Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust
Abstract
:1. Introduction
1.1. COVID-19 Vaccinations in the U.S.
1.2. Vaccine Hesitancy
1.3. Assessing Vaccine Hesitancy among Healthcare Workers and First Responders
1.4. Assessing EMS Vaccine Hesitancy
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. COVID-19 Vaccination Status
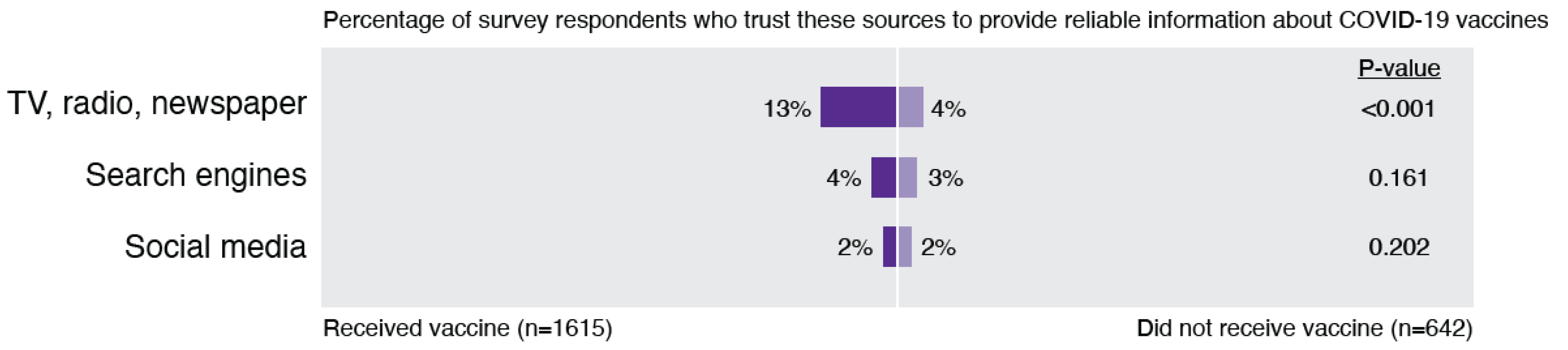
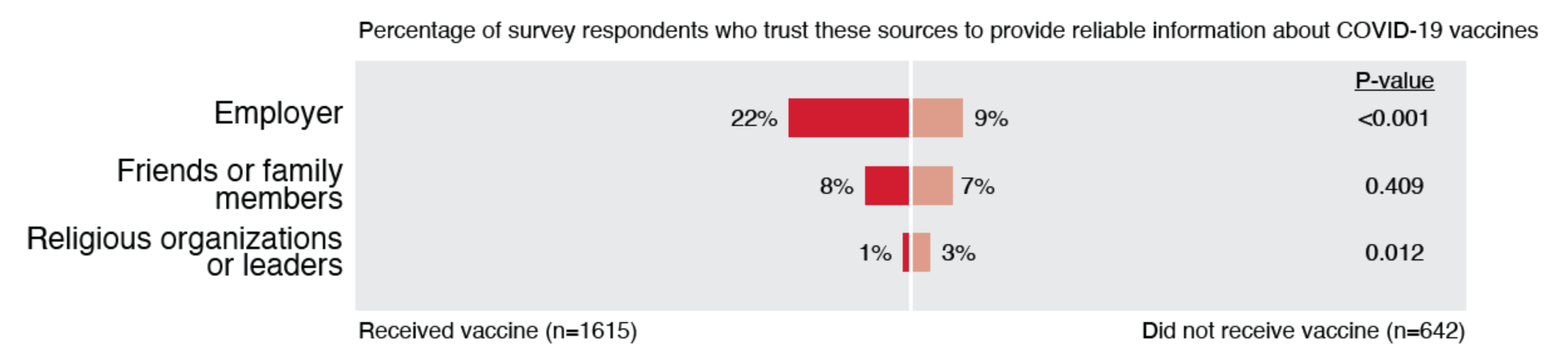
2.2.2. Trust in Information Sources
2.2.3. Open-Ended Comments
2.3. Analysis
3. Results
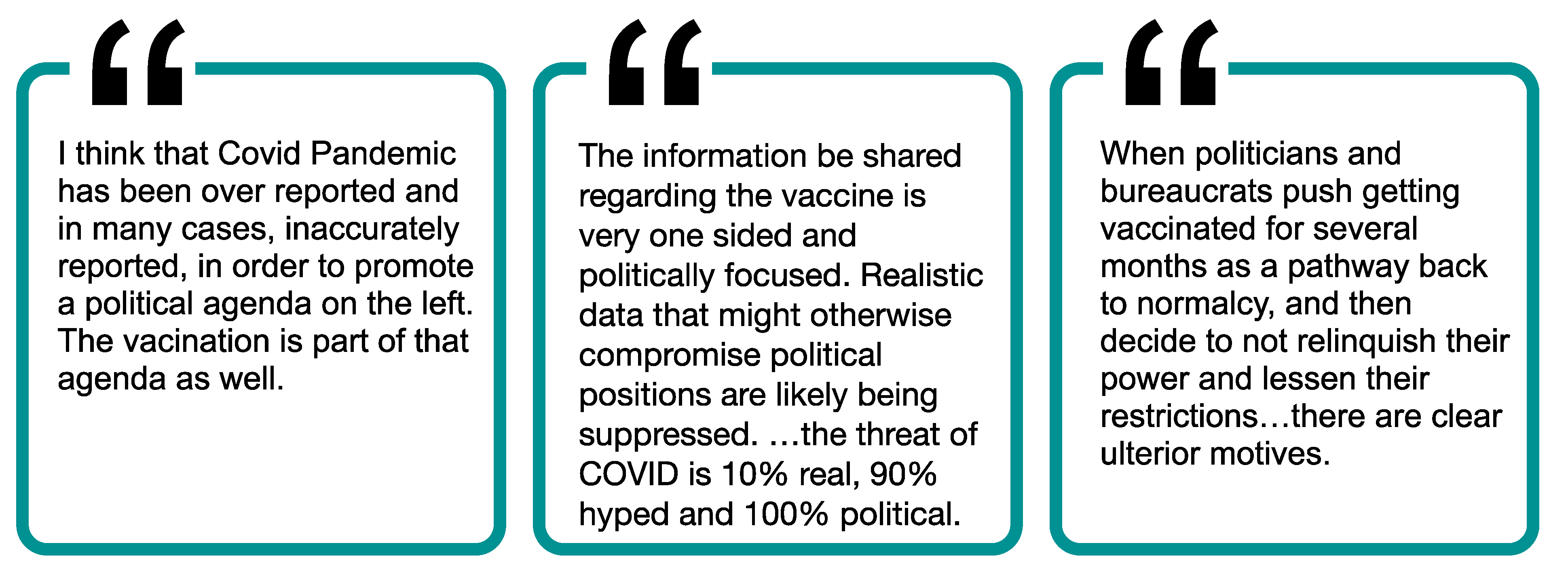
3.1. Theme 1: Low Trust in Government
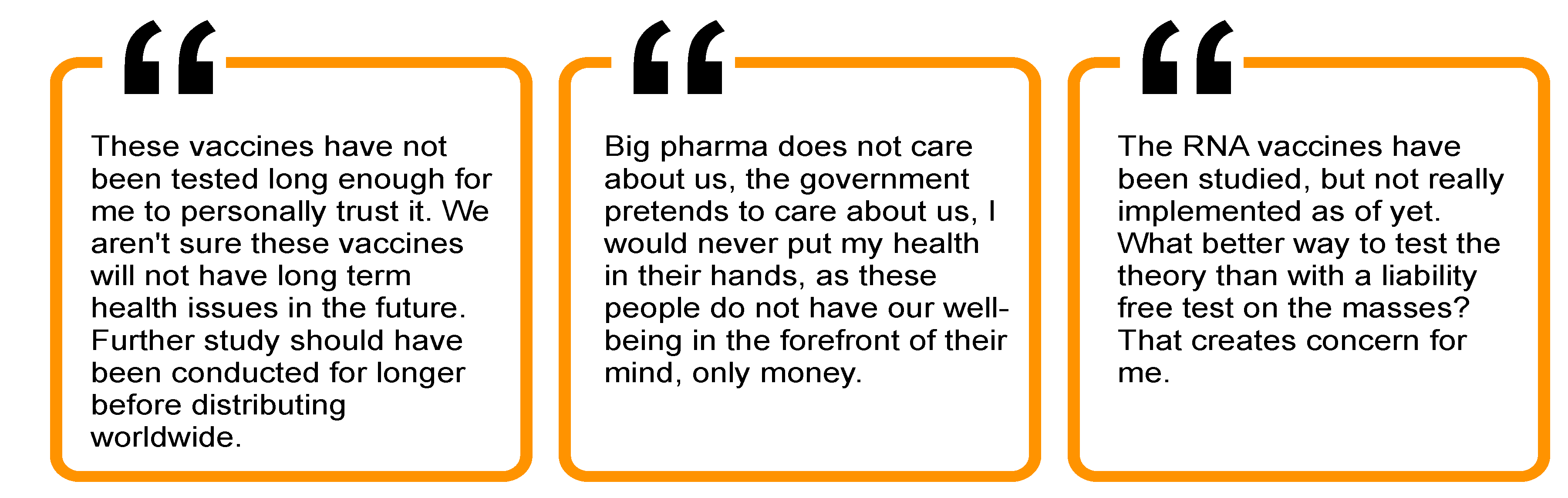
3.2. Theme 2: Mistrust in Healthcare and Medical Sources
3.3. Theme 3: Low Trust in Media
3.4. Theme 4: Low Trust in Employer and Community
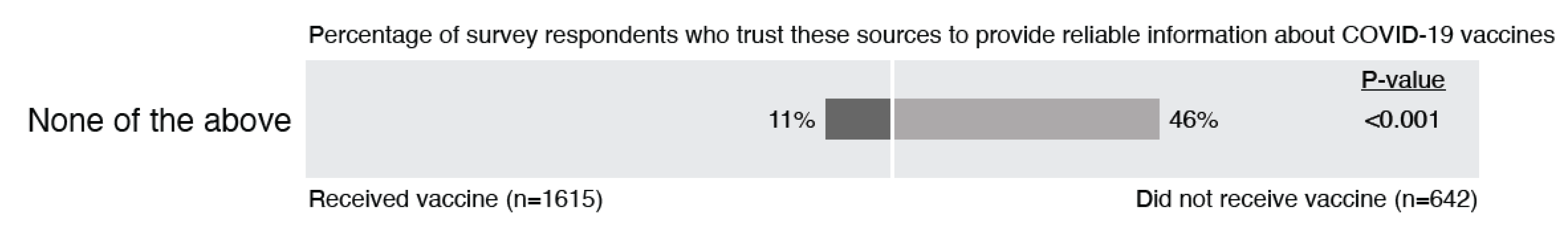
3.5. Theme 5: Many Trust No One
3.6. Additional Noteworthy Themes
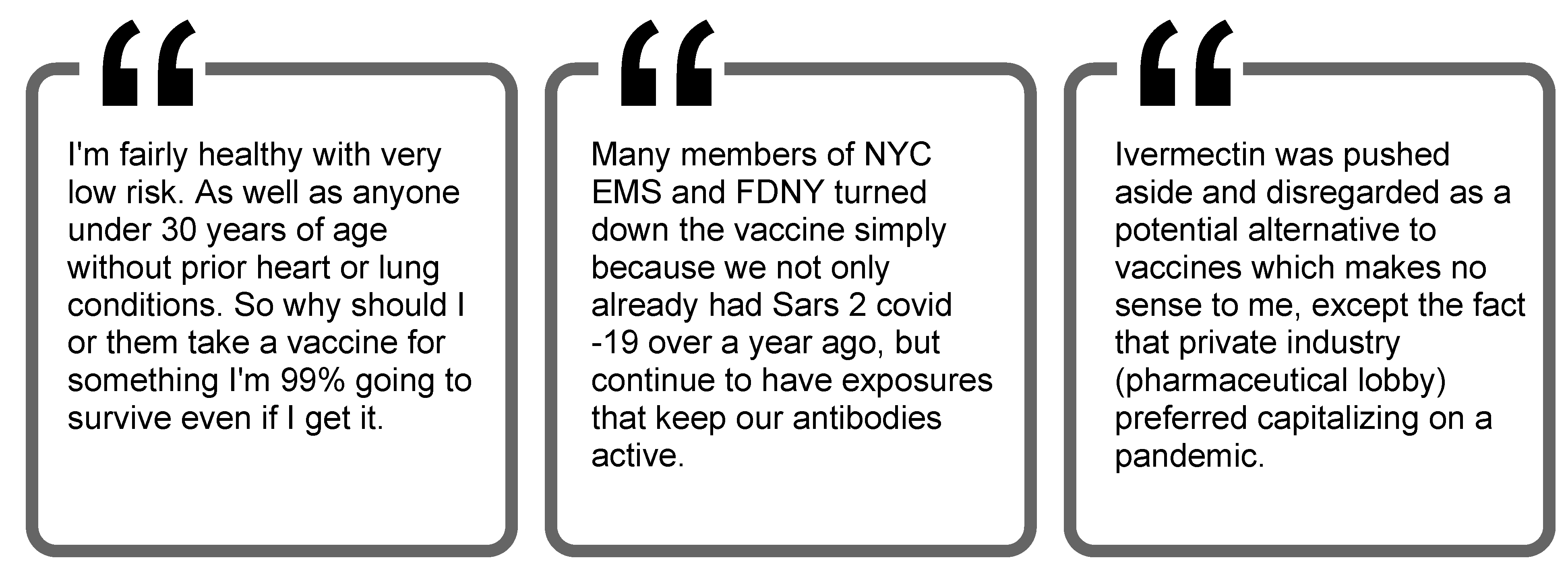
3.6.1. Some Individuals Trust in Other Options to Manage COVID-19 Rather Than the Vaccine
3.6.2. Many Argue for the Autonomy to Decide for Themselves
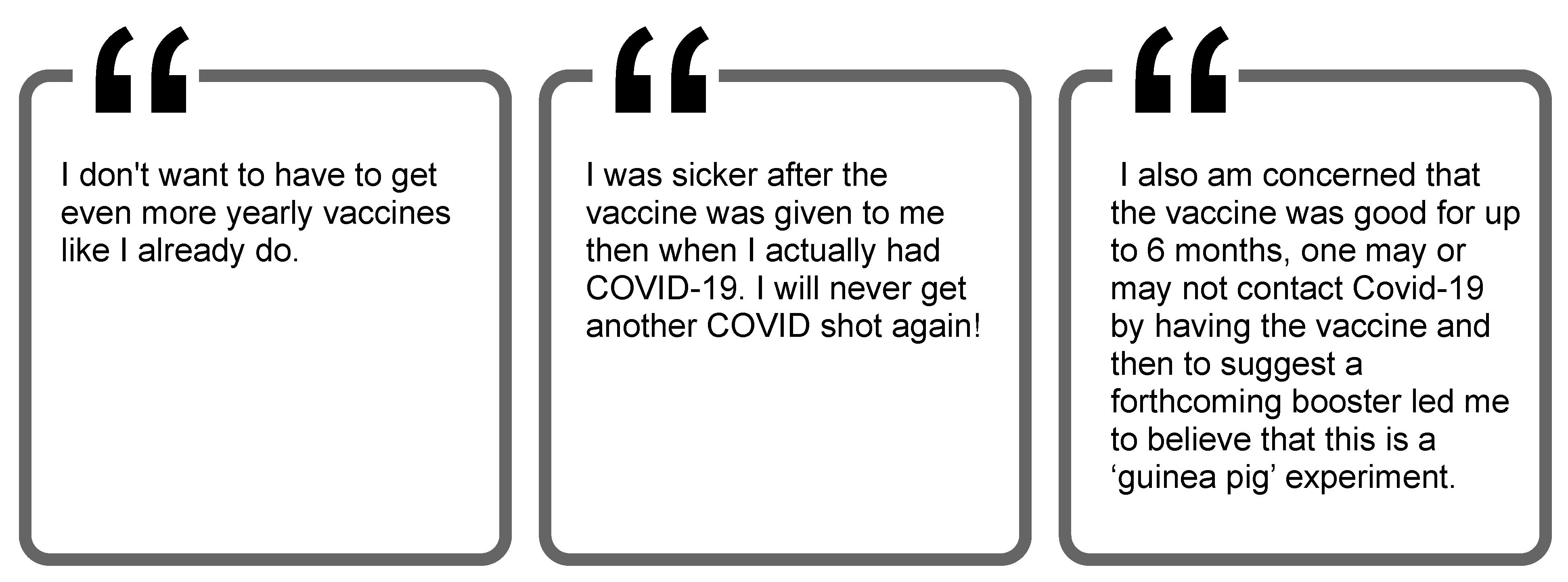
3.6.3. Negative Experiences with the Vaccine May Reduce Willingness for Booster Shots
4. Discussion
4.1. Reasons for Low Trust
4.2. Whom Do Individuals Trust?
4.3. Major Concerns of the Vaccine-Hesitant
4.4. Messaging to Improve Trust
4.5. Limitations
4.6. Final Thoughts
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Key Things to Know about COVID-19 Vaccines. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/keythingstoknow.html?s_cid=10493:covid%2019%20vaccination:sem.ga:p:RG:GM:gen:PTN:FY21 (accessed on 27 September 2021).
- World Health Organization. COVID-19 Vaccines. 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 27 September 2021).
- Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total (accessed on 20 September 2021).
- Mayo Clinic. U.S. COVID-19 Vaccine Tracker: See Your State’s Progress. 2021. Available online: https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker (accessed on 27 September 2021).
- Centers for Disease Control and Prevention. Delta Variant: What We Know about the Science. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/variants/delta-variant.html (accessed on 16 August 2021).
- Centers for Disease Control and Prevention. Variant Proportions. 2021. Available online: https://covid.cdc.gov/covid-data-tracker/#variant-proportions (accessed on 24 August 2021).
- Centers for Disease Control and Prevention. Science Brief: COVID-19 Vaccines and Vaccination. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/science/science-briefs/fully-vaccinated-people.html (accessed on 30 September 2021).
- MacDonald, N.E.; the SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- U.S. Food & Drug Administration. Comirnaty and Pfizer-BioNTech COVID-19 Vaccine. 2021. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/pfizer-biontech-covid-19-vaccine (accessed on 25 August 2021).
- Rural Health Information Hub. Rural COVID-19 Innovations: COVID-19 Vaccination. 2021. Available online: https://www.ruralhealthinfo.org/topics/covid-19/innovations/vaccination (accessed on 30 September 2021).
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. 2014. Available online: https://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf (accessed on 30 September 2021).
- Blendon, R.J.; Benson, J.M.; Hero, J.O. Public Trust in Physicians—U.S. Medicine in International Perspective. N. Engl. J. Med. 2014, 371, 1570–1572. [Google Scholar] [CrossRef] [Green Version]
- National Academies of Sciences, Engineering, and Medicine. Examining the Mistrust of Science: Proceedings of a Workshop—In Brief; National Academies Press: Seattle, WA, USA, 2017. [Google Scholar]
- Artiga, S.; Rae, M.; Claxton, G.; Garfield, R. Key Characteristics of Health Care Workers and Implications for COVID-19 Vaccination. 2021. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/key-characteristics-of-health-care-workers-and-implications-for-covid-19-vaccination/ (accessed on 30 September 2021).
- Berry, S.D.; Johnson, K.S.; Myles, L.; Herndon, L.; Montoya, A.; Fashaw, S.; Gifford, D. Lessons learned from frontline skilled nursing facility staff regarding COVID-19 vaccine hesitancy. J. Am. Geriatr. Soc. 2021, 69, 1140–1146. [Google Scholar] [CrossRef]
- National Association of State EMS Officials. 2020 National Emergency Medical Services Assessment. 2020. Available online: https://nasemso.org/wp-content/uploads/2020-National-EMS-Assessment_Reduced-File-Size.pdf (accessed on 30 September 2021).
- Nohl, A.; Afflerbach, C.; Lurz, C.; Brune, B.; Ohmann, T.; Weichert, V.; Zeiger, S.; Dudda, M. Acceptance of COVID-19 Vaccination among Front-Line Health Care Workers: A Nationwide Survey of Emergency Medical Services Personnel from Germany. Vaccines 2021, 9, 424. [Google Scholar] [CrossRef] [PubMed]
- Caban-Martinez, A.J.; Silvera, C.A.; Santiago, K.M.; Louzado-Feliciano, P.; Burgess, J.L.; Smith, D.L.; Jahnke, S.; Horn, G.P.; Graber, J.M. COVID-19 Vaccine Acceptability Among US Firefighters and Emergency Medical Services Workers: A Cross-Sectional Study. J. Occup. Environ. Med. 2021, 63, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Interim Considerations for COVID-19 Vaccination of Healthcare Personnel and Long-Term Care Facility Residents. 2020. Available online: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19/clinical-considerations.html (accessed on 16 August 2021).
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.M.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The advisory committee on immunization practices’ updated interim recommendation for allocation of COVID-19 vaccine—United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Evidence Table for COVID-19 Vaccines Allocation in Phases 1b and 1c of the Vaccination Program. 2020. Available online: https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/covid-19/evidence-table-phase-1b-1c.html (accessed on 16 August 2021).
- Department of Health and Human Services. Secretarial Directive on Eligibility to Receive COVID-19 Vaccines. 2021. Available online: https://www.hhs.gov/sites/default/files/secretarial-directive-eligibility-for-covid-19-vaccines.pdf (accessed on 16 August 2021).
- Brewer, M.B. In-group bias in the minimal intergroup situation: A cognitive-motivational analysis. Psychol. Bull. 1979, 86, 307–324. [Google Scholar] [CrossRef]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of COVID-19—preliminary report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef]
- Tufekci, Z. Why Telling People They Don’t Need Masks Backfired. The New York Times. 2020. Available online: https://www.nytimes.com/2020/03/17/opinion/coronavirus-face-masks.html (accessed on 30 September 2021).
- Dwyer, C.; Aubrey, A. CDC Now Recommends Americans Consider Wearing Cloth Face Coverings in Public. NPR. 2020. Available online: https://www.npr.org/sections/coronavirus-live-updates/2020/04/03/826219824/president-trump-says-cdc-now-recommends-americans-wear-cloth-masks-in-public (accessed on 27 September 2021).
- Ellis, R. Double Masking ‘Makes Common Sense,’ Fauci Says. WebMD. 2021. Available online: https://www.webmd.com/lung/news/20210126/double-masking-makes-common-sense-fauci-says (accessed on 30 September 2021).
- Victor, D.; Serviss, L.; Paybarah, A. In His Own Words, Trump on the Coronavirus and Masks. The New York Times. 2020. Available online: https://www.nytimes.com/2020/10/02/us/politics/donald-trump-masks.html (accessed on 30 September 2021).
- Chamberlain, S. Fauci Emails Show His Flip-Flopping on Wearing Masks to Fight COVID. New York Post. 2021. Available online: https://nypost.com/2021/06/03/fauci-emails-show-his-flip-flopping-on-wearing-masks-to-fight-covid/ (accessed on 30 September 2021).
- Gianola, S.; Jesus, T.S.; Bargeri, S.; Castellini, G. Characteristics of academic publications, preprints, and registered clinical trials on the COVID-19 pandemic. PLoS ONE 2020, 15, e0240123. [Google Scholar] [CrossRef]
- Sinha, N.; Balayla, G. Hydroxychloroquine and COVID-19. Postgrad. Med. J. 2020, 96, 550–555. [Google Scholar] [CrossRef] [Green Version]
- Meyerowitz, E.A.; Vannier, A.G.L.; Friesen, M.G.N.; Schoenfeld, S.; Gelfand, J.A.; Callahan, M.V.; Kim, A.Y.; Reeves, P.M.; Poznansky, M.C. Rethinking the role of hydroxychloroquine in the treatment of COVID-19. FASEB J. 2020, 34, 6027–6037. [Google Scholar] [CrossRef] [PubMed]
- Gregory, M.E.; Powell, J.R.; MacEwan, S.R.; Kurth, J.D.; Kenah, E.; Panchal, A.R.; McAlearney, A.S. COVID-19 vaccinations in EMS professionals: Prevalence and predictors. Prehosp. Emerg. Care 2021, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Myths and Facts about COVID-19 Vaccines. 2021. Available online: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/facts.html (accessed on 25 August 2021).
- Mayo Clinic Health System. COVID-19 Vaccine Myths Debunked. 2021. Available online: https://www.mayoclinichealthsystem.org/hometown-health/featured-topic/covid-19-vaccine-myths-debunked (accessed on 30 September 2021).
- Windsor, M. Three Things to Know About the Long-Term Side Effects of COVID Vaccines. UAB News. 2021. Available online: https://www.uab.edu/news/health/item/12143-three-things-to-know-about-the-long-term-side-effects-of-covid-vaccines (accessed on 30 September 2021).
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Crook, H.; Raza, S.; Nowell, J.; Young, M.; Edison, P. Long COVID—Mechanisms, risk factors, and management. BMJ 2021, 374, n1648. [Google Scholar] [CrossRef] [PubMed]
- Gorna, R.; MacDermott, N.; Rayner, C.; O’Hara, M.; Evans, S.; Agyen, L.; Nutland, W.; Rogers, N.; Hastie, C. Long COVID guidelines need to reflect lived experience. Lancet 2020, 397, 455–457. [Google Scholar] [CrossRef]
- Barda, N.; Dagan, N.; Ben-Shlomo, Y.; Kepten, E.; Waxman, J.; Ohana, R.; Hernán, M.A.; Lipsitch, M.; Kohane, I.; Netzer, D.; et al. Safety of the BNT162b2 mRNA COVID-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2021, 385, 1078–1090. [Google Scholar] [CrossRef]
- Phillips, N. The Coronavirus is Here to Stay—Here’s What That Means. Nature 2021. Available online: https://www.nature.com/articles/d41586-021-00396-2 (accessed on 30 September 2021).
- Shivaram, D. Why Pfizer’s FDA Approval Matters And What It Means For Vaccine Mandates. NPR. 2021. Available online: https://www.npr.org/sections/coronavirus-live-updates/2021/08/24/1030267314/pfizer-vaccine-covid-fda-approval-kids-faq-mandate (accessed on 30 September 2021).
- Hubble, M.W.; Zontek, T.L.; Richards, M.E. Predictors of Influenza Vaccination among Emergency Medical Services Personnel. Prehospital Emerg. Care 2011, 15, 175–183. [Google Scholar] [CrossRef]
- Gur-Arie, R.; Jamrozik, E.; Kingori, P. No jab, no job? Ethical issues in mandatory COVID-19 vaccination of healthcare personnel. BMJ Glob. Health 2021, 6, e004877. [Google Scholar] [CrossRef]
- Ohio Department of Health. Ohio Vax-a-Million Details Announced. 2021. Available online: https://odh.ohio.gov/wps/portal/gov/odh/media-center/odh-news-releases/odh-news-release-05-17-21 (accessed on 29 September 2021).
- Parmar, S. Harris County Will Pay You $100 To Get Your First Dose of The COVID-19 Vaccine. Houston Public Media. 2021. Available online: https://www.houstonpublicmedia.org/articles/news/health-science/2021/08/17/406205/harris-county-launches-100-incentive-program-to-combat-dwindling-vaccination-rate/ (accessed on 29 September 2021).
- Sehgal, N.K. Impact of Vax-A-Million Lottery on COVID-19 Vaccination Rates in Ohio. Am. J. Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Walkey, A.J.; Law, A.; Bosch, N.A. Lottery-Based Incentive in Ohio and COVID-19 Vaccination Rates. JAMA 2021, 326, 766. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Agley, J. Assessing changes in US public trust in science amid the COVID-19 pandemic. Public Health 2020, 183, 122–125. [Google Scholar] [CrossRef] [PubMed]






| Characteristic | Statistics (n = 2257) |
|---|---|
| Gender—n (%) | |
| Male | 1480 (65.6%) |
| Female | 747 (33.1%) |
| Missing | 30 (1.3%) |
| Age—n (%) | |
| <28 years | 524 (23.2%) |
| 29–38 years | 564 (25.0%) |
| 39–50 years | 583 (25.8%) |
| >51 years | 585 (25.9%) |
| Race and Ethnicity—n (%) | |
| White, Non-Hispanic | 1910 (84.6%) |
| Other | 269 (11.9%) |
| Missing | 78 (3.5%) |
| Certification—n (%) | |
| Basic Life Support | 900 (39.9%) |
| Advanced Life Support | 1357 (60.1%) |
| Educational Level—n (%) | |
| HS/GED | 211 (9.3%) |
| Some College | 601 (26.6%) |
| Associate’s | 413 (18.3%) |
| Bachelor’s | 508 (22.5%) |
| Master’s/Doctorate | 175 (7.8%) |
| Urbanicity—n (%) | |
| Urban/suburban | 1361 (60.3%) |
| Rural | 793 (35.1%) |
| Missing | 103 (4.6%) |
| Agency Type—n (%) | |
| Fire | 562 (24.9%) |
| Private | 476 (21.1%) |
| Government, non-fire | 293 (13.0%) |
| Hospital | 243 (10.8%) |
| Other 1 | 201 (8.9%) |
| Missing | 482 (21.4%) |
| Service Type—n (%) | |
| 911 | 657 (29.1%) |
| All Others 2 | 272 (12.1%) |
| Missing | 1328 (58.8%) |
| Years in EMS—mean (IQR) | 14.3 (18.0) |
| Employment Status—n (%) | |
| Full-Time | 1265 (56.0%) |
| Part-Time | 212 (9.4%) |
| Volunteer | 240 (10.6%) |
| Missing | 540 (23.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gregory, M.E.; MacEwan, S.R.; Gaughan, A.A.; Rush, L.J.; Powell, J.R.; Kurth, J.D.; Kenah, E.; Panchal, A.R.; Scheck McAlearney, A. Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust. Int. J. Environ. Res. Public Health 2022, 19, 644. https://doi.org/10.3390/ijerph19020644
Gregory ME, MacEwan SR, Gaughan AA, Rush LJ, Powell JR, Kurth JD, Kenah E, Panchal AR, Scheck McAlearney A. Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust. International Journal of Environmental Research and Public Health. 2022; 19(2):644. https://doi.org/10.3390/ijerph19020644
Chicago/Turabian StyleGregory, Megan E., Sarah R. MacEwan, Alice A. Gaughan, Laura J. Rush, Jonathan R. Powell, Jordan D. Kurth, Eben Kenah, Ashish R. Panchal, and Ann Scheck McAlearney. 2022. "Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust" International Journal of Environmental Research and Public Health 19, no. 2: 644. https://doi.org/10.3390/ijerph19020644
APA StyleGregory, M. E., MacEwan, S. R., Gaughan, A. A., Rush, L. J., Powell, J. R., Kurth, J. D., Kenah, E., Panchal, A. R., & Scheck McAlearney, A. (2022). Closing the Gap on COVID-19 Vaccinations in First Responders and Beyond: Increasing Trust. International Journal of Environmental Research and Public Health, 19(2), 644. https://doi.org/10.3390/ijerph19020644






