The Impact of Physical Activity at School on Body Fat Content in School-Aged Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Fat Content Measurement
2.4. Statistical Analysis
3. Results
3.1. Group Characteristics
3.2. Body Fat Content
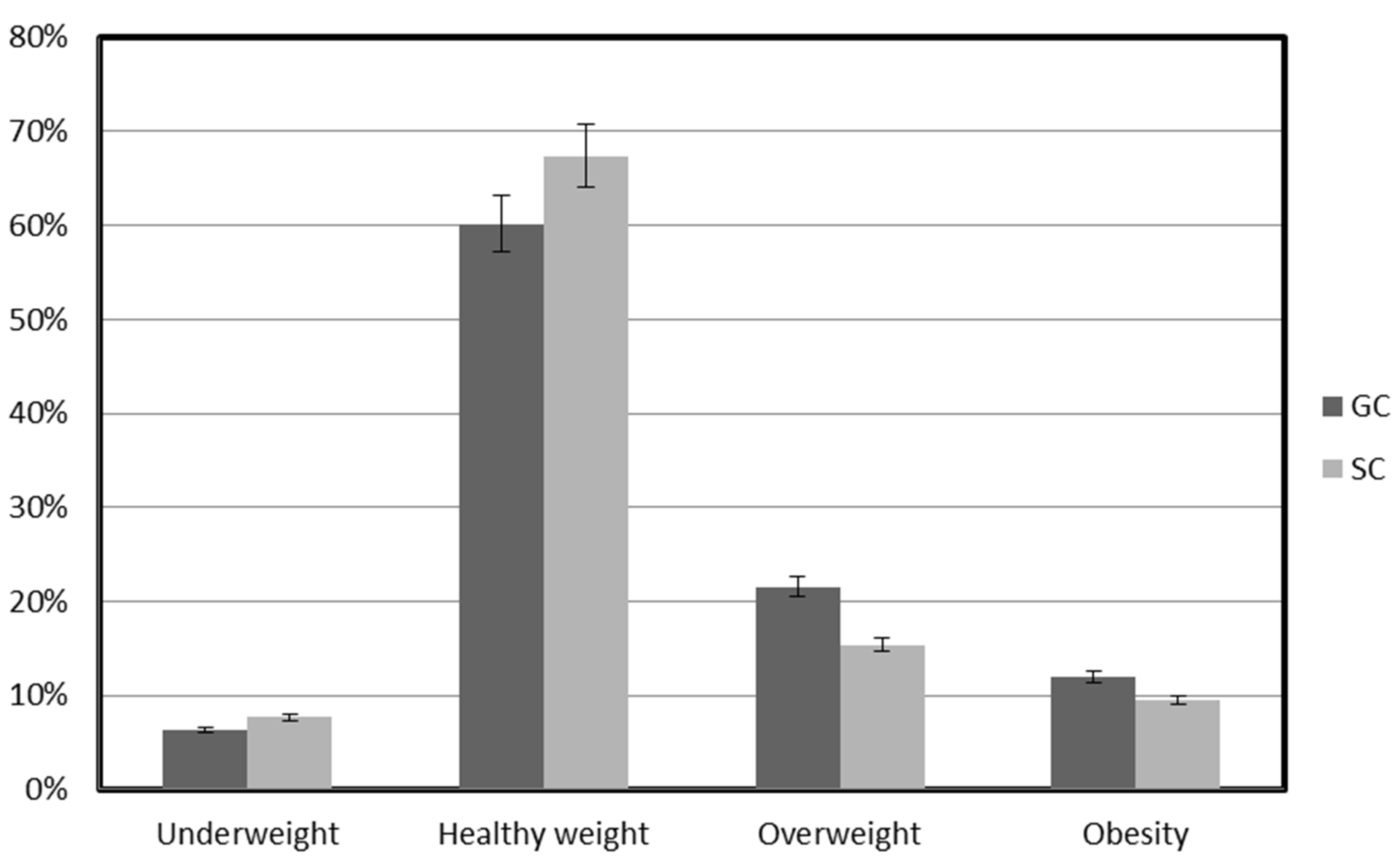
3.3. Categorization of Body Fat Content
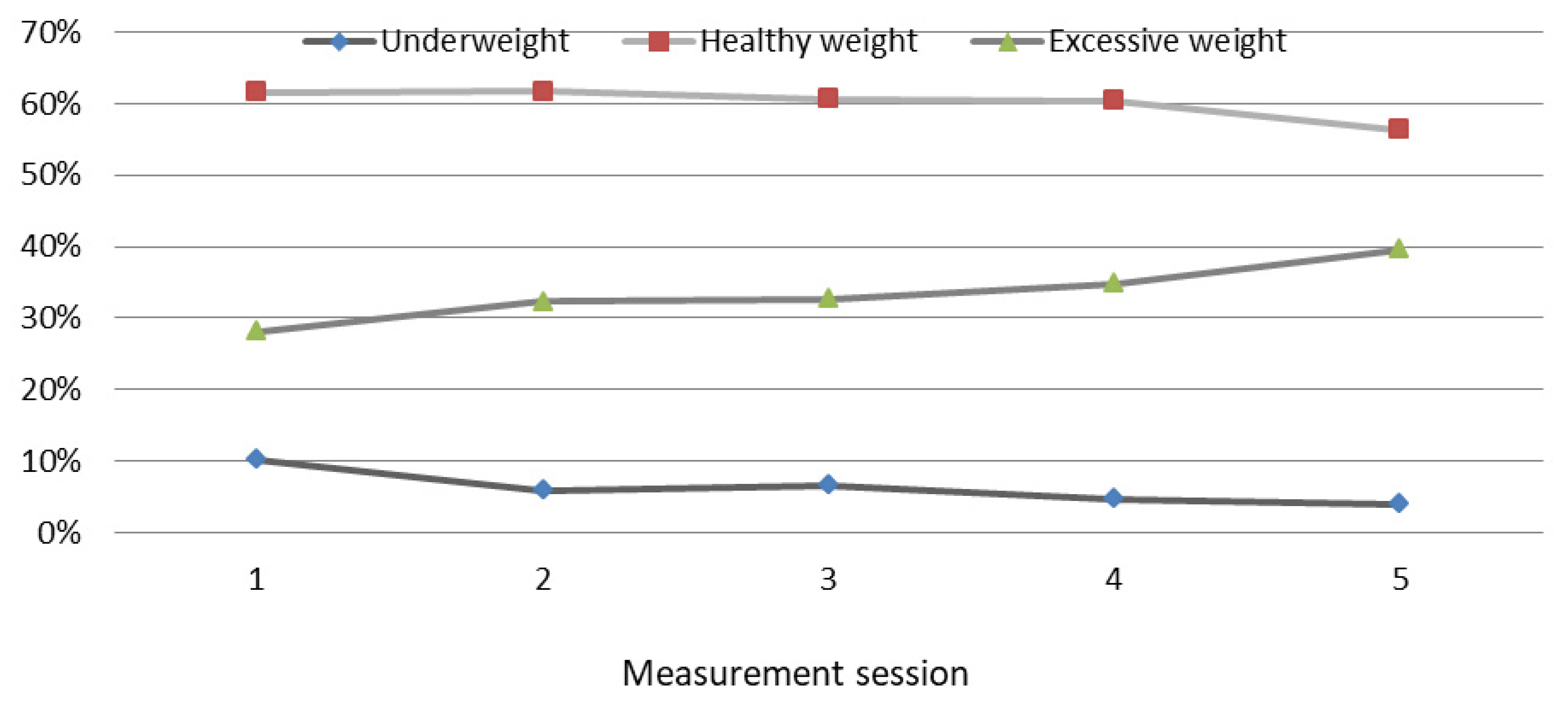
3.4. Analysis of Fat Content Variability during the Study
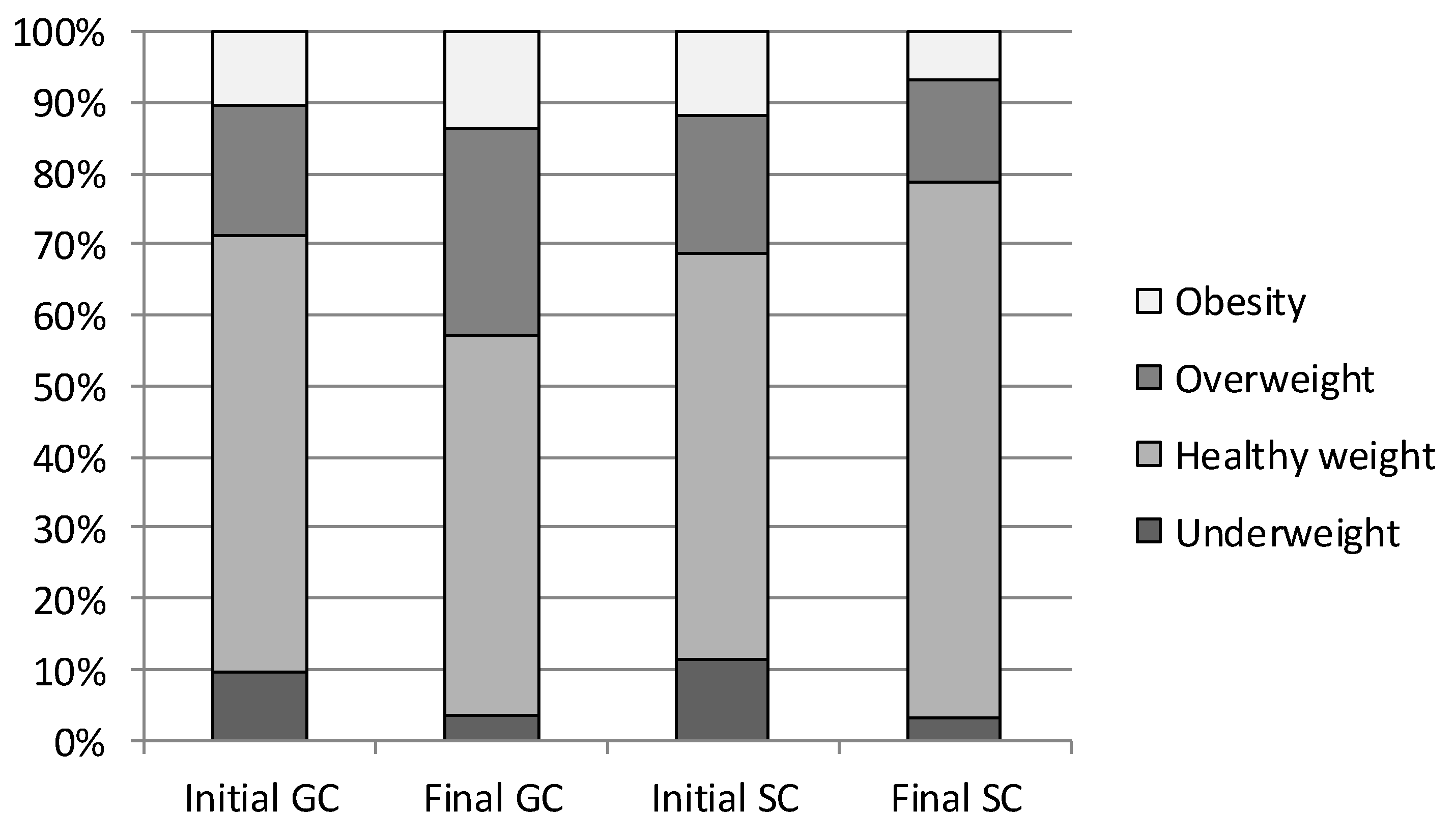
3.5. Analysis of Fat Content Variability between Initial and Final Measurements
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, E.Y.; Yoon, K.H. Epidemic obesity in children and adolescents: Risk factors and prevention. Front. Med. 2018, 12, 658–666. [Google Scholar] [CrossRef]
- Ackland, T.R.; Lohman, T.G.; Sundgot-Borgen, J.; Maughan, R.J.; Meyer, N.L.; Stewart, A.D.; Müller, W. Current status of body composition assessment in sport: Review and position statement on behalf of the ad hoc research working group on body composition health and performance, under the auspices of the I.O.C. Medical Commission. Sport. Med. 2012, 42, 227–249. [Google Scholar] [CrossRef]
- Goossens, G.H. The Metabolic Phenotype in Obesity: Fat Mass, Body Fat Distribution, and Adipose Tissue Function. Obes. Facts. 2017, 10, 207–215. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 June 2022).
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [CrossRef]
- Gensthaler, L.; Felsenreich, D.M.; Jedamzik, J.; Eichelter, J.; Nixdorf, L.; Bichler, C.; Krebs, M.; Itariu, B.; Langer, F.B.; Prager, G. Trends of Overweight and Obesity in Male Adolescents: Prevalence, Socioeconomic Status, and Impact on Cardiovascular Risk in a Central European Country. Obes. Surg. 2022, 32, 1024–1033. [Google Scholar] [CrossRef]
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; Di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European World Health Organization member states. Epidemiological data, medical-social aspects, and prevention programs. Clin. Ter. 2019, 170, 223–230. [Google Scholar]
- WHO. Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. World Health Organization. 2000. Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 14 June 2022).
- Jarosz, M.; Charzewska, J.; Wolnicka, W.; Wajszczyk, B.; Chwojnowska, Z.; Taraszewska, A.; Jaczewska-Schuetz, J. Nutritional status of children and adolescents-preliminary results the programme KIK/34 “Preventing overweight and obesity” in Swiss-Polish Cooperation Programme. Hum. Nutr. Metabol. 2016, 43, 231–238. [Google Scholar]
- Fijałkowska, A.; Oblacińska, A.; Stalmach, M. Nadwaga i Otyłość u Polskich 8-Latków w Świetle Uwarunkowań Biologicznych, Behawioralnych i Społecznych. Raport z Międzynarodowych Badań WHO European Childhood Obesity Surveillance Initiative (COSI). Warszawa. 2017. Available online: http://www.imid.med.pl/ (accessed on 12 June 2022).
- Weker, H.; Socha, P.; Szajewska, H. Raport z Badania: Kompleksowa Ocena Sposobu Żywienia Dzieci w Wieku od 5 do 36 Miesiąca Życia-Badanie Ogólnopolskie 2016 Rok Pitnus. 2016. Warszawa. 2017. Available online: https://fundacjanutricia.pl/uploads/research-files/February2021/JF44fjZMhLhAHSqb5qvk.pdf (accessed on 12 June 2022).
- World Health Organization. WHO European Regional Obesity Report 2022; World Health Organization: Geneva, Switzerland. Available online: https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf (accessed on 12 June 2022).
- Güngör, N.K. Overweight and obesity in children and adolescents. J. Clin. Res. Pediatr. Endocrinol. 2014, 6, 129–143. [Google Scholar] [CrossRef]
- Hubbard, V.S. Defining overweight and obesity: What are the issues? Am. J. Clin. Nutr. 2000, 72, 1067–1068. [Google Scholar] [CrossRef]
- Nielsen, T.R.H.; Fonvig, C.E.; Dahl, M.; Mollerup, P.M.; Lausten-Thomsen, U.; Pedersen, O.; Hansen, T.; Holm, J.C. Childhood obesity treatment; Effects on BMI SDS, body composition, and fasting plasma lipid concentrations. PLoS ONE 2018, 113, e0190576. [Google Scholar] [CrossRef]
- Vanderwall, C.; Randall Clark, R.; Eickhoff, J.; Carrel, A.L. BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr. 2017, 17, 135. [Google Scholar] [CrossRef]
- Jonnalagadda, S.S.; Skinner, R.; Moore, L. Overweight athlete: Fact or fiction? Curr. Sport. Med. Rep. 2004, 3, 198–205. [Google Scholar] [CrossRef]
- Rogol, A.D.; Clark, P.A.; Roemmich, J.N. Growth and pubertal development in children and adolescents: Effects of diet and physical activity. Am. J. Clin. Nutr. 2000, 72, 521–528. [Google Scholar] [CrossRef]
- Kuriyan, R. Body composition techniques. Indian J. Med. Res. 2018, 148, 648–658. [Google Scholar] [CrossRef]
- Weber, D.R.; Leonard, M.B.; Zemel, B.S. Body composition analysis in the pediatric population. Pediatr. Endocrinol. Rev. 2012, 10, 130–139. [Google Scholar]
- Holmes, C.J.; Racette, S.B. The Utility of Body Composition Assessment in Nutrition and Clinical Practice: An Overview of Current Methodology. Nutrients 2021, 13, 2493. [Google Scholar] [CrossRef]
- McCarthy, H.D.; Cole, T.J.; Fry, T.; Jebb, S.A.; Prentice, A.M. Body fat reference curves for children. Int. J. Obes. 2006, 30, 598–602. [Google Scholar] [CrossRef]
- Komiya, H.; Masubuchi, Y.; Mori, Y.; Tajima, N. The validity of body mass index criteria in obese school-aged children. Tohoku J. Exp. Med. 2008, 214, 27–37. [Google Scholar] [CrossRef][Green Version]
- Williams, D.P.; Going, S.B.; Lohman, T.G.; Harsha, D.W.; Srinivasan, S.R.; Webber, L.S.; Berenson, G.S. Body fatness and risk for elevated blood pressure, total cholesterol, and serum lipoprotein ratios in children and adolescents. Am. J. Public Health 1992, 82, 358–363. [Google Scholar] [CrossRef]
- Haberka, M.; Stolarz-Skrzypek, K.; Biedroń, M.; Szóstak-Janiak, K.; Partyka, M.; Olszanecka-Glinianowicz, M.; Gąsior, Z. Obesity, Visceral Fat, and Hypertension-Related Complications. Metab. Syndr. Relat. Disord. 2018, 16, 521–529. [Google Scholar] [CrossRef]
- Chwałczyńska, A.; Andrzejewski, W. Changes in Body Mass and Composition of the Body as Well as Physical Activity and Time Spent in Front of the Monitor by Students of the Wroclaw University of Health and Sport Sciences during the Period of COVID-19 Restrictions. Int. J. Environ. Res. Public Health 2021, 18, 7801. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.R. Body composition in athletes and sports nutrition: An examination of the bioimpedance analysis technique. Eur. J. Clin. Nutr. 2013, 67, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Liao, Y.; Chang, S.H.; Miyashita, M.; Stensel, D.; Chen, J.F.; Wen, L.T.; Nakamura, Y. Associations between health-related physical fitness and obesity in Taiwanese youth. J. Sport. Sci. 2013, 31, 1797–1804. [Google Scholar] [CrossRef] [PubMed]
- Burns, R.; Hannon, J.C.; Brusseau, T.A.; Shultz, B.; Eisenman, P. Indices of abdominal adiposity and cardiorespiratory fitness test performance in middle-school students. J. Obes. 2013, 2013, 912460. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Zembura, P.; Korcz, A.; Cieśla, E.; Gołdys, A.; Nałȩcz, H. Results from Poland’s 2018 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2018, 15, S395–S397. [Google Scholar] [CrossRef]
- Ng, A.K.; Hairi, N.N.; Jalaludin, M.Y.; Majid, H.A. Dietary intake, physical activity and muscle strength among adolescents: The Malaysian Health and Adolescents Longitudinal Research Team (MyHeART) study. BMJ Open 2019, 9, e026275. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Fairclough, S.; Beighle, A.; Erwin, H.; Ridgers, N. School day segmented physical activity patterns of high and low active children. BMC Publ. Health 2012, 12, 406. [Google Scholar] [CrossRef]
- Møller, N.C.; Tarp, J.; Kamelarczyk, E.F.; Brønd, J.C.; Klakk, H.; Wedderkopp, N. Do extra compulsory physical education lessons mean more physically active children—Findings from the childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). Int. J. Behav. Nutr. Phys. Act. 2014, 11, 121. [Google Scholar] [CrossRef] [PubMed]
- Dziennik Ustaw Rzeczypospolitej Polskiej. Poz. 2138 Rozporządzenie Ministra Edukacji Narodowej. w Sprawie Oddziałów i Szkół Sportowych Oraz Oddziałów i Szkół Mistrzostwa Sportowego. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20200002138/O/D20202138.pdf (accessed on 5 July 2022).
- Ip, P.; Ho, F.-W.; Louie, L.-T.; Chung, T.-H.; Cheung, Y.-F.; Lee, S.-L.; Hui, S.-C.; Ho, W.-Y.; Ho, D.-Y.; Wong, W.-S.; et al. Childhood obesity and physical activity-friendly school environments. J. Pediatr. 2017, 191, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Valkenborghs, S.R.; Noetel, M.; Hillman, C.H.; Nilsson, M.; Smith, J.J.; Ortega, F.B.; Lubans, D.R. The Impact of Physical Activity on Brain Structure and Function in Youth: A Systematic Review. Pediatrics 2019, 144, e20184032. [Google Scholar] [CrossRef] [PubMed]
- Kolanowski, W.; Ługowska, K.; Trafialek, J. Increased Physical Activity at School Benefits Arterial Blood Pressure in Children—A Prospective Follow-Up Cohort Study. Int. J. Environ. Res. Publ. Health 2022, 19, 4662. [Google Scholar] [CrossRef] [PubMed]
- Ługowska, K.; Kolanowski, W.; Trafialek, J. Eating Behaviour and Physical Fitness in 10-Year-Old Children Attending General Education and Sports Classes. Int. J. Environ. Res. Publ. Health 2020, 5, 6467. [Google Scholar] [CrossRef] [PubMed]
- Ługowska, K.; Kolanowski, W.; Trafialek, J. The Impact of Physical Activity at School on Children’s Body Mass during 2 Years of Observation. Int. J. Environ. Res. Public Health 2022, 19, 3287. [Google Scholar] [CrossRef]
- Klepac Pogrmilovic, B.; O’Sullivan, G.; Milton, K.; Biddle, S.J.H.; Pedisic, Z. A Systematic Review of Instruments for the Analysis of National-Level Physical Activity and Sedentary Behaviour Policies. Health Res. Policy Syst. 2019, 17, 86. [Google Scholar] [CrossRef]
- Ortega, F.B.; Cadenas-Sanchez, C.; Migueles, J.H.; Labayen, I.; Ruiz, J.R.; Sui, X.; Blair, S.N.; Martínez-Vizcaino, V.; Lavie, C.J. Role of Physical Activity and Fitness in the Characterization and Prognosis of the Metabolically Healthy Obesity Phenotype: A Systematic Review and Meta-analysis. Prog. Cardiovasc. Dis. 2018, 61, 190–205. [Google Scholar] [CrossRef]
- Farbo, D.J.; Rhea, D.J. A Pilot Study Examining Body Composition Classification Differences Between Body Mass Index and Bioelectrical Impedance Analysis in Children With High Levels of Physical Activity. Front. Pediatr. 2021, 9, 724053. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Orsso, C.E.; Gonzalez, M.C.; Maisch, M.J.; Haqq, A.M.; Prado, C.M. Using bioelectrical impedance analysis in children and adolescents: Pressing issues. Eur. J. Clin. Nutr. 2022, 76, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Kabiri, L.S.; Hernandez, D.C.; Mitchell, K. Reliability, Validity, and Diagnostic Value of a Pediatric Bioelectrical Impedance Analysis Scale. Child Obes. 2015, 11, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Tanita SC-240MA Instruction Manual. Tanita User Manual SC 240 MA. Available online: https://www.manualslib.com/manual/1065295/Tanita-Sc-240ma.html (accessed on 12 July 2022).
- Marfell-Jones, M.; Old, T.; Steward, A.; Carter, J.E.L. International Standards for Anthropometric Assessment; ISAK: Palmerston North, New Zealand, 2012. [Google Scholar]
- Kulaga, Z.; Litwin, M.; Tkaczyk, M.; Rózdzyńska, A.; Barwicka, K.; Grajda, A.; Swiader, A.; Gurzkowska, B.; Napieralska, E.; Pan, H. The height-, weight-, and BMI-for-age of Polish school-aged children and adolescents relative to international and local growth references. BMC Publ. Health 2010, 10, 109. [Google Scholar] [CrossRef] [PubMed]
- Van Eyck, A.; Eerens, S.; Trouet, D.; Lauwers, E.; Wouters, K.; De Winter, B.Y.; van der Lee, J.H.; Van Hoeck, K.; Ledeganck, K.J. Body composition monitoring in children and adolescents: Reproducibility and reference values. Eur. J. Pediatr. 2021, 180, 1721–1732. [Google Scholar] [CrossRef] [PubMed]
- Kyle, U.G.; Earthman, C.P.; Pichard, C.; Coss-Bu, J.A. Body composition during growth in children: Limitations and perspectives of bioelectrical impedance analysis. Eur. J.Clin. Nutr. 2015, 69, 1298–1305. [Google Scholar] [CrossRef]
- Kushner, R.F.; Gudivaka, R.; Schoeller, D.A. Clinical characteristics influencing bioelectrical impedance analysis measurements. Am. J. Clin. Nutr. 1996, 64, 423–427. [Google Scholar] [CrossRef]
- StatSoft. Elektroniczny Podręcznik Statystyki. Kraków. 2006. Available online: https://www.statsoft.pl/textbook/stathome.html (accessed on 14 July 2022).
- Sullivan, G.M.; Feinn, R. Using Effect Size—Or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
- Alpízar, M.; Frydman, T.D.; Reséndiz-Rojas, J.J.; Trejo-Rangel, M.A.; Aldecoa-Castillo, J.M. Fat Mass Index (FMI) as a Trustworthy Overweight and Obesity Marker in Mexican Pediatric Population. Children 2020, 7, 19. [Google Scholar] [CrossRef]
- Parrish, A.M.; Tremblay, M.S.; Carson, S.; Veldman, S.L.C.; Cliff, D.; Vella, S.; Chong, K.H.; Nacher, M.; del Pozo Cruz, B.; Ellis, Y.; et al. Comparing and assessing physical activity guidelines for children and adolescents: A systematic literature review and analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 16. [Google Scholar] [CrossRef]
- Vicente-Rodríguez, G.; Benito, P.J.; Casajús, J.A.; Ara, I.; Aznar, S.; Castillo, M.J.; Dorado, C.; González-Agüero, A.; González-Gallego, J.; Gonzalez-Gross, M.; et al. Physical activity, exercise and sport practice to fight against youth and childhood obesity. Nutr. Hosp. 2016, 33, 1–21. [Google Scholar]
- Słowik, J.; Grochowska-Niedworok, E.; Maciejewska-Paszek, I.; Kardas, M.; Niewiadomska, E.; Szostak-Trybuś, M.; Palka-Słowik, M.; Irzyniec, T. Nutritional Status Assessment in Children and Adolescents with Various Levels of Physical Activity in Aspect of Obesity. Obes. Facts. 2019, 12, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Korcz, A.; Monyeki, M.A. Association Between Sport Participation, Body Composition, Physical Fitness, and Social Correlates Among Adolescents: The PAHL Study. Int. J. Environ. Res. Public Health 2018, 15, 2793. [Google Scholar]
- Dassanayake, T.D.M.S.B.; Rajarathna, A.A.J.; Rajarathna, S.A. Comparison of BMI and body fat percentages between national level teenage swimmers and controls. Adv. Obes. Weight Manag. Contr. 2016, 4, 00109. [Google Scholar] [CrossRef]
- Ubago-Guisado, E.; Mata, E.; Sánchez-Sánchez, J.; Plaza-Carmona, M.; Martín-García, M.; Gallardo, L. Influence of different sports on fat mass and lean mass in growing girls. J. Sport Health Sci. 2017, 6, 213–218. [Google Scholar] [CrossRef]
- Bielec, G.; Goździejewska, A. Nutritional habits of 11–12-year-old swimmers against non-athlete peers—A pilot study. Pediatr. Endocrinol. Diabetes Metab. 2018, 24, 72–81. [Google Scholar] [CrossRef]
- Vehrs, P.R.; Fellingham, G.W.; McAferty, A.; Kelsey, L. Trends in BMI Percentile and Body Fat Percentage in Children 12 to 17 Years of Age. Children 2022, 19, 744. [Google Scholar] [CrossRef]
- Santos, L.P.; Santos, I.S.; Matijasevich, A.; Barros, A.J.D. Changes in overall and regional body fatness from childhood to early adolescence. Sci. Rep. 2019, 9, 1888. [Google Scholar] [CrossRef]
- López-Sánchez, G.F.; Sgroi, M.; D’Ottavio, S.; Díaz-Suárez, A.; González-Víllora, S.; Veronese, N.; Smith, L. Body Composition in Children and Adolescents Residing in Southern Europe: Prevalence of Overweight and Obesity According to Different International References. Front. Physiol. 2019, 10, 130. [Google Scholar] [CrossRef]
- Shaw, N.J.; Crabtree, N.J.; Kibirige, M.S.; Fordham, J.N. Ethnic and gender differences in body fat in British schoolchildren as measured by DXA. Arch. Dis. Child. 2007, 92, 872–875. [Google Scholar] [CrossRef]
- Taylor, R.W.; Grant, A.M.; Williams, S.M.; Gouldinig, A. Sex differences in regional fat distribution from pre- to postpuberty. Obesity 2010, 18, 1410–1416. [Google Scholar] [CrossRef]
- Petri, C.; Mascherini, G.; Bini, V.; Toncelli, L.; Armentano, N.; Calà, P.; Galanti, G. Evaluation of physical activity and dietary behaviors in young athletes: A pilot study. Minerva Pediatr. 2017, 69, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Mascherini, G.; Petri, C.; Ermini, E.; Bini, V.; Calà, P.; Galanti, G.; Modesti, P.A. Overweight in Young Athletes: New Predictive Model of Overfat Condition. Int. J. Environ. Res. Public Health 2019, 16, 5128. [Google Scholar] [CrossRef] [PubMed]
- Etchison, W.C.; Bloodgood, E.A.; Minton, C.P.; Thompson, N.J.; Collins, M.A.; Hunter, S.C.; Dai, H. Body mass index and percentage of body fat as indicators for obesity in an adolescent athletic population. Sport. Health 2011, 3, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Kalnina, L.; Sauka, M.; Timpka, T.; Dahlström, Ö.; Nylander, E.; Selga, G.; Ligere, R.; Karklina, H.; Priedite, I.S.; Larins, V. Body fat in children and adolescents participating in organized sports: Descriptive epidemiological study of 6048 Latvian athletes. Scand. J. Public Health 2015, 43, 615–622. [Google Scholar] [CrossRef]
- Bailey-Davis, L.; Poulsen, M.N.; Hirsch, A.G.; Pollak, J.; Glass, T.A.; Schwartz, B.S. Home Food Rules in Relation to Youth Eating Behaviors, Body Mass Index, Waist Circumference, and Percent Body Fat. J. Adolesc. Health 2017, 60, 270–276. [Google Scholar] [CrossRef]
- Petri, C.; Mascherini, G.; Bini, V.; Anania, G.; Calà, P.; Toncelli, L.; Galanti, G. Integrated total body composition versus Body Mass Index in young athletes. Minerva Pediatr. 2020, 72, 163–169. [Google Scholar] [CrossRef]
- Morimoto, A.; Nishimura, R.; Sano, H.; Matsudaira, T.; Miyashita, Y.; Shirasawa, T.; Koide, S.; Takahashi, E.; Tajima, N. Gender differences in the relationship between percent body fat (%BF) and body mass index (BMI) in Japanese children. Diabetes Res. Clin. Pract. 2007, 78, 123–125. [Google Scholar] [CrossRef]
- Freedman, D.S.; Wang, J.; Maynard, L.M.; Thorton, J.C.; Mei, Z.; Pierson, R.N.; Dietz, W.H.; Horlick, M. Relation of BMI to fat and fat-free mass amoung children and adolescents. Int. J. Obes. 2005, 29, 1–8. [Google Scholar] [CrossRef]
- Lee, K.; Lee, S.; Kim, S.Y.; Kim, S.J.; Kim, Y.J. Percent body fat cutoff values for classifying overweight and obesity recommended by the International Obesity Task Force (IOTF) in Korean children. Asia Pac. J. Clin. Nutr. 2007, 16, 649–655. [Google Scholar]
- Sardinha, L.B.; Going, S.B.; Teixeira, P.J.; Lohman, T.G. Receiver Operating Characteristic Analysis of Body Mass Index, Triceps Skinfold Thickness, and Arm Girth for Obesity Screening in Children and Adolescents. Am. J. Clin. Nutr. 1999, 70, 1090–1095. [Google Scholar] [CrossRef]
- Alves Junior, C.A.; Mocellin, M.C.; Gonçalves, E.C.A.; Silva, D.A.; Trindade, E.B. Anthropometric Indicators as Body Fat Discriminators in Children and Adolescents: A Systematic Review and Meta-Analysis. Adv. Nutr. 2017, 8, 718–727. [Google Scholar] [CrossRef] [PubMed]
- Casolo, A.; Sagelv, E.H.; Bianco, M.; Casolo, F.; Galvani, C. Effects of a structured recess intervention on physical activity levels, cardiorespiratory fitness, and anthropometric characteristics in primary school children. J. Phys. Educ. Sport 2019, 19, 1796–1805. [Google Scholar]
- Granacher, U.; Borde, R. Effects of Sport-Specific Training during the Early Stages of Long-Term Athlete Development on Physical Fitness, Body Composition, Cognitive, and Academic Performances. Front. Physiol. 2017, 8, 810. [Google Scholar] [CrossRef] [PubMed]



| Measurement Session | Average Age (Years) | Fat Mass % (kg) | p | ESs | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Total | GC | SC | ||||||||||||||
| Mean | Median | Min. | Max. | SD | 95% CI | Mean | Median | Min. | Max. | SD | 95% CI | |||||
| Average | ||||||||||||||||
| I | 10.27 | 19.77 ** (8.10) | 20.25 (8.44) | 18.10 (6.09) | 8.30 (1.80) | 47.40 (40.60) | 7.90 | 7.02–9.03 | 19.30 (7.76) | 18.20 (6.45) | 6.50 (1.70) | 37.30 (21.10) | 7.39 | 6.51–8.38 | 0.390 | 0.300 |
| II | 10.90 | 19.04 (8.28) | 19.79 (8.86) | 18.00 (7.30) | 5.70 (1.60) | 46.50 (41.80) | 8.09 | 7.19–9.25 | 18.30 (7.70) | 16.90 (6.35) | 6.40 (1.70) | 38.00 (21.90) | 7.15 | 6.35–8.18 | 0.170 | 0.900 |
| III | 11.27 | 19.55 (8.93) | 20.41 (9.62) | 18.60 (7.80) | 6.50 (1.60) | 49.00 (45.40) | 8.13 | 7.22–9.29 | 18.69 (8.24) | 17.05 (7.10) | 3.00 (1.30) | 39.00 (22.90) | 7.44 | 6.61–8.51 | 0.110 | 0.050 |
| IV | 11.90 | 19.53 (9.66) | 20.15 (10.25) | 19.10 (8.50) | 7.50 (2.30) | 45.90 (50.00) | 8.22 | 7.31–9.40 | 18.91 (9.08) | 17.85 (7.40) | 5.70 (1.70) | 38.90 (27.70) | 7.73 | 6.87–8.84 | 0.300 | 0.245 |
| V | 12.26 | 19.96 (10.45) | 20.38 (10.93) | 19.00 (9.40) | 5.90 (2.20) | 48.90 (56.50) | 8.24 | 7.32–9.42 | 19.55 (9.97) | 18.65 (8.20) | 6.00 (1.80) | 39.70 (26.70) | 8.00 | 7.11–9.16 | 0.550 | 0.520 |
| Girls | ||||||||||||||||
| I | 10.27 | 21.77 ** (8.73) | 22.12 (8.71) | 21.90 (8.00) | 8.30 (1.80) | 34.34 (18.10) | 6.76 | 5.71–8.30 | 21.38 (8.76) | 20.50 (7.50) | 6.50 (1.70) | 37.30 (21.10) | 8.16 | 6.93–9.94 | 0.590 | 0.600 |
| II | 10.90 | 21.18 (9.02) | 21.80 (9.26) | 21.30 (8.40) | 6.70 (2.20) | 37.30 (21.20) | 7.25 | 6.12–8.90 | 20.57 (8.79) | 18.70 (7.50) | 6.40 (1.70) | 38.00 (21.90) | 7.75 | 6.58–9.44 | 0.370 | 0.060 |
| III | 11.27 | 21.84 (9.77) | 22.40 (10.00) | 21.50 (8.50) | 6.50 (1.60) | 38.10 (23.20) | 6.94 | 5.86–5.15 | 21.29 (9.54) | 19.90 (8.10) | 5.50 (1.50) | 39.00 (22.90) | 7.76 | 6.45–9.26 | 0.410 | 0.390 |
| IV | 11.90 | 22.39 (10.95) | 22.88 (11.21) | 23.10 (10.00) | 8.30 (2.30) | 39.20 (26.80) | 7.36 | 6.22–9.03 | 21.90 (10.70) | 20.00 (8.90) | 6.50 (1.80) | 38.90 (27.70) | 7.97 | 6.76–9.70 | 0.490 | 0.210 |
| V | 12.26 | 23.18 (12.00) | 23.56 (12.20) | 23.90 (11.00) | 5.90 (2.20) | 39.00 (28.40) | 7.50 | 6.33–9.20 | 22.81 (11.80) | 21.40 (10.00) | 6.00 (1.80) | 39.70 (26.70) | 8.01 | 6.80–9.75 | 0.590 | 0.420 |
| Boys | ||||||||||||||||
| I | 10.27 | 17.80 ** (7.46) | 18.39 (8.17) | 15.70 (5.85) | 8.4 (2.20) | 47.4 (40.60) | 8.44 | 7.20–10.19 | 17.22 (6.76) | 15.50 (5.60) | 9.2 (2.40) | 34.3 (18.60) | 5.70 | 4.86–6.98 | 0.360 | 0.420 |
| 0.42II | 10.90 | 16.91 (7.54) | 17.78 (8.46) | 15.55 (6.00) | 5.7 (1.60) | 46.5 (41.80) | 8.35 | 7.13–10.09 | 16.04 (6.62) | 14.90 (5.50) | 7.9 (2.20) | 36.1 (18.40) | 5.72 | 4.85–6.96 | 0.170 | 0.220 |
| III | 11.27 | 17.26 (8.09) | 18.4 (9.24) | 16.15 (6.90) | 7.2 (2.10) | 49.0 (45.50) | 8.67 | 7.40–10.46 | 16.10 (6.94) | 14.20 (5.20) | 3.0 (1.30) | 33.90 (17.90) | 6.33 | 5.37–7.71 | 0.080 | 0.485 |
| IV | 11.90 | 16.67 (8.38) | 17.42 (9.30) | 16.20 (7.40) | 7.5 (2.00) | 45.9 (50.00) | 8.14 | 6.95–9.82 | 15.92 (7.47) | 14.90 (6.00) | 5.7 (1.70) | 32.00 (19.20) | 6.23 | 5.28–7.58 | 0.240 | 0.256 |
| V | 12.26 | 16.74 (8.90) | 17.21 (9.67) | 16.40 (7.75) | 6.7 (2.20) | 48.9 (56.50) | 7.75 | 6.62–9.36 | 16.28 (8.14) | 14.40 (6.40) | 6.1 (1.90) | 33.40 (23.90) | 6.59 | 5.59–8.02 | 0.470 | 0.450 |
| Fat Mass Category | Measurement Session | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||||||||||||||||
| Average Age | ||||||||||||||||||||
| 10.27 | 10.90 | 11.27 | 11.90 | 12.26 | ||||||||||||||||
| The Type of the Class | ||||||||||||||||||||
| GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | |
| Underweight | 10.28 | 11.22 | 0.096 | 0.756 | 5.95 | 10.11 | 0.622 | 0.432 | 6.66 | 7.85 | 0.367 | 0.546 | 4.80 | 6.17 | 0.505 | 0.479 | 4.04 | 2.75 | 4.413 | 0.039 |
| Healthy weight | 61.61 | 59.86 | 0.003 | 0.953 | 61.75 | 64.02 | 0.071 | 0.789 | 60.66 | 68.07 | 1.017 | 0.314 | 60.40 | 71.76 | 0.026 | 0.870 | 56.29 | 76.25 | 7.270 | 0.047 |
| Overweight | 16.50 | 18.67 | 0.764 | 0.390 | 20.78 | 13.96 | 3.031 | 0.020 | 21.04 | 15.23 | 0.111 | 0.741 | 22.75 | 13.87 | 0.182 | 0.672 | 26.65 | 14.53 | 5.248 | 0.017 |
| Obesity | 11.61 | 10.25 | 0.731 | 0.400 | 11.52 | 11.91 | 0.028 | 0.867 | 11.64 | 8.85 | 0.785 | 0.386 | 12.05 | 8.40 | 0.282 | 0.601 | 13.02 | 6.47 | 3.395 | 0.026 |
| Variables | Measurement Session | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||||||||||||||||
| Average age (years) | 10.27 | 10.90 | 11.27 | 11.90 | 12.26 | |||||||||||||||
| Class type | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p |
| Underweight | 9.58 | 11.45 | 0.708 | 0.078 | 6.02 | 11.45 | 0.001 | 0.990 | 6.78 | 8.45 | 0.114 | 0.738 | 4.55 | 6.87 | 0.038 | 0.846 | 3.52 | 3.05 | 0.080 | 0.090 |
| Healthy weight | 61.62 | 57.05 | 0.268 | 0.606 | 62.23 | 59.11 | 0.472 | 0.494 | 59.19 | 66.43 | 1.976 | 0.164 | 59.72 | 70.04 | 0.024 | 0.876 | 53.71 | 75.59 | 3.025 | 0.033 |
| Overweight | 18.45 | 19.45 | 0.010 | 0.249 | 20.50 | 15.87 | 0.212 | 0.651 | 22.53 | 15.87 | 6.180 | 0.020 | 23.15 | 14.74 | 0.250 | 0.155 | 29.25 | 14.47 | 2.031 | 0.031 |
| Obesity | 10.35 | 12.05 | 0.060 | 0.2139 | 11.25 | 13.57 | 0.377 | 0.552 | 11.50 | 9.25 | 0.382 | 0.553 | 12.58 | 8.35 | 3.159 | 0.028 | 13.52 | 6.89 | 3.014 | 0.025 |
| Variables | Measurement Session | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | ||||||||||||||||
| Average age (years) | 10.27 | 10.90 | 11.27 | 11.90 | 12.26 | |||||||||||||||
| Class type | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p | GC | SC | F | p |
| Underweight | 10.98 | 11.00 | 0.277 | 0.104 | 5.89 | 8.78 | 0.936 | 0.338 | 6.55 | 7.25 | 0.002 | 0.980 | 5.05 | 5.47 | 0.665 | 0.110 | 4.55 | 2.45 | 0.313 | 0.578 |
| Healthy weight | 61.60 | 62.66 | 0.487 | 0.489 | 61.28 | 68.92 | 0.181 | 0.671 | 62.12 | 69.71 | 0.115 | 0.734 | 61.08 | 73.08 | 0.316 | 0.576 | 58.88 | 76.91 | 5.232 | 0.031 |
| Overweight | 14.55 | 17.89 | 0.003 | 0.984 | 21.05 | 12.05 | 0.042 | 0.839 | 19.55 | 14.59 | 0.002 | 0.960 | 22.35 | 13.00 | 3.145 | 0.23 | 24.05 | 14.59 | 0.261 | 0.616 |
| Obesity | 12.87 | 8.45 | 2.004 | 0.025 | 11.78 | 10.25 | 0.051 | 0.826 | 11.78 | 8.45 | 1.987 | 0.192 | 11.52 | 8.45 | 0.208 | 0.308 | 12.52 | 6.05 | 3.929 | 0.067 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ługowska, K.; Kolanowski, W. The Impact of Physical Activity at School on Body Fat Content in School-Aged Children. Int. J. Environ. Res. Public Health 2022, 19, 12514. https://doi.org/10.3390/ijerph191912514
Ługowska K, Kolanowski W. The Impact of Physical Activity at School on Body Fat Content in School-Aged Children. International Journal of Environmental Research and Public Health. 2022; 19(19):12514. https://doi.org/10.3390/ijerph191912514
Chicago/Turabian StyleŁugowska, Katarzyna, and Wojciech Kolanowski. 2022. "The Impact of Physical Activity at School on Body Fat Content in School-Aged Children" International Journal of Environmental Research and Public Health 19, no. 19: 12514. https://doi.org/10.3390/ijerph191912514
APA StyleŁugowska, K., & Kolanowski, W. (2022). The Impact of Physical Activity at School on Body Fat Content in School-Aged Children. International Journal of Environmental Research and Public Health, 19(19), 12514. https://doi.org/10.3390/ijerph191912514







