Climate Change and Health in Urban Areas with a Mediterranean Climate: A Conceptual Framework with a Social and Climate Justice Approach
Abstract
:1. Introduction
2. Methods
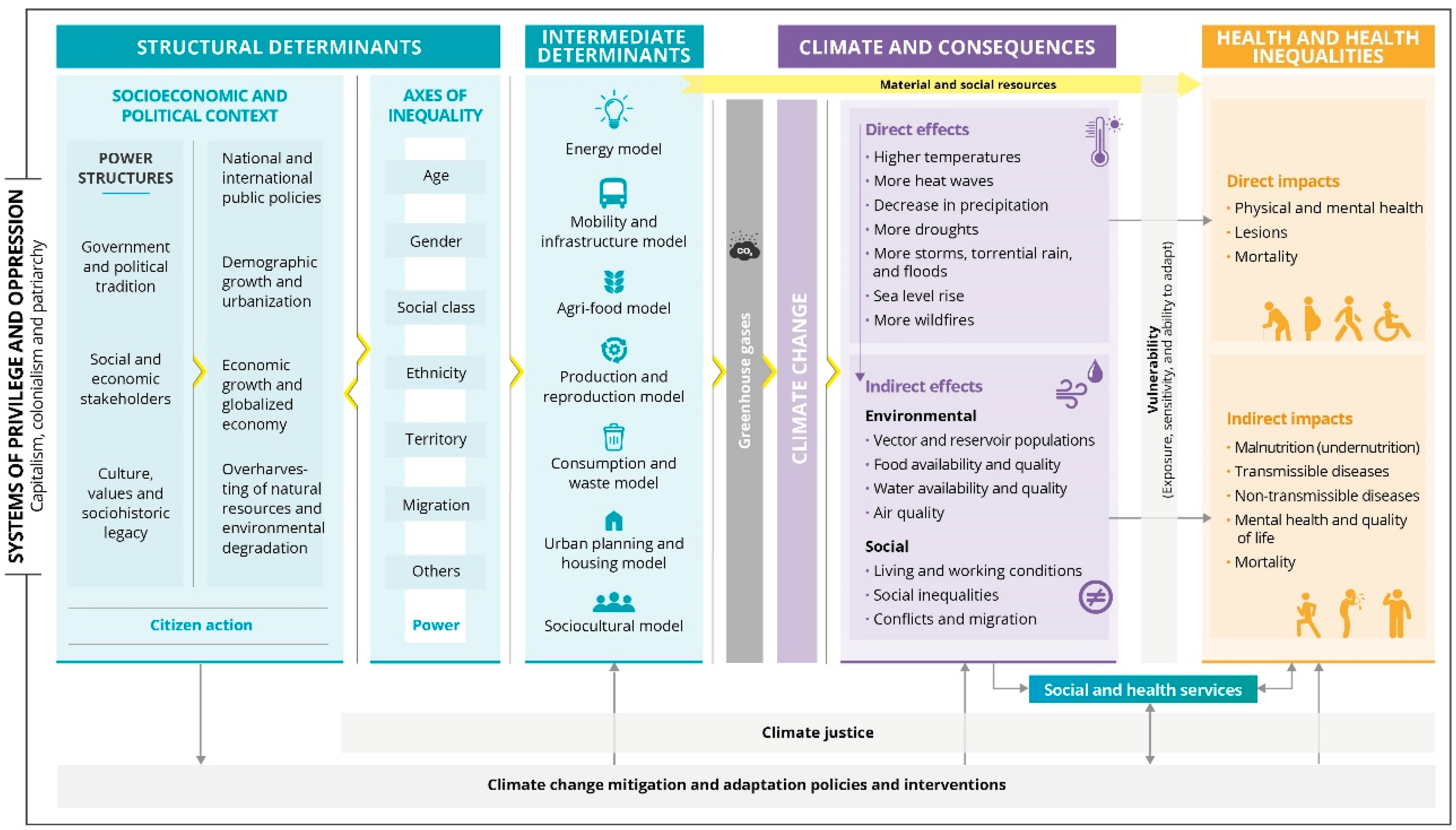
3. Description and Discussion of the Conceptual Framework
3.1. Systems of Privilege and Oppression
3.2. Structural Determinants
3.2.1. Socioeconomic and Political Context
3.2.2. Axes of Inequality
3.3. Intermediate Determinants
3.3.1. Greenhouse Gases
3.3.2. Material and Social Resources
3.4. Climate and Consequences
3.4.1. Direct Effects
3.4.2. Indirect Effects
Environmental Consequences
Social Consequences
3.5. Impacts on Health and Health Inequalities
3.5.1. Direct Impacts
3.5.2. Indirect Impacts
3.6. Vulnerability
3.7. Mitigation and Adaptation Policies and Interventions to Climate Change
3.7.1. Mitigation
3.7.2. Adaptation
3.8. Climate Justice
3.9. Social and Health Services
3.10. Conclusions and Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Acknowledgments
Conflicts of Interest
References
- Climate Emergency Declaration—Call to Declare a Climate Emergency. Available online: https://climateemergencydeclaration.org/ (accessed on 9 August 2022).
- Sheehan, M.C.; Khudairi, F.; Swaich, G.S.; Hines, W.; Mehta, S.; Fox, M.A. Urban climate-health governance: Charting the role of public health in large global city adaptation plans. PLoS Clim. 2022, 1, e0000012. [Google Scholar] [CrossRef]
- Villalbí, J.R.; Ventayol, I. Climate change and health in the urban context: The experience of Barcelona. Int. J. Health Serv. 2016, 46, 389–405. [Google Scholar] [CrossRef]
- Borrell, C.; Marí-Dell’Olmo, M.; Rodríguez-Sanz, M.; Garcia-Olalla, P.; Caylà, J.A.; Benach, J.; Muntaner, C. Socioeconomic position and excess mortality during the heat wave of 2003 in Barcelona. Eur. J. Epidemiol. 2006, 21, 633–640. [Google Scholar] [CrossRef]
- Vandentorren, S.; Bretin, P.; Zeghnoun, A.; Mandereau-Bruno, L.; Croisier, A.; Cochet, C.; Ribéron, J.; Siberan, I.; Declercq, B.; Ledrans, M. August 2003 Heat Wave in France: Risk Factors for Death of Elderly People Living at Home. Eur. J. Public Health 2006, 16, 583–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, H.; Kovats, S.; McGregor, G.; Stedman, J.; Gibbs, M.; Walton, H. The impact of the 2003 heat wave on daily mortality in England and Wales and the use of rapid weekly mortality estimates. Eurosurveillance 2005, 10, 15–16. [Google Scholar] [CrossRef]
- Brücker, G. Vulnerable populations: Lessons learnt from the summer 2003 heat waves in Europe. Euro Surveill. 2005, 10, 147. [Google Scholar] [CrossRef] [PubMed]
- Bezirtzoglou, C.; Dekas, K.; Charvalos, E. Climate changes, environment and infection: Facts, scenarios and growing awareness from the public health community within Europe. Anaerobe 2011, 17, 337–340. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J. Globalization, Climate Change, and Human Health. N. Engl. J. Med. 2013, 368, 1335–1343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watts, N.; Adger, W.N.; Agnolucci, P.; Blackstock, J.; Byass, P.; Cai, W.; Chaytor, S.; Colbourn, T.; Collins, M.; Cooper, A.; et al. Health and climate change: Policy responses to protect public health. Lancet 2015, 386, 1861–1914. [Google Scholar] [CrossRef]
- Boylan, S.; Beyer, K.; Schlosberg, D.; Mortimer, A.; Hime, N.; Scalley, B.; Alders, R.; Corvalan, C.; Capon, A. A conceptual framework for climate change, health and wellbeing in NSW, Australia. Public Health Res. Pract. 2018, 28, e2841826. [Google Scholar] [CrossRef] [PubMed]
- Crimmins, A.J.; Balbus, J.L.; Gamble, C.B.; Beard, J.E.; Bell, D.; Dodgen, R.J.; Eisen, N.; Fann, M.D.; Hawkins, S.C.; Herring, H.; et al. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; Global Change Research Program: Washington, DC, USA, 2016. [CrossRef] [Green Version]
- Füssel, H.-M.; Klein, R.J.T. PIK Report; Postdam Institute for Climate Impact Research: Potsdam, Germany, 2004. [Google Scholar]
- Hambling, T.; Weinstein, P.; Slaney, D. A Review of Frameworks for Developing Environmental Health Indicators for Climate Change and Health. Int. J. Environ. Res. Public Health 2011, 8, 2854–2875. [Google Scholar] [CrossRef]
- Barata, M.; Ligeti, E.; De Simone, G.; Dickinson, T.; Jack, D.; Penney, J.; Rahman, M.; Zimmerman, R. Climate change and human health in cities. In Cities And Climate Change—First Assessment Report of the Urban Climate Change Research Network; Rosenzweig, C., Solecki, W.D., Hammer, S.A., Mehrotra, E.S., Eds.; Cambridge University Press: Cambridge, UK, 2011; pp. 179–213. [Google Scholar]
- Dallman, P.R. Plant Life in the World’s Mediterranean Climates: California, Chile, South Africa, Australia, and the Mediterranean Basin; University of California Press: Los Angeles, CA, USA, 1998. [Google Scholar]
- Paz, S.; Negev, M.; Clermont, A.; Green, M. Health Aspects of Climate Change in Cities with Mediterranean Climate, and Local Adaptation Plans. Int. J. Environ. Res. Public Health 2016, 13, 438. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Environmental Programme Climate Change in the Mediterranean. Available online: https://www.unep.org/unepmap/resources/factsheets/climate-change (accessed on 27 July 2022).
- Mavromatidi, A.; Briche, E.; Claeys, C. Mapping and analyzing socio-environmental vulnerability to coastal hazards induced by climate change: An application to coastal Mediterranean cities in France. Cities 2018, 72, 189–200. [Google Scholar] [CrossRef]
- Moreira, F.; Viedma, O.; Arianoutsou, M.; Curt, T.; Koutsias, N.; Rigolot, E.; Barbati, A.; Corona, P.; Vaz, P.; Xanthopoulos, G.; et al. Landscape—Wildfire interactions in southern Europe: Implications for landscape management. J. Environ. Manag. 2011, 92, 2389–2402. [Google Scholar] [CrossRef] [Green Version]
- Cramer, W.; Marini, K.; Guiot, J. Climate and Environmental Change in the Mediterranean Basin—Current Situation and Risks for the Future, First Mediterranean Assessment Report (MAR1); Union for the Mediterranean, Plan Bleu, UNEP/MAP: Marseille, France, 2020. [Google Scholar]
- United Nations Department of Economic and Social Affairs. World Urbanization Prospects. The 2018 Revision; United Nations Department of Economic and Social Affairs: New York, NY, USA, 2019. [Google Scholar]
- Buma, B. Disturbance interactions: Characterization, prediction, and the potential for cascading effects. Ecosphere 2015, 6, 1–15. [Google Scholar] [CrossRef]
- Reiter, P. Climate change and mosquito-borne disease. Environ. Health Perspect. 2001, 109, 141–161. [Google Scholar] [CrossRef] [Green Version]
- Borrell, C.; Pons-Vigués, M.; Morrison, J.; Díez, È. Factors and processes influencing health inequalities in urban areas. J. Epidemiol. Community Health 2013, 67, 389–391. [Google Scholar] [CrossRef]
- Mercuriali, L.; Oliveras, L.; Marí, M.; Gómez, A.; Montalvo, T.; García-Rodríguez, A.; Pérez, G.; Villalbí, J.R. Un sistema de vigilancia de salud pública para el cambio climático en las ciudades. Gac. Sanit. 2022, 36, 283–286. [Google Scholar] [CrossRef]
- Marí-Dell’Olmo, M.; Sheehan, M.C.; Villalbí, J.R. Planning for Climate Change Workshop: Final Report; Agència de Salut Pública de Barcelona; Johns Hopkins University School of Public Health; Universitat Pompeu Fabra: Barcelona, Spain, 2019. [Google Scholar]
- Solar, O.; Irwin, A. A conceptual Framework for Action on the Social Determinants of Health, Social Determinants of Health Discussion Paper 2 (Policy and Practice); World Health Organization: Genva, Switzerland, 2010; ISBN 9789241500852. [Google Scholar]
- Borrell, C.; Malmusi, D.; Artazcoz, L.; Diez, E.; Rodríguez-Sanz, I.P.; Campos, P.; Merino, B.; Ramírez, R.; Benach, J.; Escolar, A.; et al. Propuesta de políticas e intervenciones para reducir las desigualdades sociales en salud en España. Gac. Sanit. 2012, 26, 182–189. [Google Scholar] [CrossRef]
- Krieger, N. Measures of racism, sexism, heterosexism, and gender binarism for health equity research: From structural injustice to embodied harm-an ecosocial analysis. Annu. Rev. Public Health 2019, 41, 37–62. [Google Scholar] [CrossRef] [Green Version]
- Breilh, J. Epidemiología crítica. In Ciencia Emancipadora e Interculturalidad; Lugar Editorial: Buenos Aires, Argentina, 2003; ISBN 950-892147. [Google Scholar]
- Ajuntament de Barcelona. Això No és un Simulacre. Declaració D’emergència Climàtica; Ajuntament de Barcelona: Barcelona, Spain, 2020. [Google Scholar]
- Eijgelaar, E.; Thaper, C.; Peeters, P. Antarctic cruise tourism: The paradoxes of ambassadorship, “last chance tourism” and greenhouse gas emissions. J. Sustain. Tour. 2010, 18, 337–354. [Google Scholar] [CrossRef]
- United Nations Environmental Programme Cruising and Recreational Boating in the Mediterranean. Available online: https://planbleu.org/en/page-theme/cruises-and-boating-in-the-mediterranean/ (accessed on 9 August 2022).
- Roundtable Human Rights in Tourism Human Rights in Tourism. Available online: https://www.humanrights-in-tourism.net/card/136 (accessed on 9 August 2022).
- Ruiz-Guerra, I.; Molina-Moreno, V.; Cortés-García, F.J.; Núñez-Cacho, P. Prediction of the impact on air quality of the cities receiving cruise tourism: The case of the Port of Barcelona. Heliyon 2019, 5, e01280. [Google Scholar] [CrossRef] [Green Version]
- Maragkogianni, A.; Papaefthimiou, S. Evaluating the social cost of cruise ships air emissions in major ports of Greece. Transp. Res. Part D Transp. Environ. 2015, 36, 10–17. [Google Scholar] [CrossRef]
- United Nations Humann Settlement Programme. Cities and Climate Change; Routledge: London, UK, 2013; ISBN 9781135130121. [Google Scholar]
- Scheffran, J. The Geopolitical Impact of Climate Change in the Mediterranean Region: Climate Change as a Trigger of Conflict and Migration. In European Institute of the Mediterranean Yearbook; IEMed: Barcelona, Spain, 2020. [Google Scholar]
- Thiri, M.A.; Villamayor-Tomás, S.; Scheidel, A.; Demaria, F. How social movements contribute to staying within the global carbon budget: Evidence from a qualitative meta-analysis of case studies. Ecol. Econ. 2022, 195, 107356. [Google Scholar] [CrossRef]
- Erickson, P.; Lazarus, M.; Piggot, G. Limiting fossil fuel production as the next big step in climate policy. Nat. Clim. Chang. 2018, 8, 1037–1043. [Google Scholar] [CrossRef]
- Ivanova, D.; Wood, R. The unequal distribution of household carbon footprints in Europe and its link to sustainability. Glob. Sustain. 2020, 3, e18. [Google Scholar] [CrossRef]
- Adua, L. Super polluters and carbon emissions: Spotlighting how higher-income and wealthier households disproportionately despoil our atmospheric commons. Energy Policy 2022, 162, 112768. [Google Scholar] [CrossRef]
- Oliveras, L.; Artazcoz, L.; Borrell, C.; Palència, L.; López, M.J.; Gotsens, M.; Peralta, A.; Marí-Dell’Olmo, M. The association of energy poverty with health, health care utilisation and medication use in southern Europe. SSM-Popul. Health 2020, 12, 100665. [Google Scholar] [CrossRef] [PubMed]
- Negev, M.; Zohar, M.; Paz, S. Multidimensional hazards, vulnerabilities, and perceived risks regarding climate change and Covid-19 at the city level: An empirical study from Haifa, Israel. Urban Clim. 2022, 43, 101146. [Google Scholar] [CrossRef]
- Anguelovski, I.; Connolly, J.; Brand, A.L. From landscapes of utopia to the margins of the green urban life: For whom is the new green city? City 2018, 22, 417–436. [Google Scholar] [CrossRef] [Green Version]
- Bowleg, L. The problem with the phrase women and minorities: Intersectionality-an important theoretical framework for public health. Am. J. Public Health 2012, 102, 1267–1273. [Google Scholar] [CrossRef] [PubMed]
- European Comission Eurostat Life Expectancy across EU Regions in 2020. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20220427-1 (accessed on 9 August 2022).
- The World Bank Data. Population Ages 65 and Above. Available online: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?locations=IT&most_recent_value_desc=true (accessed on 9 August 2022).
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- Food and Agriculture Organization. Food Wastage Footprint & Climate Change; FAO: Rome, Italy, 2015; pp. 1–4. [Google Scholar]
- IPCC. Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change; Masson-Delmotte, V., Zhai, P., Pirani, A., Connors, S.L., Péan, C., Berger, S., Caud, N., Chen, Y., Goldfarb, L., Gomis, M.I., et al., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2021; 2391p. [Google Scholar] [CrossRef]
- Hess, J.; Boodram, L.-L.G.; Paz, S.; Stewart Ibarra, A.M.; Wasserheit, J.N.; Lowe, R. Strengthening the global response to climate change and infectious disease threats. BMJ 2020, 371, m3081. [Google Scholar] [CrossRef] [PubMed]
- Gage, K.L.; Burkot, T.R.; Eisen, R.J.; Hayes, E.B. Climate and Vectorborne Diseases. Am. J. Prev. Med. 2008, 35, 436–450. [Google Scholar] [CrossRef] [PubMed]
- Rogers, D.J.; Packer, M.J. Vector-borne diseases, models, and global change. Lancet 1993, 342, 1282–1284. [Google Scholar] [CrossRef]
- Succo, T.; Leparc-Goffart, I.; Ferré, J.-B.; Roiz, D.; Broche, B.; Maquart, M.; Noel, H.; Catelinois, O.; Entezam, F.; Caire, D.; et al. Autochthonous dengue outbreak in Nîmes, South of France, July to September 2015. Eurosurveillance 2016, 21, 30240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bordi, L.; Carletti, F.; Lalle, E.; Colavita, F.; Meschi, S.; Di Caro, A.; Nicastri, E.; Scognamiglio, P.; Vairo, F.; Di Lallo, D.; et al. Molecular Characterization of Autochthonous Chikungunya Cluster in Latium Region, Italy. Emerg. Infect. Dis. 2018, 24, 178–180. [Google Scholar] [CrossRef] [Green Version]
- Angelini, R.; Finarelli, A.C.; Angelini, P.; Po, C.; Petropulacos, K.; Macini, P.; Fiorentini, C.; Fortuna, C.; Venturi, G.; Romi, R.; et al. An outbreak of chikungunya fever in the province of Ravenna, Italy. Wkly. Releases 2007, 12, 3260. [Google Scholar] [CrossRef]
- Engler, O.; Savini, G.; Papa, A.; Figuerola, J.; Groschup, M.; Kampen, H.; Medlock, J.; Vaux, A.; Wilson, A.; Werner, D.; et al. European Surveillance for West Nile Virus in Mosquito Populations. Int. J. Environ. Res. Public Health 2013, 10, 4869–4895. [Google Scholar] [CrossRef] [Green Version]
- Keesing, F.; Belden, L.K.; Daszak, P.; Dobson, A.; Harvell, C.D.; Holt, R.D.; Hudson, P.; Jolles, A.; Jones, K.E.; Mitchell, C.E.; et al. Impacts of biodiversity on the emergence and transmission of infectious diseases. Nature 2010, 468, 647–652. [Google Scholar] [CrossRef]
- Paz, S.; Majeed, A.; Christophides, G.K. Climate change impacts on infectious diseases in the Eastern Mediterranean and the Middle East (EMME)—Risks and recommendations. Clim. Chang. 2021, 169, 40. [Google Scholar] [CrossRef] [PubMed]
- Calvo, E.; Simó, R.; Coma, R.; Ribes, M.; Pascual, J.; Sabatés, A.; Gili, J.M.; Pelejero, C. Effects of climate change on Mediterranean marine ecosystems: The case of the Catalan Sea. Clim. Res. 2011, 50, 1–29. [Google Scholar] [CrossRef] [Green Version]
- Lacoue-Labarthe, T.; Nunes, P.A.L.D.; Ziveri, P.; Cinar, M.; Gazeau, F.; Hall-Spencer, J.M.; Hilmi, N.; Moschella, P.; Safa, A.; Sauzade, D.; et al. Impacts of ocean acidification in a warming Mediterranean Sea: An overview. Reg. Stud. Mar. Sci. 2016, 5, 1–11. [Google Scholar] [CrossRef] [Green Version]
- D’Amato, G.; Baena-Cagnani, C.E.; Cecchi, L.; Annesi-Maesano, I.; Nunes, C.; Ansotegui, I.; D’Amato, M.; Liccardi, G.; Sofia, M.; Canonica, W.G. Climate change, air pollution and extreme events leading to increasing prevalence of allergic respiratory diseases. Multidiscip. Respir. Med. 2013, 8, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Environmental Agency. Air Quality in Europe: 2021 Report. Available online: https://www.eea.europa.eu/publications/air-quality-in-europe-2021 (accessed on 9 August 2022).
- Pey, J.; Querol, X.; Alastuey, A.; Forastiere, F.; Stafoggia, M. African dust outbreaks over the Mediterranean Basin during 2001–2011: PM10 concentrations, phenomenology and trends, and its relation with synoptic and mesoscale meteorology. Atmos. Chem. Phys. 2013, 13, 1395–1410. [Google Scholar] [CrossRef] [Green Version]
- International Labour Organization. Working on a Warmer Planet. The Impact of Heat Stress on Labour Productivity and Decent Work; International Labour Organization: Geneva, Switzerland, 2019; ISBN 9789221329671. [Google Scholar]
- Fatima, S.H.; Rothmore, P.; Giles, L.C.; Varghese, B.M.; Bi, P. Extreme heat and occupational injuries in different climate zones: A systematic review and meta-analysis of epidemiological evidence. Environ. Int. 2021, 148, 106384. [Google Scholar] [CrossRef]
- Enríquez, A.R.; Marcos, M.; Álvarez-Ellacuría, A.; Orfila, A.; Gomis, D. Changes in beach shoreline due to sea level rise and waves under climate change scenarios: Application to the Balearic Islands (western Mediterranean). Nat. Hazards Earth Syst. Sci. 2017, 17, 1075–1089. [Google Scholar] [CrossRef] [Green Version]
- Hein, L.; Metzger, M.J.; Moreno, A. Potential impacts of climate change on tourism; a case study for Spain. Curr. Opin. Environ. Sustain. 2009, 1, 170–178. [Google Scholar] [CrossRef]
- Linares, C.; Díaz, J.; Negev, M.; Martínez, G.S.; Debono, R.; Paz, S. Impacts of climate change on the public health of the Mediterranean Basin population—Current situation, projections, preparedness and adaptation. Environ. Res. 2020, 182, 109107. [Google Scholar] [CrossRef]
- Carnicer, J.; Georgopoulou, E.; Hilmi, N.; Le Cozannet, G.; Lionello, P. IPCC WGII Sixth Assessment Report. FINAL DRAFT Cross-Chapter Paper 4 IPCC WGII Sixth Assessment Report Do Not Cite, Quote or Distribute CCP4-1 Total pages: 50 1 Cross-Chapter Paper 4: Mediterranean Region. Available online: https://report.ipcc.ch/ar6wg2/pdf/IPCC_AR6_WGII_CrossChapterPaper4.pdf (accessed on 9 August 2022).
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Solano Rodriguez, B.; Arnell, N.; et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021, 398, 1619–1662. [Google Scholar] [CrossRef]
- World Health Organization. COP24 Special Report: Health and Climate Change; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Patz, J.A.; McGeehin, M.A.; Bernard, S.M.; Ebi, K.L.; Epstein, P.R.; Grambsch, A.; Gubler, D.J.; Reiter, P.; Romieu, I.; Rose, J.B.; et al. The potential health impacts of climate variability and change for the United States: Executive summary of the report of the health sector of the U.S. national assessment. Environ. Health Perspect. 2000, 108, 367–376. [Google Scholar] [CrossRef]
- Gasparrini, A.; Guo, Y.; Sera, F.; Vicedo-Cabrera, A.M.; Huber, V.; Tong, S.; de Sousa Zanotti Stagliorio Coelho, M.; Nascimento Saldiva, P.H.; Lavigne, E.; Matus Correa, P.; et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 2017, 1, e360–e367. [Google Scholar] [CrossRef]
- Marí-Dell’Olmo, M.; Tobías, A.; Gómez-Gutiérrez, A.; Rodríguez-Sanz, M.; García de Olalla, P.; Camprubí, E.; Gasparrini, A.; Borrell, C. Social inequalities in the association between temperature and mortality in a South European context. Int. J. Public Health 2019, 64, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.; Patz, J. Climate Change and Public Health; Oxford University Press: Oxford, UK, 2015; ISBN 9780190202453. [Google Scholar]
- Dodgen, D.; Donato, D.; Kelly, N.; La Greca, A.; Morganstein, J.; Reser, J.; Ruzek, J.; Schweitzer, S.; Shimamoto, M.M.; Thigpen Tart, K.; et al. Chapter 8: Mental Health and Well-Being. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 217–246. [Google Scholar]
- Fountoulakis, K.N.; Savopoulos, C.; Zannis, P.; Apostolopoulou, M.; Fountoukidis, I.; Kakaletsis, N.; Kanellos, I.; Dimellis, D.; Hyphantis, T.; Tsikerdekis, A.; et al. Climate change but not unemployment explains the changing suicidality in Thessaloniki Greece (2000–2012). J. Affect. Disord. 2016, 193, 331–338. [Google Scholar] [CrossRef]
- Cheng, S.; Plouffe, R.; Nanos, S.M.; Qamar, M.; Fisman, D.N.; Soucy, J.P.R. The effect of average temperature on suicide rates in five urban California counties, 1999–2019: An ecological time series analysis. BMC Public Health 2021, 21, 974. [Google Scholar] [CrossRef] [PubMed]
- Cervellin, G.; Comelli, I.; Lippi, G.; Comelli, D.; Rastelli, G.; Ossola, P.; Marchesi, C. The number of emergency department visits for psychiatric emergencies is strongly associated with mean temperature and humidity variations. Results of a nine year survey. Emerg. Care J. 2014, 10, 2271. [Google Scholar] [CrossRef] [Green Version]
- Klinenberg, E. Heat Wave: A Social Autopsy of Disaster in Chicago, 2nd ed.; University of Chicago Press: Chicago, IL, USA, 2015; ISBN 9780226276182. [Google Scholar]
- Kovats, R.S.; Edwards, S.J.; Hajat, S.; Armstrong, B.G.; Ebi, K.L.; Menne, B.; Cowden, J.; Gerner-Smidt, P.; Hernández Pezzi, G.; Kristufkova, Z.; et al. The effect of temperature on food poisoning: A time-series analysis of salmonellosis in ten European countries. Epidemiol. Infect. 2004, 132, 443–453. [Google Scholar] [CrossRef]
- Lo Iacono, G.; Armstrong, B.; Fleming, L.E.; Elson, R.; Kovats, S.; Vardoulakis, S.; Nichols, G.L. Challenges in developing methods for quantifying the effects of weather and climate on water-associated diseases: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005659. [Google Scholar] [CrossRef]
- Cherrie, M.P.C.; Nichols, G.; Iacono, G.L.; Sarran, C.; Hajat, S.; Fleming, L.E. Pathogen seasonality and links with weather in England and Wales: A big data time series analysis David Stieb, Cecile Boot, Michelle Turner, Osmar Zaiane. BMC Public Health 2018, 18, 1067. [Google Scholar] [CrossRef] [Green Version]
- Ikeda, T.; Behera, S.K.; Morioka, Y.; Minakawa, N.; Hashizume, M.; Tsuzuki, A.; Maharaj, R.; Kruger, P. Seasonally lagged effects of climatic factors on malaria incidence in South Africa. Sci. Rep. 2017, 7, 2458. [Google Scholar] [CrossRef] [Green Version]
- Semenza, J.C.; Menne, B. Climate change and infectious diseases in Europe. Lancet Infect. Dis. 2009, 9, 365–375. [Google Scholar] [CrossRef]
- Paavola, J. Health impacts of climate change and health and social inequalities in the UK. Environ. Health A Glob. Access Sci. Source 2017, 16, 61–68. [Google Scholar] [CrossRef]
- Cariñanos, P.; Grilo, F.; Pinho, P.; Casares-Porcel, M.; Branquinho, C.; Acil, N.; Andreucci, M.B.; Anjos, A.; Bianco, P.M.; Brini, S.; et al. Estimation of the allergenic potential of urban trees and urban parks: Towards the healthy design of urban green spaces of the future. Int. J. Environ. Res. Public Health 2019, 16, 1357. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Recio, M.; Picornell, A.; Trigo, M.M.; Gharbi, D.; García-Sánchez, J.; Cabezudo, B. Intensity and temporality of airborne Quercus pollen in the southwest Mediterranean area: Correlation with meteorological and phenoclimatic variables, trends and possible adaptation to climate change. Agric. For. Meteorol. 2018, 250–251, 308–318. [Google Scholar] [CrossRef]
- Hickman, C.; Marks, E.; Pihkala, P.; Clayton, S.; Lewandowski, R.E.; Mayall, E.E.; Wray, B.; Mellor, C.; van Susteren, L. Climate anxiety in children and young people and their beliefs about government responses to climate change: A global survey. Lancet Planet. Health 2021, 5, e863–e873. [Google Scholar] [CrossRef]
- Agència de Salut Pública de Barcelona. La Salut i els Seus Determinants en L’alumnat Adolescent de Barcelona; Agència de Salut Pública de Barcelona: Barcelona, Spain, 2021; pp. 1–265. [Google Scholar]
- Adger, W.N. Vulnerability. Glob. Environ. Chang. 2006, 16, 268–281. [Google Scholar] [CrossRef]
- Balbus, J.M.; Malina, C. Identifying Vulnerable Subpopulations for Climate Change Health Effects in the United States. J. Occup. Environ. Med. 2009, 51, 33–37. [Google Scholar] [CrossRef]
- Buse, C.G.; Patrick, R. Climate change glossary for public health practice: From vulnerability to climate justice. J. Epidemiol. Community Health 2020, 74, 867–871. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Panel on Climate Change. Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Intergovernmental Panel on Climate Change: Geneva, Switzerland, 2014; ISBN 9789291691432. [Google Scholar]
- Recalde, M.; Peralta, A.; Oliveras, L.; Tirado-Herrero, S.; Borrell, C.; Palència, L.; Gotsens, M.; Artazcoz, L.; Marí-Dell’Olmo, M. Structural energy poverty vulnerability and excess winter mortality in the European Union: Exploring the association between structural determinants and health. Energy Policy 2019, 133, 110869. [Google Scholar] [CrossRef]
- Chiabai, A.; Quiroga, S.; Martinez-Juarez, P.; Higgins, S.; Taylor, T. The nexus between climate change, ecosystem services and human health: Towards a conceptual framework. Sci. Total Environ. 2018, 635, 1191–1204. [Google Scholar] [CrossRef]
- Haines, A.; Wilkinson, P.; Tonne, C.; Roberts, I. Aligning climate change and public health policies. Lancet 2009, 374, 2035–2038. [Google Scholar] [CrossRef]
- Harlan, S.L.; Pellow, D.N.; Roberts, J.T.; Bell, S.E.; Holt, W.G.; Nagel, J. Climate Justice and Inequality. In Climate Change and Society; Oxford University Press: Oxford, UK, 2015; pp. 127–163. [Google Scholar]
- Boyce, J.K.; Pastor, M. Clearing the air: Incorporating air quality and environmental justice into climate policy. Clim. Chang. 2013, 120, 801–814. [Google Scholar] [CrossRef]
- Forman, F.; Solomon, G.; Morello-Frosch, R.; Pezzoli, K. Chapter 8. Bending the Curve and Closing the Gap: Climate Justice and Public Health. Collabra 2016, 2, 22. [Google Scholar] [CrossRef] [Green Version]
- Schlosberg, D.; Collins, L.B. From environmental to climate justice: Climate change and the discourse of environmental justice. WIREs Clim. Chang. 2014, 5, 359–374. [Google Scholar] [CrossRef]
- Ebi, K.L. Facilitating Climate Justice through Community-Based Adaptation in the Health Sector. Environ. Justice 2009, 2, 191–195. [Google Scholar] [CrossRef]
- Oven, K.J.; Curtis, S.E.; Reaney, S.; Riva, M.; Stewart, M.G.; Ohlemüller, R.; Dunn, C.E.; Nodwell, S.; Dominelli, L.; Holden, R. Climate change and health and social care: Defining future hazard, vulnerability and risk for infrastructure systems supporting older people’s health care in England. Appl. Geogr. 2012, 33, 16–24. [Google Scholar] [CrossRef]
- Curtis, S.; Fair, A.; Wistow, J.; Val, D.V.; Oven, K. Impact of extreme weather events and climate change for health and social care systems. Environ. Health 2017, 16, 128. [Google Scholar] [CrossRef] [Green Version]
- Pencheon, D. Health services and climate change: What can be done? J. Health Serv. Res. Policy 2009, 14, 2–4. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marí-Dell’Olmo, M.; Oliveras, L.; Barón-Miras, L.E.; Borrell, C.; Montalvo, T.; Ariza, C.; Ventayol, I.; Mercuriali, L.; Sheehan, M.; Gómez-Gutiérrez, A.; et al. Climate Change and Health in Urban Areas with a Mediterranean Climate: A Conceptual Framework with a Social and Climate Justice Approach. Int. J. Environ. Res. Public Health 2022, 19, 12764. https://doi.org/10.3390/ijerph191912764
Marí-Dell’Olmo M, Oliveras L, Barón-Miras LE, Borrell C, Montalvo T, Ariza C, Ventayol I, Mercuriali L, Sheehan M, Gómez-Gutiérrez A, et al. Climate Change and Health in Urban Areas with a Mediterranean Climate: A Conceptual Framework with a Social and Climate Justice Approach. International Journal of Environmental Research and Public Health. 2022; 19(19):12764. https://doi.org/10.3390/ijerph191912764
Chicago/Turabian StyleMarí-Dell’Olmo, Marc, Laura Oliveras, Lourdes Estefanía Barón-Miras, Carme Borrell, Tomás Montalvo, Carles Ariza, Irma Ventayol, Lilas Mercuriali, Mary Sheehan, Anna Gómez-Gutiérrez, and et al. 2022. "Climate Change and Health in Urban Areas with a Mediterranean Climate: A Conceptual Framework with a Social and Climate Justice Approach" International Journal of Environmental Research and Public Health 19, no. 19: 12764. https://doi.org/10.3390/ijerph191912764




