Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Instruments
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ghandour, R.M.; Sherman, L.J.; Vladutiu, C.J.; Ali, M.M.; Lynch, S.E.; Bitsko, R.H.; Blumberg, S.J. Prevalence and Treatment of Depression, Anxiety, and Conduct Problems in US Children. J. Pediatr. 2018, 206, 256–267.e3. [Google Scholar] [CrossRef]
- Merikangas, K.R.; He, J.-P.; Burstein, M.; Swanson, S.A.; Avenevoli, S.; Cui, L.; Benjet, C.; Georgiades, K.; Swendsen, J. Lifetime Prevalence of Mental Disorders in U.S. Adolescents: Results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 980–989. [Google Scholar] [CrossRef]
- Bitsko, R.H.; Holbrook, J.R.; Ghandour, R.M.; Blumberg, S.J.; Visser, S.N.; Perou, R.; Walkup, J.T. Epidemiology and Impact of Health Care Provider–Diagnosed Anxiety and Depression Among US Children. J. Dev. Behav. Pediatr. 2018, 39, 395–403. [Google Scholar] [CrossRef]
- Lantos, J.D.; Yeh, H.-W.; Raza, F.; Connelly, M.; Goggin, K.; Sullivant, S.A. Suicide Risk in Adolescents During the COVID-19 Pandemic. Pediatrics 2022, 149, e2021053486. [Google Scholar] [CrossRef]
- Hails, K.A.; Petts, R.A.; Hostutler, C.A.; Simoni, M.; Greene, R.; Snider, T.C.; Riley, A.R. COVID-19 distress, negative parenting, and child behavioral problems: The moderating role of parent adverse childhood experiences. Child Abus. Negl. 2022, 130, 105450. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Vanderloo, L.M.; Keown-Stoneman, C.D.G.; Cost, K.T.; Charach, A.; Maguire, J.L.; Monga, S.; Crosbie, J.; Burton, C.; Anagnostou, E.; et al. Screen Use and Mental Health Symptoms in Canadian Children and Youth During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2140875. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. U.S. Surgeon General Issues Advisory on Youth Mental Health Crisis Further Exposed by COVID-19 Pandemic|HHS.gov. Available online: https://www.hhs.gov/about/news/2021/12/07/us-surgeon-general-issues-advisory-on-youth-mental-health-crisis-further-exposed-by-covid-19-pandemic.html (accessed on 7 December 2021).
- Collins, K.A.; Westra, H.A.; Dozois, D.J.; Burns, D.D. Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clin. Psychol. Rev. 2004, 24, 583–616. [Google Scholar] [CrossRef] [PubMed]
- Woodward, L.J.; Fergusson, D.M. Life Course Outcomes of Young People with Anxiety Disorders in Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1086–1093. [Google Scholar] [CrossRef]
- Johnson, D.; Dupuis, G.; Piche, J.; Clayborne, Z.; Colman, I. Adult mental health outcomes of adolescent depression: A systematic review. Depress. Anxiety 2018, 35, 700–716. [Google Scholar] [CrossRef]
- World Health Organization Mental Health: Suicide Data. Available online: www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed on 19 October 2021).
- National Center for Injury Prevention and Control; Centers for Disease Control and Prevention Leading Causes of Death Reports, 1981–2016. Available online: https://webappa.cdc.gov/sasweb/ncipc/leadcause.html (accessed on 19 October 2021).
- Centers for Disease Control and Prevention QuickStats: Death Rates for Motor Vehicle Traffic Injury, Suicide, and Homicide among Children and Adolescents Aged 10–14 Years—United States, 1999–2014. Available online: https://www.cdc.gov/mmwr/volumes/65/wr/mm6543a8.htm?s_cid=mm6543a8_w (accessed on 19 October 2021).
- Jones, J.D.; Boyd, R.C.; Calkins, M.E.; Ahmed, A.; Moore, T.M.; Barzilay, R.; Benton, T.D.; Gur, R.E. Parent-Adolescent Agreement About Adolescents’ Suicidal Thoughts. Pediatrics 2019, 143, e20181771. [Google Scholar] [CrossRef] [Green Version]
- Brahmbhatt, K.; Grupp-Phelan, J. Parent-Adolescent Agreement about Adolescent’s Suicidal Thoughts: A Divergence. Pediatrics 2019, 143, e20183071. [Google Scholar] [CrossRef]
- Castellví, P.; Lucas-Romero, E.; Miranda-Mendizábal, A.; Parés-Badell, O.; Almenara, J.; Alonso, I.; Blasco, M.; Cebrià, A.; Gabilondo, A.; Gili, M.; et al. Longitudinal association between self-injurious thoughts and behaviors and suicidal behavior in adolescents and young adults: A systematic review with meta-analysis. J. Affect. Disord. 2017, 215, 37–48. [Google Scholar] [CrossRef]
- Butzer, B.; Ebert, M.; Telles, S.; Khalsa, S.B.S. School-based Yoga Programs in the United States: A Survey. Adv. Mind Body Med. 2015, 29, 18–26. [Google Scholar]
- Sun, Y.; Lamoreau, R.; O’Connell, S.; Horlick, R.; Bazzano, A. Yoga and Mindfulness Interventions for Preschool-Aged Children in Educational Settings: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6091. [Google Scholar] [CrossRef]
- Butzer, B.; Bury, D.; Telles, S.; Khalsa, S.B.S. Implementing yoga within the school curriculum: A scientific rationale for improving social-emotional learning and positive student outcomes. J. Child. Serv. 2016, 11, 3–24. [Google Scholar] [CrossRef]
- Bazzano, A.N.; Anderson, C.E.; Hylton, C.; Gustat, J. Effect of mindfulness and yoga on quality of life for elementary school students and teachers: Results of a randomized controlled school-based study. Psychol. Res. Behav. Manag. 2018, 11, 81–89. [Google Scholar] [CrossRef]
- Mendelson, T.; Greenberg, M.T.; Dariotis, J.K.; Gould, L.F.; Rhoades, B.L.; Leaf, P.J. Feasibility and Preliminary Outcomes of a School-Based Mindfulness Intervention for Urban Youth. J. Abnorm. Child Psychol. 2010, 38, 985–994. [Google Scholar] [CrossRef]
- Butzer, B.; Lorusso, A.; Shin, S.H.; Khalsa, S.B. Evaluation of Yoga for Preventing Adolescent Substance Use Risk Factors in a Middle School Setting: A Preliminary Group-Randomized Controlled Trial. J. Youth Adolesc. 2016, 46, 603–632. [Google Scholar] [CrossRef]
- James-Palmer, A.; Anderson, E.Z.; Zucker, L.; Kofman, Y.; Daneault, J.-F. Yoga as an Intervention for the Reduction of Symptoms of Anxiety and Depression in Children and Adolescents: A Systematic Review. Front. Pediatr. 2020, 8, 78. [Google Scholar] [CrossRef]
- Felver, J.C.; Razza, R.; Morton, M.L.; Clawson, A.J.; Mannion, R.S. School-based yoga intervention increases adolescent resilience: A pilot trial. J. Child Adolesc. Ment. Health 2020, 32, 1–10. [Google Scholar] [CrossRef]
- Folkman, S.; Lazarus, R.S.; Dunkel-Schetter, C.; DeLongis, A.; Gruen, R.J. Dynamics of a stressful encounter: Cognitive appraisal, coping, and encounter outcomes. J. Pers. Soc. Psychol. 1986, 50, 992–1003. [Google Scholar] [CrossRef]
- Lazarus, R.S. Emotions and Interpersonal Relationships: Toward a Person-Centered Conceptualization of Emotions and Coping. J. Personal. 2005, 74, 9–46. [Google Scholar] [CrossRef]
- Hodgkinson, S.; Godoy, L.; Beers, L.S.; Lewin, A. Improving Mental Health Access for Low-Income Children and Families in the Primary Care Setting. Pediatrics 2017, 139, e20151175. [Google Scholar] [CrossRef]
- Schickedanz, A.; Dreyer, B.P.; Halfon, N. Childhood Poverty: Understanding and Preventing the Adverse Impacts of a Most-Prevalent Risk to Pediatric Health and Well-Being. Pediatr. Clin. N. Am. 2015, 62, 1111–1135. [Google Scholar] [CrossRef]
- Larson, K.; Russ, S.A.; Kahn, R.S.; Flores, G.; Goodman, E.; Cheng, T.L.; Halfon, N. Health Disparities: A Life Course Health Development Perspective and Future Research Directions. In Handbook of Life Course Health Development; Halfon, N., Forrest, C., Lerner, R., Faustman, E., Eds.; Springer: Cham, Switzerland, 2017; pp. 499–520. [Google Scholar] [CrossRef]
- Campbell, M.K.; Piaggio, G.; Elbourne, D.R.; Altman, D.G. Consort 2010 statement: Extension to cluster randomised trials. BMJ 2012, 345, e5661. [Google Scholar] [CrossRef]
- Khalsa, S.B.S.; Hickey-Schultz, L.; Cohen, D.; Steiner, N.; Cope, S. Evaluation of the Mental Health Benefits of Yoga in a Secondary School: A Preliminary Randomized Controlled Trial. J. Ment. Health Adm. 2011, 39, 80–90. [Google Scholar] [CrossRef]
- Chen, D.D.; Pauwels, L. Perceived Benefits of Incorporating Yoga into Classroom Teaching: Assessment of the Effects of “Yoga Tools for Teachers”. Adv. Phys. Educ. 2014, 04, 138–148. [Google Scholar] [CrossRef]
- Randomizer. Available online: https://www.randomizer.org/ (accessed on 17 February 2022).
- U.S. Department of Education. Available online: https://www2.ed.gov/about/offices/list/ocr/504faq.html#interrelationship (accessed on 17 February 2022).
- Johnson, J.G.; Harris, E.S.; Spitzer, R.L.; Williams, J.B. The patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J. Adolesc. Health 2002, 30, 196–204. [Google Scholar] [CrossRef]
- Birmaher, B.; Brent, D.A.; Chiappetta, L.; Bridge, J.; Monga, S.; Baugher, M. Psychometric Properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A Replication Study. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 1230–1236. [Google Scholar] [CrossRef]
- Kraag, G.; Zeegers, M.P.; Kok, G.; Hosman, C.; Abu-Saad, H.H. School programs targeting stress management in children and adolescents: A meta-analysis. J. Sch. Psychol. 2006, 44, 449–472. [Google Scholar] [CrossRef]
- Feiss, R.; Dolinger, S.B.; Merritt, M.; Reiche, E.; Martin, K.; Yanes, J.A.; Thomas, C.M.; Pangelinan, M. A Systematic Review and Meta-Analysis of School-Based Stress, Anxiety, and Depression Prevention Programs for Adolescents. J. Youth Adolesc. 2019, 48, 1668–1685. [Google Scholar] [CrossRef] [PubMed]
- Ellis, B.J.; Del Giudice, M.; Dishion, T.J.; Figueredo, A.J.; Gray, P.; Griskevicius, V.; Hawley, P.H.; Jacobs, W.J.; James, J.; Volk, A.A.; et al. The evolutionary basis of risky adolescent behavior: Implications for science, policy, and practice. Dev. Psychol. 2012, 48, 598–623. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, S.B.S.; Butzer, B. Yoga in school settings: A research review. Ann. N. Y. Acad. Sci. 2016, 1373, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Butzer, B.; Day, D.; Potts, A.; Ryan, C.; Coulombe, S.; Davies, B.; Weidknecht, K.; Ebert, M.; Flynn, L.; Khalsa, S.B. Effects of a Classroom-Based Yoga Intervention on Cortisol and Behavior in Second- and Third-Grade Students. J. Evid.-Based Integr. Med. 2014, 20, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Vorkapic, C.; Feitoza, J.M.; Marchioro, M.; Simões, J.; Kozasa, E.; Telles, S. Are There Benefits from Teaching Yoga at Schools? A Systematic Review of Randomized Control Trials of Yoga-Based Interventions. Evid.-Based Complement. Altern. Med. 2015, 2015, 345835. [Google Scholar] [CrossRef]
- Hagen, I.; Nayar, U.S. Yoga for Children and Young People’s Mental Health and Well-Being: Research Review and Reflections on the Mental Health Potentials of Yoga. Front. Psychiatry 2014, 5, 35. [Google Scholar] [CrossRef]
- Dariotis, J.K.; Mirabal-Beltran, R.; Cluxton-Keller, F.; Gould, L.F.; Greenberg, M.T.; Mendelson, T. A Qualitative Evaluation of Student Learning and Skills Use in a School-Based Mindfulness and Yoga Program. Mindfulness 2015, 7, 76–89. [Google Scholar] [CrossRef]
- Johnstone, K.M.; Kemps, E.; Chen, J. A Meta-Analysis of Universal School-Based Prevention Programs for Anxiety and Depression in Children. Clin. Child Fam. Psychol. Rev. 2018, 21, 466–481. [Google Scholar] [CrossRef]
- Masia-Warner, C.; Nangle, D.W.; Hansen, D. Bringing evidence-based child mental health services to the schools: General issues and specific populations. Educ. Treat. Child. 2006, 29, 165–172. [Google Scholar]
- Barrett, P.; Turner, C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. Br. J. Clin. Psychol. 2001, 40, 399–410. [Google Scholar] [CrossRef]
- Barrett, P.M.; Pahl, K.M. School-Based Intervention: Examining a Universal Approach to Anxiety Management. J. Psychol. Couns. Sch. 2005, 16, 55–75. [Google Scholar] [CrossRef]
- Moran, P.; Coffey, C.; Romaniuk, H.; Olsson, C.; Borschmann, R.; Carlin, J.B.; Patton, G.C. The natural history of self-harm from adolescence to young adulthood: A population-based cohort study. Lancet 2012, 379, 236–243. [Google Scholar] [CrossRef] [Green Version]


| Variable | Total | Intervention Group | Control Group | t/χ2 | p-Value |
|---|---|---|---|---|---|
| Sex | (n = 82) | ||||
| Male | 44 (53.7%) | 23 (57.5%) | 21 (50.0%) | 0.463 | 0.50 |
| Female | 38 (46.3%) | 17 (42.5%) | 21 (50.0%) | ||
| Race | (n = 82) | 3.403 | 0.32 | ||
| Asian | 6 (7.3%) | 3 (7.5%) | 3 (7.1%) | ||
| Af. Am. | 55 (67.1%) | 30 (75.0%) | 25 (59.5%) | ||
| White | 19 (23.2%) | 7 (17.5%) | 12 (28.6%) | ||
| Multi-racial | 2 (2.4%) | 0 | 2 (4.8%) | ||
| Ethnicity | (n = 82) | 1.00 | |||
| Non-Hispanic | 80 (97.6%) | 39 (97.5%) | 41 (97.6%) | ||
| Eligibility for lunch | (n = 82) | 1.233 | 0.27 | ||
| Full price | 42 (51.2%) | 23 (57.5%) | 19 (45.2%) | ||
| Free or reduced | 40 (48.8%) | 17 (42.5%) | 23 (54.8%) | ||
| IEP | (n = 82) | 2.347 | 0.30 | ||
| Disability | 5 (6.1%) | 4 (10.0%) | 1 (2.4%) | ||
| Gifted/Talented | 22 (26.8%) | 9 (22.5%) | 13 (31.0%) | ||
| No IEP | 55 (67.1%) | 27 (67.5%) | 28 (66.7%) | ||
| 504 Plan | (n = 82) | 0.658 | 0.42 | ||
| Yes | 13 (15.9%) | 5 (12.5%) | 8 (19.0%) | ||
| No | 69 (84.1%) | 35 (87.5%) | 34 (81.0%) | ||
| PHQA | |||||
| Baseline (n = 79) | 4.97 ± 5.684 | 4.61 ± 4.595 | 5.32 ± 6.574 | 0.561 | 0.58 |
| SCARED a | |||||
| Baseline (n = 82) | 11.82 ± 8.303 | 10.44 ± 7.104 | 13.07 ± 9.161 | 1.444 | 0.15 |
| Total | Intervention Group | Control Group | t/χ2 | p-Value | |
|---|---|---|---|---|---|
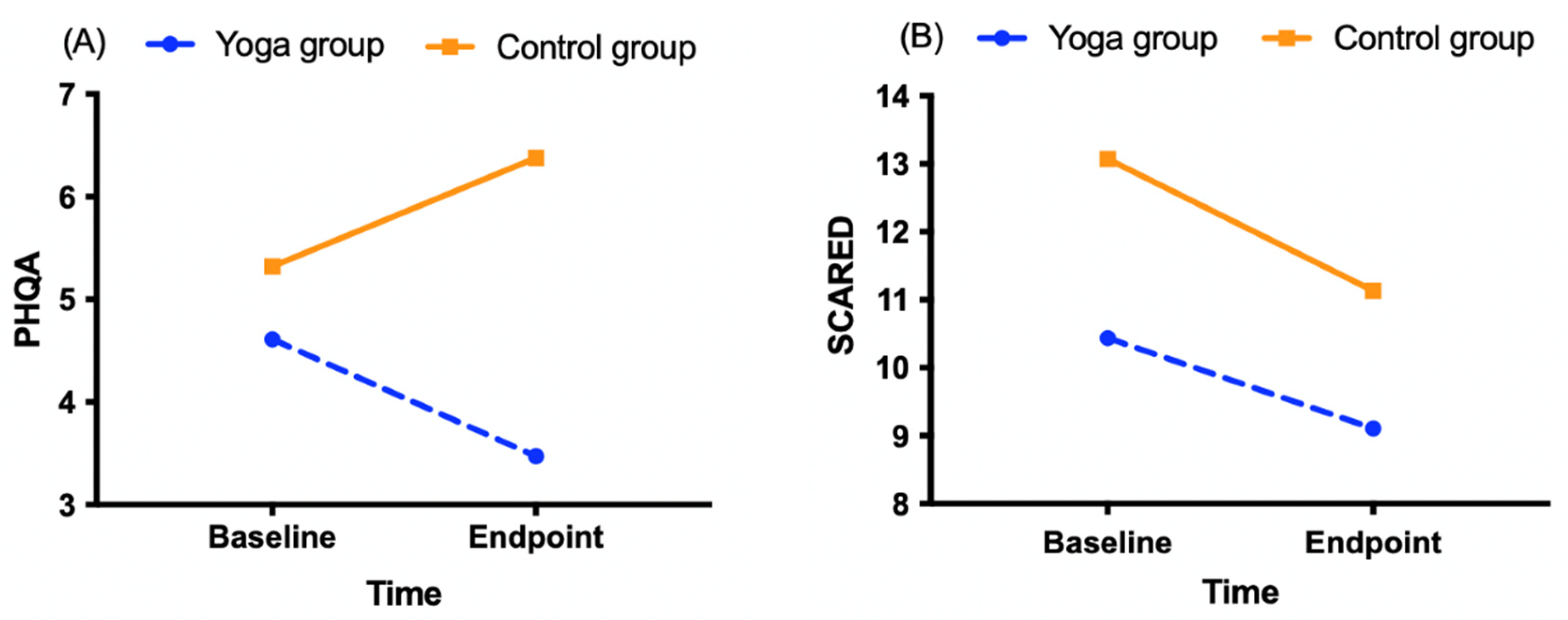
| PHQA | |||||
| Baseline | 4.97 ± 5.684 | 4.61 ± 4.595 | 5.32 ± 6.574 | 0.561 | 0.58 |
| Endpoint | 4.95 ± 5.995 | 3.47 ± 4.37 | 6.38 ± 6.997 | 2.120 | 0.037 * |
| SCARED | |||||
| Baseline | 11.82 ± 8.303 | 10.44 ± 7.104 | 13.07 ± 9.161 | 1.444 | 0.15 |
| Endpoint | 10.12 ± 8.296 | 9.11 ± 7.866 | 11.13 ± 8.690 | 1.066 | 0.29 |
| MD CG-IG | Group Effect | Time Effect | Group × Time Effect | |||||
|---|---|---|---|---|---|---|---|---|
| Wald χ2 | p-Value | Wald χ2 | p-Value | Wald χ2 | p-Value | |||
| PHQA (n = 80) | Baseline | 1.20 (−1.54, 3.93) | 1.852 | 0.174 | 0.011 | 0.918 | 3.695 | 0.055 |
| Endpoint | 2.46 (−0.23, 5.14) | |||||||
| SCARED (n = 81) | Baseline | 1.98 (−1.51, 5.48) | 1.935 | 0.164 | 8.77 | 0.003 | 0.343 | 0.558 |
| Endpoint | 2.71 (−0.84, 6.26) | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bazzano, A.N.; Sun, Y.; Chavez-Gray, V.; Akintimehin, T.; Gustat, J.; Barrera, D.; Roi, C. Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting. Int. J. Environ. Res. Public Health 2022, 19, 12076. https://doi.org/10.3390/ijerph191912076
Bazzano AN, Sun Y, Chavez-Gray V, Akintimehin T, Gustat J, Barrera D, Roi C. Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting. International Journal of Environmental Research and Public Health. 2022; 19(19):12076. https://doi.org/10.3390/ijerph191912076
Chicago/Turabian StyleBazzano, Alessandra N., Yaoyao Sun, Vaughne Chavez-Gray, Temitope Akintimehin, Jeanette Gustat, Denise Barrera, and Cody Roi. 2022. "Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting" International Journal of Environmental Research and Public Health 19, no. 19: 12076. https://doi.org/10.3390/ijerph191912076
APA StyleBazzano, A. N., Sun, Y., Chavez-Gray, V., Akintimehin, T., Gustat, J., Barrera, D., & Roi, C. (2022). Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting. International Journal of Environmental Research and Public Health, 19(19), 12076. https://doi.org/10.3390/ijerph191912076








