Exercise Selection and Common Injuries in Fitness Centers: A Systematic Integrative Review and Practical Recommendations
Abstract
:1. Introduction
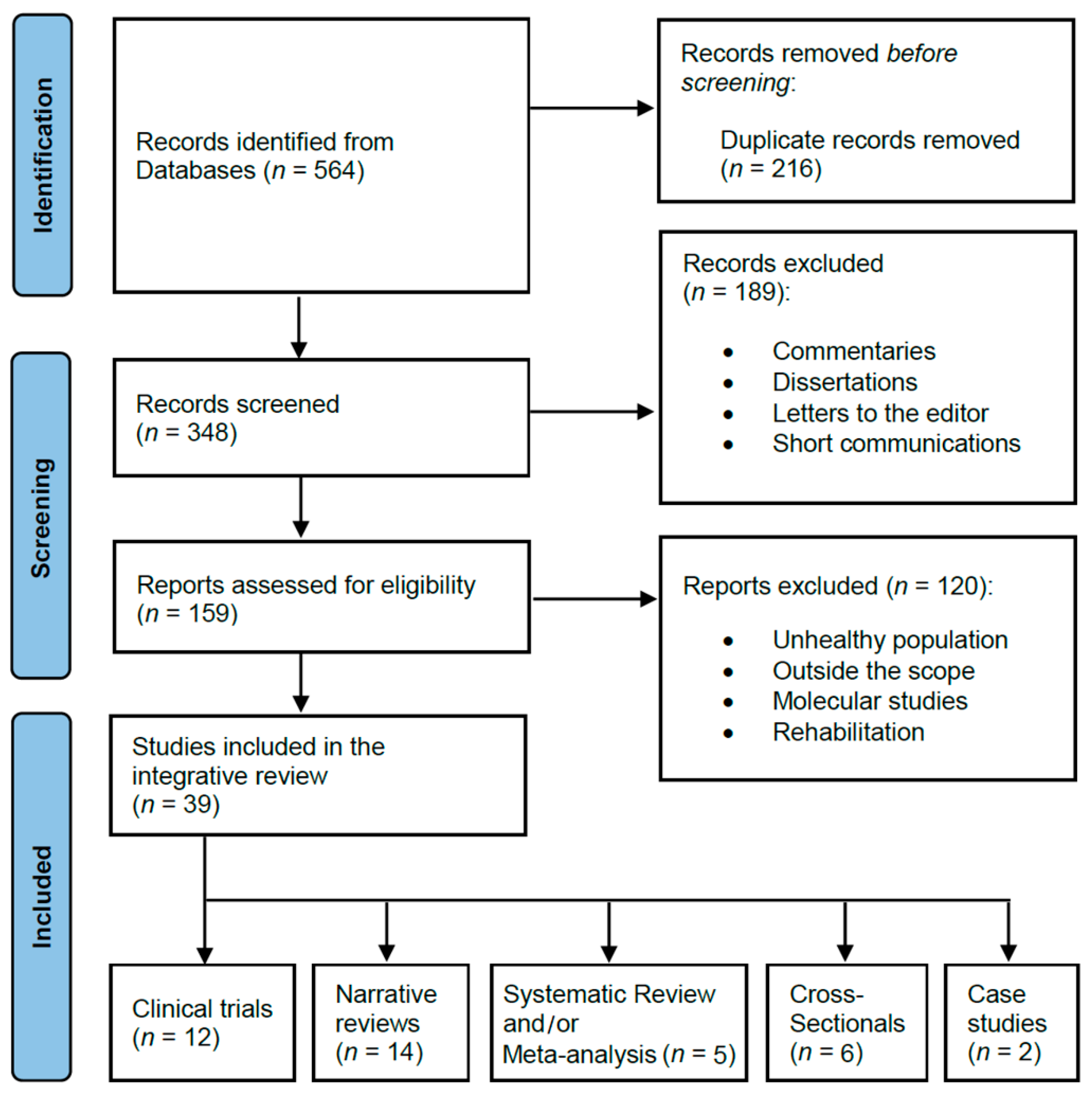
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
2.4. Study Selection and Data Collection Process
3. Results
4. Discussion
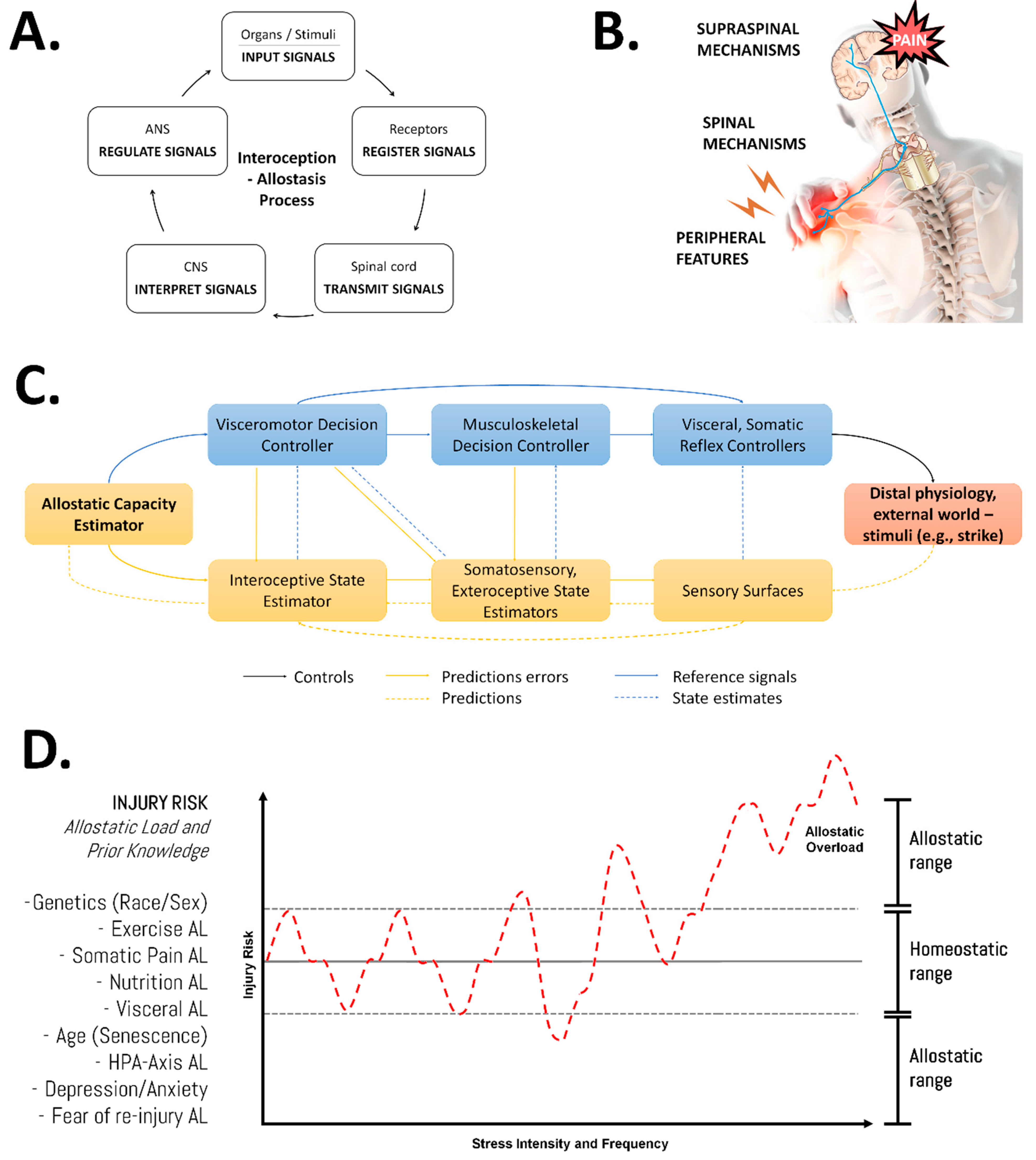
4.1. Underlying Factors
4.2. Exercise Modifications
4.3. Practical Recommendations
- Establish the objectives prior to the start of the weight RT program and opt for a non-linear (undulating) periodization model ordering the exercises to be implemented. Undulating periodization of RT has been shown to be more effective than a linear approach to increase strength and body composition in several populations [114,115,116,117].
- Consider all training variables that directly impact the targeted phenotype, regardless of the work demand by large or small muscle groups. Refer to Rosa et al. (2022) for a recent meta-analysis on the comparison of the effectiveness of single versus multijoint resistance exercises on muscle hypertrophy [118].
- Dedicate familiarization training sessions for teaching, observing, or correcting exercise techniques. This needs to be done independently of the experience level of the athletes or exercisers and the resistance to be used (machines, free weights, suspension).
- The principle of safety in RT indicates that the exercises selected must preserve the integrity and health of the subjects. Start from easy to more complex exercises (from machines to free weights with low load) or those that require greater control (free weights with moderate-to-high loads or suspension RT).
- To reduce the risk of injuries, ask for any pre-existing injuries or medical conditions, monitor for fatigue, and modify or eliminate suboptimal movement patterns or exercises entirely in persons not capable of performing them [60].
- The exercises selected should consider all of the muscles and joints involved in the biomechanical movement, avoiding methodological errors such as prescribing the “bench press” for the exclusive development of the pectoralis. All muscles involved in each exercise should be analyzed for a correct prescription, thereby avoiding overuse injuries in certain body regions [41,58].
- Precondition the muscle regions involved in sequential exercises (derived from weightlifting) with pulling or pushing exercises.
- Prioritize movements that require large muscle groups at the beginning of the session. In this sense, fitness practitioners should perform the most demanding, challenging exercises early in their training sessions and should avoid tiredness, fatigue, technical errors, and excessive overload [43].
- Although further research is warranted, practitioners should be aware of the role of myofascial fasciae and muscle chains involved in human movement to avoid incorrect body positions. Readers are encouraged to read a recent systematic review on exercise interventions to improve postural problems [119].
- The exercises selected should obey the optimal range of motion of the joints involved, avoiding overloading the joint limits.
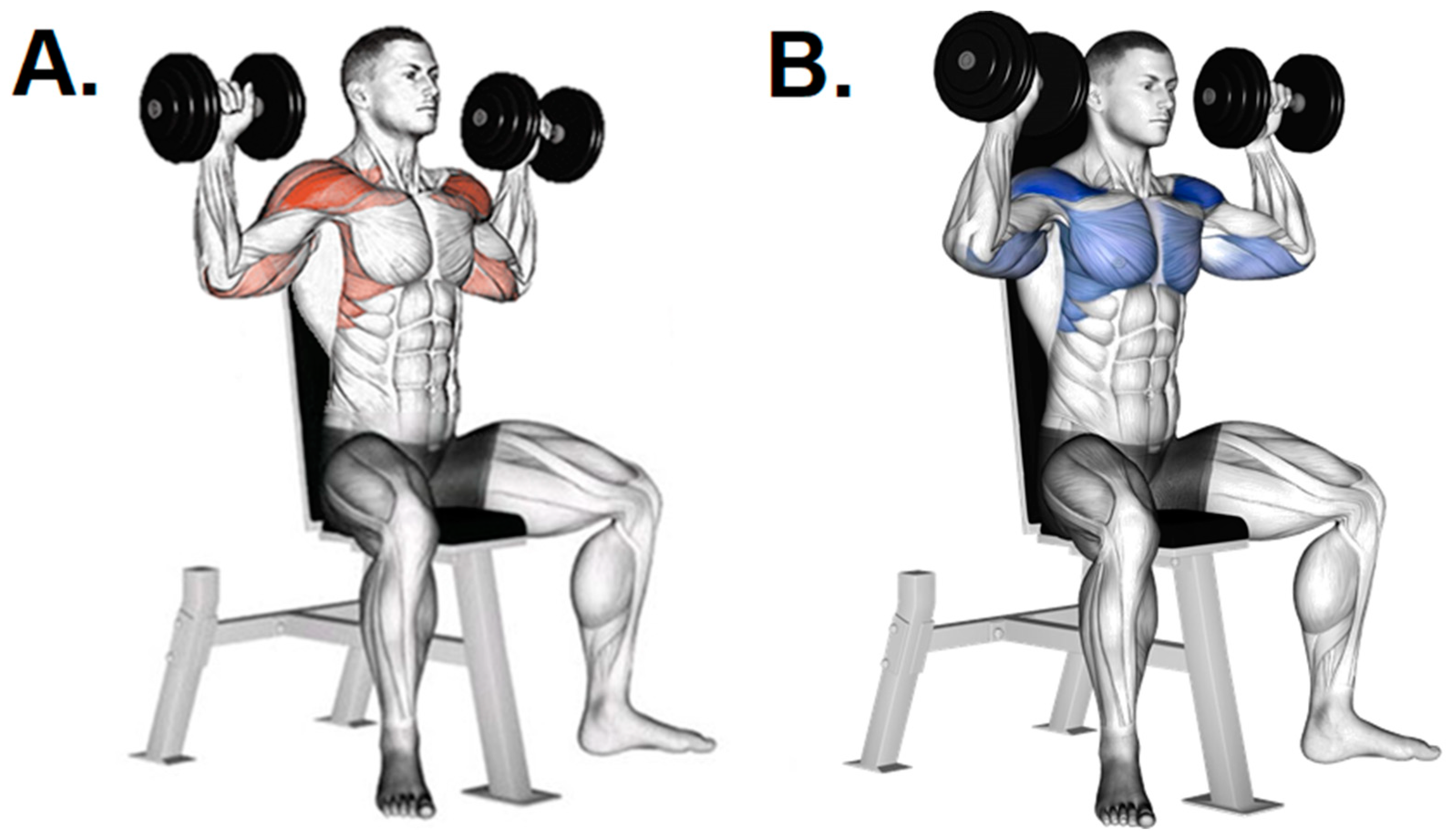
- Due to the frequent reinforcement in RT of the imbalance of the external rotators and scapulothoracic muscles to the internal rotators at the shoulder, besides the stretching of the internal rotators, the incorporation of exercises to strengthen the lower trapezius, scapulothoracic muscles, and external rotators might mitigate common strength imbalances (anterior shoulder instability) and pain.
- To prevent frequent RT-induced shoulder disorders the end-range “high-five” position (upper arm in 90° abduction, elbow in 90° flexion, and terminal external rotation of the shoulder) should be avoided [33,41]. Therefore, practitioners are encouraged to select exercises that require bringing the bar to the front of the torso (latissimus pull-downs or barbell presses to the front) instead of behind the neck.
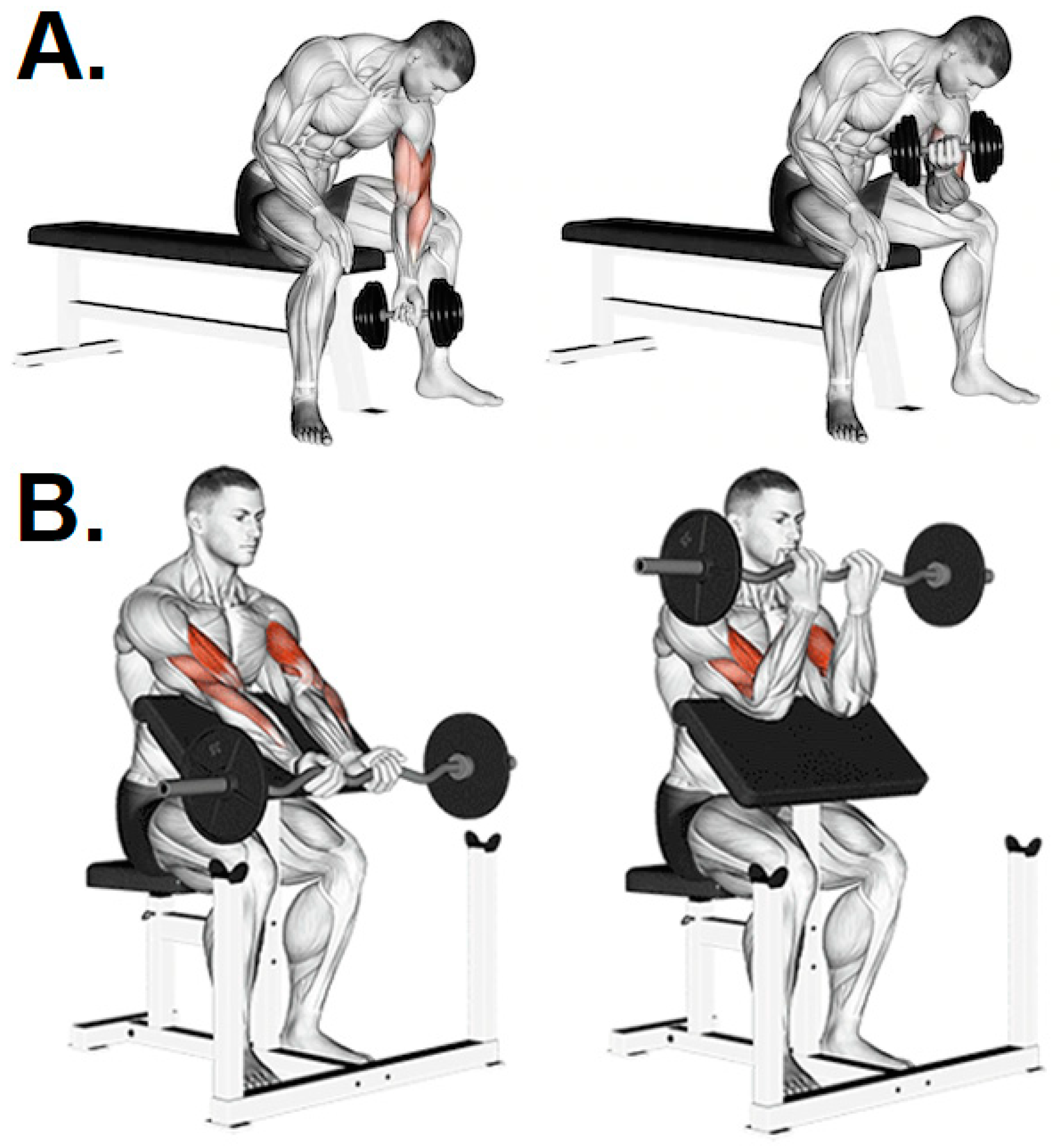
- In case of musculoskeletal discomfort when performing one of the exercises, opt for another exercise that meets the same objective (i.e., changing the prescription and technique of the exercises). The injury risk in some exercises is easily “mitigated” by a variation in execution. For example, biceps curls with an EZ bar instead of a straight bar; triceps presses with a 45° grip or rope; and no maximum stretch in exercises such as pullovers, flies, and dips.
- Core training should be considered for ACL injury prevention. It has been demonstrated that it improves the extremity alignment in the frontal plane and muscle activation during sports-related tasks [68].
- The rating of perceived exertion and pain scales have been recognized as valid markers of internal load [120] and pain thresholds [121]. These easy-to-apply methodologies help to accurately monitor intensity and to adjust the RT program [11], taking advantage of the interoception process for control within the allostasis model [88]. PNE might be used as an intervention strategy to reduce kynophobia (refer to Vélez-Gutiérrez et al. [122] for a recent short commentary on cortical changes).
- Amateur and competitive bodybuilders should be aware that the consumption of AAS is a significant risk factor for several musculoskeletal disorders besides upper- and lower-limb injuries. Relevant predictors of the high frequency of PIED use include age, sex, educational level, and socioeconomic status [123,124], as well as psychological aspects associated with the constant dissatisfaction with body image of people attending PFC (e.g., bigorexia) [125].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barbieri, D.; Zaccagni, L. Strength training for children and adolescents: Benefits and risks. Coll. Antropol. 2013, 37 (Suppl. S2), 219–225. [Google Scholar] [PubMed]
- Cannataro, R.; Cione, E.; Bonilla, D.A.; Cerullo, G.; Angelini, F.; D’Antona, G. Strength training in elderly: An useful tool against sarcopenia. Front. Sports Act. Living 2022, 4, 287. [Google Scholar] [CrossRef] [PubMed]
- Kraschnewski, J.L.; Sciamanna, C.N.; Poger, J.M.; Rovniak, L.S.; Lehman, E.B.; Cooper, A.B.; Ballentine, N.H.; Ciccolo, J.T. Is strength training associated with mortality benefits? A 15 year cohort study of US older adults. Prev. Med. 2016, 87, 121–127. [Google Scholar] [CrossRef]
- Sanchez-Moreno, M.; Rodriguez-Rosell, D.; Pareja-Blanco, F.; Mora-Custodio, R.; Gonzalez-Badillo, J.J. Movement Velocity as Indicator of Relative Intensity and Level of Effort Attained During the Set in Pull-Up Exercise. Int. J. Sports Physiol. Perform. 2017, 12, 1378–1384. [Google Scholar] [CrossRef]
- Vikmoen, O.; Raastad, T.; Seynnes, O.; Bergstrom, K.; Ellefsen, S.; Ronnestad, B.R. Effects of Heavy Strength Training on Running Performance and Determinants of Running Performance in Female Endurance Athletes. PLoS ONE 2016, 11, e0150799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aagaard, P.; Andersen, J.L. Effects of strength training on endurance capacity in top-level endurance athletes. Scand. J. Med. Sci. Sports 2010, 20, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Chaabene, H.; Prieske, O.; Negra, Y.; Granacher, U. Change of direction speed: Toward a strength training approach with accentuated eccentric muscle actions. Sports Med. 2018, 48, 1773–1779. [Google Scholar] [CrossRef] [PubMed]
- Eckardt, N. Lower-extremity resistance training on unstable surfaces improves proxies of muscle strength, power and balance in healthy older adults: A randomised control trial. BMC Geriatr. 2016, 16, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maiorana, A.; Levinger, I.; Davison, K.; Smart, N.; Coombes, J.; Accredited Exercise Physiologists, E.; Sports Science, A. Exercise prescription is not just for medical doctors: The benefits of shared care by physicians and exercise professionals. Br. J. Sports Med. 2018, 52, 879–880. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, E.J.; Hegedus, S.R.; Wright, A.; Dickson, T.; Stern, B.D. Individualized Exercise Prescription for Athletes Using a Construct-Based Model. Sports Med. 2022, 52, 2315–2320. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, D.A.; Perez-Idarraga, A.; Odriozola-Martinez, A.; Kreider, R.B. The 4R’s Framework of Nutritional Strategies for Post-Exercise Recovery: A Review with Emphasis on New Generation of Carbohydrates. Int. J. Environ. Res. Public Health 2020, 18, 103. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Muller, P.; Gronwald, T.; Muller, N.G. Dose-Response Matters!—A Perspective on the Exercise Prescription in Exercise-Cognition Research. Front. Psychol. 2019, 10, 2338. [Google Scholar] [CrossRef] [Green Version]
- Grgic, J.; Lazinica, B.; Garofolini, A.; Schoenfeld, B.J.; Saner, N.J.; Mikulic, P. The effects of time of day-specific resistance training on adaptations in skeletal muscle hypertrophy and muscle strength: A systematic review and meta-analysis. Chronobiol. Int. 2019, 36, 449–460. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, B.J.; Ogborn, D.; Krieger, J.W. Dose-response relationship between weekly resistance training volume and increases in muscle mass: A systematic review and meta-analysis. J. Sports Sci. 2017, 35, 1073–1082. [Google Scholar] [CrossRef]
- Harries, S.K.; Lubans, D.R.; Callister, R. Systematic Review and Meta-analysis of Linear and Undulating Periodized Resistance Training Programs on Muscular Strength. J. Strength Cond. Res. 2015, 29, 1113–1125. [Google Scholar] [CrossRef]
- Lucini, D.; Pagani, M. Exercise Prescription to Foster Health and Well-Being: A Behavioral Approach to Transform Barriers into Opportunities. Int. J. Environ. Res. Public Health 2021, 18, 968. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.C.; Lai, J.S.K.; Yip, J.; Cheung, J.P.Y. Increased Computer Use is Associated with Trunk Asymmetry That Negatively Impacts Health-Related Quality of Life in Early Adolescents. Patient Prefer. Adherence 2021, 15, 2289–2302. [Google Scholar] [CrossRef]
- Hides, J.A.; Mendis, M.D.; Franettovich Smith, M.M.; Miokovic, T.; Cooper, A.; Low Choy, N. Association between altered motor control of trunk muscles and head and neck injuries in elite footballers—An exploratory study. Man. Ther. 2016, 24, 46–51. [Google Scholar] [CrossRef]
- Knapik, J.J. The importance of physical fitness for injury prevention: Part 1. J. Spec. Oper. Med. 2015, 15, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Eickhoff-Shemek, J.M.; Topalian, T. Virtual Fitness Programs: Safety and Legal Liability Issues to Consider: Part 1. ACSM’S Health Fit. J. 2022, 26, 48–51. [Google Scholar] [CrossRef]
- Wong, A.Y.L.; Karppinen, J.; Samartzis, D. Low back pain in older adults: Risk factors, management options and future directions. Scoliosis Spinal Disord. 2017, 12, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Noll, M.; Candotti, C.T.; da Rosa, B.N.; do Valle, M.B.; Antoniolli, A.; Vieira, A.; Loss, J.F. High prevalence of inadequate sitting and sleeping postures: A three-year prospective study of adolescents. Sci. Rep. 2017, 7, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Mañago, M.M.; Glick, S.; Hebert, J.R.; Coote, S.; Schenkman, M. Strength Training to Improve Gait in People with Multiple Sclerosis: A Critical Review of Exercise Parameters and Intervention Approaches. Int. J. MS Care 2019, 21, 47–56. [Google Scholar] [CrossRef] [Green Version]
- Rahyussalim, A.J.; Zufar, M.L.L.; Kurniawati, T. Significance of the Association between Disc Degeneration Changes on Imaging and Low Back Pain: A Review Article. Asian Spine J. 2019, 13, 245. [Google Scholar] [CrossRef] [Green Version]
- Whittemore, R.; Knafl, K. The integrative review: Updated methodology. J. Adv. Nurs 2005, 52, 546–553. [Google Scholar] [CrossRef]
- Hopia, H.; Latvala, E.; Liimatainen, L. Reviewing the methodology of an integrative review. Scand. J. Caring Sci. 2016, 30, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Ardern, C.L.; Buttner, F.; Andrade, R.; Weir, A.; Ashe, M.C.; Holden, S.; Impellizzeri, F.M.; Delahunt, E.; Dijkstra, H.P.; Mathieson, S.; et al. Implementing the 27 PRISMA 2020 Statement items for systematic reviews in the sport and exercise medicine, musculoskeletal rehabilitation and sports science fields: The PERSiST (implementing Prisma in Exercise, Rehabilitation, Sport medicine and SporTs science) guidance. Br. J. Sports Med. 2022, 56, 175–195. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, D.A.; De Leon, L.G.; Alexander-Cortez, P.; Odriozola-Martinez, A.; Herrera-Amante, C.A.; Vargas-Molina, S.; Petro, J.L. Simple anthropometry-based calculations to monitor body composition in athletes: Scoping review and reference values. Nutr. Health 2021, 28, 95–109. [Google Scholar] [CrossRef]
- Gho, C.; Petro, J.L.; Bonilla, D.A. Influencia de la acupuntura sobre el tratamiento de lesiones deportivas y el rendimiento atlético: Una revisión integradora. Rev. Int. Acupunt. 2020, 14, 64–75. [Google Scholar] [CrossRef]
- Jagodzinski, M.; Haasper, C.; Krettek, C. Disorders of the patellofemoral joint induced by weight training. Unfallchirurg 2009, 112, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Ackel-D’Elia, C.; Vancini, R.L.; Castelo, A.; Nouailhetas, V.L.A.; Silva, A.C.d. Absence of the predisposing factors and signs and symptoms usually associated with overreaching and overtraining in physical fitness centers. Clinics 2010, 65, 1161–1166. [Google Scholar] [CrossRef] [Green Version]
- Faigenbaum, A.D.; Myer, G.D. Resistance training among young athletes: Safety, efficacy and injury prevention effects. Br. J. Sports Med. 2010, 44, 56–63. [Google Scholar] [CrossRef] [Green Version]
- Kolber, M.J.; Beekhuizen, K.S.; Cheng, M.S.; Hellman, M.A. Shoulder injuries attributed to resistance training: A brief review. J. Strength Cond. Res. 2010, 24, 1696–1704. [Google Scholar] [CrossRef] [PubMed]
- Lavallee, M.E.; Balam, T. An overview of strength training injuries: Acute and chronic. Curr. Sports Med. Rep. 2010, 9, 307–313. [Google Scholar] [CrossRef]
- Malliaropoulos, N.; Mendiguchia, J.; Pehlivanidis, H.; Papadopoulou, S.; Valle, X.; Malliaras, P.; Maffulli, N. Hamstring exercises for track and field athletes: Injury and exercise biomechanics, and possible implications for exercise selection and primary prevention. Br. J. Sports Med. 2012, 46, 846–851. [Google Scholar] [CrossRef]
- Löfgren, B.; Dencker, M.; Nilsson, J.-Å.; Karlsson, M.K. A 4-year exercise program in children increases bone mass without increasing fracture risk. Pediatrics 2012, 129, e1468–e1476. [Google Scholar] [CrossRef] [Green Version]
- Escamilla, R.F.; MacLeod, T.D.; Wilk, K.E.; Paulos, L.; Andrews, J.R. ACL Strain and Tensile Forces for Weight Bearing and Non—Weight-Bearing Exercises After ACL Reconstruction: A Guide to Exercise Selection. J. Orthop. Sports Phys. Ther. 2012, 42, 208–220. [Google Scholar] [CrossRef] [Green Version]
- Jamison, S.T.; McNeilan, R.J.; Young, G.S.; Givens, D.L.; Best, T.M.; Chaudhari, A.M. Randomized controlled trial of the effects of a trunk stabilization program on trunk control and knee loading. Med. Sci. Sports Exerc. 2012, 44, 1924–1934. [Google Scholar] [CrossRef] [Green Version]
- Seynnes, O.R.; Kamandulis, S.; Kairaitis, R.; Helland, C.; Campbell, E.-L.; Brazaitis, M.; Skurvydas, A.; Narici, M.V. Effect of androgenic-anabolic steroids and heavy strength training on patellar tendon morphological and mechanical properties. J. Appl. Physiol. 2013, 115, 84–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sousa, N.; Mendes, R.; Monteiro, G.; Abrantes, C. Progressive resistance strength training and the related injuries in older adults: The susceptibility of the shoulder. Aging Clin. Exp. Res. 2014, 26, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Kolber, M.J.; Corrao, M.; Hanney, W.J. Characteristics of anterior shoulder instability and hyperlaxity in the weight-training population. J. Strength Cond. Res. 2013, 27, 1333–1339. [Google Scholar] [CrossRef] [PubMed]
- Doyscher, R.; Kraus, K.; Finke, B.; Scheibel, M. Acute and overuse injuries of the shoulder in sports. Orthopade 2014, 43, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Siewe, J.; Marx, G.; Knöll, P.; Eysel, P.; Zarghooni, K.; Graf, M.; Herren, C.; Sobottke, R.; Michael, J. Injuries and overuse syndromes in competitive and elite bodybuilding. Int. J. Sports Med. 2014, 35, 943–948. [Google Scholar] [CrossRef] [PubMed]
- Pearson, S.J.; Hussain, S.R. Region-specific tendon properties and patellar tendinopathy: A wider understanding. Sports Med. 2014, 44, 1101–1112. [Google Scholar] [CrossRef]
- DeWeese, B.H.; Hornsby, G.; Stone, M.; Stone, M.H. The training process: Planning for strength–power training in track and field. Part 2: Practical and applied aspects. J. Sport Health Sci. 2015, 4, 318–324. [Google Scholar] [CrossRef] [Green Version]
- Kanayama, G.; DeLuca, J.; Meehan, W.P., 3rd; Hudson, J.I.; Isaacs, S.; Baggish, A.; Weiner, R.; Micheli, L.; Pope, H.G., Jr. Ruptured Tendons in Anabolic-Androgenic Steroid Users: A Cross-Sectional Cohort Study. Am. J. Sports Med. 2015, 43, 2638–2644. [Google Scholar] [CrossRef]
- Jakobsen, J.R.; Mackey, A.; Knudsen, A.; Koch, M.; Kjaer, M.; Krogsgaard, M. Composition and adaptation of human myotendinous junction and neighboring muscle fibers to heavy resistance training. Scand. J. Med. Sci. Sports 2017, 27, 1547–1559. [Google Scholar] [CrossRef]
- Hameed, M.; Sahu, A.; Johnson, M.B. Muscle mania: The quest for the perfect body. BMJ Case Rep. 2016, 2016, bcr2016217208. [Google Scholar] [CrossRef]
- Peña, G.; Heredia, J.; Lloret, C.; Martín, M.; Da Silva-Grigoletto, M.E. Iniciación al entrenamiento de fuerza en edades tempranas: Revisión. Rev. Andal. Med. Deporte 2016, 9, 41–49. [Google Scholar] [CrossRef] [Green Version]
- Ruivo, R.; Carita, A.; Pezarat-Correia, P. The effects of training and detraining after an 8 month resistance and stretching training program on forward head and protracted shoulder postures in adolescents: Randomised controlled study. Man. Ther. 2016, 21, 76–82. [Google Scholar] [CrossRef]
- Thorborg, K.; Bandholm, T.; Zebis, M.; Andersen, L.L.; Jensen, J.; Holmich, P. Large strengthening effect of a hip-flexor training programme: A randomized controlled trial. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2346–2352. [Google Scholar] [CrossRef] [PubMed]
- Keogh, J.W.; Winwood, P.W. The Epidemiology of Injuries Across the Weight-Training Sports. Sports Med. 2017, 47, 479–501. [Google Scholar] [CrossRef] [Green Version]
- Zwolski, C.; Quatman-Yates, C.; Paterno, M.V. Resistance Training in Youth: Laying the Foundation for Injury Prevention and Physical Literacy. Sports Health 2017, 9, 436–443. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bourne, M.N.; Timmins, R.G.; Opar, D.A.; Pizzari, T.; Ruddy, J.D.; Sims, C.; Williams, M.D.; Shield, A.J. An evidence-based framework for strengthening exercises to prevent hamstring injury. Sports Med. 2018, 48, 251–267. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Schultz, J.; Timgren, J.; Staelgraeve, K.; Miller, M.; Liu, Y. An electromyographic and kinetic comparison of conventional and Romanian deadlifts. J. Exerc. Sci. Fit. 2018, 16, 87–93. [Google Scholar] [CrossRef]
- Lauersen, J.B.; Andersen, T.E.; Andersen, L.B. Strength training as superior, dose-dependent and safe prevention of acute and overuse sports injuries: A systematic review, qualitative analysis and meta-analysis. Br. J. Sports Med. 2018, 52, 1557–1563. [Google Scholar] [CrossRef] [Green Version]
- Strömbäck, E.; Aasa, U.; Gilenstam, K.; Berglund, L. Prevalence and Consequences of Injuries in Powerlifting: A Cross-sectional Study. Orthop. J. Sports Med. 2018, 6, 2325967118771016. [Google Scholar] [CrossRef] [Green Version]
- Walters, B.K.; Read, C.R.; Estes, A.R. The effects of resistance training, overtraining, and early specialization on youth athlete injury and development. J. Sports Med. Phys. Fit. 2018, 58, 1339–1348. [Google Scholar] [CrossRef]
- Pichardo, A.W.; Oliver, J.L.; Harrison, C.B.; Maulder, P.S.; Lloyd, R.S.; Kandoi, R. Effects of Combined Resistance Training and Weightlifting on Injury Risk Factors and Resistance Training Skill of Adolescent Males. J. Strength Cond. Res. 2021, 35, 3370–3377. [Google Scholar] [CrossRef]
- Batterson, A.M.; Froelich, R.K.; Schleck, C.D.; Laskowski, E.R. Injury Rate and Patterns in Group Strength-Endurance Training Classes. Mayo Clin. Proc. 2020, 95, 468–475. [Google Scholar] [CrossRef]
- Ritsch, M. Verletzungen und Überlastungsschäden im Kraftsport. Sports Orthop. Traumatol. 2020, 36, 260–270. [Google Scholar] [CrossRef]
- Barranco-Ruiz, Y.; Villa-Gonzalez, E.; Martinez-Amat, A.; Da Silva-Grigoletto, M.E. Prevalence of Injuries in Exercise Programs Based on Crossfit((R)), Cross Training and High-Intensity Functional Training Methodologies: A Systematic Review. J. Hum. Kinet. 2020, 73, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, R.V.; Dantas, M.; Motas, D.G.; Gantois, P.; Aidar, F.J.; Dantas, P.M.S.; Queiros, V.S.; Cesario, T.M.; Cabral, B. Retrospective Study of Risk Factors and the Prevalence of Injuries in HIFT. Int. J. Sports Med. 2020, 41, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, M.S.; Kumar, P.; John, R.; Hooda, A. Bilateral Quadriceps Rupture in an Elite Weight Lifter: A Case Report and Review of Literature. Indian J. Orthop. 2020, 54, 339–347. [Google Scholar] [CrossRef]
- Urbanczyk, C.A.; Prinold, J.A.I.; Reilly, P.; Bull, A.M.J. Avoiding high-risk rotator cuff loading: Muscle force during three pull-up techniques. Scand. J. Med. Sci. Sports 2020, 30, 2205–2214. [Google Scholar] [CrossRef] [PubMed]
- Ferri-Caruana, A.; Prades-Insa, B.; Serra, A.P. Effects of pelvic and core strength training on biomechanical risk factors for anterior cruciate ligament injuries. J. Sports Med. Phys. Fit. 2020, 60, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Dudagoitia, E.; García-de-Alcaraz, A.; Andersen, L.L. Safety of powerlifting: A literature review. Sci. Sports 2021, 36, e59–e68. [Google Scholar] [CrossRef]
- Jeong, J.; Choi, D.H.; Shin, C.S. Core Strength Training Can Alter Neuromuscular and Biomechanical Risk Factors for Anterior Cruciate Ligament Injury. Am. J. Sports Med. 2021, 49, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Colado, J.C.; Garcia-Masso, X. Technique and safety aspects of resistance exercises: A systematic review of the literature. Phys. Sportsmed. 2009, 37, 104–111. [Google Scholar] [CrossRef]
- Macho, J.; Mudrak, J.; Slepicka, P. Enhancing the Self: Amateur Bodybuilders Making Sense of Experiences With Appearance and Performance-Enhancing Drugs. Front. Psychol. 2021, 12, 648467. [Google Scholar] [CrossRef]
- Odriozola, J.M. Ayudas ergogénicas en el deporte. Arbor 2000, 165, 171–185. [Google Scholar] [CrossRef] [Green Version]
- Llewellyn, W. Molecular Nutrition, 9th ed.; Anabolics: Aurora, CO, USA, 2009; 212p. [Google Scholar]
- Greenway, C.W.; Price, C. Muscle dysmorphia and self-esteem in former and current users of anabolic-androgenic steroids. Perform. Enhanc. Health 2020, 7, 100154. [Google Scholar] [CrossRef]
- Stannard, J.P.; Bucknell, A.L. Rupture of the triceps tendon associated with steroid injections. Am. J. Sports Med. 1993, 21, 482–485. [Google Scholar] [CrossRef] [PubMed]
- Powell, C.; Chang, C.; Naguwa, S.M.; Cheema, G.; Gershwin, M.E. Steroid induced osteonecrosis: An analysis of steroid dosing risk. Autoimmun. Rev. 2010, 9, 721–743. [Google Scholar] [CrossRef]
- Mendiratta, V.; Khan, A.; Solanki, R.S. Avascular necrosis: A rare complication of steroid therapy for pemphigus. Indian J. Dermatol. 2008, 53, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother. Psychosom. 2021, 90, 11–27. [Google Scholar] [CrossRef]
- McEwen, B.S. Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Ann. N. Y. Acad. Sci. 1998, 840, 33–44. [Google Scholar] [CrossRef]
- Sterling, P.; Eyer, J. Allostasis: A new paradigm to explain arousal pathology. In Handbook of Life Stress, Cognition and Health; John Wiley & Sons: Oxford, UK, 1988; pp. 629–649. [Google Scholar]
- Holtzman, B.; Popp, K.L.; Tenforde, A.S.; Parziale, A.L.; Taylor, K.; Ackerman, K.E. Low energy availability surrogates associated with lower bone mineral density and bone stress injury site. PM R 2022, 14, 587–596. [Google Scholar] [CrossRef]
- Huang, K.; Ihm, J. Sleep and Injury Risk. Curr. Sports Med. Rep. 2021, 20, 286–290. [Google Scholar] [CrossRef]
- Bonilla, D.A.; Moreno, Y.; Petro, J.L.; Forero, D.A.; Vargas-Molina, S.; Odriozola-Martinez, A.; Orozco, C.A.; Stout, J.R.; Rawson, E.S.; Kreider, R.B. A Bioinformatics-Assisted Review on Iron Metabolism and Immune System to Identify Potential Biomarkers of Exercise Stress-Induced Immunosuppression. Biomedicines 2022, 10, 724. [Google Scholar] [CrossRef]
- Krause, J.S.; DiPiro, N.D.; Saunders, L.L.; Newman, S.D.; Banik, N.L.; Park, S. Allostatic load and spinal cord injury: Review of existing research and preliminary data. Top. Spinal Cord. Inj. Rehabil. 2014, 20, 137–146. [Google Scholar] [CrossRef] [Green Version]
- Miranda-Comas, G.; Zaman, N.; Ramin, J.; Gluck, A. The Role of Workload Management in Injury Prevention, Athletic, and Academic Performance in the Student-Athlete. Curr. Sports Med. Rep. 2022, 21, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, A.W.; Armitano-Lago, C.N.; Sathyan, A.; MacPherson, R.; Cohen, K.; Silva, P.L. The Intelligent Phenotypic Plasticity Platform (IP(3)) for Precision Medicine-Based Injury Prevention in Sport. Methods Mol. Biol. 2022, 2393, 877–903. [Google Scholar] [CrossRef] [PubMed]
- Corcoran, A.W.; Hohwy, J. Allostasis, interoception, and the free energy principle: Feeling our way forward. In The Interoceptive Mind: From Homeostasis to Awareness; Tsakiris, M., De Preester, H., Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar] [CrossRef]
- Fitzcharles, M.A.; Cohen, S.P.; Clauw, D.J.; Littlejohn, G.; Usui, C.; Hauser, W. Nociplastic pain: Towards an understanding of prevalent pain conditions. Lancet 2021, 397, 2098–2110. [Google Scholar] [CrossRef]
- Sennesh, E.; Theriault, J.; Brooks, D.; van de Meent, J.W.; Barrett, L.F.; Quigley, K.S. Interoception as modeling, allostasis as control. Biol. Psychol. 2022, 167, 108242. [Google Scholar] [CrossRef]
- Benjamin, M. The fascia of the limbs and back—A review. J. Anat. 2009, 214, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Dischiavi, S.L.; Wright, A.A.; Hegedus, E.J.; Bleakley, C.M. Biotensegrity and myofascial chains: A global approach to an integrated kinetic chain. Med. Hypotheses 2018, 110, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Joseph, L.H.; Pirunsan, U.; Sitilertpisan, P.; Paungmali, A. Effect of lumbopelvic myofascial force transmission on glenohumeral kinematics–A myo-fascia-biomechanical hypothesis. Pol. Ann. Med. 2017, 24, 276–282. [Google Scholar] [CrossRef]
- Bordoni, B.; Myers, T. A Review of the Theoretical Fascial Models: Biotensegrity, Fascintegrity, and Myofascial Chains. Cureus 2020, 12, e7092. [Google Scholar] [CrossRef] [PubMed]
- Atkins, S.J.; Bentley, I.; Brooks, D.; Burrows, M.P.; Hurst, H.T.; Sinclair, J.K. Electromyographic response of global abdominal stabilizers in response to stable-and unstable-base isometric exercise. J. Strength Cond. Res. 2015, 29, 1609–1615. [Google Scholar] [CrossRef] [PubMed]
- Behm, D.G.; Leonard, A.M.; Young, W.B.; Bonsey, W.A.; MacKinnon, S.N. Trunk muscle electromyographic activity with unstable and unilateral exercises. J. Strength Cond. Res. 2005, 19, 193–201. [Google Scholar] [CrossRef]
- Vera-García, F.; Barbado, D.; Moreno-Pérez, V.; Hernández-Sánchez, S.; Juan-Recio, C.; Elvira, J. Core stability: Concepto y aportaciones al entrenamiento y la prevención de lesiones. Rev. Andal. Med. Deporte 2015, 8, 79–85. [Google Scholar] [CrossRef]
- Vera-García, F.; Barbado, D.; Moreno-Pérez, V.; Hernández-Sánchez, S.; Juan-Recio, C.; Elvira, J. Core stability: Evaluación y criterios para su entrenamiento. Rev. Andal. Med. Deporte 2015, 8, 130–137. [Google Scholar] [CrossRef]
- Hazebroek-Kampschreur, A.; Hofman, A. Prevalence of trunk abnormalities in eleven-year-old schoolchildren in Rotterdam, The Netherlands. J. Pediatr. Orthop. 1992, 12, 480–484. [Google Scholar] [CrossRef] [PubMed]
- Zakeri, Y.; Baraz, S.; Gheibizadeh, M.; Saidkhani, V. Relationship between backpack weight and prevalence of lordosis, kyphosis, scoliosis and dropped shoulders in elementary students. Int. J. Pediatr. 2016, 4, 1859–1866. [Google Scholar] [CrossRef]
- Katzman, W.; Cawthon, P.; Hicks, G.E.; Vittinghoff, E.; Shepherd, J.; Cauley, J.A.; Harris, T.; Simonsick, E.M.; Strotmeyer, E.; Womack, C. Association of spinal muscle composition and prevalence of hyperkyphosis in healthy community-dwelling older men and women. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 67, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Lugo, R.; Kung, P.; Ma, C.B. Shoulder biomechanics. Eur. J. Radiol. 2008, 68, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Murray, I.R.; Goudie, E.B.; Petrigliano, F.A.; Robinson, C.M. Functional anatomy and biomechanics of shoulder stability in the athlete. Clin. Sports Med. 2013, 32, 607–624. [Google Scholar] [CrossRef]
- Schoenfeld, B.J.; Sonmez, R.G.; Kolber, M.J.; Contreras, B.; Harris, R.; Ozen, S. Effect of hand position on EMG activity of the posterior shoulder musculature during a horizontal abduction exercise. J. Strength Cond. Res. 2013, 27, 2644–2649. [Google Scholar] [CrossRef] [PubMed]
- Nunes, J.P.; Costa, B.D.V.; Kassiano, W.; Kunevaliki, G.; Castro, E.S.P.; Rodacki, A.L.F.; Fortes, L.S.; Cyrino, E.S. Different Foot Positioning During Calf Training to Induce Portion-Specific Gastrocnemius Muscle Hypertrophy. J. Strength Cond. Res. 2020, 34, 2347–2351. [Google Scholar] [CrossRef] [PubMed]
- Trebs, A.A.; Brandenburg, J.P.; Pitney, W.A. An electromyography analysis of 3 muscles surrounding the shoulder joint during the performance of a chest press exercise at several angles. J. Strength Cond. Res. 2010, 24, 1925–1930. [Google Scholar] [CrossRef]
- Saeterbakken, A.H.; Mo, D.A.; Scott, S.; Andersen, V. The Effects of Bench Press Variations in Competitive Athletes on Muscle Activity and Performance. J. Hum. Kinet. 2017, 57, 61–71. [Google Scholar] [CrossRef] [Green Version]
- Stastny, P.; Golas, A.; Blazek, D.; Maszczyk, A.; Wilk, M.; Pietraszewski, P.; Petr, M.; Uhlir, P.; Zajac, A. A systematic review of surface electromyography analyses of the bench press movement task. PLoS ONE 2017, 12, e0171632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aasa, U.; Svartholm, I.; Andersson, F.; Berglund, L. Injuries among weightlifters and powerlifters: A systematic review. Br. J. Sports Med. 2017, 51, 211–219. [Google Scholar] [CrossRef] [Green Version]
- Wallden, M.; Nijs, J. Before & beyond the pain—Allostatic load, central sensitivity and their role in health and function. J. Bodyw. Mov. Ther. 2021, 27, 388–392. [Google Scholar] [CrossRef]
- Kapreli, E.; Athanasopoulos, S. The anterior cruciate ligament deficiency as a model of brain plasticity. Med. Hypotheses 2006, 67, 645–650. [Google Scholar] [CrossRef] [PubMed]
- Ajimsha, M.S.; Shenoy, P.D.; Gampawar, N. Role of fascial connectivity in musculoskeletal dysfunctions: A narrative review. J. Bodyw. Mov. Ther. 2020, 24, 423–431. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Graven-Nielsen, T.; Svarrer, H.; Svensson, P. The influence of low back pain on muscle activity and coordination during gait: A clinical and experimental study. Pain 1996, 64, 231–240. [Google Scholar] [CrossRef]
- Courtney, C.A.; Kavchak, A.E.; Lowry, C.D.; O’Hearn, M.A. Interpreting Joint Pain: Quantitative Sensory Testing in Musculoskeletal Management. J. Orthop. Sports Phys. Ther. 2010, 40, 818–825. [Google Scholar] [CrossRef]
- Robins, H.; Perron, V.; Heathcote, L.; Simons, L. Pain Neuroscience Education: State of the Art and Application in Pediatrics. Children 2016, 3, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prestes, J.; Frollini, A.B.; de Lima, C.; Donatto, F.F.; Foschini, D.; de Cássia Marqueti, R.; Figueira, A., Jr.; Fleck, S.J. Comparison between linear and daily undulating periodized resistance training to increase strength. J. Strength. Cond. Res. 2009, 23, 2437–2442. [Google Scholar] [CrossRef] [PubMed]
- Vargas-Molina, S.; Petro, J.L.; Romance, R.; Bonilla, D.A.; Schoenfeld, B.J.; Kreider, R.B.; Benítez-Porres, J. Menstrual cycle-based undulating periodized program effects on body composition and strength in trained women: A pilot study. Sci. Sports 2022. [Google Scholar] [CrossRef]
- Vargas-Molina, S.; García-Sillero, M.; Romance, R.; Petro, J.L.; Jiménez-García, J.D.; Bonilla, D.A.; Kreider, R.B.; Benítez-Porres, J. Traditional and Undulating Periodization on Body Composition, Strength Levels and Physical Fitness in Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 4522. [Google Scholar] [CrossRef]
- Moesgaard, L.; Beck, M.M.; Christiansen, L.; Aagaard, P.; Lundbye-Jensen, J. Effects of Periodization on Strength and Muscle Hypertrophy in Volume-Equated Resistance Training Programs: A Systematic Review and Meta-analysis. Sports Med. 2022, 52, 1647–1666. [Google Scholar] [CrossRef]
- Rosa, A.; Vazquez, G.; Grgic, J.; Balachandran, A.T.; Orazem, J.; Schoenfeld, B.J. Hypertrophic Effects of Single- Versus Multi-Joint Exercise of the Limb Muscles: A Systematic Review and Meta-analysis. Strength Cond. J. 2022. ahead of print. [Google Scholar] [CrossRef]
- Bayattork, M.; Skold, M.B.; Sundstrup, E.; Andersen, L.L. Exercise interventions to improve postural malalignments in head, neck, and trunk among adolescents, adults, and older people: Systematic review of randomized controlled trials. J. Exerc. Rehabil. 2020, 16, 36–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falk Neto, J.H.; Tibana, R.A.; de Sousa, N.M.F.; Prestes, J.; Voltarelli, F.A.; Kennedy, M.D. Session Rating of Perceived Exertion Is a Superior Method to Monitor Internal Training Loads of Functional Fitness Training Sessions Performed at Different Intensities When Compared to Training Impulse. Front. Physiol. 2020, 11, 919. [Google Scholar] [CrossRef]
- Lau, W.Y.; Blazevich, A.J.; Newton, M.J.; Wu, S.S.; Nosaka, K. Assessment of Muscle Pain Induced by Elbow-Flexor Eccentric Exercise. J. Athl. Train. 2015, 50, 1140–1148. [Google Scholar] [CrossRef] [Green Version]
- Vélez-Gutiérrez, J.M.; Petro, J.L.; Aburto-Corona, J.A.; Vargas-Molina, S.; Kreider, R.B.; Bonilla, D.A. Cortical Changes as a Result of Sports Injuries: A Short Commentary. Cuerpo, Cultura y Movimiento 2022, 12, 1–13. [Google Scholar] [CrossRef]
- Zahnow, R.; McVeigh, J.; Bates, G.; Hope, V.; Kean, J.; Campbell, J.; Smith, J. Identifying a typology of men who use anabolic androgenic steroids (AAS). Int. J. Drug Policy 2018, 55, 105–112. [Google Scholar] [CrossRef]
- Rontogianni, M.O.; Kanellopoulou, A.; Markozannes, G.; Bouras, E.; Derdemezis, C.; Doumas, M.T.; Sigounas, D.E.; Tzovaras, V.T.; Vakalis, K.; Panagiotakos, D.B.; et al. Prevalence and Determinants of Sex-Specific Dietary Supplement Use in a Greek Cohort. Nutrients 2021, 13, 2857. [Google Scholar] [CrossRef]
- Schneider, C.; Agthe, M.; Yanagida, T.; Voracek, M.; Hennig-Fast, K. Effects of muscle dysmorphia, social comparisons and body schema priming on desire for social interaction: An experimental approach. BMC Psychol. 2017, 5, 19. [Google Scholar] [CrossRef] [PubMed]

| Type of Study | Participants | Aim | Instruments or Procedure | Main Findings/Conclusions | Reference |
|---|---|---|---|---|---|
| Narrative Review/Qualitative Analysis | 30 references (includes articles from their year of publication until 2009) | To analyze the influential factors in the development of patellofemoral pain syndrome. | Literature search of epidemiological and clinical aspects. A retrospective, citation-based methodology was applied. | Besides genetic characteristics or some noxa, patellofemoral malalignment, high loads and overuse, uncontrolled exercises, and AAS represent risk factors for injuries. Individual training concepts with controlled exercises that reduce peak loads are desireable. | Jagodzinski et al., 2009 [30] |
| Cross-sectional/Quantitative Analysis | n = 413 (216M; 197F) Only 60 subjects participated in the laboratory analysis. | To assess the predisposing factors, signs, and symptoms usually associated with OVR or OVT in members of PFC. | Questionnaire of 41 questions to evaluate OVR/OVT + POMS questionnaire + hematological and biochemical (CK activity, cortisol, total T, free T) analyses | The absence of predisposing factors and signs/symptoms associated with OVR or OVT states was evidenced in fitness practitioners in Sao Paulo, Brazil. Thus, detecting people engaged in excessive exercise training needs to be confirmed. | Ackel-D’Elia et al., 2010 [31] |
| Narrative Review/Qualitative Analysis | 91 references from which 27 were clinical trials (from their year of publication until 2010) | To review the current epidemiology of injury related to the safety and efficacy of RT among youth and to provide age-appropriate training recommendations for children and adolescents | Literature search with practical and applied aspects. A retrospective, citation-based methodology was applied. | Lack of supervision in strength training in the youth population is associated with an injury rate due to inadequate technical execution and load control. Musculoskeletal injuries during RT do not appear to be superior to other sports modalities and activities. | Faigenbaum & Myer, 2010 [32] |
| Narrative Review/Qualitative Analysis | 82 references (includes articles from their year of publication until 2009). | To present an overview of the literature pertaining to shoulder injuries in the RT population and to elucidate the etiological risk factors hypothesized to be associated with the more common injuries. | Literature search in PUBMED, CINAHL, SPORTDiscus, and OVID databases using key words including resistance training, shoulder, bodybuilding, weightlifting, shoulder injury, and shoulder disorder. | Up to 36% of documented RT-related injuries and disorders occur at the shoulder complex. Deltoid to external rotators and upper to lower trapezius muscles should be strengthened to mitigate strength imbalances associated with RT. Train flexibility to increase internal rotation and avoid the end-range “high-five” position may prevent the development of anterior shoulder instability and pain. | Kolber et al., 2010 [33] |
| Narrative Review/Qualitative Analysis | 38 references (includes articles from year of publication to 2010). | To introduce the history of strength training, explain the many different styles of strength training, and discuss common injuries specific to each style. | Literature search with practical and applied aspects. A retrospective, citation-based methodology was applied. | The most common acute non-urgent injuries are muscular strains and ligamentous sprains, while urgent injuries are fractures, dislocations, and tendon ruptures. Patellar dislocation and acute meniscal tears are rarely reported. Most injuries are related to accidents or overexertion although each style of strength training has its own principal injuries, both acute and chronic, related to the individual technique. | Lavallee & Balam, 2010 [34] |
| Narrative Review/Qualitative Analysis | 68 references (includes articles from year of publication to 2011). | To review the possible role and effects of eccentric strength training for injury prevention and use this, together with injury biomechanics, as a basis to suggest an eccentric exercise classification criteria applicable to the track and field athletes. | Literature search with practical and applied aspects. A retrospective, citation-based methodology was applied. | Hip flexion or knee extension exercises that actively lengthen the hamstrings should be trained. Focus on the long head of the biceps femoris, proximal semitendinosus, adductor magnus, and semimembranosus, based on plyometric and eccentric exercises. | Malliaropoulos et al., 2012 [35] |
| Non-randomized prospective controlled study/Quantitative Analysis | A cohort of children aged 7 to 9 years: 446 boys and 362 girls in the intervention group (2675 person-years) and 807 boys and 780 girls in the control group (5661 person-years). | To evaluate whether an extended exercise intervention program (40 min per day of school physical education for 4 years including strength-based exercises) in children could produce long-term skeletal benefits without increasing the fracture incidence. | BMC (g) and bone width (cm) were assessed by DXA of the whole body, lumbar spine, femoral neck, and trochanter + fracture index recorded in the city hospital records. | A 4-year exercise program in children aged 7 to 9 years increased bone mass and size without affecting the fracture risk. In the girls, there was a gradually higher gain in femoral neck and trochanter BMCs and femoral neck width with each tertile of higher duration of physical activity. A similar pattern was found in the children, reaching significance in the lumbar spine BMC and femoral neck width. | Löfgren et al., 2012 [36] |
| Narrative Review/Qualitative Analysis | 63 references (includes articles from their year of publication until 2012) | To discuss the biomechanical factors related to ACL loading during common weight-bearing and non-weight-bearing exercises and to guide clinicians regarding exercise selection and progression for patients with ACL pathology or reconstruction. | Literature search on tensile strength and strain energy density data of the ACL in different exercises. | It highlights that the load on the ACL is greater in exercises without supporting body mass (double-leg and single-leg squats, lunges); for example, squatting with a vertical trunk position, which decreases hamstrings activity and increases quadriceps activity, leading to higher ACL loading. Caution should be taken in exercises with high knee flexion angle or heel raise since they generate more ACL loading. | Escamilla et al., 2012 [37] |
| RCT/Quantitative Analysis | n = 37 healthy males (only 22 were included in the analysis) were divided into two 6-week training groups: RT and RT + TS | To investigate the effectiveness of a training program including focused TS exercises on improving lower extremity biomechanics, athletic performance, and trunk or core measures (control, endurance, and strength) compared with a program incorporating only RT. | ACL strain analyzed by biomechanical loading without anticipation with Vicon MX-F40 and Bertec 4060-10 systems + trunk control and core strength using a sudden force release test with an OMEGA DM-465 load cell system + core endurance using McGill protocols for lateral plank, pronated plank, and trunk flexor exercises + lower limb strength + sports performance analysis. | Despite the lack of differences between groups, which may have been due to inter-subject variability and sample size, RT generated greater risk of ACL rupture while the RT + TS program was able to limit potential negative effects. In addition, only the RT + TS group generated improvements in CORE strength and endurance. | Jamison et al., 2012 [38] |
| Prospective Clinical Trial/Quantitative Analysis | n = 24 volunteers: eight RT-trained individuals using AAS; eight RT-trained individuals who had never used AAS; and eight subjects without any history of regular RT or AAS abuse | To examine in vivo mechanical properties of patellar tendons subjected to long-term exposure to overloading and AAS abuse by comparing highly trained individuals using AAS to trained and untrained subjects without any history of AAS. | Supplementation and drugs report + maximal knee extension isometric torque using an isokinetic dynamometer (System 3, Biodex Medical Systems) + muscle thickness, pennation angle, fascicle length, CSA of the patellar tendon, and tendon mechanical and material properties using ultrasonography (10–25 MHz transducer MyLab25) | The CSA of the tendon was greater in RT-trained subjects who did not use AAS. The patellar tendon generated more stiffness, more stress, and greater tensile modulus in subjects using AAS, which may limit tendon safety probably due to alterations in collagen remodeling. | Seynnes et al., 2013 [39] |
| Narrative Review/Qualitative Analysis | 39 references (includes articles from year of publication to 2013). | To discuss the PRT-related injuries and present an overview of documented shoulder injuries among older adults, presenting a brief review of its anatomy, and to discern the possible mechanisms of injury and risk factors. | Literature search in PubMed database using the following specific search terms: strength-training injuries, resistance-training injuries, sports injuries in the elderly, shoulder complex, shoulder injury, and shoulder disorder. | The combination of unfavorable positions, fatigue, and unproper technique during exercises, such as bench press, behind-the-neck pull-downs, military presses, and chest flies may lead to AI and rotator cuff injuries (especially in older population). Preventive exercise based on the lower trapezius and external rotators is advised to mitigate strength imbalances. | Sousa et al., 2013 [40] |
| Cross-sectional/Quantitative Analysis | n = 159 healthy male subjects (123 with weight RT training experience and 36 with no history of weight RT participation as control group) | (i) To determine if men who participate in weight RT present with clinical characteristics of shoulder hyperlaxity and AI. (ii) To determine if there is difference between the presence of these conditions among weight RT participants when compared with a control group. (iii) To investigate the association of exercise selection with clinical characteristics of AI. | A detailed questionnaire to document specific training patterns that includedfrequency, presence of pain, and exercise selection + load and shift test (to detect and quantify anterior glenohumeral joint instability) + apprehension test (to detect anterior glenohumeral joint instability) + relocation test (to diagnose anterior instability). All measurements were performed on the non-dominant arm. | The rates of pain and positive apprehension and relocation tests were significantly higher in trained subjects than in untrained subjects. The injury risk in the weight RT population might be reduced by changes in exercise selection and technique. For example, it is advisable to make modifications in exercises such as behind-the-neck pull-down or military press by bringing the bar down to the front chest (avoiding the high-five position). Also, incorporating reinforcement work in the external rotators might prevent the injury risk for anterior shoulder instability and pain. | Kolber et al., 2013 [41] |
| Narrative Review/Qualitative Analysis | 49 references (includes articles from their year of publication until 2014). | To overview the frequency, type, and developmental mechanisms of shoulder injuries as a function of various sports. | Selective literature search in the PubMed database taking into account authors’ experience and research results as well as international and national recommendations. | Acute (e.g., traumatic dislocations, acromioclavicular joint dislocations, traumatic tendon ruptures, labral and cartilage defects, and fractures) and chronic (e.g., bursitis and tendinitis, secondary forms of impingement with rotator cuff and labral lesions) injuries are are particularly common in throwing and impact sports (e.g., tennis, golf, handball, and volleyball) but also in contact and extreme sports (e.g., judo, martial arts, bodybuilding, weightlifting, motocross, and downhill mountain biking). The type and frequency of injuries are strongly dependent on the risk and load profile of the individual. | Doyscher et al., 2014 [42] |
| Retrospective cross-sectional study/Quantitative Analysis | n = 71 (54M; 17F) German elite and competitive bodybuilders (33.9 ± 9.2 years). | To investigate rates of injury, pain during workouts or overusesyndromes, as well as the influence of particular intrinsic and external factors | Five-parts questionnaire: demographics and general information + workout-related data and pain symptoms + frequency and localization of previous injuries or musculoskeletal disorders + general health disorders + lifestyle, nutrition, and medical therapy | The squat and bench press exercises most frequently generate pain in lower and upper limbs during workouts, respectively. The highest injury rates were found in the shoulder, elbow, lumbar spine, and knee (>40 years-old athletes exhibiting higher injury rates). The injury rate in elite and competitive bodybuilders (0.24 injuries per 1000 h of bodybuilding) is lower compared to other weightlifting (e.g., powerlifting, strongman, or Olympic lifting). | Siewe et al., 2014 [43] |
| Narrative Review/Qualitative Analysis | 83 references (includes articles from year of publication to 2011). | (i) To provide a review of the literature with respect to regionspecific tendon properties, in association with patellar tendinopathy; (ii) to outline the automated tracking method as used by recent studies for the determination of regionspecific mechanical properties to inspire future research; (iii) to discuss potential treatment strategies for the management of patellar tendinopathy. | Literature search in PubMed database using the following specific search terms: patellar tendinopathy, patellar tendinitis, jumper’s knee, patellar tendon, tendon injury, region specific tendon properties, mechanical properties, tendon strain, treatment. | Patellar tendinopathy is a common musculoskeletal disorder affecting a wide range of amateur and elite athletes, especially those that participate in jumping events. Tendinopathy appears to result in an increased tendon CSA concomitant with decreased stiffness. The use of eccentric exercise or heavy–slow strength training can optimize the prevention and recovery of patellar tendinopathy and pain reduction in athletes. In general, any activity that exposes a region of the tendon to the largest forces could be considered a potential risk factor. | Pearson & Hussain, 2014 [44] |
| Narrative Review/Qualitative Analysis | 49 references (includes articles from their year of publication until 2015). | Planning proposals for strength–power training, allowing for logical integration and manipulation of training variables including exercise selection. | Literature search with practical and applied aspects. A retrospective, citation-based methodology was applied. | To maximize the transfer-of-training effect and reduce injuries in strength or power athletes, it is doubtful that single-joint exercises will have as much impact on performance as multijoint training exercises. Advanced athletes require greater variation in exercise selection, volume, and intensity of training compared to beginning athletes. | DeWeese et al., 2015 [45] |
| Cross-sectional/Quantitative Analysis | n = 142 male bodybuilders (35–55 years); 88 reported consuming AAS in the last two years while 54 did not have used AAS. | To provide more quantitative data on the association of AAS use with tendon rupture by assessing the history of tendon rupture in a large cohort of AAS users and comparison nonusers. | Medical history + history of surgical interventions + epidemiological instrument + anthropometric assessment + anti-doping and PIEDs analysis in urine and hair + medical evaluation (cardiovascular function). | AAS abusers have a higher tendon injury risk than non-AAS-using bodybuilders. In addition, upper body tendon ruptures were exclusively reported in the participants who consumed AAS. | Kanayama et al., 2015 [46] |
| RCT/Quantitative Analysis | n = 15 (11M; 4F) divided into three groups: control, acute training group, and training group for four weeks. | To describe the distribution of macrophages and matrix proteins in human MTJ and adjoining muscle fibers and to investigate the influence of heavy RT (quadriceps and hamstrings muscle groups) on this distribution. | Sample from the semitendinosus and gracilis tendons + immunohistochemical analysis of collagen types and macrophage density. Subjects were healthy except for an isolated ACL rupture and scheduled for reconstruction surgery; however, they were able to perform daily activities so could not be classified as inactive. | Quadriceps exercises included leg press and leg extensions. Hamstrings exercises included Nordic hamstring, lying leg curls, supine one-leg curls, and reverse hyperextensions. The 4-week heavy RT program resulted in more collagen XIV, macrophages, and Tenascin-C content in the endomysium, which may indicate an optimal remodeling process and adaptations for injury prevention in the MTJ region. | Jakobsen et al., 2017 [47] |
| Case study/Quantitative Analysis | An amateur 25-years old bodybuilder with 4 years of experience. | To describe the case of a young man who self-aministred PIEDs and suffered from pain and reduced mobility of the right elbow for several months. | Medical history (repeated hospital admissions) + biochemical analysis + ultrasound and NMR imaging of the subject’s right arm + X-ray of the left shoulder. | X-ray showed osteoarthritic changes at the glenohumeral junction and reverse Hill–Sachs defect, in addition to abnormal hepatomarkers. The causes are attributed to the excessive use of PIEDs and injected oils, lack of load control, and psychological problems. | Hameed et al., 2016 [48] |
| Systematic Review/Qualitative Analysis | 67 references (includes articles from January 1995 to January 2014). | To summarize and update scientific knowledge on different topics and guidelines related to the prescription of strength training in young prepubertal and adolescent populations. | Literature search in PubMed, Scopus, SportDiscus, ScienceDirect, and Google Scholar databases using the following specific search terms: children, adolescents, youth, youth athletes, pediatric, strength training, resistance training, weight training, motor performance skill. | Causes of strength-training-related injuries in young population are due to misuse of equipment, excessive loads, faulty techniques, or lack of qualified supervision. Avoid or minimize exercises that involve excessive load or compression or shear stress to the spine. Qualified adult instruction, low coach/athlete ratio, frequent and quality feedback, and execution of new exercises without fatigue are recommended. | Peña et al., 2016 [49] |
| RCT/Quantitative Analysis | n = 88 (59F; 29M) Portuguese adolescents (15-17 years old) were randomly assigned to a control (n = 46) or experimental (n = 42) group. | (i) To evaluate the effects of a 32-weeks resistance and stretching training program applied in physical education classes on forward head posture and protracted shoulder. (ii) To evaluate in adolescents submitted to strength and stretching exercises the effects of a 16-week detraining period. | Strengthening and stretching exercises + posture alignment assessment (cervical and shoulder angle) with photogrammetric method using a software for postural analysis + ASES questionnaire for self-assessment of shoulder pain and function, as well as neck pain. | A 32-week posture corrective exercise program (strength and stretching), in addition to physical education classes, improves postural control with increases in cervical and shoulder angles in adolescents aged 15 to 17 years. In addition, when a four-month detraining period is given, the adaptations are not lost. | Ruivo et al., 2016 [50] |
| RCT/Quantitative Analysis | n = 33 (15F; 18 M) physically active participants were randomly assigned to hip flexor training (n = 16) or control (n = 17); only 26 completed the study and were included in the analysis. | To investigate the feasibility and effect of a novel simple hip flexor strength training program in healthy subjects, using elastic bands as external loading. | Maximal isomeric hip flexion strength in the dominant leg using a hand-held dynamometer (Powertrack II Commander, JTECH Medical) + delayed onset muscle soreness (pain) using numerical rating scale + rate of perceived exertion using the BorgCR10 scale | A 6-week hip flexor strength training program using elastic bands with isometric action on the dominant leg improved hip flexor muscle strength by 17%. These types of interventions may favor the prevention and treatment of acute long-term hip flexor injuries, such as acute rectus femoris injuries and longstanding iliopsoas-related pain and impingement. | Thorborg et al., 2016 [51] |
| Systematic Review/Qualitative Analysis | 20 references (includes articles from their year of publication until 2015). | To systematically review the injury epidemiology of weight training sports using a list of injury epidemiology outcomes advocated by the IOC and to evaluate if demographic features influence the injury epidemiology. | Literature search in PubMed, SPORTDiscus, CINAHL, and Embase databases using Boolean algorithms containing key words such as wound, rupture, sprain, strain, and tear in weight training sports (weightlifting, powerlifting, bodybuilding, strongman, Highland Games, and CrossFit). | Mild (exercise execution required modification) to moderate (stopped performing the exercise) injuries were reported in the shoulders, knee, and lower back. The injury rate in weight sports (≈1–2 injuries per athlete per year and ≈2–4 injuries per 1000 h of training/competition exposure) was lower than those reported in most team sports, with Highland Games and strongman having the highest rates. | Keogh & Winwood, 2017 [52] |
| Narrative Review/Qualitative Analysis | 134 references (includes articles from 1982 to 2016). | To synthesize and review the most recent literature related to young athlete development as it pertains to resistance training and physical literacy. | Literature search in PubMed and SPORTDiscus databases using: strength training OR resistance training AND children, strength training OR resistance training AND adolescents, strength training OR resistance training AND injury prevention, physical literacy, and young athlete development. | Weight RT training serves as injury prevention. A multifaceted RT program with skilled instruction can ensure that diversification of motor skill development occurs before the onset of puberty, preventing patellofemoral disorders, fractures, or ACL tears. | Zwolski et al., 2017 [53] |
| Narrative Review/Qualitative Analysis | 110 references (includes articles from year of publication to May 2017). | To provide an evidence-based framework for the selection of hamstring strengthening exercises that reduce the rate of injury to this muscle group. | Literature search in Scopus and PubMed databases using three Boolean algorithms. | The benefits of strength training may be due to increased biceps femoris long head fascicle length, possibly a rightward shift in the angle of peak knee flexor torque, and improved eccentric knee flexor strength. | Bourne et al., 2018 [54] |
| RCT/Quantitative Analysis | 21M (22.4 ± 2.2 years old with at least three years of strength training experience performing traditional and Romanian deadlifts). | To determine which deadlift technique is a better training protocol between the conventional and Romanian deadlifts as indicated by the greater demand in muscle activities and joint kinetics. | Fifty-nine markers were placed on anatomical landmarks for kinematic analysis using a six-camera VICON motion capture system + ground reaction force data using AMIT force plates + EMG analysis using the Desktop DTS, a three-channel wireless system. | The conventional deadlift resulted in significantly greater EMG activities ofthe rectus femoris and gluteus maximus than those of the Romanian deadlift. Additionally, convenitional deadlift produced greater knee and ankle net joint torques than the Romanian version. In conclusion, the conventional deadlift might be a better technique for training lower extremity muscles. | Lee et al., 2018 [55] |
| Systematic Review with Meta-Analysis/Qualitative and Quantitative Analysis | Six references (includes articles from year of publication 2017). A total of 7738 subjects aged from 12 to 40 years. | To systematically identify and analyze qualitatively and quantitatively RCTs of strength training-based sports injury prevention programs. | Literature search in PubMed, Embase, Web of Science, and SPORTDiscus databases for RCTs using keywords related to exercise programs, prevention, injury, and diagnoses. | Significant reduction in acute hamstring and ACL injuries by incorporating strengthening of the frequently injured muscles. To prevent ACL injury and reduce anterior knee pain, it is advisable to improve strength and coordination in the knees, pelvis, and core. Incorporate familiarization phase, recovery weeks, and individualized programs to reduce the risk of injury from overuse. | Lauersen et al., 2018 [56] |
| Cross-sectional/Quantitative Analysis | n = 104 (53F; 51M) subelite Swedish powerlifters | To investigate the prevalence, localization, and characterization of injuries among Swedish subelite classic powerlifters, with an emphasis on differences between men and women, and to investigate whether training and lifestyle factors are associated with an injury. | Web-based adapted questionnaire: the majority of questions required a dichotomous answer (yes/no), while the other questions offered several categorical answers or called for an open-ended response. | The lumbopelvic region, shoulder, and hip present more injuries in both sexes (70% reported a current injury, and 87% reported being injured during the past 12 months). Women more frequently experienced injuries in the neck and thoracic region than men. Incorporating rehabilitation exercises, emphasis on technique, warm-up, and flexibility are associated with significant improvements. | Strömbäck et al., 2018 [57] |
| Narrative Review/Qualitative Analysis | 62 references (includes articles from year of publication to 2016). | To review the National Strength and Conditioning Association’s 2016 Position Statement on Long-Term Athletic Development. | Literature search in the PubMed database using the following specific search terms: youth sports injuries, early sports specialization, training and maturation, training versus developmental stage, and long-term athletic development. | Weight RT has been shown to reduce the risk of injury in youth population. Besides adequate recovery time, it is recommended that children and adolescents train strength two to three days per week (between 60 and 80% 1RM, 8 to 15 reps). Exercises that increase the genu varu/valgus, joint hypermobility, leg length discrepances, pelvic rotation, height, muscle tightness, large Q angle, and ratio of explosive-to-static strength might increase the risk of injuries. | Walters et al., 2018 [58] |
| RCT/Quantitative Analysis | 67 New Zealand school boys (aged 12–14 years) were randomily assigned to either combined RT (n = 21), combined RT + weightlifting (n = 19), or control (n = 27) | To investigate how combined RT with or without weightlifting movements affect injury risk factors (jump landing kinematics and interlimb asymmetry) as well as resistance training skill. | Anthropometric measures + resistance training skills battery + tuck jump assessment + single-leg horizontal jump + modified star excursion balance test + isometric midthigh pull test | A 28-week combined RT program improved tuck jump scores more than combined RT + weightlifting and regular physical education curriculum. Practitioners can use a combination of traditional RT, plyometric, and weightlifting training to reduce injury risk factors associated with jump landings and improve resistance training skill competency. | Pichardo et al., 2019 [59] |
| Prospective Clinical Trial/Quantitative Analysis | n = 100 (80F; 20M) healthy adults (22 to 64 years) | To identify the injury rate during HIFT (e.g., “boot camp”-style classes, military training, or CrossFit). | Self-reported injury rate and injury location + self-reported training time + demographic data + record of exercise types and pain | The injury rate during HIFT was 9.0 injuries per 1000 training hours. No sex differences were found. The most common locations injured were knees and back, particularly with non-ballistic weightlifting (free weights), plyometrics, and calisthenics, as well as burpees and squats. | Batterson et al., 2020 [60] |
| Narrative Review/Qualitative Analysis | 55 references (includes articles from year of publication to 2020). | To overview injuries and overload damage in weight RT. | Literature search with clinical and practical aspects. A retrospective, citation-based methodology was applied. | The shoulder, knee, and lower back are the most common locations for injuries. Exercises such as behind-the-neck presses, behind-the-neck lat pulls, biceps curls with the straight bar, triceps presses with the straight bar, good mornings, and exercises in maximum stretch should generally be avoided. | Ritsch 2020 [61] |
| Systematic Review/Qualitative Analysis | 12 references from 2010 to 2018. | To analyze in detail the prevalence of injuries occurring in training based on the CrossFit®, cross-training, or HIFT modalities. | Literature search in PubMed, Web of Science, SPORTDiscus, and Scopus databases using Boolean algorithms containing CrossFit, extreme conditioning program, cross-training, HIFT (high-intensity functional training), and HIPT (high-intensity power training). | The shoulder joint is the anatomical area with the highest prevalence of injury in CrossFit®, cross-training, or HIFT methodologies (9/12 studies). The rate or ratio of injury depends on a wide variety of variables to consider (previous injuries, protocol used, presence of qualified coaches, etc.). | Barranco-Ruiz et al., 2020 [62] |
| Retrospective cross-sectional study/Quantitative Analysis | n = 213 (112M; 101F) from three Brazilian PFC. | To verify the anatomical sites with the highest occurrence of injuries and the number and possible risk factors for injuries in HIFT practitioners in the last six months. | Questionnaire as retrospective survey to evaluate injury rate. | In total, 38.50% of the participants had suffered some type of injury caused by the HIFT training routine, and about 70.7% experienced their first injury only after initiating training. The injury rate was 7.1 injuries for every 1000 h of training (higher risk in advanced practitioners), and the majority of the injuries affected the shoulder, lumbar area, knee, and wrist. Injury causes were incorrect execution techniques, recurrent efforts, and high loads. | Texeira et al., 2020 [63] |
| Case study with literature review/Quantitative and Qualitative Analysis | A 26-years old elite weightlifter with 4 years of experience. | To describe the case of a elite weightlifter who suffered from bilateral quadriceps muscle/tendon rupture. Also, to assess the risk factors, types of presentation, and management of such cases by revieweling literature. | Medical history + clinical examination + NMR imaging of both legs + literature search in PubMed using Boolean terms with keywords such as bilateral quadriceps muscle, quadriceps muscle, rupture, tear, lacerations, and sports. | The case of the elite weightlifter who ruptured both his quadriceps muscles/tendons during competition was retrospectively found to have a history of AAS use. The literature review revealed 11 cases of sports-related bilateral quadriceps tendon ruptures, five of which were weightlifters and two were in bodybuilders (5/7 had a history of AAS use, infuencing the extensor mechanism strength). | Dhillon et al., 2020 [64] |
| Clinical trial/Qualitative Analysis | n = 11 (26.8 ± 2.4 years) healthy male participants with > 3 years of RT experience | (i) To quantify, with musculoskeletal modeling, the loading of key upper limb and torso muscles during several pull-up variants. (ii) To examine the effect of different kinematic strategies on muscle recruitments. (iii) To highlight potential injury risks in concentric loading of vulnerable structures in these tasks. | Retro-reflective passive markers (21) were placed on anatomical landmarks of the thorax, clavicle, humerus, and forearm, and a scapula tracker incorporating three markers was placed along the scapular spine + kinematic data using a 9-camera optical motion system (200 Hz Vicon) + external kinetic data using a force platform (1000 Hz Kistler) + UK National Shoulder Model was used to simulate biomechanics of the clavicle, scapula, humerus, and forearm | There is potential injury risk in concentric loading of vulnerable structures, specifically the rotator cuff muscles, under complex and strenuous movement patterns involving high upper limb elevation. Given their heavy load and multiplanar complexity, pull-ups should be implemented as a late-stage component in shoulder rehabilitation and conditioning programs. All three pull-up variants (front, wide, and reverse grips) should be incorporated into the exercise program with systematic progression to provide greater global strengthening of the torso and upper limb musculature. | Urbanczyk et al., 2020 [65] |
| RCT/Qualitative Analysis | n = 29 female soccer players (16.4 ± 1.6 years) were randomly assigned to experimental (n = 18) or control (n = 11). | To evaluate the changes in biomechanical risk factors for an ACL injury after participation in a pelvic and core strength training program in female team players. | All measures were collected during bilateral and unilateral drop jumps. Knee frontal plane projection angle + hip, knee, and ankle peak flexion angles + jump height | An in-season 8-weeks pelvic and core strength training program (twice per week) resulted in improvements on ACL injury risk factors and vertical drop jump performance. Strengthening this body part might support injury prevention while increasing jumping performance. | Ferri-Caruana et al., 2020 [66] |
| Systematic Review/Qualitative Analysis | 11 references (includes articles from from year of publication to January 2020). | To analyse the literature concerning powerlifting injuries, focusing on the injury rates, areas of injury, and biomechanical movement analysis. | Literature search in PubMed and Google Scholar databases using the search terms powerlifting and injury. | The injury rates in powerlifting were between 1.0 and 4.4 per 1000 h of training (lower than other strength sports). Most injuries were found in shoulders, lower back, elbows, and knees. Experienced lifters were more prone to overuse or chronic injuries, whereas novice lifters were more likely to experience acute injuries. | Dudagoitia et al., 2021 [67] |
| RCT/Qualitative Analysis | n = 48 recreationally active men (22.4 ± 2.6 years) were randomly assigned to experimental (n = 32) or control (n = 16). | To examine the effects of core muscle strengthening on lower extremity joint kinematics and muscle activation of selected trunk and lower extremity muscles during side-step cutting. | Kinematic data of the trunk, hip, knee, and ankle joints using a 3-dimensional motion capture system (Motion Analysis Corp) + electromyography analysis (LXM5308) + core stability test using prone and sideplank endurance tests | A 10-week core strength training program alters the motor control strategy and at-risk biomechanical parameters associated with an ACL injury during the cutting maneuver by reducing the knee valgus and hip adduction angles and increasing the vastus medialis/lateralis and hamstring/quadricep activation ratio. | Jeong et al., 2021 [68] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bonilla, D.A.; Cardozo, L.A.; Vélez-Gutiérrez, J.M.; Arévalo-Rodríguez, A.; Vargas-Molina, S.; Stout, J.R.; Kreider, R.B.; Petro, J.L. Exercise Selection and Common Injuries in Fitness Centers: A Systematic Integrative Review and Practical Recommendations. Int. J. Environ. Res. Public Health 2022, 19, 12710. https://doi.org/10.3390/ijerph191912710
Bonilla DA, Cardozo LA, Vélez-Gutiérrez JM, Arévalo-Rodríguez A, Vargas-Molina S, Stout JR, Kreider RB, Petro JL. Exercise Selection and Common Injuries in Fitness Centers: A Systematic Integrative Review and Practical Recommendations. International Journal of Environmental Research and Public Health. 2022; 19(19):12710. https://doi.org/10.3390/ijerph191912710
Chicago/Turabian StyleBonilla, Diego A., Luis A. Cardozo, Jorge M. Vélez-Gutiérrez, Adrián Arévalo-Rodríguez, Salvador Vargas-Molina, Jeffrey R. Stout, Richard B. Kreider, and Jorge L. Petro. 2022. "Exercise Selection and Common Injuries in Fitness Centers: A Systematic Integrative Review and Practical Recommendations" International Journal of Environmental Research and Public Health 19, no. 19: 12710. https://doi.org/10.3390/ijerph191912710
APA StyleBonilla, D. A., Cardozo, L. A., Vélez-Gutiérrez, J. M., Arévalo-Rodríguez, A., Vargas-Molina, S., Stout, J. R., Kreider, R. B., & Petro, J. L. (2022). Exercise Selection and Common Injuries in Fitness Centers: A Systematic Integrative Review and Practical Recommendations. International Journal of Environmental Research and Public Health, 19(19), 12710. https://doi.org/10.3390/ijerph191912710











