How Do Healthy Women Perceive the Risk of Breast Cancer? The Role of Illness Perceptions and Compared Risk between Portugal and the U.A.E
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Brief Illness Perception Questionnaire (Brief-IPQ)
2.4. Risk Perceptions (Perceived Individual Risk and Compared Risk)
2.5. Beliefs on Preventive Behaviors for Breast Cancer
2.6. Age Estimations for Breast Cancer and Screening
2.7. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Comparison between Groups on the Study Variables
3.2.1. Illness Perceptions and Risk Perception (Individual Perceived Risk and Comparative Risk)
3.2.2. Family History of Breast Cancer
3.2.3. Beliefs about Preventive Behaviors
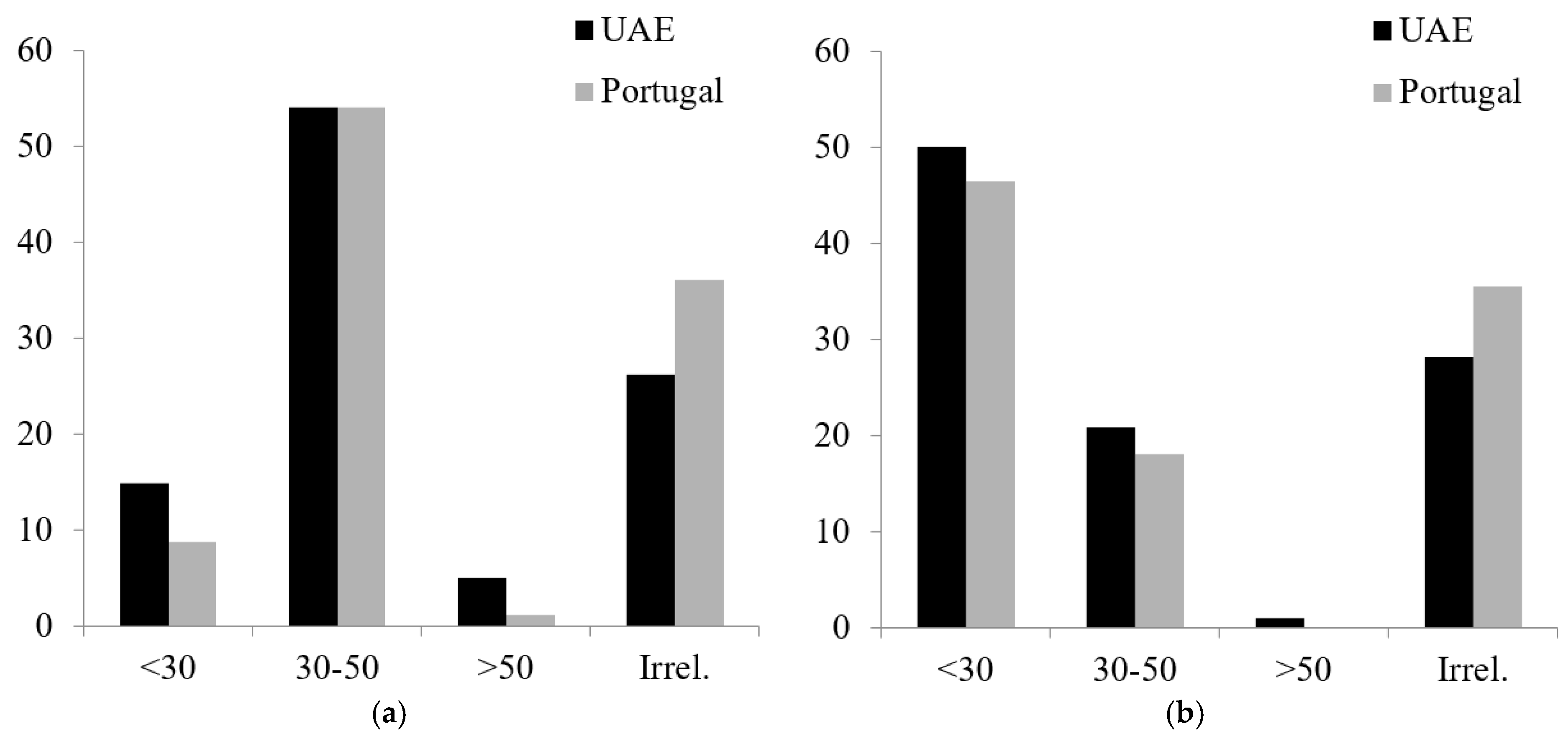
3.2.4. Beliefs about Age Probability of Getting BC and Undergoing Screening to Prevent BC
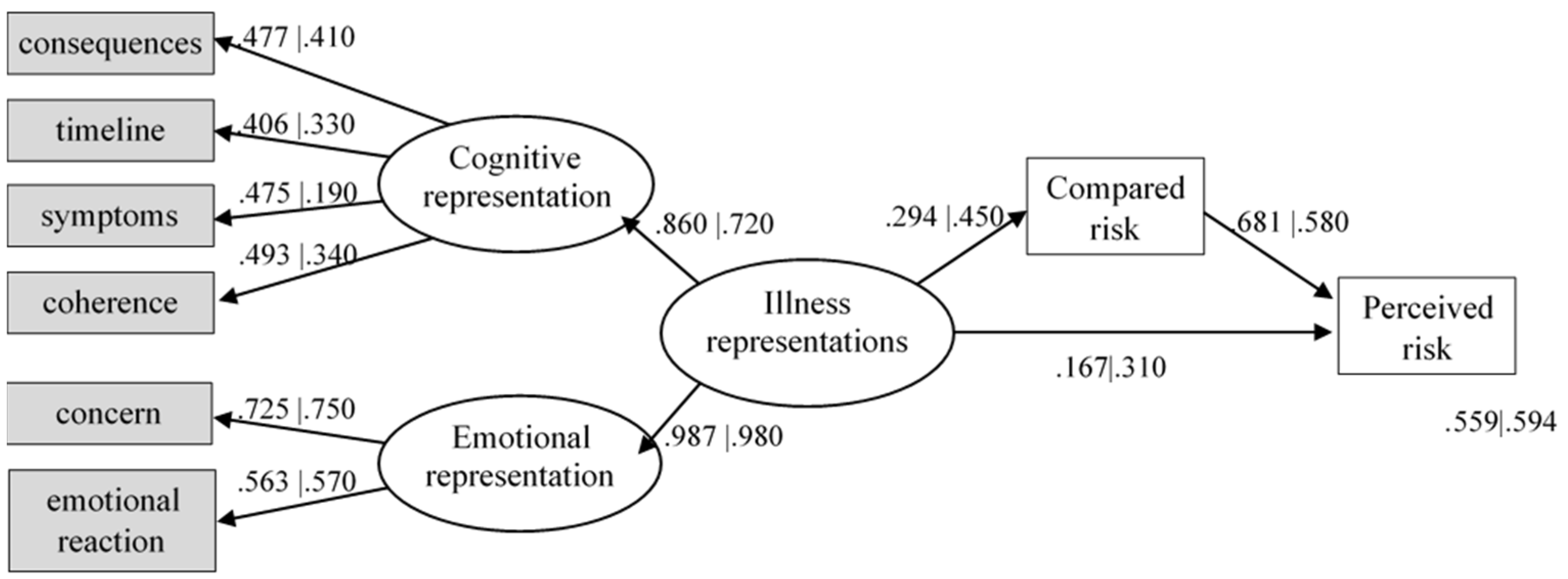
3.3. To Explore Predictors of Individual Risk Perception for BC in Healthy Young Women in Each Country
4. Discussion
5. Conclusions
- (a)
- The importance of comparative risk as a mediator between illness perception of BC and perceived individual risk, raising important questions to inform future approaches to assess perceived risk for BC and their influence in adopting protective behaviors.
- (b)
- How social comparison and reduced risk perceptions may undermine the need for screening and breast self-examination.
- (c)
- How the content of illness perceptions may serve as the basis for appraisals of likelihood and severity, influencing perceived individual risk mediated by compared risk.
- (d)
- How demographic characteristics and psychosocial factors can influence perceived risk, suggesting the need to integrate these factors into the design and implementation of future educational interventions.
- (e)
- Interventions must consider the needs and characteristics of the target groups by providing culturally appropriate strategies to promote early detection behaviors for BC.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wild, C.P.; Weiderpass, E.; Stewart, B.W. World Cancer Report: Cancer Research for Cancer Prevention; International Agency for Research on Cancer: Lyon, France, 2020. [Google Scholar]
- World Health Organization. Breast Cancer. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 15 September 2022).
- World Health Organization. Non-Communicable Diseases, Breast Cancer, Early Detection. 2021. Available online: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cancer/news/news/2012/2/early-detection-of-common-cancers/breast-cancer (accessed on 15 September 2022).
- Albeshan, S.M.; Mackey, M.G.; Hossain, S.Z.; Alfuraih, A.A.; Brennan, P.C. Breast Cancer Epidemiology in Gulf Cooperation Council Countries: A Regional and International Comparison. Clin. Breast Cancer 2018, 18, e381–e392. [Google Scholar] [CrossRef] [PubMed]
- Najjar, H.; Easson, A. Age at diagnosis of breast cancer in Arab nations. Int. J. Surg. 2010, 8, 448–452. [Google Scholar] [CrossRef] [PubMed]
- Al-Shamsi, H.; Alrawi, S. Breast cancer screening in the United Arab Emirates: Is it time to call for a screening at an earlier age? J. Cancer Prev. Curr. Res. 2018, 9, 123–126. [Google Scholar] [CrossRef]
- World Health Organization. Cancer country profile UAE. Int. Agency Res. Cancer 2020, 1–2. Available online: https://www.who.int/publications/m/item/cancer-are-2020 (accessed on 15 September 2022).
- Syse, A.; Geller, B. A Cross-Cultural Perspective on Challenges Facing Comparative Cancer Survivorship Research. J. Cancer Epidemiol. 2011, 2011, 1–9. [Google Scholar] [CrossRef][Green Version]
- Badr, L.K.; Bourdeanu, L.; Alatrash, M.; Bekarian, G. Breast Cancer Risk Factors: A Cross- Cultural Comparison between the West and the East. Asian Pac. J. Cancer Prev. 2018, 19, 2109–2116. [Google Scholar] [CrossRef]
- Donnelly, T.T.; Al Khater, A.H.; Al-Bader, S.B.; Al Kuwari, M.G.; Al-Meer, N.; Malik, M.; Singh, R.; Jong, F.C.D. Arab Women’s Breast Cancer Screening Practices: A Literature Review. Asian Pac. J. Cancer Prev. 2013, 14, 4519–4528. [Google Scholar] [CrossRef]
- Fearon, D.; Hughes, S.; Brearley, S.G. Experiences of breast cancer in Arab countries. A thematic synthesis. Qual. Life Res. 2020, 29, 313–324. [Google Scholar] [CrossRef] [PubMed]
- Anwar, M.M.; Khalil, D.M. Breast cancer knowledge, attitude and practice among medical and non-medical university students. J. Public Health 2020, 29, 871–878. [Google Scholar] [CrossRef]
- Leventhal, H.; Brissette, I.; Leventhal, E.A. The common-sense model of self-regulation of health and illness. In The Self-Regulation of Health & Illness Behaviour; Cameron, L.D., Leventhal, H., Eds.; Routledge: London, UK, 2003; pp. 42–60. [Google Scholar]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef]
- Benyamini, Y. Health and Illness Perceptions. In The Oxford Handbook of Health Psychology; Oxford University Press: Oxford, UK, 2011; pp. 285–318. [Google Scholar] [CrossRef]
- Kus, T.; Aktas, G.; Ekici, H.; Elboga, G.; Djamgoz, S. Illness perception is a strong parameter on anxiety and depression scores in early-stage breast cancer survivors: A single-center cross-sectional study of Turkish patients. Support. Care Cancer 2017, 25, 3347–3355. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Baek, J.-M.; Jeon, Y.-W.; Im, E.-O. Illness perception and sense of well-being in breast cancer patients. Patient Prefer. Adherence 2019, 13, 1557–1567. [Google Scholar] [CrossRef] [PubMed]
- McCorry, N.K.; Dempster, M.; Quinn, J.; Hogg, A.; Newell, J.; Moore, M.; Kelly, S.; Kirk, S.J. Illness perception clusters at diagnosis predict psychological distress among women with breast cancer at 6 months post diagnosis. Psycho-Oncology 2013, 22, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Freeman-Gibb, L.A.; Janz, N.K.; Katapodi, M.; Zikmund-Fisher, B.; Northouse, L. The relationship between illness representations, risk perception and fear of cancer recurrence in breast cancer survivors. Psycho-Oncology 2017, 26, 1270–1277. [Google Scholar] [CrossRef] [PubMed]
- Kaptein, A.A.; Schoones, J.W.; Fischer, M.J.; Thong, M.S.Y.; Kroep, J.R.; Van Der Hoeven, K.J.M. Illness Perceptions in Women with Breast Cancer—A Systematic Literature Review. Curr. Breast Cancer Rep. 2015, 7, 117–126. [Google Scholar] [CrossRef]
- Rees, G.; Fry, A.; Cull, A.; Sutton, S. Illness perceptions and distress in women at increased risk of breast cancer. Psychol. Health 2004, 19, 749–765. [Google Scholar] [CrossRef]
- Fischer, M.J.; Inoue, K.; Matsuda, A.; Kroep, J.; Nagai, S.; Tozuka, K.; Momiyama, M.; Weijl, N.I.; Langemeijer-Bosman, D.; Ramai, S.R.S.; et al. Cross-cultural comparison of breast cancer patients’ Quality of Life in the Netherlands and Japan. Breast Cancer Res. Treat. 2017, 166, 459–471. [Google Scholar] [CrossRef]
- Kaptein, A.A.; Yamaoka, K.; Snoei, L.; Van Der Kloot, W.A.; Inoue, K.; Tabei, T.; Kroep, J.R.; Krol-Warmerdam, E.; Ranke, G.; Meirink, C.; et al. Illness Perceptions and Quality of Life in Japanese and Dutch Women with Breast Cancer. J. Psychosoc. Oncol. 2013, 31, 83–102. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, A.; Groarke, A. Can risk and illness perceptions predict breast cancer worry in healthy women? J. Health Psychol. 2016, 21, 2052–2062. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Gibbons, F.X.; Gerrard, M.; McCaul, K.D.; Weinstein, N.D. Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2007, 26, 136–145. [Google Scholar] [CrossRef]
- Wendt, S.J. Perception of future risk of breast cancer and coronary heart disease in female undergraduates. Psychol. Health Med. 2005, 10, 253–262. [Google Scholar] [CrossRef]
- Fehniger, J.; Livaudais-Toman, J.; Karliner, L.; Kerlikowske, K.; Tice, J.; Quinn, J.; Ozanne, E.; Kaplan, C.P. Perceived Versus Objective Breast Cancer, Breast Cancer Risk in Diverse Women. J. Women’s Health 2014, 23, 420–427. [Google Scholar] [CrossRef]
- French, D.P.; Hevey, D.; Sutton, S.; Kinmonth, A.L.; Marteau, T.M. Personal and Social Comparison Information about Health Risk: Reaction to information and information search. J. Health Psychol. 2006, 11, 497–510. [Google Scholar] [CrossRef] [PubMed]
- Renn, B.; Rohrmann, O. Cross-Cultural Risk Perception: State and Challenges. Technology, Risk, and Society (An International Series in Risk Analysis). In Cross-Cultural Risk Perception; Springer: Boston, MA, USA, 2000; Volume 13, pp. 211–233. [Google Scholar]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The Brief Illness Perception Questionnaire. Psychosomatics 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, E.; Wilkes, C.; Koschwanez, H.; Weinman, J.A.; Norton, S.; Petrie, K.J. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol. Health 2015, 30, 1361–1385. [Google Scholar] [CrossRef] [PubMed]
- Figueiras, M.; Marcelino, D.S.; Claudino, A.; Cortes, M.A.; Maroco, J.; Weinman, J. Patients’ illness schemata of hypertension: The role of beliefs for the choice of treatment. Psychol. Health 2010, 25, 507–517. [Google Scholar] [CrossRef]
- Reynolds, L.; Broadbent, E.; Ellis, C.J.; Gamble, G.; Petrie, K.J. Patients’ drawings illustrate psychological and functional status in heart failure. J. Psychosom. Res. 2007, 63, 525–532. [Google Scholar] [CrossRef]
- Figueiras, M.J.; Maroco, J.; Monteiro, R.; Caeiro, R.; Neto, D.D. Discerning the impact of personal and situational variables in risk perception of coronary heart disease. J. Health Psychol. 2017, 22, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.J.L.; Corner, A. Communicating environmental risks: Clarifying the severity effect in interpretations of verbal probability expressions. J. Exp. Psychol. Learn. Mem. Cogn. 2011, 37, 1571–1578. [Google Scholar] [CrossRef]
- Cameron, L.D.; Reeve, J. Risk perceptions, worry, and attitudes about genetic testing for breast cancer susceptibility. Psychol. Health 2006, 21, 211–230. [Google Scholar] [CrossRef] [PubMed]
- Gerend, M.A.; Aiken, L.S.; West, S.G.; Erchull, M.J. Beyond Medical Risk: Investigating the Psychological Factors Underlying Women’s Perceptions of Susceptibility to Breast Cancer, Heart Disease, and Osteoporosis. Health Psychol. 2004, 23, 247–258. [Google Scholar] [CrossRef] [PubMed]
- Khazaee-Pool, M.; Montazeri, A.; Majlessi, F.; Foroushani, A.R.; Nedjat, S.; Shojaeizadeh, D. Breast cancer-preventive behaviors: Exploring Iranian women’s experiences. BMC Women’s Health 2014, 14, 41. [Google Scholar] [CrossRef] [PubMed]
- Shahab, L.; McGowan, J.A.; Waller, J.; Smith, S.G. Prevalence of beliefs about actual and mythical causes of cancer and their association with socio-demographic and health-related characteristics: Findings from a cross-sectional survey in England. Eur. J. Cancer 2018, 103, 308–316. [Google Scholar] [CrossRef] [PubMed]
- IBM. IBM SPSS Statistics for Windows, Version 26.0; IBM Corp: New York, NY, USA, 2017. [Google Scholar]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. Available online: http://www.ncbi.nlm.nih.gov/pubmed/17695343 (accessed on 15 September 2022). [CrossRef] [PubMed]
- Rosseel, Y. lavaan: AnRPackage for Structural Equation Modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- De Castro, E.K.K.; Lawrenz, P.; Romeiro, F.B.; De Lima, N.B.; Haas, S.A. Percepção da Doença e Enfrentamento em Mulheres com Câncer de Mama. Psicol. Teor. Pesqui. 2016, 32, 1–6. [Google Scholar] [CrossRef][Green Version]
- Leventhal, H.; Halm, E.; Horowitz, C.; Leventhal, E.A.; Ozakinci, G. Living with Chronic Illness: A contextualized, self-regulation approach. In The SAGE Handbook of Health Psychology; SAGE: Thousand Oaks, CA, USA, 2005; pp. 197–240. [Google Scholar]
- Cameron, L.D. Illness risk representations and motivations to engage in protective behavior: The case of skin cancer risk. Psychol. Health 2008, 23, 91–112. [Google Scholar] [CrossRef] [PubMed]
- Alves, S.A.V.; Weller, M. Breast Cancer Risk Perception and Mammography Screening Behavior of Women in Northeast Brazil. Women’s Health Rep. 2020, 1, 150–158. [Google Scholar] [CrossRef] [PubMed]
- Momenimovahed, Z.; Salehiniya, H. Epidemiological characteristics of and risk factors for breast cancer in the world. Breast Cancer Targets Ther. 2019, 11, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Inumaru, L.E.; Silveira, É.A.; Naves, M.M. Risk and protective factors for breast cancer: A systematic review. Cad. Saude Publica 2011, 27, 1259–1270. [Google Scholar] [CrossRef]
- Zucchetti, B.M.; Peccatori, F.A.; Codacci-Pisanelli, G. Pregnancy and Lactation: Risk or Protective Factors for Breast Cancer? Adv. Exp. Med. Biol. 2020, 1252, 195–197. [Google Scholar] [CrossRef]
- Okely, J.A.; Weiss, A.; Gale, C.R. The interaction between individualism and wellbeing in predicting mortality: Survey of Health Ageing and Retirement in Europe. J. Behav. Med. 2018, 41, 1–11. [Google Scholar] [CrossRef]
- Elsayed, A.A.; Mohammed, H. Prevention of Breast Cancer : Effects of Early Education on Knowledge and Practice of University Students in Saudi Arabia. IOSR JNHS 2019, 8, 1–9. [Google Scholar] [CrossRef]
- Ahmad, S.R.; Ahmad, A.A.; Abdullah, A.N.; Bin, S.R.A.; Amer, A.S.; Aisha, T.; Shahid, I.M. Awareness Level, Knowledge and Attitude towards Breast Cancer between Medical and Non-Medical University Students in Makkah Region: A Cross Sectional Study. Int. J. Cancer Clin. Res. 2019, 6. [Google Scholar] [CrossRef]
- Mehdi, I.; Monem, E.A.; Al Bahrani, B.; Al Kharusi, S.; Nada, A.M.; Al Lawati, J.; Al Lawati, N. Age at diagnosis of female breast cancer in Oman: Issues and implications. South Asian J. Cancer 2014, 3, 101–106. [Google Scholar] [CrossRef]
- Leventhal, H. Next Steps for examining the common-sense of health behaviour. Health Psychol. Rev. 2019, 13, 487–489. [Google Scholar] [CrossRef]
- DeLongis, A.; Morstead, T. Bringing the social context into research using the common-sense model. Health Psychol. Rev. 2019, 13, 481–483. [Google Scholar] [CrossRef]
| Variables | UAE | Portugal | t-Test | Signif. |
|---|---|---|---|---|
| Illness Perceptions (Range: 0–10) | Mean (sd) | Mean (sd) | (df; value) | p-value |
| Consequences | 8.13 (2.20) | 9.03 (1.79) | (571.8; −5.64) | <0.001 |
| Identity (symptoms) | 6.13 (2.56) | 6.66 (2.41) | (640; −2.69) | 0.007 |
| Timeline | 6.02 (1.79) | 6.97 (1.68) | (640; −6.90) | <0.001 |
| Personal control | 5.57 (2.36) | 6.20 (2.42) | (640; −3.30) | 0.001 |
| Treatment control | 3.14 (2.30) | 2.19 (1.78) | (556.3; 5.79) | <0.001 |
| Concern | 6.52 (2.69) | 7.88 (2.16) | (568.1; −6.97) | <0.001 |
| Coherence | 4.96 (2.53) | 4.17 (2.21) | (594.1; 4.18) | <0.001 |
| Emotional representation | 6.36 (2.93) | 7.20 (2.47) | (584.1; −3.92) | <0.001 |
| Risk Perception (Range: 0–10) | Mean (sd) | Mean (sd) | (df; value) | p-value |
| Individual perceived risk | 3.43 (2.47) | 5.40 (2.50) | (640; −9.99) | <0.001 |
| Compared risk | 3.30 (2.50) | 4.84 (2.49) | (640; −7.76) | <0.001 |
| Beliefs about preventive behaviors (Range: 0–10) | Mean (sd) | Mean (sd) | (df; value) | p-value |
| Healthy diet | 7.22 (2.80) | 7.65 (2.28) | (572.3; −2.09) | 0.037 |
| Non-smoker | 7.88 (2.80) | 7.86 (2.54) | (640; 0.093) | 0.926 |
| Not being overweight | 6.88 (2.96) | 7.13 (2.66) | (602.3; −1.12) | 0.263 |
| Physically active | 7.67 (2.65) | 7.97 (2.57) | (640; 0.087) | 0.931 |
| Breastfeeding | 5.28 (3.12) | 5.09 (3.15) | (640; 0.783) | 0.434 |
| Regular self-breast examination | 7.97 (2.57) | 9.18 (1.75) | (512.0; −6.83) | <0.001 |
| Routine screening (mammogram, clinical assessment) | 7.65 (2.65) | 9.04 (1.88) | (525.5; −7.54) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Figueiras, M.J.; Neto, D.D.; Marôco, J.; Carmo, C. How Do Healthy Women Perceive the Risk of Breast Cancer? The Role of Illness Perceptions and Compared Risk between Portugal and the U.A.E. Int. J. Environ. Res. Public Health 2022, 19, 12923. https://doi.org/10.3390/ijerph191912923
Figueiras MJ, Neto DD, Marôco J, Carmo C. How Do Healthy Women Perceive the Risk of Breast Cancer? The Role of Illness Perceptions and Compared Risk between Portugal and the U.A.E. International Journal of Environmental Research and Public Health. 2022; 19(19):12923. https://doi.org/10.3390/ijerph191912923
Chicago/Turabian StyleFigueiras, Maria J., David Dias Neto, Joao Marôco, and Catarina Carmo. 2022. "How Do Healthy Women Perceive the Risk of Breast Cancer? The Role of Illness Perceptions and Compared Risk between Portugal and the U.A.E" International Journal of Environmental Research and Public Health 19, no. 19: 12923. https://doi.org/10.3390/ijerph191912923
APA StyleFigueiras, M. J., Neto, D. D., Marôco, J., & Carmo, C. (2022). How Do Healthy Women Perceive the Risk of Breast Cancer? The Role of Illness Perceptions and Compared Risk between Portugal and the U.A.E. International Journal of Environmental Research and Public Health, 19(19), 12923. https://doi.org/10.3390/ijerph191912923







