Abstract
Background: There is conflicting evidence with respect to whether early opioid prescribing (EOP) within the first two weeks of acute Low Back Pain (LBP) onset is associated with the length of disability (LOD). The aim of this systematic review was to examine the relationship between EOP and LOD in individuals with acute LBP. Methods: A systematic search of Medline, EMBASE, and CINAHL was conducted. The Newcastle–Ottawa scale was used to assess the methodological quality of included studies. A narrative synthesis of findings was used owing to between-study heterogeneity. Results: Six cohort studies using workers’ compensation administrative data on 178,130 adults with LBP were included. Most studies were of good methodological quality. One study reported that LBP cases with EOP had higher LOD by 4 days than cases without EOP. Two studies reported that each 100 mg morphine equivalent amount (MEA) was associated with an increase in mean LOD by 0.4 day (95% confidence interval (CI): 0.3, 0.5) and 0.4 day (95% CI: 0.3, 0.4). One study showed that LBP cases with EOP had a higher hazard of continuation of time loss benefits by 1.94 (95% CI 1.86, 2.02). One study reported a dose–response relationship between MEA of EOP and LOD ranging between 5.2 days (95% CI 14.6, 25.0) for 1–140 mg MEA and 69.1 (95% CI 49.3, 89.0) for 450+ mg MEA. One study reported that LBP cases with EOP had a higher mean LOD by 3.8 days, but there was no statistically significant relationship between EOP and LOD (Hazard ratio 1.02; 95% CI 0.91, 1.13). Conclusions: The use of early opioid in the management of acute uncomplicated LBP is associated with prolonged disability duration. Further research on factors influencing inadequate adherence to evidence-based guidelines and optimal strategies to modify such factors may improve disability outcomes among patients presenting with acute LBP.
Keywords:
opioids; opiates; low back pain; return to work; sick leave; length of disability; systematic review 1. Introduction
Lower back pain (LBP) is a global public health problem. Most people of all age groups experience at least one episode of LBP during their lifetime [1,2]. In 2019, the global age-standardized point prevalence and incidence of LBP were 7% (95% confidence interval (CI) 6.2, 7.9) and 2.7% (95% CI 2.4, 3.1), respectively [3]. In the Global Burden of Disease study conducted in 2019, LBP was the third leading cause of years lived with disabilities (YLDs), accounting for 7.4% (95% CI 6.2, 8.7) of the global YLDs [4]. Most acute episodes of LBP recover spontaneously within a few weeks, but about one-third and one-quarter of people with LBP experience recurrent and chronic LBP, respectively [5,6]. Persistent LBP is associated with adverse long-term outcomes on the individual (e.g., depression, anxiety, sleep disorders, job dissatisfaction, prolonged length of disability, and negative body image) [7,8] and results in very high costs to the healthcare system associated with medical care and work disability [3,9,10,11].
Several factors were found to be associated with persistent and disabling LBP, including LBP-related factors (previous episodes of LBP, LBP intensity, and presence of leg pain), lifestyle factors (obesity, smoking, and low levels of physical activity), psychological factors (depression, catastrophizing, and fear avoidance beliefs), and occupational and socioeconomic factors (physical workloads, low education level, workers’ compensation (WC) policies, and dissatisfaction with work) [1,12,13,14,15]. In addition, healthcare factors such as early MRI scanning within four weeks of LBP onset and, of particular interest, early opioid prescribing (EOP) within two weeks of LBP onset were identified as strong predictors of an increased length of disability (LOD) [16,17]. In addition, visceral referred pain, which is a vague pain originating from visceral organs that is felt at another body location, is a commonly overlooked cause of musculoskeletal pain [18,19]. It can be explained, at least in part, by the sensitization of peripheral nerves that occurs in acute and chronic systemic inflammatory processes [20]. For example, gastrointestinal complaints, such as diarrhea, were found to be associated with LBP [21,22].
EOP within the first two weeks of LBP onset may be crucial in enabling individuals with acute LBP an earlier return to daily activities. However, adverse side effects such as drowsiness, cognitive impairment [23], addiction, and overdosing may place the individual at risk and delay recovery [24,25]. Clinical guidelines emphasize the avoidance of opioids in the management of acute LBP, with a focus on reassurance, staying active, and the use of non-steroidal anti-inflammatory drugs and acetaminophen if needed, with opioids reserved only for severe and unresponsive cases and only for several days [26,27,28]. Despite these recommendations, around 60% and 28% of cases presenting with LBP in ED and primary care are prescribed EOP, respectively [15,29]. EOP in acute LBP is associated with an increased LOD at two years of follow-up [17], a higher risk for surgery [17,30], and increased healthcare utilization (e.g., physiotherapy, imaging, hospital admission, and surgery) [30,31]. However, one study by Lee and colleagues demonstrated conflicting findings in which no statistically significant association was found between EOP and LOD in acute LBP [30]. To clarify and consolidate these conflicting findings, this study aims to undertake a systematic approach to review the literature, investigating the relationship between EOP and LOD in individuals with acute uncomplicated LBP.
2. Materials and Methods
The protocol for this review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42021260723 (available from: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=260723, accessed on the 26 August 2022).
2.1. Search Strategy
The report of this systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [32]. A comprehensive search utilizing Medline, EMBASE, and CINAHL databases from their inception until 14 March 2022 was conducted. Controlled vocabularies and free-text terms on opioids, LBP, and work disability were used (Supplemental File S1). In addition, experts in the field were contacted, reference lists of all relevant papers were screened, and citations of included papers were traced using the Web of Science Citation Index. No restrictions on the language of publication or study design were applied.
2.2. Criteria for Considering Studies for the Review
2.2.1. Inclusion Criteria
All epidemiologic study designs examining the association between EOP and LOD in adults presenting with acute uncomplicated LBP were considered for inclusion. EOP was defined as prescribing opioid medications for LBP within the first 15 days of seeking medical treatment for acute LBP [17]. Therefore, studies including adults (aged 18 years and older) presenting with an acute, occupational, or non-specific LBP were eligible for inclusion. The outcome measure was the measure of association between EOP and LOD defined as the number of work disability days (absence from work) due to the current episode of LBP [14,33].
2.2.2. Exclusion Criteria
Studies were excluded if they included patients with chronic or complicated LBP, such as multiple and severe injuries, infection, cancer, or autoimmune disease.
2.3. Study Selection Process
All identified papers were independently reviewed by two reviewers and any disagreements were resolved by a third independent adjudicator. Retrieved records were imported to the Covidence web-based application, and duplicates were deleted. In the first stage, titles and abstracts of the remaining studies were screened against the inclusion and exclusion criteria, and irrelevant studies were excluded. In the second stage, full-texts of all potentially relevant studies, or when a decision could not be made based on the titles and abstracts, were retrieved and reviewed against the inclusion and exclusion criteria. Reasons for study exclusions at the full-text review stage are reported in the PRISMA flow diagram (Figure 1). The study selection process was performed independently by two reviewers, and any disagreements were resolved through consensus-based discussion or by involving a third reviewer.
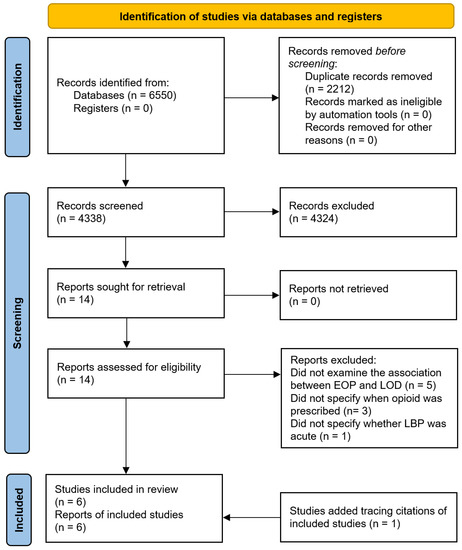
Figure 1.
The PRISMA flow diagram of studies in the review.
2.4. Quality Assessment
A quality assessment of included studies was conducted independently by two reviewers using the Newcastle–Ottawa scale (NOS) for cohort studies (Supplemental File S2) [34], and any disagreements were resolved by discussion or involving a third reviewer until a consensus was achieved. This tool assesses the quality of cohort studies using a “star system” for three main perspectives including selection of study cohorts, comparability of study cohorts, and the ascertainment of the outcome of interest. Each study can be given a maximum of eight 8 stars (4 stars for the process of cohorts’ selection, 2 stars for the comparability of the study cohorts, and 3 stars for ascertainment of the outcome). To summarize the methodological quality for each included study, the NOS was converted to one of the following methodological quality criteria recommended by the Agency for Healthcare Research and Quality: (a) good methodological quality (3 or 4 stars for selection of cohorts, 1 or 2 stars for comparability of cohorts, and 2 or 3 stars for ascertainment of the outcome); (b) fair methodological quality (2 stars for selection of cohorts, 1 or 2 stars for comparability of cohorts, and 2 or 3 stars ascertainment of the outcome); (c) poor methodological quality (0 or for selection of cohorts, 0 stars for comparability of cohorts, or 0 or 1 stars ascertainment of the outcome) [35].
2.5. Data Extraction
Data on the following items were extracted from each included study: aim, design, setting, source of data, study population, sample size, inclusion and exclusion criteria, follow-up duration, independent variables controlled for in multivariable analysis, and summary measures of association between EOP and LOD with corresponding CI. All necessary data were available in all included studies. Therefore, no authors were contacted. Two reviewers extracted the data from included studies independently, and disagreements were addressed by discussion or involvement of a third reviewer. One of the current review authors (MS) co-authored two of the included studies. Therefore, to avoid any potential reviewer bias, MS was not involved in data extraction or the risk of bias assessment for those two studies.
2.6. Data Analysis
We considered performing a meta-analysis. However, this was not feasible due to heterogeneity between included studies in measures of association between EOP and LOD. Therefore, a narrative synthesis was used.
3. Results
3.1. Study Selection
This systematic review search identified 6550 records. Of these, 2212 duplicates were removed, and 4324 records were excluded based on screening of titles and abstracts. After the full-text evaluation of the remaining 14 studies, nine studies did not meet the inclusion criteria and were excluded. Furthermore, one study was identified by tracing citations of included papers. A total of six studies were included in this systematic review. A flow diagram of the literature search and study selection process is shown in Figure 1.
3.2. Study Characteristics
Table 1 presents the characteristics of included studies. All included studies collected data from WC administrative databases and used a retrospective cohort design. Five studies were performed in the United States (US) [15,17,30,36,37], and one was performed in Canada [38]. Two of the included papers used the same sample to explore the association between various individual-level (including EOP), neighborhood, and state-level variables and LOD in patients with LBP [15,37]. However, each of the two studies addressed a different objective meeting the inclusion criteria of this review. The total number of individuals with LBP was 178,130 with a sample size ranging between 2887 and 59,656. The mean age of participants ranged from 37 to 41 years. All studies included more men than women with proportions ranging between 62% and 72% (Table 1). The studies involved cases with acute uncomplicated LBP that were identified using the International Classification of Diseases, Ninth Revision (ICD-9) codes [15,17,30,36,37], or the nature of injury and body part codes [38]. EOP was described as an opioid prescription within two days of the initial ED visit [30], a week of the first medical visit [36], or the first 15 days of the injury or filing a WC claim [15,17,37,38]. The LOD was described as the number of days lost from work estimated based on temporary total and temporary partial wage replacement payments truncated at one year [15,30,36,37,38] or two years [17].

Table 1.
Characteristics of included studies.
3.3. Quality Assessment
Five studies demonstrated good methodological quality [15,17,30,37,38] and the remaining study [36] was of poor quality [36] (Table 2). Four studies scored 9 starts on the NOS in terms of selection, comparability, and outcome [15,17,30,37]. One study scored 8 out of 9 stars for not adjusting for LBP severity [38]. One study scored 7 out of 9 stars, with no stars given for the comparability domain for reporting only descriptive statistics describing the relationship between EOP and LOD [36].

Table 2.
Quality assessment of studies using the Newcastle–Ottawa scale.
3.4. The Association between EOP and LOD
All included studies aimed to investigate the association between EOP and LOD. Five studies used multivariable analyses while consistently adjusting for age and gender as potential confounders, whereas one study did not report adjusted analysis (Table 3). The follow-up period for all studies was one year except for one study, which had a follow-up duration of two years [17].

Table 3.
The relationship between EOP and length of disability.
One study showed that LBP cases who were prescribed opioids within the first week of the first medical visit had a higher median LOD by four days than those who were not prescribed opioids at one year of follow-up [36]. Two studies reported that each 100 mg morphine equivalent amount (MEA) prescribed within the first two weeks of LBP onset was associated with an increase in the adjusted geometric mean of LOD by 0.4 day (95% CI: 0.3, 0.5) [37] and 0.4 day (95% CI: 0.3, 0.4) at one year of follow-up [15]. One study showed that cases who were prescribed opioids within the first two weeks of LBP onset had a higher hazard of continuation of time loss benefits by 1.94 (95% CI 1.86, 2.02) than cases who did not receive EOP at one year of follow-up [38]. One study reported that, compared to cases who were not prescribed opioids within the first two weeks of LBP onset, cases who received EOP had increased mean LOD days with an increasing MEA in a linear dose–response relationship over two years of follow-up: 5.2 days (95% CI −14.6, 25.0) for 1–140 mg MEA, 21.9 days (95% CI 3.2, 40.6) for 141–225 mg MEA, 43.8 days (95% CI 23.7, 63.9) for 226–450 mg MEA, and 69.1 (95% CI 49.3, 89.0) for 450+ mg MEA [17]. The last study reported that LBP cases who received opioid prescriptions within 2 days of the initial ED visit had a higher mean LOD by 3.8 days than those who were not prescribed opioids, but no statistically significant relationship was observed between EOP and LOD at one year of follow-up (hazard ratio 1.02; 95% CI: 0.91, 1.13) [30].
4. Discussion
This is the first study to systematically review the relationship between EOP in the first two weeks of LBP onset and the LOD in patients with acute uncomplicated LBP. Six studies with a total of 178,130 LBP cases were included in this review. The mean age of the participants was approximately 40 years with the majority being males (~70%). The samples included in the studies were representative of their respective population as they were collected from WC administrative data from the state of California [36], the entire US [15,17,30,37], and the WC Board of Alberta, Canada, which covers the majority of injured workers in that province [38].
Overall, the six studies showed that LBP cases prescribed early opioids had increased LOD duration than cases who were not prescribed early opioids at one and two years of follow-up. Only five studies presented adjusted associations between EOP and LOD [15,17,30,37,38]. Of these five studies, four studies found statistically significant associations between EOP and LOD [15,17,37,38], with one study showing a dose–response relationship between MEA and LOD duration at two years of follow-up [17]. The study by Lee and colleagues reported an increased mean LOD among LBP cases prescribed with opioid prescriptions within 2 days of the initial ED visit by 3.8 days than LBP cases who were not prescribed opioids, but the relationship between EOP and LOD was not statically significant [30]. This contradictory finding could be explained by the differences in the definition of EOP in the included studies. Lee and colleagues define EOP as opioid use within two days of the initial visit to ED, while other studies include EOP within one week [36] or two weeks of acute LBP onset [15,17,37,38].
The exact causal mechanisms explaining the relationship between EOP and LOD in acute uncomplicated LBP are not clear. Previous studies showed that EOP for acute LBP was associated with subsequent opioid dose escalation and prolonged opioid use [17,30,39] and increased healthcare utilization, including surgery [17]. Therefore, increased LOD and delayed returns to work among LBP receiving opioids could be explained by adverse side effects associated with opioids, such as drowsiness, cognitive impairment, mood disorders, falls, fractures, and other injuries including road traffic accidents [23,40,41].
The present review showed that EOP is associated with increased LOD among patients presenting with acute LBP, which supports clinical guidelines discouraging the routine use of opioids in the management of acute LBP [26,27,28]. More research is needed to identify factors influencing non-evidence-based EOP for acute LBP cases, including patient, clinician, and contextual factors. Such information may shed light on optimal strategies for bridging the gap between evidence and practice relating to EOP for LBP.
Strengths and Limitations
The present study used a comprehensive search strategy covering relevant bibliographic databases. In addition, included studies had large longitudinal samples of LBP cases extracted from WC administrative databases capturing detailed information on medical diagnoses, medical care, and wage replacement for work disability provided for cases presenting with acute LBP, with follow-up durations ranging between one and two years. In addition, all included studies except one were of good methodological quality.
One of the limitations of this systematic review is that we were unable to quantitatively synthesize the data using meta-analysis due to the methodological heterogeneity between the included studies. Furthermore, five of the six included studies were conducted in the US, and one study was conducted in Canada, which may reduce the generalizability of the results to other parts of the world with different healthcare systems. The WC administrative databases, the primary source of data in the included studies, lack information on several factors associated with LOD in patients with acute LBP, such as pain severity, functional limitations, psychosocial factors, occupation, job physical requirements, recovery expectations, fear-avoidance, and support at work. However, a prospective cohort study from the UK reported that opioids prescribing for acute LBP cases in primary care were associated with functional disability measured using the Roland-Morris Disability Questionnaire at 6 months of follow-up, even after adjusting for anxiety, depression, fear of movement, pain self-efficacy, and coping strategies [42]. Another limitation is that estimating LOD using wage replacement data may underestimate the true LOD and work absence because the discontinuation of indemnity payments does not imply recovery and return to work. Nevertheless, this approach is frequently used in work disability studies and was found to be an equitable measure that reasonably reflects the total work loss [43]. Furthermore, other longer-term effects of EOP such as addiction and long-term disability should be considered in future studies.
5. Conclusions
The use of early opioid in the management of acute uncomplicated LBP is associated with prolonged disability duration. Adherence to clinical guidelines discouraging the use of opioids for acute LBP may improve functions and prevent prolonged disabilities among patients with acute LBP. Further research on factors influencing inadequate adherence to evidence-based guidelines and optimal strategies to modify such factors may improve disability outcomes among patients presenting with acute LBP.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph191912114/s1. Supplemental File S1. PRISMA 2009 Checklist. Supplemental File S2. Full search strategy. Supplemental File S3. Newcastle-Ottawa quality assessment scale for cohort studies. Reference [44] is cited in the supplementary materials.
Author Contributions
Conceptualization, M.S. and B.A.-O.; data curation, A.R.I., B.A.S., M.O.M., M.E.E., M.A.S., M.S. and B.A.-O.; formal analysis, A.R.I., B.A.S., M.O.M., M.E.E., M.A.S., M.S. and B.A.-O.; investigation, B.A.-O. and M.S.; methodology, B.A.-O. and M.S.; supervision, B.A.-O.; writing—original draft, A.R.I., B.A.S., M.O.M., M.E.E., M.A.S. and B.A.-O.; writing—review and editing, A.R.I., B.A.S., M.O.M., M.E.E., M.A.S., M.S. and B.A.-O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank Qatar University and Khalifa University of Science, Technology, and Research for supporting this project.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Becker, A.; Held, H.; Redaelli, M.; Strauch, K.; Chenot, J.F.; Leonhardt, C.; Keller, S.; Baum, E.; Pfingsten, M.; Hildebrandt, J.; et al. Low back pain in primary care: Costs of care and prediction of future health care utilization. Spine 2010, 35, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Chen, M.; Wu, X.; Lin, S.; Tao, C.; Cao, H.; Shao, Z.; Xiao, G. Global, regional and national burden of low back pain 1990–2019: A systematic analysis of the Global Burden of Disease study 2019. J. Orthop. Transl. 2022, 32, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [CrossRef]
- Costa, L.d.M.; Maher, C.G.; Hancock, M.J.; McAuley, J.H.; Herbert, R.D.; Costa, L.O. The prognosis of acute and persistent low-back pain: A meta-analysis. CMAJ 2012, 184, E613–E624. [Google Scholar] [CrossRef]
- da Silva, T.; Mills, K.; Brown, B.T.; Herbert, R.D.; Maher, C.G.; Hancock, M.J. Risk of Recurrence of Low Back Pain: A Systematic Review. J. Orthop. Sports Phys. 2017, 47, 305–313. [Google Scholar] [CrossRef]
- Andersson, G.B. Epidemiological features of chronic low-back pain. Lancet 1999, 354, 581–585. [Google Scholar] [CrossRef]
- Gore, M.; Sadosky, A.; Stacey, B.R.; Tai, K.S.; Leslie, D. The burden of chronic low back pain: Clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 2012, 37, E668–E677. [Google Scholar] [CrossRef]
- Lambeek, L.C.; van Tulder, M.W.; Swinkels, I.C.; Koppes, L.L.; Anema, J.R.; van Mechelen, W. The trend in total cost of back pain in The Netherlands in the period 2002 to 2007. Spine 2011, 36, 1050–1058. [Google Scholar] [CrossRef]
- Deyo, R.A.; Mirza, S.K.; Turner, J.A.; Martin, B.I. Overtreating chronic back pain: Time to back off? J. Am. Board Fam. Med. 2009, 22, 62–68. [Google Scholar] [CrossRef]
- Dagenais, S.; Caro, J.; Haldeman, S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008, 8, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Steenstra, I.A.; Verbeek, J.H.; Heymans, M.W.; Bongers, P.M. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature. Occup. Env. Med. 2005, 62, 851–860. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Maher, C.G.; Wiech, K.; Van Zundert, J.; Meloto, C.B.; Diatchenko, L.; Battié, M.C.; Goossens, M.; Koes, B.; Linton, S.J. Low back pain. Nat. Rev. Dis Primers 2018, 4, 52. [Google Scholar] [CrossRef] [PubMed]
- Shraim, M.; Cifuentes, M.; Willetts, J.L.; Marucci-Wellman, H.R.; Pransky, G. Regional socioeconomic disparities in outcomes for workers with low back pain in the United States. Am. J. Ind. Med. 2017, 60, 472–483. [Google Scholar] [CrossRef]
- Shraim, M.; Cifuentes, M.; Willetts, J.L.; Marucci-Wellman, H.R.; Pransky, G. Length of Disability and Medical Costs in Low Back Pain: Do State Workers' Compensation Policies Make a Difference? J. Occup. Env. Med. 2015, 57, 1275–1283. [Google Scholar] [CrossRef]
- Shraim, B.A.; Shraim, M.A.; Ibrahim, A.R.; Elgamal, M.E.; Al-Omari, B.; Shraim, M. The association between early MRI and length of disability in acute lower back pain: A systematic review and narrative synthesis. BMC Musculoskelet Disord 2021, 22, 983. [Google Scholar] [CrossRef]
- Webster, B.S.; Verma, S.K.; Gatchel, R.J. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery and late opioid use. Spine 2007, 32, 2127–2132. [Google Scholar] [CrossRef]
- Oliva-Pascual-Vaca, Á.; González-González, C.; Oliva-Pascual-Vaca, J.; Piña-Pozo, F.; Ferragut-Garcías, A.; Fernández-Domínguez, J.C.; Heredia-Rizo, A.M. Visceral Origin: An Underestimated Source of Neck Pain. A Systematic Scoping Review. Diagnostics 2019, 9, 186. [Google Scholar] [CrossRef]
- Giamberardino, M.; Affaitati, G.C. Costantini. Visceral Referred Pain. J. Musculoskelet. Pain 2010, 18, 403–410. [Google Scholar] [CrossRef]
- Cervero, F. Central sensitization and visceral hypersensitivity: Facts and fictions. Scand. J. Pain 2014, 5, 49–50. [Google Scholar] [CrossRef]
- Bikbov, M.M.; Kazakbaeva, G.M.; Zainullin, R.M.; Salavatova, V.F.; Gilmanshin, T.R.; Arslangareeva, I.I.; Nikitin, N.A.; Mukhamadieva, S.R.; Yakupova, D.F.; Panda-Jonas, S.; et al. Prevalence of and factors associated with low Back pain, thoracic spine pain and neck pain in Bashkortostan, Russia: The Ural Eye and Medical Study. BMC Musculoskelet Disord 2020, 21, 64. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.D.; Russell, A.; Hodges, P.W. How common is back pain in women with gastrointestinal problems? Clin. J. Pain 2008, 24, 199–203. [Google Scholar] [CrossRef]
- Benyamin, R.; Trescot, A.M.; Datta, S.; Buenaventura, R.; Adlaka, R.; Sehgal, N.; Glaser, S.E.; Vallejo, R. Opioid complications and side effects. Pain Physician 2008, 11, S105–S120. [Google Scholar] [CrossRef] [PubMed]
- Manchikanti, L.; Singh, A. Therapeutic opioids: A ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician 2008, 11, S63–S88. [Google Scholar] [CrossRef]
- Ballantyne, J.C.; LaForge, S.K. Opioid dependence and addiction during opioid treatment of chronic pain. Pain 2007, 129, 235–255. [Google Scholar] [CrossRef] [PubMed]
- van Tulder, M.; Becker, A.; Bekkering, T.; Breen, A.; del Real, M.T.; Hutchinson, A.; Koes, B.; Laerum, E.; Malmivaara, A. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. Eur. Spine J. 2006, 15 (Suppl. S2), S169–S191. [Google Scholar] [CrossRef]
- National Guideline, C. National Guideline, C. National Institute for Health and Care Excellence: Guidelines. In Low Back Pain and Sciatica in Over 16s: Assessment and Management; National Institute for Health and Care Excellence (NICE): London, UK, 2016. [Google Scholar]
- Qaseem, A.; Wilt, T.J.; McLean, R.M.; Forciea, M.A.; Denberg, T.D.; Barry, M.J.; Boyd, C.; Chow, R.D.; Fitterman, N.; Harris, R.P.; et al. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann. Intern. Med. 2017, 166, 514–530. [Google Scholar] [CrossRef]
- Jeffrey Kao, M.C.; Minh, L.C.; Huang, G.Y.; Mitra, R.; Smuck, M. Trends in ambulatory physician opioid prescription in the United States, 1997-2009. PM R 2014, 6, 575–582.e574. [Google Scholar] [CrossRef]
- Lee, S.S.; Choi, Y.; Pransky, G.S. Extent and Impact of Opioid Prescribing for Acute Occupational Low Back Pain in the Emergency Department. J. Emerg. Med. 2016, 50, 376–384. [Google Scholar] [CrossRef]
- Vogt, M.T.; Kwoh, C.K.; Cope, D.K.; Osial, T.A.; Culyba, M.; Starz, T.W. Analgesic usage for low back pain: Impact on health care costs and service use. Spine 2005, 30, 1075–1081. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, M.A.; Webster, B.S.; Courtney, T.K.; Matz, S.; Tacci, J.A.; Christiani, D.C. Clinical management and the duration of disability for work-related low back pain. J. Occup. Env. Med. 2000, 42, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Wells, G.; Shea, B.; Shea, B.; O’Connell, D.; Peterson, J.; Welch; Losos, M.; Tugwell, P.; Ga, S.W.; et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; University of Ottawa: Ottawa, ON, Canada, 2014. [Google Scholar]
- Viswanathan, M.; Ansari, M.; Berkman, N.; Chang, S.; Hartling, L.; McPheeters, L.; Santaguida, P.; Shamliyan, T.; Singh, K.; Tsertsvadze, A.; et al. Assessing the Risk of Bias of Individual Studies in Systematic Reviews of Health Care Interventions. Agency for healthcare research and quality methods guide for comparative effectiveness reviews. In AHRQ Methods for Effective Health Care; U.S. Department of Health & Human Services, Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012. [Google Scholar]
- Gaspar, F.W.; Thiese, M.S.; Wizner, K.; Hegmann, K. Guideline adherence and lost workdays for acute low back pain in the California workers' compensation system. PLoS ONE 2021, 16, e0253268. [Google Scholar] [CrossRef] [PubMed]
- Shraim, M.; Cifuentes, M.; Willetts, J.L.; Marucci-Wellman, H.R.; Pransky, G. Why does the adverse effect of inappropriate MRI for LBP vary by geographic location? An exploratory analysis. BMC Musculoskelet Disord 2019, 20, 574. [Google Scholar] [CrossRef] [PubMed]
- Gross, D.P.; Stephens, B.; Bhambhani, Y.; Haykowsky, M.; Bostick, G.P.; Rashiq, S. Opioid prescriptions in canadian workers' compensation claimants: Prescription trends and associations between early prescription and future recovery. Spine (Phila Pa 1976) 2009, 34, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes, M.; Webster, B.; Genevay, S.; Pransky, G. The course of opioid prescribing for a new episode of disabling low back pain: Opioid features and dose escalation. Pain 2010, 151, 22–29. [Google Scholar] [CrossRef]
- Verster, J.C.; Veldhuijzen, D.S.; Volkerts, E.R. Effects of an opioid (oxycodone/paracetamol) and an NSAID (bromfenac) on driving ability, memory functioning, psychomotor performance, pupil size, and mood. Clin. J. Pain 2006, 22, 499–504. [Google Scholar] [CrossRef]
- Deyo, R.A.; Von Korff, M.; Duhrkoop, D. Opioids for low back pain. BMJ 2015, 350, g6380. [Google Scholar] [CrossRef]
- Ashworth, J.; Green, D.J.; Dunn, K.M.; Jordan, K.P. Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up? Pain 2013, 154, 1038–1044. [Google Scholar] [CrossRef]
- Krause, N.; Dasinger, L.K.; Deegan, L.J.; Brand, R.J.; Rudolph, L. Alternative approaches for measuring duration of work disability after low back injury based on administrative workers' compensation data. Am. J. Ind. Med. 1999, 35, 604–618. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).