026) | (1.802~2.096) | |
| Educational level | |||
| Primary or below | 1(ref) | 1(ref) | 1(ref) |
| Secondary or high school | 1.248 *** | 0.720 *** | 0.822 *** |
| (1.218~1.278) | (0.656~0.790) | (0.798~0.847) | |
| College or above | 0.809 *** | 0.523 *** | 0.512 *** |
| (0.774~0.846) | (0.413~0.663) | (0.486~0.540) | |
| Household income | |||
| Lower than average | 1(ref) | 1(ref) | 1(ref) |
| Equal to or higher than average | 0.909 *** | 0.659 *** | 1.033 * |
| (0.889~0.930) | (0.606~0.716) | (1.004~1.064) | |
| Work type | |||
| Unemployed | 1(ref) | 1(ref) | 1(ref) |
| Self employed | 1.694 *** | 0.847 *** | 1.381 *** |
| (1.646~1.744) | (0.774~0.927) | (1.330~1.435) | |
| Employed by others | 2.517 *** | 0.749 *** | 1.654 *** |
| (2.440~2.597) | (0.660~0.852) | (1.590–1.722) | |
| Current drinker | |||
| No | 1(ref) | 1(ref) | 1(ref) |
| Yes | 5.141 *** | 3.997 *** | 1.835 *** |
| (5.009~5.276) | (3.551~4.499) | (1.780~1.890) | |
| Physical activity | |||
| No | 1(ref) | 1(ref) | 1(ref) |
| Yes | 0.922 *** | 0.954 | 0.796 *** |
| (0.902~0.943) | (0.883~1.030) | (0.774~0.818) | |
| Observations | 146,694 | 74,457 | 72,237 |
| Number of Average Daily Cigarettes | 2010 | 2012 | 2014 | 2016 | 2018 | Difference | ||
|---|---|---|---|---|---|---|---|---|
| Weighted Means (90% CI) | Weighted Means (90% CI) | Weighted Means (90% CI) | Weighted Means (90% CI) | Weighted Means (90% CI) | 2010–2014 | 2014–2018 | 2010–2018 | |
| Individuals | 16.96 (16.55–17.36) | 16.19 (15.78–16.60) | 15.83 (15.42–16.24) | 15.50 (15.07–15.94) | 15.12 (14.76–15.48) | −1.125 *** | −0.710 *** | −1.836 *** |
| Gender | ||||||||
| Female | 12.14 (11.27–13.01) | 13.03 (12.09–13.96) | 12.12 (10.97–13.28) | 10.95 (9.86–12.04) | 11.27 (10.20–12.34) | −0.013 | −0.855 | −0.869 |
| Male | 17.21 (16.81–17.63) | 16.37 (15.96–16.78) | 16.03 (15.62–16.44) | 15.83 (15.39–16.26) | 15.33 (14.96–15.69) | −1.187 *** | −0.705 *** | −1.892 *** |
| Region | – | |||||||
| East | 16.74 (16.02–17.45) | 16.39 (16.05–16.74) | 16.09 (15.49–16.69) | 15.97 (15.35–16.59) | 15.36 (14.78–15.95) | −0.652 * | −0.722 ** | −1.374 *** |
| Central | 16.93 (16.25–17.60) | 16.61 (15.90–17.32) | 16.37 (15.71– 17.03) | 16.00 (15.54–16.47) | 15.53 (15.06–15.99) | −0.555 | −0.845 ** | −1.401 *** |
| West | 17.26 (16.53–17.98) | 15.37 (14.45–16.28) | 14.86 (14.00–15.71) | 14.21 (13.71–14.71) | 14.35 (13.73–14.97) | −2.398 *** | −0.508 | −2.906 *** |
| Residence | ||||||||
| Rural | 17.54 (16.98–18.08) | 16.92 (16.34–17.49) | 16.10 (15.53–16.66) | 15.67 (15.18–16.17) | 15.23 (14.72–15.73) | −1.441 *** | −0.869 *** | −2.310 *** |
| Urban | 16.31 (15.85–16.78) | 15.50 (15.07–15.93) | 15.63 (15.15–16.11) | 15.38 (14.79–15.96) | 15.04 (14.60–15.49) | −0.681 * | −0.586 * | −1.267 *** |
| Education | ||||||||
| Primary or below | 17.52 (16.99–18.06) | 17.12 (16.50–17.74) | 16.58 (15.98–17.18) | 16.15 (15.47–16.82) | 16.46 (15.82–17.10) | −0.945 ** | −0.121 | −1.066 *** |
| Secondary or high school | 16.84 (16.28–17.40) | 15.68 (15.22–16.13) | 15.78 (15.31–16.24) | 15.22 (14.76–15.69) | 14.79 (14.37–15.22) | −1.062 *** | −0.986 *** | −2.048 *** |
| College or above | 13.92 (13.05–14.78) | 13.80 (12.95–14.64) | 11.97 (11.20–12.75) | 12.27 (11.51–13.03) | 12.19 (11.41–12.97) | −1.943 *** | 0.219 | −1.724 *** |
| Age, years | ||||||||
| 16–29 | 13.24 (12.39–14.09) | 11.93 (11.27–12.59) | 12.25 (11.73–12.77) | 10.94 (10.37–11.52) | 10.51 (9.98–11.04) | −0.990 ** | −1.739 *** | −2.729 *** |
| 30–39 | 17.08 (16.44–17.73) | 16.05 (15.48–16.63) | 14.77 (14.23–15.31) | 14.32 (13.80–14.84) | 13.97 (13.42–14.52) | −2.309 *** | −0.802 * | −3.110 *** |
| 40–49 | 19.18 (18.45–19.92) | 17.88 (17.32–18.45) | 17.38 (16.68–18.09) | 16.58 (15.98–17.18) | 16.27 (15.61–16.93) | −1.800 *** | −1.117 ** | −2.917 *** |
| 50–59 | 18.59 (17.78–19.40) | 18.75 (18.06–19.44) | 18.18 (17.40–18.95) | 17.90 (17.24–18.56) | 17.88 (17.20–18.56) | −0.415 | −0.297 | −0.712 |
| 60–69 | 18.24 (16.88–19.61) | 16.45 (15.65–17.25) | 16.99 (16.04–17.95) | 16.82 (15.99–17.66) | 16.49 (15.83–17.15) | −1.254 | −0.503 | −1.757 * |
| ≥70 | 13.19 (12.19–14.18) | 13.39 (12.54–14.23) | 11.94 (10.98–12.90) | 12.69 (11.48–13.90) | 12.93 (12.03–13.83) | −1.250 * | 0.992 | −0.257 |
| Number of Average Daily Cigarettes | Total | Women | Men |
|---|---|---|---|
| Coef. (90% CI) | Coef. (90% CI) | Coef. (90% CI) | |
| Marital status | |||
| Unmarried | |||
| Married or cohabited | −0.025 | −1.824 | 0.023 |
| (−0.406~0.356) | (−3.714~0.066) | (−0.367~0.412) | |
| Divorced or widowed | 0.384 | −1.182 | 0.66 * |
| (−0.142~0.909) | (−3.188~0.824) | (0.103~1.218) | |
| Educational level | |||
| Primary or below | |||
| Secondary or high school | −0.739 *** | −0.858 * | −0.932 *** |
| (−0.949~−0.530) | (−1.669~−0.0478) | (−1.149~−0.716) | |
| College or above | −2.713 *** | −1.69 | −2.932 *** |
| (−3.128~−2.299) | (−3.772~0.393) | (−3.356~−2.508) | |
| Household income | |||
| Lower than average | |||
| Equal to or higher than average | 0.515 *** | 0.163 | 0.513 *** |
| (0.312~0.718) | (−0.525~0.851) | (0.302~0.723) | |
| Work type | |||
| Unemployed | |||
| Self employed | 0.717 *** | −0.540 | 0.511 *** |
| (0.442~0.991) | (−1.323~0.243) | (0.222~0.800) | |
| Employed by others | 0.469 *** | −.385 | 0.135 |
| (0.176~0.761) | (−1.537~0.767) | (−0.171~0.440) | |
| Current drinker | |||
| No | |||
| Yes | 2.064 *** | 2.854 *** | 1.806 *** |
| (1.866~2.262) | (1.886~3.821) | (1.603~2.010) | |
| Physical activity | |||
| No | |||
| Yes | −1.429 *** | −0.836 ** | −1.473 *** |
| (−1.631~−1.227) | (−1.478~−0.194) | (−1.683~−1.263) | |
| Observations | 43,495 | 2,399 | 41,096 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, G.; Zhan, J.; Fu, H. Trends in Smoking Prevalence and Intensity between 2010 and 2018: Implications for Tobacco Control in China. Int. J. Environ. Res. Public Health 2022, 19, 670. https://doi.org/10.3390/ijerph19020670
Zhang G, Zhan J, Fu H. Trends in Smoking Prevalence and Intensity between 2010 and 2018: Implications for Tobacco Control in China. International Journal of Environmental Research and Public Health. 2022; 19(2):670. https://doi.org/10.3390/ijerph19020670
Chicago/Turabian StyleZhang, Guoting, Jiajia Zhan, and Hongqiao Fu. 2022. "Trends in Smoking Prevalence and Intensity between 2010 and 2018: Implications for Tobacco Control in China" International Journal of Environmental Research and Public Health 19, no. 2: 670. https://doi.org/10.3390/ijerph19020670
APA StyleZhang, G., Zhan, J., & Fu, H. (2022). Trends in Smoking Prevalence and Intensity between 2010 and 2018: Implications for Tobacco Control in China. International Journal of Environmental Research and Public Health, 19(2), 670. https://doi.org/10.3390/ijerph19020670





