Impact of Non-Face-to-Face Teaching with Passive Training on Personal Protective Equipment Use in Health Science Students: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
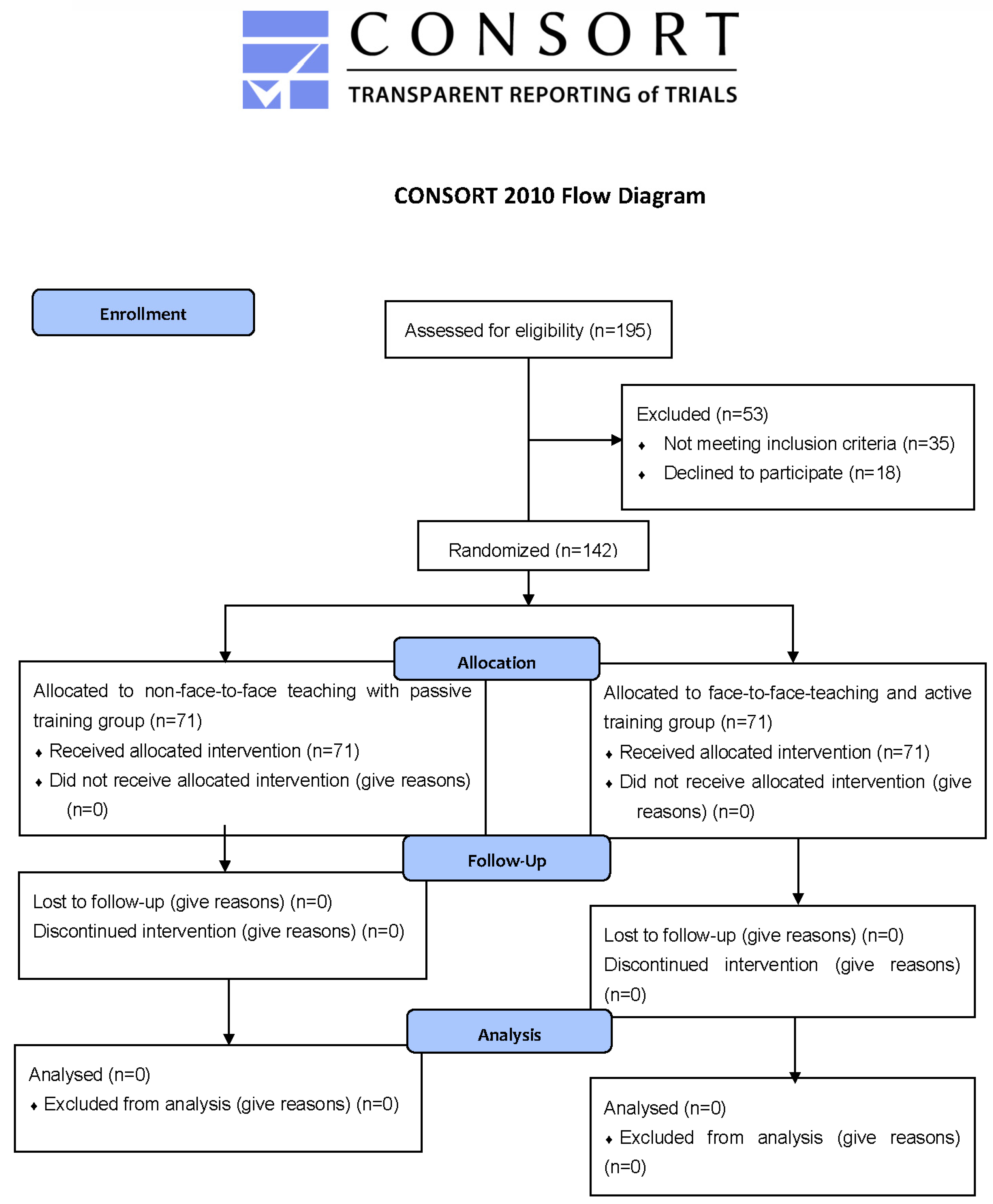
2.1. Study Design and Participants
2.2. Study Protocol
2.3. Study Variables
3. Results
3.1. Sample Description
3.2. Self-Assessment of the Management of PPE in the Total Study Population According to Training Modalities
3.2.1. Considering the Response Options as Categorical Variables
3.2.2. Considering Means of the Response Options
3.3. Tasks Violated and Time Needed to Accomplish the PPPE Protocol
3.4. Perceived Satisfaction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Crisol-Moya, E.; Romero-López, M.A.; Caurcel-Cara, M.J. Active Methodologies in Higher Education: Perception and Opinion as Evaluated by Professors and Their Students in the Teaching-Learning Process. Front. Psychol. 2020, 11, 1703. [Google Scholar] [CrossRef]
- Nabovati, E.; Jeddi, F.R.; Ghaffari, F.; Mirhoseini, F. The effects of simulation training on learning of health information systems: A scoping review. J. Educ. Health Promot. 2022, 11, 4. [Google Scholar] [PubMed]
- Ayaz, O.; Ismail, F.W. Healthcare Simulation: A Key to the Future of Medical Education—A Review. Adv. Med. Educ. Pract. 2022, 13, 301–308. [Google Scholar] [CrossRef]
- Roussin, C.; Sawyer, T.; Weinstock, P. Assessing competency using simulation: The SimZones approach. BMJ Simul. Technol. Enhanc. Learn. 2020, 6, 262–267. [Google Scholar] [CrossRef]
- Tseng, L.P.; Hou, T.H.; Huang, L.P.; Ou, Y.K. Effectiveness of applying clinical simulation scenarios and integrating information technology in medical-surgical nursing and critical nursing courses. BMC Nurs. 2021, 20, 229. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Cross, S.; Attoe, C. The Use of in situ Simulation in Healthcare Education: Current Perspectives. Adv. Med. Educ. Pract. 2020, 11, 893–903. [Google Scholar] [CrossRef] [PubMed]
- Effectiveness of Simulation-Based Nursing Education Depending on Fidelity: A Meta-Analysis|BMC Medical Education|Full Text. Available online: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-016-0672-7 (accessed on 24 July 2022).
- Archana, S.; Nilakantam, S.R.; Hathur, B.; Dayananda, M. The Need and Art of Establishing Skill and Simulation Centers to Strengthen Skill-Based Medical Education: Learning Insights and Experience. Ann. Afr. Med. 2021, 20, 247–254. [Google Scholar] [PubMed]
- Lamé, G.; Dixon-Woods, M. Using clinical simulation to study how to improve quality and safety in healthcare. BMJ Simul. Technol. Enhanc. Learn. 2020, 6, 87–94. [Google Scholar] [CrossRef] [Green Version]
- Chick, R.C.; Clifton, G.T.; Peace, K.M.; Propper, B.W.; Hale, D.F.; Alseidi, A.A.; Vreeland, T.J. Using Technology to Maintain the Education of Residents During the COVID-19 Pandemic. J. Surg. Educ. 2020, 77, 729–732. [Google Scholar] [CrossRef]
- Atwa, H.; Shehata, M.H.; Al-Ansari, A.; Kumar, A.; Jaradat, A.; Ahmed, J.; Deifalla, A. Online, Face-to-Face, or Blended Learning? Faculty and Medical Students’ Perceptions During the COVID-19 Pandemic: A Mixed-Method Study. Front. Med. 2022, 9, 791352. [Google Scholar] [CrossRef]
- Battista, R.A.; Ferraro, M.; Piccioni, L.O.; Malzanni, G.E.; Bussi, M. Personal Protective Equipment (PPE) in COVID 19 Pandemic. J. Occup. Environ. Med. 2021, 63, e80–e85. [Google Scholar] [CrossRef] [PubMed]
- Yeon, J.H.; Shin, Y.S. Effects of Education on the Use of Personal Protective Equipment for Reduction of Contamination: A Randomized Trial. SAGE Open Nurs. 2020, 6, 2377960820940621. [Google Scholar] [CrossRef] [PubMed]
- Mosher, C.; Mukhtar, F.; Alnaami, N.; Akkielah, Y.A.; Alsharif, J.; Khan, T.; Taskiran, H.C.; Zafar, M. Donning and Doffing of Personal Protective Equipment: Perceived Effectiveness of Virtual Simulation Training to Decrease COVID-19 Transmission and Contraction. Cureus 2022, 14, e22943. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, C.A. OxMaR: Open Source Free Software for Online Minimization and Randomization for Clinical Trials. PLoS ONE 2014, 9, e110761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC. Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. 2020. Available online: https://www.cdc.gov/coronavirus/2019-ncov/communication/print-resources.html (accessed on 24 July 2022).
- Steps to Put on Personal Protective Equipment (PPE). Available online: https://www.who.int/bangladesh/emergencies/coronavirus-disease-(covid-19)-update/steps-to-put-on-personal-protective-equipment-(ppe) (accessed on 24 July 2022).
- Pozo, J.I.; Pérez Echeverría, M.P.; Cabellos, B.; Sánchez, D.L. Teaching and Learning in Times of COVID-19: Uses of Digital Technologies During School Lockdowns. Front. Psychol. 2021, 12, 656776. Available online: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.656776 (accessed on 24 July 2022). [CrossRef]
- Torda, A.; Shulruf, B. It’s what you do, not the way you do it—Online versus face-to-face small group teaching in first year medical school. BMC Med. Educ. 2021, 21, 541. [Google Scholar] [CrossRef]
- Singal, A.; Bansal, A.; Chaudhary, P.; Singh, H.; Patra, A. Anatomy education of medical and dental students during COVID-19 pandemic: A reality check. Surg. Radiol. Anat. 2021, 43, 515–521. [Google Scholar] [CrossRef]
- Cho, M.K.; Kim, M.Y. Factors Affecting Learning Satisfaction in Face-to-Face and Non-Face-to-Face Flipped Learning among Nursing Students. Int. J. Environ. Res. Public Health 2021, 18, 8641. [Google Scholar] [CrossRef]
- Zaghal, A.; Marley, C.; Rahhal, S.; Hassanieh, J.; Saadeh, R.; El-Rifai, A.; Qaraqe, T.; ElBejjani, M.; Jaafar, R.; Hoballah, J.J. Face-to-face versus distance learning of basic suturing skills in novice learners: A quantitative prospective randomized trial. BMC Med. Educ. 2022, 22, 290. [Google Scholar] [CrossRef]
- Comparison of In-Person and Telesimulation for Critical Care Training during the COVID-19 Pandemic. Available online: https://www.atsjournals.org/doi/epdf/10.34197/ats-scholar.2021-0053OC (accessed on 8 August 2022).
- Dost, S.; Hossain, A.; Shehab, M.; Abdelwahed, A.; Al-Nusair, L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: A national cross-sectional survey of 2721 UK medical students. BMJ Open 2020, 10, e042378. [Google Scholar] [CrossRef]
- Rudolph, J.W.; Raemer, D.B.; Simon, R. Establishing a safe container for learning in simulation: The role of the presimulation briefing. Simul. Healthc. J. Soc. Simul. Healthc. 2014, 9, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Independent and Joint Effects of Teacher Enthusiasm and Motivation on Student Motivation and Experiences: A Field Experiment | Semantic Scholar. Available online: https://www.semanticscholar.org/paper/Independent-and-joint-effects-of-teacher-enthusiasm-Frenzel-Taxer/0c03473176692f16c03ebc3b7014431c5f1f227d (accessed on 4 October 2022).
- Displayed Enthusiasm Attracts Attention and Improves Recall—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/33325548/ (accessed on 4 October 2022).
- Does Speaker’s Voice Enthusiasm Affect Social Cue, Cognitive Load and Transfer in Multimedia Learning? | Emerald Insight. Available online: https://www.emerald.com/insight/content/doi/10.1108/ILS-11-2019-0124/full/html (accessed on 4 October 2022).
- Does Displayed Enthusiasm Favour Recall, Intrinsic Motivation and Time Estimation?—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/26211683/ (accessed on 4 October 2022).
- Dabrowski, M.; Steliga, A.; Dabrowska, A.; Smereka, J.; Szarpak, Ł. Use simulation to improve the effectiveness of PPE in COVID-19. Disaster Emerg. Med. J. 2020, 5, 171–173. [Google Scholar]
- Jen, H.J.; Chou, K.R.; Chang, C.Y. Fostering Nursing Staff Competence in Personal Protective Equipment Education during COVID-19: A Mobile-Video Online Learning Approach. Int. J. Environ. Res. Public Health 2022, 19, 9238. [Google Scholar] [CrossRef] [PubMed]
- Hoedl, M.; Eglseer, D.; Bauer, S. Associations between personal protective equipment and nursing staff stress during the COVID-19 pandemic. J. Nurs. Manag. 2021, 29, 2374–2382. [Google Scholar] [CrossRef] [PubMed]
- Verbeek, J.H.; Rajamaki, B.; Ijaz, S.; Sauni, R.; Toomey, E.; Blackwood, B.; Tikka, C.; Ruotsalainen, J.H.; Balci, F.S.K. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Syst. Rev. 2020, 2020, CD011621. [Google Scholar]
- Hung, P.P.; Choi, K.S.; Chiang, V.C.L. Using interactive computer simulation for teaching the proper use of personal protective equipment. CIN Comput. Inform. Nurs. 2015, 33, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Hannum, D.; Cycan, K.; Jones, L.; Stewart, M.; Morris, S.; Markowitz, S.M.; Wong, E.S. The effect of respirator training on the ability of healthcare workers to pass a qualitative fit test. Infect. Control Hosp. Epidemiol. 1996, 17, 636–640. [Google Scholar] [CrossRef]
- Shigayeva, A.; Green, K.; Raboud, J.M.; Henry, B.; Simor, A.E.; Vearncombe, M.; Zoutman, D.; Loeb, M.; McGeer, A.; Team, S.H.I. Factors Associated With Critical-Care Healthcare Workers’ Adherence to Recommended Barrier Precautions During the Toronto Severe Acute Respiratory Syndrome Outbreak. Infect. Control Hosp. Epidemiol. 2007, 28, 1275–1283. [Google Scholar] [CrossRef]
- Online Classes versus Traditional Classes? Comparison during COVID-19—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/35233404/ (accessed on 4 October 2022).
- Currat, L.; Suppan, M.; Gartner, B.A.; Daniel, E.; Mayoraz, M.; Harbarth, S.; Suppan, L.; Stuby, L. Impact of Face-to-Face Teaching in Addition to Electronic Learning on Personal Protective Equipment Doffing Proficiency in Student Paramedics: Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 3077. [Google Scholar] [CrossRef]
- Díaz-Guio, D.A.; Ríos-Barrientos, E.; Santillán-Roldan, P.A.; Mora-Martinez, S.; Díaz-Gómez, A.S.; Martínez-Elizondo, J.A.; Barrientos-Aguiñaga, A.; Arroyo-Romero, M.N.; Ricardo-Zapata, A.; Rodríguez-Morales, A.J. Online-synchronized clinical simulation: An efficient teaching-learning option for the COVID-19 pandemic time and: Beyond. Adv. Simul. 2021, 6, 30. [Google Scholar] [CrossRef]
- Nichol, K.; Bigelow, P.; O’Brien-Pallas, L.; McGeer, A.; Manno, M.; Holness, D.L. The individual, environmental, and organizational factors that influence nurses’ use of facial protection to prevent occupational transmission of communicable respiratory illness in acute care hospitals. Am. J. Infect. Control 2008, 36, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.L.; Yang, S.; Luo, H.X.; You, J.P. The Error-Prone Operational Steps and Key Sites of Self-Contamination During Donning and Doffing of Personal Protective Equipment by Health Care Workers. In Disaster Medicine and Public Health Preparedness; Society for Disaster Medicine and Public Health, Inc.: Onancock, VA, USA, 2021; pp. 1–6. [Google Scholar]
- Suen, L.K.P.; Guo, Y.P.; Tong, D.W.K.; Leung, P.H.M.; Lung, D.; Ng, M.S.P.; Lai, T.K.H.; Lo, K.Y.K.; Au-Yeung, C.H.; Yu, W. Self-contamination during doffing of personal protective equipment by healthcare workers to prevent Ebola transmission. Antimicrob. Resist. Infect. Control 2018, 7, 157. [Google Scholar] [CrossRef] [PubMed]
- Casalino, E.; Astocondor, E.; Sanchez, J.C.; Díaz-Santana, D.E.; Del Aguila, C.; Carrillo, J.P. Personal protective equipment for the Ebola virus disease: A comparison of 2 training programs. Am. J. Infect. Control 2015, 43, 1281–1287. [Google Scholar] [CrossRef] [PubMed]
- Salway, R.J.; Williams, T.; Londono, C.; Roblin, P.; Koenig, K.; Arquilla, B. Comparing Training Techniques in Personal Protective Equipment Use. Prehosp. Disaster Med. 2020, 35, 364–371. [Google Scholar] [CrossRef]
| Total | Face-to-Face Teaching with Active Training | Non-Face-to-Face Teaching with Passive Training | ||
|---|---|---|---|---|
| N = 142 | N = 72 (50.7) | N = 70 (49.3) | p Value | |
| Gender | ||||
| Women | 90 (63.4) | 49 (54.4) | 41 (45.6) | 0.241 |
| Age (years) | 22.54 ± 6.39 | 23.44 ± 7.49 | 21.61 ± 4.91 | 0.088 |
| Degree | ||||
| Nursing | 46 (32.4) | 22 (47.8) | 24 (52.2) | 0.635 |
| Physiotherapy | 96 (67.6) | 50 (52.1) | 46 (47.9) | |
| Academic Year | ||||
| 1st | 40 (28.2) | 16 (40.0) | 24 (60.0) | 0.279 |
| 2nd | 31 (21.8) | 17 (54.8) | 24 (45.2) | |
| 3rd | 71 (50.0) | 39 (54.9) | 32 (45.1) | |
| Campus | ||||
| Granada | 46 (32.4) | 22 (47.8) | 24 (52.2) | 0.635 |
| Melilla | 96 (67.6) | 50 (52.1) | 46 (47.9) | |
| Please Rate the Extent to which You Agree or Disagree with Each of the Following Statements: | Response | Total (N = 142) | Face-to-Face Teaching with Active Training (N = 72) | Non-Face-to-Face Teaching with Passive Training (N = 70) | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | p Value | ||
| 1. I felt confident in donning prior to receiving this training | Strongly Disagree | 24 (16.9) | 15 (62.5) | 9 (37.5) | 0.272 |
| In Disagreement | 22 (15.5) | 12 (54.5) | 10 (45.5) | ||
| Neutral | 31 (21.8) | 12 (38.7) | 19 (61.3) | ||
| In Agreement | 35 (24.6) | 15 (42.9) | 20 (57.1) | ||
| Totally Agree | 30 (21.1) | 18 (60.0) | 12 (40.0) | ||
| 2. I felt confident in doffing prior to receiving this training | Strongly Disagree | 28 (19.7) | 18 (64.3) | 10 (35.7) | 0.125 |
| In Disagreement | 23 (16.2) | 11(47.8) | 12 (52.2) | ||
| Neutral | 35 (24.6) | 14 (40.0) | 21 (60.0) | ||
| In Agreement | 26 (18.3) | 10 (38.5) | 16 (61.5) | ||
| Totally Agree | 30 (21.1) | 19 (63.3) | 11 (36.7) | ||
| 3. The training that I received explained the steps of donning and doffing adequately for me | Strongly Disagree | 1 (0.7) | 0 (0.0) | 1 (100.0) | 0.467 |
| In Disagreement | 2 (1.4) | 0 (0.0) | 2 (100.0) | ||
| Neutral | 3 (2.1) | 2 (66.7) | 1 (33.3) | ||
| In Agreement | 27 (19.0) | 13 (48.1) | 14 (51.9) | ||
| Totally Agree | 109 (76.8) | 57 (52.3) | 52 (47.7) | ||
| 4. I felt more confident in donning after receiving this training | Strongly Disagree | 1 (0.7) | 0 (0.0) | 1 (100.0) | 0.177 |
| In Disagreement | 0 (0.0) | ||||
| Neutral | 5 (3.5) | 1 (20.0) | 4 (80.0) | ||
| In Agreement | 23 (16.2) | 9 (39.1) | 14 (60.9) | ||
| Totally Agree | 113 (79.6) | 62 (54.9) | 51 (45.1) | ||
| 5. I felt more confident in doffing after receiving this training | Strongly Disagree | 1 (0.7) | 0 (0.0) | 1 (100.0) | 0.192 |
| In Disagreement | 0 (0.0) | ||||
| Neutral | 2 (1.4) | 0 (0.0) | 2 (100.0) | ||
| In Agreement | 29 (20.4) | 12 (41.4) | 17 (58.6) | ||
| Totally Agree | 110 (77.5) | 60 (54.5) | 50 (45.5) | ||
| 6. This training capture my attention | Strongly Disagree | 1 (0.7) | 0 (0.0) | 1 (100.0) | 0.190 |
| In Disagreement | 2 (1.4) | 0 (0.0) | 2 (100.0) | ||
| Neutral | 6 (4.2) | 5 (83.3) | 1 (16.7) | ||
| In Agreement | 27 (19.0) | 12 (44.4) | 15 (55.6) | ||
| Totally Agree | 106 (74.6) | 55 (51.9) | 51 (48.1) |
| Please Rate the Extent to which you Agree or Disagree with Each of the Following Statements: | Total (N = 142) | Face-to-Face Teaching with Active Training (N = 72) | Non-Face-to-Face Teaching with Passive Training (N = 70) | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p Value | |
| 1. I felt confident in donning prior to receiving this training | 3.18 (1.38) | 3.13 (1.49) | 3.23 (1.26) | 0.656 |
| 2. I felt confident in doffing prior to receiving this training | 3.05 (1.41) | 3.01 (1.54) | 3.09 (1.27) | 0.762 |
| 3. The training that I received explained the steps of donning and doffing adequately for me | 4.70 (0.65) | 4.76 (0.49) | 4.63 (0.78) | 0.221 |
| 4. I felt more confident in donning after receiving this training | 4.74 (0.59) | 4.85 (0.39) | 4.63 (0.73) | 0.029 |
| 5. I felt more confident in doffing after receiving this training | 4.74 (0.55) | 4.83 (0.37) | 4.64 (0.68) | 0.042 |
| 6. This training capture my attention | 4.65 (0.69) | 4.69 (0.59) | 4.61 (0.79) | 0.494 |
| Tasks Violated | ||||
|---|---|---|---|---|
| Total (N = 142) | Face-to-Face Teaching with Active Training (N = 72) | Non-Face-to-Face Teaching with Passive Training (N = 70) | ||
| N (%) | N (%) | N (%) | p Value | |
| Donning Tasks Completed | ||||
| 1. Hand hygiene | 17 (12.0) | 12 (70.6) | 5 (29.4) | 0.080 |
| 2. Put on the isolation gown and tie the straps | 14 (9.9) | 8 (57.1) | 6 (42.9) | 0.612 |
| 3. Put on the mask correctly (mold the metal band to the shape of the nose with your hands and cover up to the bottom of the chin; nose and mouth must be protected) | 48 (33.8) | 27 (56.3) | 21 (43.8) | 0.345 |
| 4. Put on protective glasses | 18 (12.7) | 7 (38.9) | 11 (61.1) | 0.283 |
| 5. Put on the gloves (cover the cuffs of the gown, without leaving bare skin on the wrists) | 22 (15.5) | 11 (50.0) | 11 (50.0) | 0.943 |
| Doffing Tasks Completed | ||||
| 1. Remove gloves using the correct technique to avoid hand contamination | 34 (23.9) | 14 (41.2) | 20 (58.8) | 0.203 |
| 2. Take off the gown (untie straps gently, without abrupt movements, from the shoulders down and away from the body) | 43 (30.3) | 16 (37.2) | 27 (62.8) | 0.034 |
| 3. Hand hygiene | 31 (21.8) | 12 (38.7) | 19 (61.3) | 0.131 |
| 4. Remove goggles (pulling the back of the temple and pulling it forward away from the head, without touching the front) | 27 (19.0) | 10 (37.0) | 17 (63.0) | 0.114 |
| 5. Take off the mask (do not touch the front part) | 17 (12.0) | 5 (29.4) | 12 (70.6) | 0.061 |
| 6. Hand hygiene | 29 (20.4) | 14 (48.3) | 15 (51.7) | 0.769 |
| Total (N = 142) | Face-to-Face Teaching with Active Training (N = 72) | Non-Face-to-Face Teaching with Passive Training (N = 70) | ||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p Value | |
| Time for donning (seconds) | 120.55 (38.87) | 120.90 (40.01) | 120.19 (37.95) | 0.913 |
| Time for doffing (seconds) | 71.46 (24.41) | 75.11 (28.53) | 67.71 (18.75) | 0.070 |
| Total number of tasks violated | 1.87 (1.91) | 1.53 (1.78) | 2.23 (1.99) | 0.029 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rueda-Medina, B.; Aguilar-Ferrándiz, M.E.; Esteban-Burgos, A.A.; Tapia Haro, R.M.; Casas-Barragán, A.; Velando-Soriano, A.; Gil-Gutiérrez, R.; Correa-Rodríguez, M. Impact of Non-Face-to-Face Teaching with Passive Training on Personal Protective Equipment Use in Health Science Students: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 12981. https://doi.org/10.3390/ijerph191912981
Rueda-Medina B, Aguilar-Ferrándiz ME, Esteban-Burgos AA, Tapia Haro RM, Casas-Barragán A, Velando-Soriano A, Gil-Gutiérrez R, Correa-Rodríguez M. Impact of Non-Face-to-Face Teaching with Passive Training on Personal Protective Equipment Use in Health Science Students: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(19):12981. https://doi.org/10.3390/ijerph191912981
Chicago/Turabian StyleRueda-Medina, Blanca, María Encarnación Aguilar-Ferrándiz, Ana Alejandra Esteban-Burgos, Rosa María Tapia Haro, Antonio Casas-Barragán, Almudena Velando-Soriano, Rocío Gil-Gutiérrez, and María Correa-Rodríguez. 2022. "Impact of Non-Face-to-Face Teaching with Passive Training on Personal Protective Equipment Use in Health Science Students: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 19: 12981. https://doi.org/10.3390/ijerph191912981
APA StyleRueda-Medina, B., Aguilar-Ferrándiz, M. E., Esteban-Burgos, A. A., Tapia Haro, R. M., Casas-Barragán, A., Velando-Soriano, A., Gil-Gutiérrez, R., & Correa-Rodríguez, M. (2022). Impact of Non-Face-to-Face Teaching with Passive Training on Personal Protective Equipment Use in Health Science Students: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(19), 12981. https://doi.org/10.3390/ijerph191912981







