Accessibility in People with Disabilities in Primary Healthcare Centers: A Dimension of the Quality of Care
Abstract
:1. Introduction
National and International Universal Accessibility Regulations
2. Materials and Methods
2.1. Data Collection
2.2. Analysis Methods
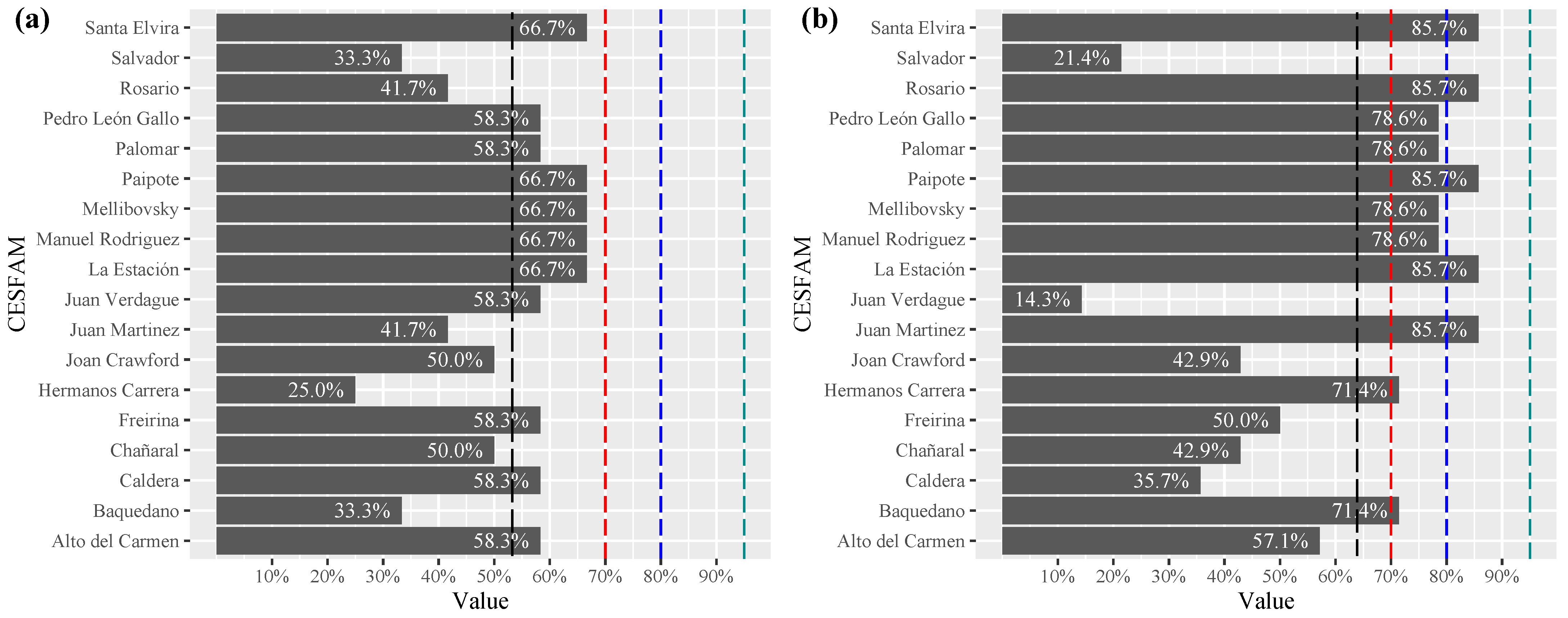
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CESFAM | Family Healthcare Center |
| DALCO | Ambulation, Apprehension, Location and Communication |
| LCL | Lower Control Limit |
| MAIS | Comprehensive Health Care Model |
| PHC | Primary Healthcare |
| SOME | Medical and Statistic Orientation Service |
| UN | United Nations |
| WHO | World Health Organization |
References
- Servicio Nacional de la Discapacidad. II Estudio Nacional de la Discapacidad 2015. 2015. Available online: https://www.senadis.gob.cl/pag/355/1197/ii_estudio_nacional_de_discapacidad (accessed on 17 June 2022).
- Groce, N.; Kett, M.; Lang, R.; Trani, J.F. Disability and Poverty: The need for a more nuanced understanding of implications for development policy and practice. Third World Q. 2011, 32, 1493–1513. [Google Scholar] [CrossRef]
- Mitra, S.; Posarac, A.; Vick, B. Disability and Poverty in Developing Countries: A Multidimensional Study. World Dev. 2013, 41, 1–18. [Google Scholar] [CrossRef]
- Mitra, S.; Sambamoorthi, U. Disability prevalence among adults: Estimates for 54 countries and progress toward a global estimate. Disabil. Rehabil. 2014, 36, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Organización Mundial de la Salud. Discapacidad: Proyecto de Acción Mundial de la OMS Sobre Discapacidad 2014–2021: Mejor Salud para Todas Las Personas Con Discapacidad: Informe de la Secretaría; Technical Report 16; Organización Mundial de la Salud: Ginebra, Switzerland, 2014; Available online: https://apps.who.int/iris/bitstream/handle/10665/170540/A67_16-sp.pdf?sequence=1&isAllowed=y (accessed on 19 June 2022).
- Haidar, O.M.; Lamarche, P.A.; Levesque, J.F.; Pampalon, R. The Influence of Individuals’ Vulnerabilities and Their Interactions on the Assessment of a Primary Care Experience. Int. J. Health Serv. 2018, 48, 798–819. [Google Scholar] [CrossRef]
- de Oliveira, P.M.P.; Mariano, M.R.; Pagliuca, L.M.F.; da Silva, J.M.; de Almeida, P.C.; Oliveira, G.O.B. Socio-economic profile of people with disabilities: A health impact. Health 2015, 7, 633–638. [Google Scholar] [CrossRef]
- Gupta, I.; Guin, P. Health Status and Access to Health Services in Indian Slums. Health 2015, 7, 245–255. [Google Scholar] [CrossRef]
- Levesque, J.F.; Pineault, R.; Hamel, M.; Roberge, D.; Kapetanakis, C.; Simard, B.; Prud’homme, A. Emerging organisational models of primary healthcare and unmet needs for care: Insights from a population-based survey in Quebec province. BMC Fam. Pract. 2012, 13, 66. [Google Scholar] [CrossRef]
- Davidsson, N.; Södergård, B. Access to Healthcare among People with Physical Disabilities in Rural Louisiana. Soc. Work Public Health 2016, 31, 188–195. [Google Scholar] [CrossRef]
- Kaur Khakh, A.; Fast, V.; Shahid, R. Spatial Accessibility to Primary Healthcare Services by Multimodal Means of Travel: Synthesis and Case Study in the City of Calgary. Int. J. Environ. Res. Public Health 2019, 16, 170. [Google Scholar] [CrossRef]
- World Health Organization. Disability and Health. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/disability-and-health (accessed on 19 June 2022).
- Grabovschi, C.; Loignon, C.; Fortin, M. Mapping the concept of vulnerability related to health care disparities: A scoping review. BMC Health Serv. Res. 2013, 13, 94. [Google Scholar] [CrossRef] [Green Version]
- Freeman, T.; Baum, F.; Lawless, A.; Javanparast, S.; Jolley, G.; Labonté, R.; Bentley, M.; Boffa, J.; Sanders, D. Revisiting the ability of Australian primary healthcare services to respond to health inequity. Aust. J. Prim. Health 2016, 22, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Brolan, C.E.; Ware, R.S.; Lennox, N.G.; Gomez, M.T.; Kay, M.; Hill, P.S. Invisible populations: Parallels between the health of people with intellectual disability and people of a refugee background. Aust. J. Prim. Health 2011, 17, 210–213. [Google Scholar] [CrossRef] [PubMed]
- Mremi, I.R.; Mbise, M.; Chaula, J.A. Distribution of primary health care facilities in Mtwara District, Tanzania: Availability and accessibility of services. Tanzan. J. Health Res. 2018, 20, 1–8. [Google Scholar] [CrossRef]
- Ragoasha, M.V.; Maritz, J.; Cooper, A.K. Geospatial accessibility analysis of primary health care clinics in the Mbizana local municipality in the Eastern Cape. In Proceedings of the AfricaGEO 2018, Ekuhurleni, South Africa, 17–19 September 2018; Research Space: Pretoria, South Africa, 2021; pp. 52–65. Available online: http://hdl.handle.net/10204/10597 (accessed on 11 June 2022).
- Báscolo, E.; Houghton, N.; Del Riego, A. Types of health systems reforms in latin america and results in health access and coverage. Rev. Panam. Salud Publica/Pan Am. J. Public Health 2018, 42, e126. [Google Scholar] [CrossRef]
- Chapman, A.R. The social determinants of health, health equity, and human rights. Health Hum. Rights 2010, 12, 17. [Google Scholar]
- Richard, L.; Furler, J.; Densley, K.; Haggerty, J.; Russell, G.; Levesque, J.F.; Gunn, J. Equity of access to primary healthcare for vulnerable populations: The IMPACT international online survey of innovations. Int. J. Equity Health 2016, 15, 64. [Google Scholar] [CrossRef]
- Khanassov, V.; Pluye, P.; Descoteaux, S.; Haggerty, J.L.; Russell, G.; Gunn, J.; Levesque, J.F. Organizational interventions improving access to community-based primary health care for vulnerable populations: A scoping review. Int. J. Equity Health 2016, 15, 168. [Google Scholar] [CrossRef]
- Esmeraldo Áfio, A.C.; de Carvalho, L.; Marques, J.F.; Pinheiro de Oliveira, P.M.; de Almeida, P.C.; Freitag Pagliuca, L.M. Physical accessibility for disabled people: Analysis of toilet facilities in primary health care units. Open J. Nurs. 2016, 6, 948–957. [Google Scholar] [CrossRef]
- dos Santos Amaral, F.L.J.S.; Alves Motta, M.H.; Pereira Gomes da Silva, L.; Bezerra Alves, S. Fatores associados com a dificuldade no acesso de idosos com deficiência aos serviços de saude. Cienc. e Saude Coletiva 2012, 17, 2991–3001. [Google Scholar] [CrossRef]
- Alvial, X.; Rojas, A.; Carrasco, R.; Duran, C.; Fernandez-Campusano, C. Overuse of Health Care in the Emergency Services in Chile. Int. J. Environ. Res. Public Health 2021, 18, 3082. [Google Scholar] [CrossRef]
- Hirmas Adauy, M.; Angulo Poffald, L.; Jasmen Sepúlveda, A.M.; Aguilera Sanhueza, X.; Delgado Becerra, I.; Vega Morales, J. Barreras y facilitadores de acceso a la atención de salud: Una revisión sistemática cualitativa. Rev. Panam. Salud Publica/Pan Am. J. Public Health 2013, 33, 223–229. Available online: https://iris.paho.org/bitstream/handle/10665.2/9196/a09v33n3.pdf?sequence=1&isAllowed=y (accessed on 11 June 2022). [CrossRef] [PubMed] [Green Version]
- Coss-Mandiola, J.; Vanegas-López, J.; Rojas, A.; Carrasco, R.; Dubo, P.; Campillay-Campillay, M. Characterization of Communes with Quality Accredited Primary Healthcare Centers in Chile. Int. J. Environ. Res. Public Health 2022, 19, 9189. [Google Scholar] [CrossRef] [PubMed]
- Frenk, J. El concepto y la medición de accesibilidad. Salud Publica Mex. 1985, 27, 438–453. [Google Scholar] [PubMed]
- Imrie, R.; Luck, R. Designing inclusive environments: Rehabilitating the body and the relevance of universal design. Disabil. Rehabil. 2014, 36, 1315–1319. [Google Scholar] [CrossRef]
- Díaz de León-Castañeda, C. Revisión de temas fundamentales en sistemas de salud. Rev. Med. Inst. Mex. Seguro Soc. 2018, 56, 295–304. [Google Scholar]
- Mojica, C.M.; Flores, B.; Ketchum, N.S.; Liang, Y. Health Care Access, Utilization, and Cancer Screening Among Low-Income Latina Women. Hisp. Health Care Int. 2017, 15, 160–165. [Google Scholar] [CrossRef]
- Fougeyrollas, P.; Boucher, N.; Edwards, G.; Grenier, Y.; Noreau, L. The disability creation process model: A comprehensive explanation of disabling situations as a guide to developing policy and service programs. Scand. J. Disabil. Res. 2019, 21, 25–37. [Google Scholar] [CrossRef]
- Hailemariam, M.; Fekadu, A.; Selamu, M.; Medhin, G.; Prince, M.; Hanlon, C. Equitable access to integrated primary mental healthcare for people with severe mental disorders in Ethiopia: A formative study. Int. J. Equity Health 2016, 15, 121. [Google Scholar] [CrossRef]
- Brenes, F. Hispanics, Mental Health, and Discriminating Policies: Brief Report. Hisp. Health Care Int. 2019, 17, 178–180. [Google Scholar] [CrossRef]
- Instituto Nacional de Normalización. Norma Chilena NCh3267:2012 Sistemas de Gestión—Gestión de la Inclusión de Personas Con Discapacidad; Instituto Nacional de Normalización: Santiago, Chile, 2012; p. 15. Available online: https://ecommerce.inn.cl/nch3267201245789 (accessed on 24 June 2022).
- Comité Técnico AEN/CTN. UNE 170001-2 Accesibilidad Universal Parte 2: Sistema de Gestión de la Accesibilidad; UNE—Comités Técnicos de Normalización: Madrid, España, 2007; p. 12. Available online: https://www.une.org/encuentra-tu-norma/busca-tu-norma/norma?c=N0040253 (accessed on 24 June 2022).
- Instituto Nacional de Normalización. NCh3267:2021: Sistemas de Gestión—Gestión de la Inclusión de Personas Con Discapacidad; Instituto Nacional de Normalización: Santiago, Chile, 2021; Available online: https://ecommerce.inn.cl/nch3267202178844 (accessed on 24 June 2022).
- Skempes, D.; Bickenbach, J. Developing human rights based indicators to support country monitoring of rehabilitation services and programmes for people with disabilities: A study protocol. BMC Int. Health Hum. Rights 2015, 15, 25. [Google Scholar] [CrossRef]
- Ribeiro, J.P.; Mamed, S.N.; Souza, M.R.; de Souza, M.M.; Rosso, C.F.W. Acessibilidade aos serviços de saúde na Atenção Básica do Estado de Goiás. Rev. Eletrônica Enferm. 2016, 17, 1–11. [Google Scholar] [CrossRef]
- Ministerio de Salud. Orientaciones para la Implementación del Modelo de Atención Integral de Salud Familiar y Comunitaria; Technical Report; Ministerio de Salud, Gobierno de Chile: Santiago, Chile, 2012; Available online: https://www.minsal.cl/portal/url/item/e7b24eef3e5cb5d1e0400101650128e9.pdf (accessed on 21 June 2022).
- Groenewegen, P.P.; Kroneman, M.; Spreeuwenberg, P. Physical accessibility of primary care facilities for people with disabilities: A cross-sectional survey in 31 countries. BMC Health Serv. Res. 2021, 21, 107. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Normalización. NCh3271:2012 Criterios DALCO para Facilitar la Accesibilidad Universal; Instituto Nacional de Normalización: Santiago, Chile, 2012; p. 19. Available online: https://ecommerce.inn.cl/nch3271201245788 (accessed on 20 June 2022).
- Conrado Peranovich, A. Capacidades y retos del monitoreo sobre la disponibilidad y el acceso a los servicios de salud en Argentina. Salud Colect. 2017, 13, 73–90. [Google Scholar] [CrossRef]
- McColl, M.A.H.; Shortt, S.; Hunter, D.; Dorland, J.; Godwin, M.; Rosser, W.; Shaw, R. Access and Quality of Primary Care for People With Disabilities: A Comparison of Practice Factors. J. Disabil. Policy Stud. 2010, 21, 131–140. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ Br. Med. J. 2014, 348, g1687. [Google Scholar] [CrossRef]
- Johannesen, D.T.S.; Wiig, S. Why adopt ISO 9001 certification in hospitals? A case study of external triggers and sensemaking in an emergency department in Norway. Saf. Health 2017, 3, 7. [Google Scholar] [CrossRef]
- Araujo, M. Indicadores de Calidad: Criterios Para la Definición de Umbrales; Monografías de Apoyo a la Acreditación; Gobierno de Chile, Superintendencia de Salud: Santiago, Chile, 2010; Volume 2, p. 32. Available online: https://www.supersalud.gob.cl/observatorio/671/articles-6697_recurso_1.pdf (accessed on 24 June 2022).
- Li, Z.; Cui, Y.; Li, L.; Chen, R.; Dong, L.; Du, J. Hierarchical Amplitude-Aware Permutation Entropy-Based Fault Feature Extraction Method for Rolling Bearings. Entropy 2022, 24, 310. [Google Scholar] [CrossRef]
- Son, W.J.; Cho, I.S. Analysis of Trends in Mega-Sized Container Ships Using the K-Means Clustering Algorithm. Appl. Sci. 2022, 12, 2115. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2022; Available online: https://www.r-project.org/ (accessed on 27 May 2022).
- Instituto Nacional de Estadísticas. Resultados Censo 2017: Por País, Regiones y Comunas: Región de Atacama. Online. 2018. Available online: http://resultados.censo2017.cl/Region?R=R03 (accessed on 3 July 2022).
- Adugna, M.B.; Nabbouh, F.; Shehata, S.; Ghahari, S. Barriers and facilitators to healthcare access for children with disabilities in low and middle income sub-Saharan African countries: A scoping review. BMC Health Serv. Res. 2020, 20, 15. [Google Scholar] [CrossRef]
- Monteiro Cruz, D.; Sousa do Nascimento, L.R.; Guerreiro Vieira da Silva, D.M.; Dornelles Schoeller, S. Redes de apoio à pessoa com deficiência física. Cienc. y enfermería 2015, 21, 23–33. [Google Scholar] [CrossRef]
- Moscoso-Porras, M.; Fuhs, A.K.; Carbone, A. Access barriers to medical facilities for people with physical disabilities: The case of Peru. Cad. Saude Publica 2019, 35, e00050417. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Planificación. Ley 20422 Establece Normas Sobre Igualdad de Oportunidades e Inclusión Social de Personas Con Discapacidad. Online. 2010. Available online: https://www.bcn.cl/leychile/navegar?idNorma=1010903&idParte= (accessed on 8 July 2022).
- Meynell, L. Aimi Hamraie Building Access: Universal Design and the Politics of Disability. Genealogy 2019, 3, 8. [Google Scholar] [CrossRef] [Green Version]
- Boudeguer Simonetti, A.; Prett Weber, P.; Squella Fernández, P. Guía de Consulta Accesibilidad Universal: Ciudades y Espacios para Todos; Corporación Ciudad Accesible: Santiago, Chile, 2014; p. 223. Available online: https://www.ciudadaccesible.cl/wp-content/uploads/2011/08/Gu%C3%ADa-de-Accesibilidad-Universal-2014.pdf (accessed on 21 June 2022).
- Naciones Unidas. Convención Sobre los Derechos de las Personas con Discapacidad: Observaciones Finales Sobre el Informe Inicial de Chile. Technical Report; Convención Sobre Los Derechos de Las Personas Con Discapacidad, Naciones Unidas. 2016. Available online: http://docstore.ohchr.org/SelfServices/FilesHandler.ashx?enc=6QkG1d%2FPPRiCAqhKb7yhsrBkvDLHrFFq8wSOe2z9g3hjZkwUlxbU0X83VfBDhw8%2BVIBUwQlwe77CxKPsxbMrbaqhMlNJx6jkeDn%2FvtIhzABOlVvYiEc5aE2OnG9z1MjRSvcKHuFAYwTRb1EmYoD5LA%3D%3D (accessed on 20 June 2022).
- Titus, S.K.; Kataoka-Yahiro, M. A Systematic Review of Barriers to Access-to-Care in Hispanics with Type 2 Diabetes. J. Transcult. Nurs. 2018, 30, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Relaciones Exteriores. Decreto 201 Promulga la Convención de Las Naciones Unidas Sobre Los Derechos de Las Personas Con Discapacidad y su Protocolo Facultativo. 2008. Available online: https://vlex.cl/vid/promulga-naciones-unidas-facultativo-240339006 (accessed on 8 July 2022).
- Sánchez-Torres, D.A. Accesibilidad a los servicios de salud: Debate teórico sobre determinantes e implicaciones en la política pública de salud. Rev. Med. Inst. Mex. Seguro Soc. 2017, 55, 82–89. Available online: https://www.redalyc.org/articulo.oa?id=457749297021 (accessed on 20 June 2022). [PubMed]
- Rezapour, R.; Tabrizi, J.S.; Farahbakhsh, M.; Saadati, M.; Abdolahi, H.M. Developing Iranian primary health care quality framework: A national study. BMC Public Health 2019, 19, 911. [Google Scholar] [CrossRef]
- Ministerio de Salud; Subsecretaría de Salud Pública. Ley 20584 Regula Los Derechos y Deberes Que Tienen Las Personas en Relación Con Acciones Vinculadas a su Atención en Salud. 2012. Available online: https://www.bcn.cl/leychile/navegar?idNorma=1039348 (accessed on 13 July 2022).
- Skarstad, K. Human rights through the lens of disability. Netherlands Q. Hum. Rights 2018, 36, 24–42. [Google Scholar] [CrossRef]
- Lee, J.E.; Kim, H.R.; Shin, H.I. Accessibility of medical services for persons with disabilities: Comparison with the general population in Korea. Disabil. Rehabil. 2014, 36, 1728–1734. [Google Scholar] [CrossRef]
- Kuenburg, A.; Fellinger, P.; Fellinger, J. Health Care Access Among Deaf People. J. Deaf Stud. Deaf Educ. 2016, 21, 1–10. [Google Scholar] [CrossRef]
- Emond, A.; Ridd, M.; Sutherland, H.; Allsop, L.; Alexander, A.; Kyle, J. Access to primary care affects the health of Deaf people. Br. J. Gen. Pract. 2015, 65, 95–96. [Google Scholar] [CrossRef]
- Withers, J.; Speight, C. Health Care for Individuals with Hearing Loss or Vision Loss. N. C. Med. J. 2017, 78, 107–112. [Google Scholar] [CrossRef]
- Hughes, R.B.; Robinson-Whelen, S.; Knudson, C. Cancer Disparities Experienced by People with Disabilities. Int. J. Environ. Res. Public Health 2022, 19, 9187. [Google Scholar] [CrossRef] [PubMed]
- Malbon, E.; Carey, G.; Meltzer, A. Personalisation schemes in social care: Are they growing social and health inequalities? BMC Public Health 2019, 19, 805. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.; Lowton, K.; Scambler, S. Threats to embodied well-being: An exploration of how disabled people negotiate barriers in hospital settings. Health 2019, 24, 535–551. [Google Scholar] [CrossRef] [PubMed]






| Criteria | Description | Standards |
|---|---|---|
| Participation | People with disabilities and their families are co-responsible for making diagnoses, advising, and proposing improvement measures in the health center, in order to promote universal access for all. | It measures nine criteria: existence of a diagnosis on the situation of universal accessibility in the center, participation in a consultative or decision-making council for people with disabilities, priority on waiting lists, monitoring of access barriers, participation in the regional disability table, design of duties and rights letter adapted to people with disabilities, system of claims, suggestions and congratulations adapted to people with disabilities, and existence of a facilitator for communication with deaf people, among others. |
| Information | Creation of systems that facilitate access to communication for people with disabilities, especially those with sensory or cognitive difficulties. | It measures seven criteria; the available information is in Chilean sign language, Braille, and in various formats such as written, video and audio, and also considers the training of staff to communicate assertively with people with disabilities. |
| Access Chain | First contact: Access to the primary health center through public transport. | It measures in four criteria, travel times, existence of universal public transport, accessible whereabouts, inventory of routes to reach the health center, existence of ramps and their characteristics. |
| Second contact: Infrastructure that facilitates and ensures the free movement of the people with disabilities. The wheelchair is taken as a reference, under the idea that if a wheelchair circulates in a space, anyone with another technical aid can access it. | It measures on 6 criteria and 13 sub-criteria; exclusive parking for people with disabilities, ramps, handrails, access doors and access areas, floors, among others. | |
| Third contact: Until you reach the place destined for customer service, accessibility chain. | It measures on five criteria and seven sub-criteria; shift height, universal public guidance service, corridors, circulation areas and waiting rooms, among others. | |
| Architectural Aspects | Implementation of universal design in the rest of the dependencies of the health center. | It measures in 3 criteria and 14 sub criteria; universal bathroom, door handles, floors, corridors, stairs, signage, among others. |
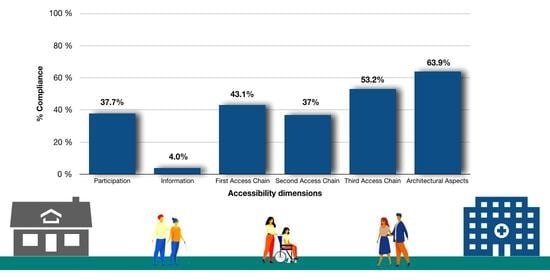
| N° | Accessibility Dimensions | % Compliance |
|---|---|---|
| 1 | Participation | 37.7 |
| 2 | Information | 4.0 |
| 3 | First Access Chain | 43.1 |
| 4 | Second Access Chain | 37.0 |
| 5 | Third Access Chain | 53.2 |
| 6 | Architectural Aspects | 63.9 |
| Average fulfillment of all accessibility dimensions | 39.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Campillay-Campillay, M.; Calle-Carrasco, A.; Dubo, P.; Moraga-Rodríguez, J.; Coss-Mandiola, J.; Vanegas-López, J.; Rojas, A.; Carrasco, R. Accessibility in People with Disabilities in Primary Healthcare Centers: A Dimension of the Quality of Care. Int. J. Environ. Res. Public Health 2022, 19, 12439. https://doi.org/10.3390/ijerph191912439
Campillay-Campillay M, Calle-Carrasco A, Dubo P, Moraga-Rodríguez J, Coss-Mandiola J, Vanegas-López J, Rojas A, Carrasco R. Accessibility in People with Disabilities in Primary Healthcare Centers: A Dimension of the Quality of Care. International Journal of Environmental Research and Public Health. 2022; 19(19):12439. https://doi.org/10.3390/ijerph191912439
Chicago/Turabian StyleCampillay-Campillay, Maggie, Ana Calle-Carrasco, Pablo Dubo, Jorge Moraga-Rodríguez, Juan Coss-Mandiola, Jairo Vanegas-López, Alejandra Rojas, and Raúl Carrasco. 2022. "Accessibility in People with Disabilities in Primary Healthcare Centers: A Dimension of the Quality of Care" International Journal of Environmental Research and Public Health 19, no. 19: 12439. https://doi.org/10.3390/ijerph191912439
APA StyleCampillay-Campillay, M., Calle-Carrasco, A., Dubo, P., Moraga-Rodríguez, J., Coss-Mandiola, J., Vanegas-López, J., Rojas, A., & Carrasco, R. (2022). Accessibility in People with Disabilities in Primary Healthcare Centers: A Dimension of the Quality of Care. International Journal of Environmental Research and Public Health, 19(19), 12439. https://doi.org/10.3390/ijerph191912439