Medication Non-Adherence in Rheumatology, Oncology and Cardiology: A Review of the Literature of Risk Factors and Potential Interventions
Abstract
:1. Introduction
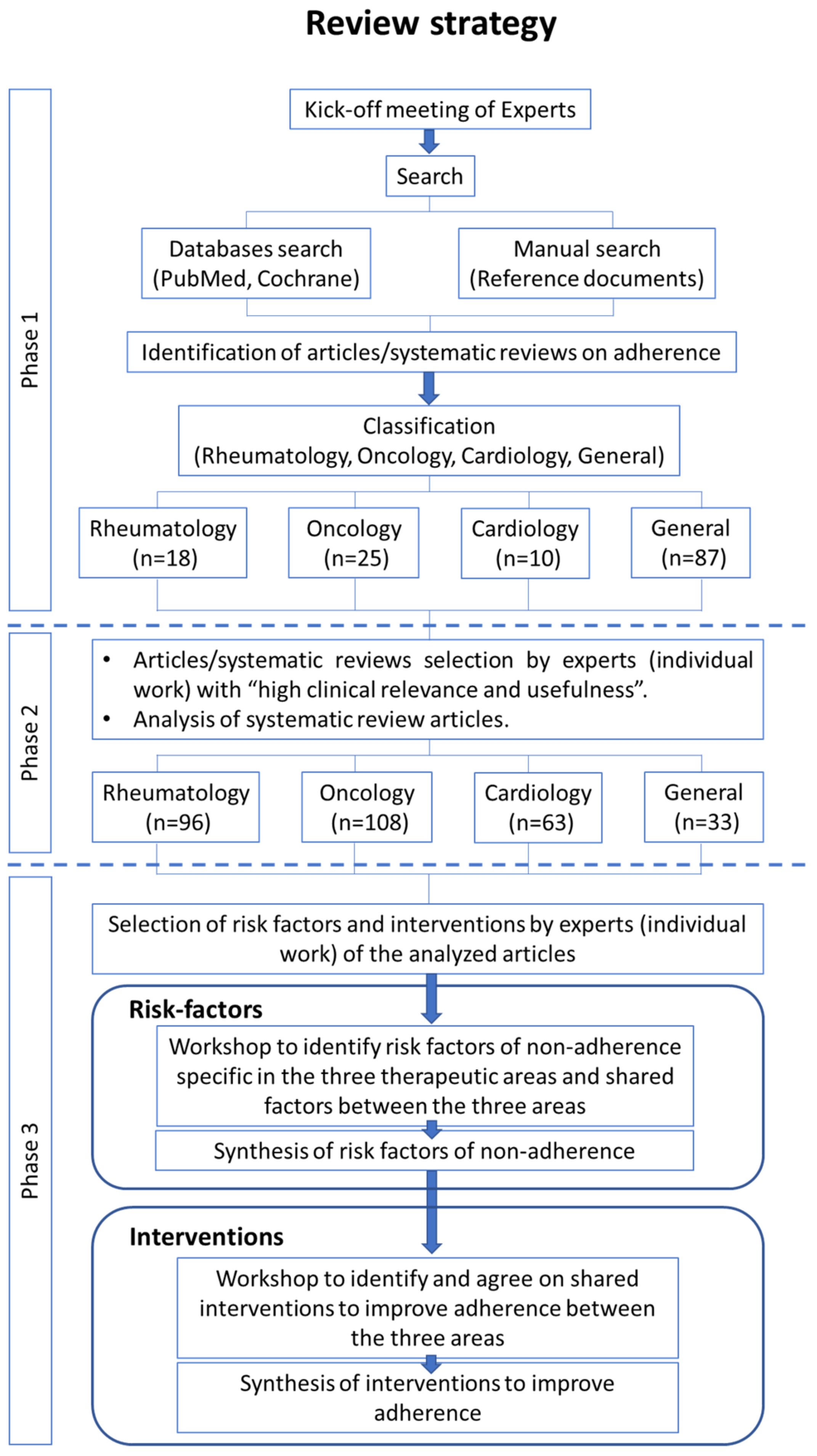
2. Materials and Methods
3. Results
3.1. General Description of the Search Results
3.2. Risk-Factors for Non-Adherence in Rheumatic Diseases
| Rheumatology | |
|---|---|
| Socioeconomic |
|
| Healthcare system |
|
| Patient | |
| Condition | |
| Therapy | |
3.3. Risk Factors for Non-Adherence in Oncology
3.4. Risk Factors for Non-Adherence in Cardiology
| Cardiology | |
|---|---|
| Socioeconomic |
|
| Healthcare system |
|
| Patient |
|
| Condition |
|
| Therapy |
|
3.5. Shared Non-Adherence Risk-Factors
| Socioeconomic | |
|---|---|
| Socioeconomic |
|
| Healthcare system |
|
| Patient |
|
| Condition |
|
| Therapy |
|
3.6. Interventions for Improving Adherence
| Intervention Type | |
|---|---|
| Educative |
|
| |
| Behavioral |
|
| Cognitive |
|
| Affective |
|
| Multifaceted |
|
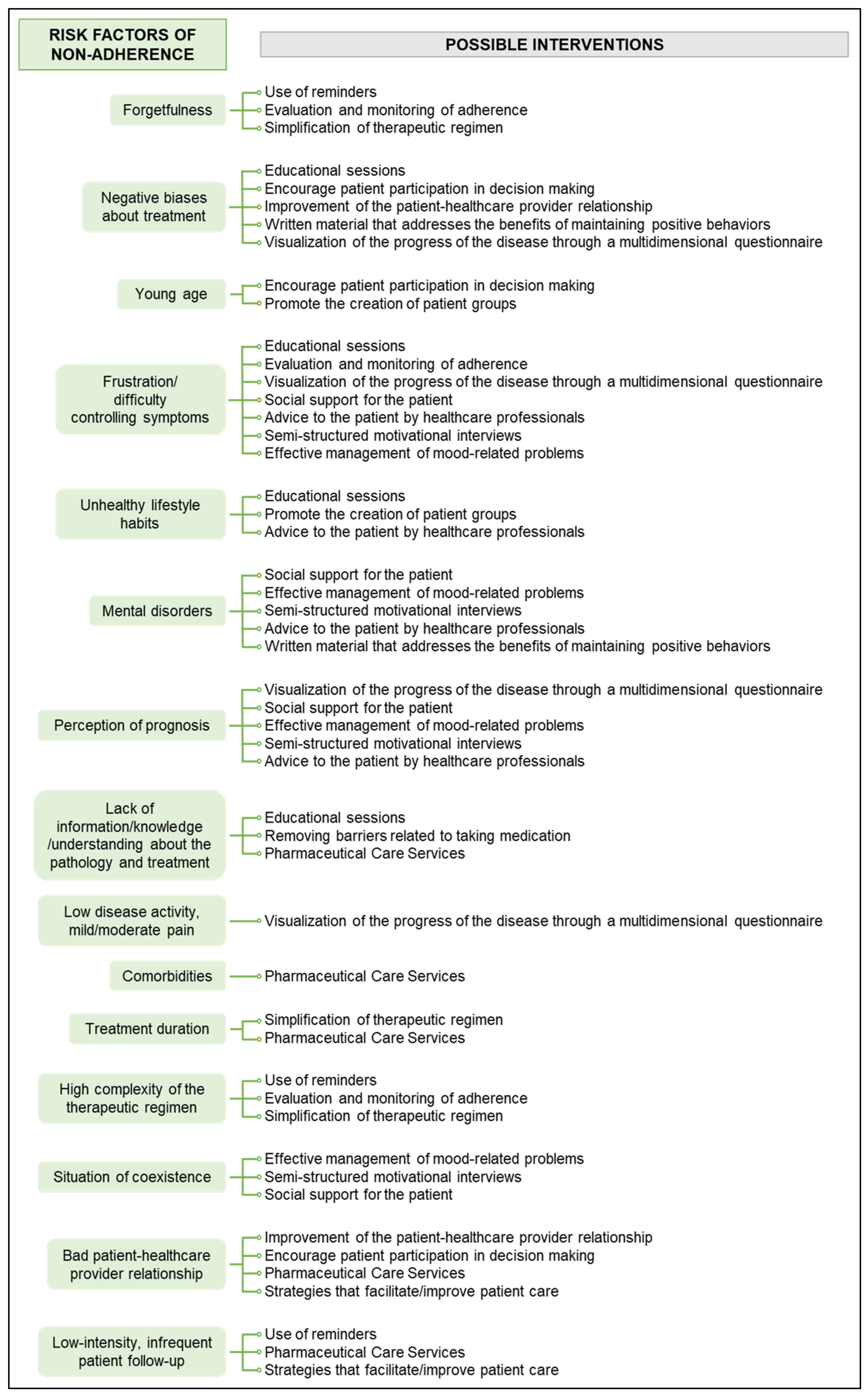
3.7. Proposed Interventions to Address Non-Adherence Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Adherence to Long Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Brown, M.T.; Bussell, J.K. Medication Adherence: WHO Cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [PubMed]
- Claxton, A.J.; Cramer, J.; Pierce, C. A Systematic Review of the Associations between Dose Regimens and Medication Compliance. Clin. Ther. 2001, 23, 1296–1310. [Google Scholar] [CrossRef]
- Nieuwlaat, R.; Wilczynski, N.; Navarro, T.; Hobson, N.; Jeffery, R.; Keepanasseril, A.; Agoritsas, T.; Mistry, N.; Iorio, A.; Jack, S.; et al. Interventions for Enhancing Medication Adherence. Cochrane Database Syst. Rev. 2014, 2014, CD000011. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, F.; Maron, D.J.; Knowles, J.W.; Virani, S.S.; Lin, S.; Heidenreich, P.A. Association of Statin Adherence with Mortality in Patients with Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2019, 4, 206–213. [Google Scholar] [CrossRef]
- Walsh, C.A.; Cahir, C.; Tecklenborg, S.; Byrne, C.; Culbertson, M.A.; Bennett, K.E. The Association between Medication Non-Adherence and Adverse Health Outcomes in Ageing Populations: A Systematic Review and Meta-Analysis. Br. J. Clin. Pharmacol. 2019, 85, 2464–2478. [Google Scholar] [CrossRef]
- Jansen, E.M.; van de Hei, S.J.; Dierick, B.J.H.; Kerstjens, H.A.M.; Kocks, J.W.H.; van Boven, J.F.M. Global Burden of Medication Non-Adherence in Chronic Obstructive Pulmonary Disease (COPD) and Asthma: A Narrative Review of the Clinical and Economic Case for Smart Inhalers. J. Thorac. Dis. 2021, 13, 3846–3864. [Google Scholar] [CrossRef]
- Murali, K.M.; Mullan, J.; Chen, J.H.C.; Roodenrys, S.; Lonergan, M. Medication Adherence in Randomized Controlled Trials Evaluating Cardiovascular or Mortality Outcomes in Dialysis Patients: A Systematic Review. BMC Nephrol. 2017, 18, 42. [Google Scholar] [CrossRef]
- Smith, D.; Lovell, J.; Weller, C.; Kennedy, B.; Winbolt, M.; Young, C.; Ibrahim, J. A Systematic Review of Medication Non-Adherence in Persons with Dementia or Cognitive Impairment. PLoS ONE 2017, 12, e0170651. [Google Scholar] [CrossRef]
- Cutler, R.L.; Fernandez-Llimos, F.; Frommer, M.; Benrimoj, C.; Garcia-Cardenas, V. Economic Impact of Medication Non-Adherence by Disease Groups: A Systematic Review. BMJ Open 2018, 8, e016982. [Google Scholar] [CrossRef]
- Kennedy-Martin, T.; Boye, K.S.; Peng, X. Cost of Medication Adherence and Persistence in Type 2 Diabetes mellitus: A Literature Review. Patient Prefer. Adherence 2017, 11, 1103–1117. [Google Scholar] [CrossRef] [Green Version]
- Campbell, L.; Masquillier, C.; Thunnissen, E.; Ariyo, E.; Tabana, H.; Sematlane, N.; Delport, A.; Dube, L.T.; Knight, L.; Flechner, T.K.; et al. Social and Structural Determinants of Household Support for ART Adherence in Low- and Middle-Income Countries: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 3808. [Google Scholar] [CrossRef]
- Bitton, A.; Choudhry, N.K.; Matlin, O.S.; Swanton, K.; Shrank, W.H. The Impact of Medication Adherence on Coronary Artery Disease Costs and Outcomes: A Systematic Review. Am. J. Med. 2013, 126, e7–e357. [Google Scholar] [CrossRef]
- Brown, M.T.; Bussell, J.; Dutta, S.; Davis, K.; Strong, S.; Mathew, S. Medication Adherence: Truth and Consequences. Am. J. Med. Sci. 2016, 351, 387–399. [Google Scholar] [CrossRef]
- Danielson, E.; Melin-Johansson, C.; Modanloo, M. Adherence to Treatment in Patients with Chronic Diseases: From Alertness to Persistence. Int. J. Community Based Nurs. Midwifery 2019, 7, 248–257. [Google Scholar] [CrossRef]
- Lemay, J.; Waheedi, M.; Al-Sharqawi, S.; Bayoud, T. Medication Adherence in Chronic Illness: Do Beliefs about Medications Play a Role? Patient Prefer. Adherence 2018, 12, 1687–1698. [Google Scholar] [CrossRef]
- Jimmy, B.; Jose, J. Patient Medication Adherence: Measures in Daily Practice. Oman Med. J. 2011, 26, 155–159. [Google Scholar] [CrossRef]
- Kini, V.; Ho, P.M. Interventions to Improve Medication Adherence: A Review. JAMA 2018, 320, 2461–2473. [Google Scholar] [CrossRef]
- Iuga, A.O.; McGuire, M.J. Adherence and Health Care Costs. Risk Manag. Healthc. Policy 2014, 7, 35–44. [Google Scholar] [CrossRef]
- Esbensen, B.A.; Kennedy, N.; Brodin, N. Prevention and Adherence in Rheumatic and Musculoskeletal Disease. Best Pract. Res. Clin. Rheumatol. 2020, 34, 101525. [Google Scholar] [CrossRef]
- Balsa, A.; García de Yébenes, M.J.; Carmona, L. Multilevel Factors Predict Medication Adherence in Rheumatoid Arthritis: A 6-Month Cohort Study. Ann. Rheum. Dis. 2022, 81, 327–334. [Google Scholar] [CrossRef]
- Anghel, L.-A.; Farcaş, A.M.; Oprean, R.N. Medication Adherence and Persistence in Patients with Autoimmune Rheumatic Diseases: A Narrative Review. Patient Prefer. Adherence 2018, 12, 1151–1166. [Google Scholar] [CrossRef] [PubMed]
- Spoelstra, S.L.; Rittenberg, C.N. Assessment and Measurement of Medication Adherence: Oral Agents for Cancer. Clin. J. Oncol. Nurs. 2015, 19, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Clark, R.; Tu, P.; Bosworth, H.B.; Zullig, L.L. Breast Cancer Oral Anti-Cancer Medication Adherence: A Systematic Review of Psychosocial Motivators and Barriers. Breast Cancer Res. Treat. 2017, 165, 247–260. [Google Scholar] [CrossRef] [PubMed]
- Riles, E.M.; Jain, V.A.; Fendrick, A.M. Medication Adherence and Heart Failure. Curr. Cardiol. Rep. 2014, 16, 458. [Google Scholar] [CrossRef]
- Durand, H.; Hayes, P.; Morrissey, E.C.; Newell, J.; Casey, M.; Murphy, A.W.; Molloy, G.J. Medication Adherence among Patients with Apparent Treatment-Resistant Hypertension: Systematic Review and Meta-Analysis. J. Hypertens. 2017, 35, 2346–2357. [Google Scholar] [CrossRef]
- Ahmad, F.B.; Anderson, R.N. The Leading Causes of Death in the US for 2020. JAMA 2021, 325, 1829–1830. [Google Scholar] [CrossRef]
- Pascual-Ramos, V.; Contreras-Yáñez, I. Motivations for Inadequate Persistence with Disease Modifying Anti-Rheumatic Drugs in Early Rheumatoid Arthritis: The Patient’s Perspective. BMC Musculoskelet. Disord. 2013, 14, 336. [Google Scholar] [CrossRef]
- Raimond, V.C.; Feldman, W.B.; Rome, B.N.; Kesselheim, A.S. Why France Spends Less Than the United States on Drugs: A Comparative Study of Drug Pricing and Pricing Regulation. Milbank Q. 2021, 99, 240–272. [Google Scholar] [CrossRef]
- De Cuyper, E.; de Gucht, V.; Maes, S.; van Camp, Y.; de Clerck, L.S. Determinants of Methotrexate Adherence in Rheumatoid Arthritis Patients. Clin. Rheumatol. 2016, 35, 1335–1339. [Google Scholar] [CrossRef]
- Waimann, C.A.; Marengo, M.F.; de Achaval, S.; Cox, V.L.; Garcia-Gonzalez, A.; Reveille, J.D.; Richardson, M.N.; Suarez-Almazor, M.E. Electronic Monitoring of Oral Therapies in Ethnically Diverse and Economically Disadvantaged Patients with Rheumatoid Arthritis: Consequences of Low Adherence. Arthritis Rheum. 2013, 65, 1421–1429. [Google Scholar] [CrossRef] [Green Version]
- Quinlan, P.; Price, K.O.; Magid, S.K.; Lyman, S.; Mandl, L.A.; Stone, P.W. The Relationship among Health Literacy, Health Knowledge, and Adherence to Treatment in Patients with Rheumatoid Arthritis. HSS J. 2013, 9, 42–49. [Google Scholar] [CrossRef]
- Evers, A.W.M.; Kraaimaat, F.W.; van Riel, P.L.C.M.; de Jong, A.J.L. Tailored Cognitive-Behavioral Therapy in Early Rheumatoid Arthritis for Patients at Risk: A Randomized Controlled Trial. Pain 2002, 100, 141–153. [Google Scholar] [CrossRef]
- Arturi, P.; Schneeberger, E.E.; Sommerfleck, F.; Buschiazzo, E.; Ledesma, C.; Maldonado Cocco, J.A.; Citera, G. Adherence to Treatment in Patients with Ankylosing Spondylitis. Clin. Rheumatol. 2013, 32, 1007–1015. [Google Scholar] [CrossRef]
- Cho, S.-K.; Sung, Y.-K.; Choi, C.-B.; Bae, S.-C. Impact of Comorbidities on TNF Inhibitor Persistence in Rheumatoid Arthritis Patients: An Analysis of Korean National Health Insurance Claims Data. Rheumatol. Int. 2012, 32, 3851–3856. [Google Scholar] [CrossRef]
- Abdul-Sattar, A.B.; Abou El Magd, S.A. Determinants of Medication Non-Adherence in Egyptian Patients with Systemic Lupus Erythematosus: Sharkia Governorate. Rheumatol. Int. 2015, 35, 1045–1051. [Google Scholar] [CrossRef]
- Morgan, C.; McBeth, J.; Cordingley, L.; Watson, K.; Hyrich, K.L.; Symmons, D.P.M.; Bruce, I.N. The Influence of Behavioural and Psychological Factors on Medication Adherence over Time in Rheumatoid Arthritis Patients: A Study in the Biologics Era. Rheumatology 2015, 54, 1780–1791. [Google Scholar] [CrossRef]
- Müller, R.; Kallikorm, R.; Põlluste, K.; Lember, M. Compliance with Treatment of Rheumatoid Arthritis. Rheumatol. Int. 2012, 32, 3131–3135. [Google Scholar] [CrossRef]
- Caplan, L.; Wolfe, F.; Michaud, K.; Quinzanos, I.; Hirsh, J.M. Strong Association of Health Literacy with Functional Status among Rheumatoid Arthritis Patients: A Cross-Sectional Study. Arthritis Care Res. 2014, 66, 508–514. [Google Scholar] [CrossRef]
- Betegnie, A.-L.; Gauchet, A.; Lehmann, A.; Grange, L.; Roustit, M.; Baudrant, M.; Bedouch, P.; Allenet, B. Why Do Patients with Chronic Inflammatory Rheumatic Diseases Discontinue Their Biologics? An Assessment of Patients’ Adherence Using a Self-Report Questionnaire. J. Rheumatol. 2016, 43, 724–730. [Google Scholar] [CrossRef]
- Saad, A.A.; Ashcroft, D.M.; Watson, K.D.; Hyrich, K.L.; Noyce, P.R.; Symmons, D.P.M. Persistence with Anti-Tumour Necrosis Factor Therapies in Patients with Psoriatic Arthritis: Observational Study from the British Society of Rheumatology Biologics Register. Arthritis Res. Ther. 2009, 11, R52. [Google Scholar] [CrossRef] [Green Version]
- Glintborg, B.; Højgaard, P.; Lund Hetland, M.; Steen Krogh, N.; Kollerup, G.; Jensen, J.; Chrysidis, S.; Jensen Hansen, I.M.; Holland-Fischer, M.; Højland Hansen, T.; et al. Impact of Tobacco Smoking on Response to Tumour Necrosis Factor-Alpha Inhibitor Treatment in Patients with Ankylosing Spondylitis: Results from the Danish Nationwide DANBIO Registry. Rheumatology 2016, 55, 659–668. [Google Scholar] [CrossRef] [PubMed]
- Treharne, G.J.; Lyons, A.C.; Kitas, G.D. Medication Adherence in Rheumatoid Arthritis: Effects of Psychosocial Factors. Psychol. Health Med. 2004, 9, 337–349. [Google Scholar] [CrossRef]
- Tuncay, R.; Eksioglu, E.; Cakir, B.; Gurcay, E.; Cakci, A. Factors Affecting Drug Treatment Compliance in Patients with Rheumatoid Arthritis. Rheumatol. Int. 2007, 27, 743–746. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.; Mulherin, D. The Influence of Medication Beliefs and Other Psychosocial Factors on Early Discontinuation of Disease-Modifying Anti-Rheumatic Drugs. Musculoskelet. Care 2007, 5, 148–159. [Google Scholar] [CrossRef]
- Contreras-Yáñez, I.; Ponce De León, S.; Cabiedes, J.; Rull-Gabayet, M.; Pascual-Ramos, V. Inadequate Therapy Behavior Is Associated to Disease Flares in Patients with Rheumatoid Arthritis Who Have Achieved Remission with Disease-Modifying Antirheumatic Drugs. Am. J. Med. Sci. 2010, 340, 282–290. [Google Scholar] [CrossRef]
- Garcia-Gonzalez, A.; Richardson, M.; Garcia Popa-Lisseanu, M.; Cox, V.; Kallen, M.A.; Janssen, N.; Ng, B.; Marcus, D.M.; Reveille, J.D.; Suarez-Almazor, M.E. Treatment Adherence in Patients with Rheumatoid Arthritis and Systemic Lupus Erythematosus. Clin. Rheumatol. 2008, 27, 883–889. [Google Scholar] [CrossRef]
- Neame, R.; Hammond, A. Beliefs about Medications: A Questionnaire Survey of People with Rheumatoid Arthritis. Rheumatology 2005, 44, 762–767. [Google Scholar] [CrossRef]
- Pascual-Ramos, V.; Contreras-Yáñez, I.; Villa, A.R.; Cabiedes, J.; Rull-Gabayet, M. Medication Persistence over 2 Years of Follow-up in a Cohort of Early Rheumatoid Arthritis Patients: Associated Factors and Relationship with Disease Activity and with Disability. Arthritis Res. Ther. 2009, 11, R26. [Google Scholar] [CrossRef]
- Spruill, T.M.; Ogedegbe, G.; Harrold, L.R.; Potter, J.; Scher, J.U.; Rosenthal, P.B.; Greenberg, J.D. Association of Medication Beliefs and Self-Efficacy with Adherence in Urban Hispanic and African-American Rheumatoid Arthritis Patients. Ann. Rheum. Dis. 2014, 73, 317–318. [Google Scholar] [CrossRef]
- De Klerk, E.; van der Heijde, D.; Landewé, R.; van der Tempel, H.; Urquhart, J.; van der Linden, S. Patient Compliance in Rheumatoid Arthritis, Polymyalgia Rheumatica, and Gout. J. Rheumatol. 2003, 30, 44–54. [Google Scholar]
- Stockl, K.M.; Shin, J.S.; Lew, H.C.; Zakharyan, A.; Harada, A.S.M.; Solow, B.K.; Curtis, B.S. Outcomes of a Rheumatoid Arthritis Disease Therapy Management Program Focusing on Medication Adherence. J. Manag. Care Pharm. 2010, 16, 593–604. [Google Scholar] [CrossRef] [Green Version]
- Van den Bemt, B.J.F.; van den Hoogen, F.H.J.; Benraad, B.; Hekster, Y.A.; van Riel, P.L.C.M.; van Lankveld, W. Adherence Rates and Associations with Nonadherence in Patients with Rheumatoid Arthritis Using Disease Modifying Antirheumatic Drugs. J. Rheumatol. 2009, 36, 2164–2170. [Google Scholar] [CrossRef]
- Neugut, A.I.; Subar, M.; Wilde, E.T.; Stratton, S.; Brouse, C.H.; Hillyer, G.C.; Grann, V.R.; Hershman, D.L. Association between Prescription Co-Payment Amount and Compliance with Adjuvant Hormonal Therapy in Women with Early-Stage Breast Cancer. J. Clin. Oncol. 2011, 29, 2534–2542. [Google Scholar] [CrossRef]
- Wigertz, A.; Ahlgren, J.; Holmqvist, M.; Fornander, T.; Adolfsson, J.; Lindman, H.; Bergkvist, L.; Lambe, M. Adherence and Discontinuation of Adjuvant Hormonal Therapy in Breast Cancer Patients: A Population-Based Study. Breast Cancer Res. Treat. 2012, 133, 367–373. [Google Scholar] [CrossRef]
- Greer, J.A.; Amoyal, N.; Nisotel, L.; Fishbein, J.N.; MacDonald, J.; Stagl, J.; Lennes, I.; Temel, J.S.; Safren, S.A.; Pirl, W.F. A Systematic Review of Adherence to Oral Antineoplastic Therapies. Oncologist 2016, 21, 354–376. [Google Scholar] [CrossRef]
- Xu, S.; Yang, Y.; Tao, W.; Song, Y.; Chen, Y.; Ren, Y.; Liu, J.; Pang, D. Tamoxifen Adherence and Its Relationship to Mortality in 116 Men with Breast Cancer. Breast Cancer Res. Treat. 2012, 136, 495–502. [Google Scholar] [CrossRef]
- Trabulsi, N.; Riedel, K.; Winslade, N.; Gregoire, J.-P.; Meterissian, S.; Abrahamovicz, M.; Tamblyn, R.; Mayo, N.; Meguerditchian, A. Adherence to Anti-Estrogen Therapy in Seniors with Breast Cancer: How Well Are We Doing? Breast J. 2014, 20, 632–638. [Google Scholar] [CrossRef]
- Efficace, F.; Baccarani, M.; Rosti, G.; Cottone, F.; Castagnetti, F.; Breccia, M.; Alimena, G.; Iurlo, A.; Rossi, A.R.; Pardini, S.; et al. Investigating Factors Associated with Adherence Behaviour in Patients with Chronic Myeloid Leukemia: An Observational Patient-Centered Outcome Study. Br. J. Cancer 2012, 107, 904–909. [Google Scholar] [CrossRef]
- Bender, C.M.; Gentry, A.L.; Brufsky, A.M.; Casillo, F.E.; Cohen, S.M.; Dailey, M.M.; Donovan, H.S.; Dunbar-Jacob, J.; Jankowitz, R.C.; Rosenzweig, M.Q.; et al. Influence of Patient and Treatment Factors on Adherence to Adjuvant Endocrine Therapy in Breast Cancer. Oncol. Nurs. Forum 2014, 41, 274–285. [Google Scholar] [CrossRef]
- Kahn, K.L.; Schneider, E.C.; Malin, J.L.; Adams, J.L.; Epstein, A.M. Patient Centered Experiences in Breast Cancer: Predicting Long-Term Adherence to Tamoxifen Use. Med. Care 2007, 45, 431–439. [Google Scholar] [CrossRef]
- Eliasson, L.; Clifford, S.; Barber, N.; Marin, D. Exploring Chronic Myeloid Leukemia Patients’ Reasons for Not Adhering to the Oral Anticancer Drug Imatinib as Prescribed. Leuk. Res. 2011, 35, 626–630. [Google Scholar] [CrossRef]
- Geissler, J.; Sharf, G.; Bombaci, F.; Daban, M.; de Jong, J.; Gavin, T.; Pelouchova, J.; Dziwinski, E.; Hasford, J.; Hoffmann, V.S. Factors Influencing Adherence in CML and Ways to Improvement: Results of a Patient-Driven Survey of 2546 Patients in 63 Countries. J. Cancer Res. Clin. Oncol. 2017, 143, 1167–1176. [Google Scholar] [CrossRef]
- Noens, L.; van Lierde, M.-A.; de Bock, R.; Verhoef, G.; Zachée, P.; Berneman, Z.; Martiat, P.; Mineur, P.; van Eygen, K.; MacDonald, K.; et al. Prevalence, Determinants, and Outcomes of Nonadherence to Imatinib Therapy in Patients with Chronic Myeloid Leukemia: The ADAGIO Study. Blood 2009, 113, 5401–5411. [Google Scholar] [CrossRef]
- Kirk, M.C.; Hudis, C.A. Insight into Barriers against Optimal Adherence to Oral Hormonal Therapy in Women with Breast Cancer. Clin. Breast Cancer 2008, 8, 155–161. [Google Scholar] [CrossRef]
- Muluneh, B.; Deal, A.; Alexander, M.D.; Keisler, M.D.; Markey, J.M.; Neal, J.M.; Bernard, S.; Valgus, J.; Dressler, L.G. Patient Perspectives on the Barriers Associated with Medication Adherence to Oral Chemotherapy. J. Oncol. Pharm. Pract. 2018, 24, 98–109. [Google Scholar] [CrossRef]
- Stanton, A.L.; Petrie, K.J.; Partridge, A.H. Contributors to Nonadherence and Nonpersistence with Endocrine Therapy in Breast Cancer Survivors Recruited from an Online Research Registry. Breast Cancer Res. Treat. 2014, 145, 525–534. [Google Scholar] [CrossRef]
- Rust, C.; Davis, C. Health Literacy and Medication Adherence in Underserved African-American Breast Cancer Survivors: A Qualitative Study. Soc. Work Health Care 2011, 50, 739–761. [Google Scholar] [CrossRef]
- Verbrugghe, M.; Verhaeghe, S.; Lauwaert, K.; Beeckman, D.; van Hecke, A. Determinants and Associated Factors Influencing Medication Adherence and Persistence to Oral Anticancer Drugs: A Systematic Review. Cancer Treat. Rev. 2013, 39, 610–621. [Google Scholar] [CrossRef]
- Corrente, J. Oral Chemotherapy, a Tough Pill to Swallow: A Systematic Review. Master’s Thesis, Rhode Island College, Providence, RI, USA, 2016. [Google Scholar]
- Wu, E.Q.; Johnson, S.; Beaulieu, N.; Arana, M.; Bollu, V.; Guo, A.; Coombs, J.; Feng, W.; Cortes, J. Healthcare Resource Utilization and Costs Associated with Non-Adherence to Imatinib Treatment in Chronic Myeloid Leukemia Patients. Curr. Med. Res. Opin. 2010, 26, 61–69. [Google Scholar] [CrossRef]
- Darkow, T.; Henk, H.J.; Thomas, S.K.; Feng, W.; Baladi, J.-F.; Goldberg, G.A.; Hatfield, A.; Cortes, J. Treatment Interruptions and Non-Adherence with Imatinib and Associated Healthcare Costs: A Retrospective Analysis among Managed Care Patients with Chronic Myelogenous Leukaemia. Pharmacoeconomics 2007, 25, 481–496. [Google Scholar] [CrossRef]
- McCowan, C.; Shearer, J.; Donnan, P.T.; Dewar, J.A.; Crilly, M.; Thompson, A.M.; Fahey, T.P. Cohort Study Examining Tamoxifen Adherence and Its Relationship to Mortality in Women with Breast Cancer. Br. J. Cancer 2008, 99, 1763–1768. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atkins, L.; Fallowfield, L. Intentional and Non-Intentional Non-Adherence to Medication amongst Breast Cancer Patients. Eur. J. Cancer 2006, 42, 2271–2276. [Google Scholar] [CrossRef] [PubMed]
- Barron, T.I.; Connolly, R.; Bennett, K.; Feely, J.; Kennedy, M.J. Early Discontinuation of Tamoxifen: A Lesson for Oncologists. Cancer 2007, 109, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Partridge, A.H.; Wang, P.S.; Winer, E.P.; Avorn, J. Nonadherence to Adjuvant Tamoxifen Therapy in Women with Primary Breast Cancer. J. Clin. Oncol. 2003, 21, 602–606. [Google Scholar] [CrossRef]
- Manning, M.; Bettencourt, B.A. Depression and Medication Adherence among Breast Cancer Survivors: Bridging the Gap with the Theory of Planned Behaviour. Psychol. Health 2011, 26, 1173–1187. [Google Scholar] [CrossRef]
- Spoelstra, S.L.; Given, B.A.; Given, C.W.; Grant, M.; Sikorskii, A.; You, M.; Decker, V. An Intervention to Improve Adherence and Management of Symptoms for Patients Prescribed Oral Chemotherapy Agents: An Exploratory Study. Cancer Nurs. 2013, 36, 18–28. [Google Scholar] [CrossRef]
- Sedjo, R.L.; Devine, S. Predictors of Non-Adherence to Aromatase Inhibitors among Commercially Insured Women with Breast Cancer. Breast Cancer Res. Treat. 2011, 125, 191–200. [Google Scholar] [CrossRef]
- Jacobs, J.M.; Pensak, N.A.; Sporn, N.J.; MacDonald, J.J.; Lennes, I.T.; Safren, S.A.; Pirl, W.F.; Temel, J.S.; Greer, J.A. Treatment Satisfaction and Adherence to Oral Chemotherapy in Patients with Cancer. J. Oncol. Pract. 2017, 13, e474–e485. [Google Scholar] [CrossRef]
- Schneider, S.M.; Adams, D.B.; Gosselin, T. A Tailored Nurse Coaching Intervention for Oral Chemotherapy Adherence. J. Adv. Pract. Oncol. 2014, 5, 163–172. [Google Scholar]
- Maurice, A.; Howell, A.; Evans, D.G.; O’Neil, A.C.; Scobie, S. Predicting Compliance in a Breast Cancer Prevention Trial. Breast J. 2006, 12, 446–450. [Google Scholar] [CrossRef]
- Blanchette, P.S.; Lam, M.; Richard, L.; Allen, B.; Shariff, S.Z.; Vandenberg, T.; Pritchard, K.I.; Chan, K.K.W.; Louie, V.A.; Desautels, D.; et al. Factors Associated with Endocrine Therapy Adherence among Post-Menopausal Women Treated for Early-Stage Breast Cancer in Ontario, Canada. Breast Cancer Res. Treat. 2020, 179, 217–227. [Google Scholar] [CrossRef]
- Demissie, S.; Silliman, R.A.; Lash, T.L. Adjuvant Tamoxifen: Predictors of Use, Side Effects, and Discontinuation in Older Women. J. Clin. Oncol. 2001, 19, 322–328. [Google Scholar] [CrossRef]
- Llarena, N.C.; Estevez, S.L.; Tucker, S.L.; Jeruss, J.S. Impact of Fertility Concerns on Tamoxifen Initiation and Persistence. JNCI J. Natl. Cancer Inst. 2015, 107, djv202. [Google Scholar] [CrossRef]
- Grunfeld, E.A.; Hunter, M.S.; Sikka, P.; Mittal, S. Adherence Beliefs among Breast Cancer Patients Taking Tamoxifen. Patient Educ. Couns. 2005, 59, 97–102. [Google Scholar] [CrossRef]
- Friese, C.R.; Pini, T.M.; Li, Y.; Abrahamse, P.H.; Graff, J.J.; Hamilton, A.S.; Jagsi, R.; Janz, N.K.; Hawley, S.T.; Katz, S.J.; et al. Adjuvant Endocrine Therapy Initiation and Persistence in a Diverse Sample of Patients with Breast Cancer. Breast Cancer Res. Treat. 2013, 138, 931–939. [Google Scholar] [CrossRef]
- Walker, H.E.; Rosenberg, S.M.; Stanton, A.L.; Petrie, K.J.; Partridge, A.H. Perceptions, Attributions, and Emotions Toward Endocrine Therapy in Young Women with Breast Cancer. J. Adolesc. Young Adult Oncol. 2016, 5, 16–23. [Google Scholar] [CrossRef]
- Rust, C.F.; Davis, C.; Moore, M.R. Medication Adherence Skills Training for African-American Breast Cancer Survivors: The Effects on Health Literacy, Medication Adherence, and Self-Efficacy. Soc. Work Health Care 2015, 54, 33–46. [Google Scholar] [CrossRef]
- Liu, Y.; Malin, J.L.; Diamant, A.L.; Thind, A.; Maly, R.C. Adherence to Adjuvant Hormone Therapy in Low-Income Women with Breast Cancer: The Role of Provider-Patient Communication. Breast Cancer Res. Treat. 2013, 137, 829–836. [Google Scholar] [CrossRef]
- Kimmick, G.; Edmond, S.N.; Bosworth, H.B.; Peppercorn, J.; Marcom, P.K.; Blackwell, K.; Keefe, F.J.; Shelby, R.A. Medication Taking Behaviors among Breast Cancer Patients on Adjuvant Endocrine Therapy. Breast 2015, 24, 630–636. [Google Scholar] [CrossRef]
- Van Londen, G.J.; Donovan, H.S.; Beckjord, E.B.; Cardy, A.L.; Bovbjerg, D.H.; Davidson, N.E.; Morse, J.Q.; Switzer, G.E.; Verdonck-de Leeuw, I.M.; Dew, M.A. Perspectives of Postmenopausal Breast Cancer Survivors on Adjuvant Endocrine Therapy-Related Symptoms. Oncol. Nurs. Forum 2014, 41, 660–668. [Google Scholar] [CrossRef]
- Decker, V.; Spoelstra, S.; Miezo, E.; Bremer, R.; You, M.; Given, C.; Given, B. A Pilot Study of an Automated Voice Response System and Nursing Intervention to Monitor Adherence to Oral Chemotherapy Agents. Cancer Nurs. 2009, 32, E20–E29. [Google Scholar] [CrossRef]
- Simon, R.; Latreille, J.; Matte, C.; Desjardins, P.; Bergeron, E. Adherence to Adjuvant Endocrine Therapy in Estrogen Receptor-Positive Breast Cancer Patients with Regular Follow-Up. Can. J. Surg. 2014, 57, 26–32. [Google Scholar] [CrossRef] [Green Version]
- Murthy, V.; Bharia, G.; Sarin, R. Tamoxifen Non-Compliance: Does It Matter? Lancet Oncol. 2002, 3, 654. [Google Scholar] [CrossRef]
- Bhattacharya, D.; Easthall, C.; Willoughby, K.A.; Small, M.; Watson, S. Capecitabine Non-Adherence: Exploration of Magnitude, Nature and Contributing Factors. J. Oncol. Pharm. Pract. 2012, 18, 333–342. [Google Scholar] [CrossRef]
- Winterhalder, R.; Hoesli, P.; Delmore, G.; Pederiva, S.; Bressoud, A.; Hermann, F.; von Moos, R. Self-Reported Compliance with Capecitabine: Findings from a Prospective Cohort Analysis. Oncology 2011, 80, 29–33. [Google Scholar] [CrossRef]
- Philipovskiy, A.; Campbell, A.; Heydarian, R.; Castillo, B.; Dwivedi, A.K.; McCallum, R.; Aguilera, R.; Gaur, S.; Nahleh, Z. Adherence to Adjuvant Aromatase Inhibitor Therapy Among Postmenopausal Hispanic/Latino Women with Breast Cancer. Anticancer Res. 2020, 40, 857–864. [Google Scholar] [CrossRef]
- Brito, C.; Portela, M.C.; de Vasconcellos, M.T.L. Adherence to Hormone Therapy among Women with Breast Cancer. BMC Cancer 2014, 14, 397. [Google Scholar] [CrossRef]
- Mallick, R.; Cai, J.; Wogen, J. Predictors of Non-Adherence to Systemic Oral Therapy for Advanced Hepatocellular Carcinoma. Curr. Med. Res. Opin. 2013, 29, 1701–1708. [Google Scholar] [CrossRef]
- Hershman, D.L.; Tsui, J.; Meyer, J.; Glied, S.; Hillyer, G.C.; Wright, J.D.; Neugut, A.I. The Change from Brand-Name to Generic Aromatase Inhibitors and Hormone Therapy Adherence for Early-Stage Breast Cancer. J. Natl. Cancer Inst. 2014, 106, dju319. [Google Scholar] [CrossRef]
- Hershman, D.L.; Shao, T.; Kushi, L.H.; Buono, D.; Tsai, W.Y.; Fehrenbacher, L.; Kwan, M.; Gomez, S.L.; Neugut, A.I. Early Discontinuation and Non-Adherence to Adjuvant Hormonal Therapy Are Associated with Increased Mortality in Women with Breast Cancer. Breast Cancer Res. Treat. 2011, 126, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Hershman, D.L.; Kushi, L.H.; Shao, T.; Buono, D.; Kershenbaum, A.; Tsai, W.-Y.; Fehrenbacher, L.; Gomez, S.L.; Miles, S.; Neugut, A.I. Early Discontinuation and Nonadherence to Adjuvant Hormonal Therapy in a Cohort of 8,769 Early-Stage Breast Cancer Patients. J. Clin. Oncol. 2010, 28, 4120–4128. [Google Scholar] [CrossRef] [PubMed]
- Makubate, B.; Donnan, P.T.; Dewar, J.A.; Thompson, A.M.; McCowan, C. Cohort Study of Adherence to Adjuvant Endocrine Therapy, Breast Cancer Recurrence and Mortality. Br. J. Cancer 2013, 108, 1515–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hershman, D.L.; Kushi, L.H.; Hillyer, G.C.; Coromilas, E.; Buono, D.; Lamerato, L.; Bovbjerg, D.H.; Mandelblatt, J.S.; Tsai, W.-Y.; Zhong, X.; et al. Psychosocial Factors Related to Non-Persistence with Adjuvant Endocrine Therapy among Women with Breast Cancer: The Breast Cancer Quality of Care Study (BQUAL). Breast Cancer Res. Treat. 2016, 157, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Fink, A.K.; Gurwitz, J.; Rakowski, W.; Guadagnoli, E.; Silliman, R.A. Patient Beliefs and Tamoxifen Discontinuance in Older Women with Estrogen Receptor--Positive Breast Cancer. J. Clin. Oncol. 2004, 22, 3309–3315. [Google Scholar] [CrossRef]
- Grundmark, B.; Garmo, H.; Zethelius, B.; Stattin, P.; Lambe, M.; Holmberg, L. Anti-Androgen Prescribing Patterns, Patient Treatment Adherence and Influencing Factors; Results from the Nationwide PCBaSe Sweden. Eur. J. Clin. Pharmacol. 2012, 68, 1619–1630. [Google Scholar] [CrossRef]
- Bhatta, S.S.; Hou, N.; Moton, Z.N.; Polite, B.N.; Fleming, G.F.; Olopade, O.I.; Huo, D.; Hong, S. Factors Associated with Compliance to Adjuvant Hormone Therapy in Black and White Women with Breast Cancer. SpringerPlus 2013, 2, 356. [Google Scholar] [CrossRef]
- Hsieh, K.-P.; Chen, L.-C.; Cheung, K.-L.; Chang, C.-S.; Yang, Y.-H. Interruption and Non-Adherence to Long-Term Adjuvant Hormone Therapy Is Associated with Adverse Survival Outcome of Breast Cancer Women—An Asian Population-Based Study. PLoS ONE 2014, 9, e87027. [Google Scholar] [CrossRef]
- Ma, A.M.T.; Barone, J.; Wallis, A.E.; Wu, N.J.; Garcia, L.B.; Estabrook, A.; Rosenbaum-Smith, S.M.; Tartter, P.I. Noncompliance with Adjuvant Radiation, Chemotherapy, or Hormonal Therapy in Breast Cancer Patients. Am. J. Surg. 2008, 196, 500–504. [Google Scholar] [CrossRef]
- Partridge, A.H.; Archer, L.; Kornblith, A.B.; Gralow, J.; Grenier, D.; Perez, E.; Wolff, A.C.; Wang, X.; Kastrissios, H.; Berry, D.; et al. Adherence and Persistence with Oral Adjuvant Chemotherapy in Older Women with Early-Stage Breast Cancer in CALGB 49907: Adherence Companion Study 60104. J. Clin. Oncol. 2010, 28, 2418–2422. [Google Scholar] [CrossRef]
- Marin, D.; Bazeos, A.; Mahon, F.-X.; Eliasson, L.; Milojkovic, D.; Bua, M.; Apperley, J.F.; Szydlo, R.; Desai, R.; Kozlowski, K.; et al. Adherence Is the Critical Factor for Achieving Molecular Responses in Patients with Chronic Myeloid Leukemia Who Achieve Complete Cytogenetic Responses on Imatinib. J. Clin. Oncol. 2010, 28, 2381–2388. [Google Scholar] [CrossRef]
- Sadahiro, S.; Ohki, S.; Yamaguchi, S.; Takahashi, T.; Otani, Y.; Tsukikawa, S.; Yamamura, T.; Takemiya, S.; Nagasaki, H.; Nishiyama, K.; et al. Feasibility of a Novel Weekday-on/Weekend-off Oral UFT Schedule as Postoperative Adjuvant Chemotherapy for Colorectal Cancer. UFT Compliance Study Group, Kanagawa, Japan. Cancer Chemother. Pharm. 2000, 46, 180–184. [Google Scholar] [CrossRef]
- Lash, T.L.; Fox, M.P.; Westrup, J.L.; Fink, A.K.; Silliman, R.A. Adherence to Tamoxifen over the Five-Year Course. Breast Cancer Res. Treat. 2006, 99, 215–220. [Google Scholar] [CrossRef]
- Gebbia, V.; Bellavia, M.; Banna, G.L.; Russo, P.; Ferraù, F.; Tralongo, P.; Borsellino, N. Treatment Monitoring Program for Implementation of Adherence to Second-Line Erlotinib for Advanced Non-Small-Cell Lung Cancer. Clin. Lung Cancer 2013, 14, 390–398. [Google Scholar] [CrossRef]
- Lee, H.-S.; Lee, J.-Y.; Ah, Y.-M.; Kim, H.-S.; Im, S.-A.; Noh, D.-Y.; Lee, B.K. Low Adherence to Upfront and Extended Adjuvant Letrozole Therapy among Early Breast Cancer Patients in a Clinical Practice Setting. Oncology 2014, 86, 340–349. [Google Scholar] [CrossRef]
- Santoleri, F.; Sorice, P.; Lasala, R.; Rizzo, R.C.; Costantini, A. Patient Adherence and Persistence with Imatinib, Nilotinib, Dasatinib in Clinical Practice. PLoS ONE 2013, 8, e56813. [Google Scholar] [CrossRef]
- Santoleri, F.; Lasala, R.; Ranucci, E.; la Barba, G.; di Lorenzo, R.; Vetrò, A.; di Bartolomeo, P.; Costantini, A. Medication Adherence to Tyrosine Kinase Inhibitors: 2-Year Analysis of Medication Adherence to Imatinib Treatment for Chronic Myeloid Leukemia and Correlation with the Depth of Molecular Response. Acta Haematol. 2016, 136, 45–51. [Google Scholar] [CrossRef]
- Fernández-Ribeiro, F.; Olivera-Fernández, R.; Crespo-Diz, C. Adherence and Safety Study in Patients on Treatment with Capecitabine. Farm. Hosp. 2017, 41, 204–221. [Google Scholar] [CrossRef]
- Bardel, A.; Wallander, M.-A.; Svärdsudd, K. Factors Associated with Adherence to Drug Therapy: A Population-Based Study. Eur. J. Clin. Pharmacol. 2007, 63, 307–314. [Google Scholar] [CrossRef]
- Ho, P.M.; Spertus, J.A.; Masoudi, F.A.; Reid, K.J.; Peterson, E.D.; Magid, D.J.; Krumholz, H.M.; Rumsfeld, J.S. Impact of Medication Therapy Discontinuation on Mortality after Myocardial Infarction. Arch. Intern. Med. 2006, 166, 1842–1847. [Google Scholar] [CrossRef]
- Kripalani, S.; Gatti, M.E.; Jacobson, T.A. Association of Age, Health Literacy, and Medication Management Strategies with Cardiovascular Medication Adherence. Patient Educ. Couns. 2010, 81, 177–181. [Google Scholar] [CrossRef]
- Sandoval, D.; Chacón, J.; Muñoz, R.; Henríquez, Ó.; Koch, E.; Romero, T. Influencia de Factores Psicosociales En La Adherencia al Tratamiento Farmacológico Antihipertensivo: Resultados de Una Cohorte Del Programa de Salud Cardiovascular de La Región Metropolitana, Chile. Rev. Méd. Chile 2014, 142, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.C.; Shrank, W.H.; Cutler, D.; Jan, S.; Fischer, M.A.; Liu, J.; Avorn, J.; Solomon, D.; Brookhart, M.A.; Choudhry, N.K. Patient, Physician, and Payment Predictors of Statin Adherence. Med. Care 2010, 48, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Roth, M.T.; Esserman, D.A.; Ivey, J.L.; Weinberger, M. Racial Disparities in Quality of Medication Use in Older Adults: Findings from a Longitudinal Study. Am. J. Geriatr. Pharmacother. 2011, 9, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Castellano, J.M.; Copeland-Halperin, R.; Fuster, V. Aiming at Strategies for a Complex Problem of Medical Nonadherence. Glob. Heart 2013, 8, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Benner, J.S.; Glynn, R.J.; Mogun, H.; Neumann, P.J.; Weinstein, M.C.; Avorn, J. Long-Term Persistence in Use of Statin Therapy in Elderly Patients. JAMA 2002, 288, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.S.; Bohn, R.L.; Knight, E.; Glynn, R.J.; Mogun, H.; Avorn, J. Noncompliance with Antihypertensive Medications: The Impact of Depressive Symptoms and Psychosocial Factors. J. Gen. Intern. Med. 2002, 17, 504–511. [Google Scholar] [CrossRef]
- Maddox, T.M.; Ho, P.M. Medication Adherence and the Patient with Coronary Artery Disease: Challenges for the Practitioner. Curr. Opin. Cardiol. 2009, 24, 468–472. [Google Scholar] [CrossRef]
- Burnier, M. Medication Adherence and Persistence as the Cornerstone of Effective Antihypertensive Therapy. Am. J. Hypertens. 2006, 19, 1190–1196. [Google Scholar] [CrossRef]
- Nair, V.K.; Belletti, D.A.; Doyle, J.J.; Allen, R.R.; McQueen, R.B.; Saseen, J.J.; Vande Griend, J.; Patel, V.J.; McQueen, A.; Jan, S. Understanding Barriers to Medication Adherence in the Hypertensive Population by Evaluating Responses to a Telephone Survey. Patient Prefer. Adherence 2011, 5, 195–206. [Google Scholar] [CrossRef]
- Bowry, A.D.K.; Shrank, W.H.; Lee, J.L.; Stedman, M.; Choudhry, N.K. A Systematic Review of Adherence to Cardiovascular Medications in Resource-Limited Settings. J. Gen. Intern. Med. 2011, 26, 1479–1491. [Google Scholar] [CrossRef]
- Rublee, D.A.; Chen, S.-Y.; Mardekian, J.; Wu, N.; Rao, P.; Boulanger, L. Evaluation of Cardiovascular Morbidity Associated with Adherence to Atorvastatin Therapy. Am. J. Ther. 2012, 19, 24–32. [Google Scholar] [CrossRef]
- Dragomir, A.; Côté, R.; Roy, L.; Blais, L.; Lalonde, L.; Bérard, A.; Perreault, S. Impact of Adherence to Antihypertensive Agents on Clinical Outcomes and Hospitalization Costs. Med. Care 2010, 48, 418–425. [Google Scholar] [CrossRef]
- Breekveldt-Postma, N.S.; Penning-van Beest, F.J.A.; Siiskonen, S.J.; Falvey, H.; Vincze, G.; Klungel, O.H.; Herings, R.M.C. The Effect of Discontinuation of Antihypertensives on the Risk of Acute Myocardial Infarction and Stroke. Curr. Med. Res. Opin. 2008, 24, 121–127. [Google Scholar] [CrossRef]
- Rosenberg, S.M.; Petrie, K.J.; Stanton, A.L.; Ngo, L.; Finnerty, E.; Partridge, A.H. Interventions to Enhance Adherence to Oral Antineoplastic Agents: A Scoping Review. J. Natl. Cancer Inst. 2020, 112, 443–465. [Google Scholar] [CrossRef]
- Hurtado-de-Mendoza, A.; Cabling, M.L.; Lobo, T.; Dash, C.; Sheppard, V.B. Behavioral Interventions to Enhance Adherence to Hormone Therapy in Breast Cancer Survivors: A Systematic Literature Review. Clin. Breast Cancer 2016, 16, 247–255.e3. [Google Scholar] [CrossRef]
- Marengo, M.F.; Suarez-Almazor, M.E. Improving Treatment Adherence in Patients with Rheumatoid Arthritis: What Are the Options? Int. J. Clin. Rheumtol. 2015, 10, 345–356. [Google Scholar] [CrossRef]
- Van den Bemt, B.J.F.; Zwikker, H.E.; van den Ende, C.H.M. Medication Adherence in Patients with Rheumatoid Arthritis: A Critical Appraisal of the Existing Literature. Expert Rev. Clin. Immunol. 2012, 8, 337–351. [Google Scholar] [CrossRef]
- Van den Bemt, B.J.F.; van Lankveld, W.G.J.M. How Can We Improve Adherence to Therapy by Patients with Rheumatoid Arthritis? Nat. Clin. Pract. Rheumatol. 2007, 3, 681. [Google Scholar] [CrossRef]
- Agher, D.; Sedki, K.; Tsopra, R.; Despres, S.; Jaulent, M.-C. Influence of Connected Health Interventions for Adherence to Cardiovascular Disease Prevention: A Scoping Review. Appl. Clin. Inform. 2020, 11, 544–555. [Google Scholar] [CrossRef]
- Xu, H.-Y.; Yu, Y.-J.; Zhang, Q.-H.; Hu, H.-Y.; Li, M. Tailored Interventions to Improve Medication Adherence for Cardiovascular Diseases. Front. Pharmacol. 2020, 11, 510339. [Google Scholar] [CrossRef]
- Garfield, S.; Judah, G. Learning from Successes: Designing Medication Adherence Intervention Research so That We Can Learn What Works and Why. BMJ Qual. Saf. 2021, 31, 83–85. [Google Scholar] [CrossRef]
- González-Bueno, J.; Calvo-Cidoncha, E.; Nieto-Martín, M.D.; Pérez-Guerrero, C.; Ollero-Baturone, M.; Santos-Ramos, B. Selection of Interventions Aimed at Improving Medication Adherence in Patients with Multimorbidity. Eur. J. Hosp. Pharm. 2019, 26, 39–45. [Google Scholar] [CrossRef]
- Allemann, S.S.; Nieuwlaat, R.; van den Bemt, B.J.F.; Hersberger, K.E.; Arnet, I. Matching Adherence Interventions to Patient Determinants Using the Theoretical Domains Framework. Front. Pharmacol. 2016, 7, 429. [Google Scholar] [CrossRef]
- Anderson, L.J.; Nuckols, T.K.; Coles, C.; Le, M.M.; Schnipper, J.L.; Shane, R.; Jackevicius, C.; Lee, J.; Pevnick, J.M. A Systematic Overview of Systematic Reviews Evaluating Medication Adherence Interventions. Am. J. Health Syst. Pharm. 2020, 77, 138–147. [Google Scholar] [CrossRef]
- Becerra, V.; Gracia, A.; Desai, K.; Abogunrin, S.; Brand, S.; Chapman, R.; García Alonso, F.; Fuster, V.; Sanz, G. Cost-Effectiveness and Public Health Benefit of Secondary Cardiovascular Disease Prevention from Improved Adherence Using a Polypill in the UK. BMJ Open 2015, 5, e007111. [Google Scholar] [CrossRef]
- Birand, N.; Boşnak, A.S.; Diker, Ö.; Abdikarim, A.; Başgut, B. The Role of the Pharmacist in Improving Medication Beliefs and Adherence in Cancer Patients. J. Oncol. Pharm. Pract. 2019, 25, 1916–1926. [Google Scholar] [CrossRef]
- Muluneh, B.; Schneider, M.; Faso, A.; Amerine, L.; Daniels, R.; Crisp, B.; Valgus, J.; Savage, S. Improved Adherence Rates and Clinical Outcomes of an Integrated, Closed-Loop, Pharmacist-Led Oral Chemotherapy Management Program. J. Oncol. Pract. 2018, 14, e324–e334. [Google Scholar] [CrossRef]
- Holle, L.M.; Bilse, T.; Alabelewe, R.M.; Kintzel, P.E.; Kandemir, E.A.; Tan, C.J.; Weru, I.; Chambers, C.R.; Dobish, R.; Handel, E.; et al. International Society of Oncology Pharmacy Practitioners (ISOPP) Position Statement: Role of the Oncology Pharmacy Team in Cancer Care. J. Oncol. Pharm. Pract. 2021, 27, 785–801. [Google Scholar] [CrossRef]
- Marengoni, A.; Monaco, A.; Costa, E.; Cherubini, A.; Prados-Torres, A.; Muth, C.; Melis, R.J.F.; Pasina, L.; van der Cammen, T.J.M.; Palmer, K.; et al. Strategies to Improve Medication Adherence in Older Persons: Consensus Statement from the Senior Italia Federanziani Advisory Board. Drugs Aging 2016, 33, 629–637. [Google Scholar] [CrossRef]
- Oñatibia-Astibia, A.; Malet-Larrea, A.; Larrañaga, B.; Gastelurrutia, M.Á.; Calvo, B.; Ramírez, D.; Cantero, I.; Garay, Á.; Goyenechea, E. Tailored Interventions by Community Pharmacists and General Practitioners Improve Adherence to Statins in a Spanish Randomized Controlled Trial. Health Serv. Res. 2019, 54, 658–668. [Google Scholar] [CrossRef]
- Patton, D.E.; Cadogan, C.A.; Ryan, C.; Francis, J.J.; Gormley, G.J.; Passmore, P.; Kerse, N.; Hughes, C.M. Improving Adherence to Multiple Medications in Older People in Primary Care: Selecting Intervention Components to Address Patient-Reported Barriers and Facilitators. Health Expect. Int. J. Public Particip. Health Care Health Policy 2018, 21, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Doggrell, S.A. A Review of Interventions ≥ 6 Months by Pharmacists on Adherence to Medicines in Cardiovascular Disease: Characteristics of What Works and What Doesn’t. Res. Soc. Adm. Pharm. 2019, 15, 119–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogedegbe, G.O.; Boutin-Foster, C.; Wells, M.T.; Allegrante, J.P.; Isen, A.M.; Jobe, J.B.; Charlson, M.E. A Randomized Controlled Trial of Positive-Affect Intervention and Medication Adherence in Hypertensive African Americans. Arch. Intern. Med. 2012, 172, 322–326. [Google Scholar] [CrossRef] [PubMed]
- Amini, M.; Zayeri, F.; Salehi, M. Trend Analysis of Cardiovascular Disease Mortality, Incidence, and Mortality-to-Incidence Ratio: Results from Global Burden of Disease Study 2017. BMC Public Health 2021, 21, 401. [Google Scholar] [CrossRef]
- Kumamaru, H.; Lee, M.P.; Choudhry, N.K.; Dong, Y.-H.; Krumme, A.A.; Khan, N.; Brill, G.; Kohsaka, S.; Miyata, H.; Schneeweiss, S.; et al. Using Previous Medication Adherence to Predict Future Adherence. J. Manag. Care Spec. Pharm. 2018, 24, 1146–1155. [Google Scholar] [CrossRef]
- Franklin, J.M.; Krumme, A.A.; Shrank, W.H.; Matlin, O.S.; Brennan, T.A.; Choudhry, N.K. Predicting Adherence Trajectory Using Initial Patterns of Medication Filling. Am. J. Manag. Care 2015, 21, e537–e544. [Google Scholar]
- Wang, L.; Fan, R.; Zhang, C.; Hong, L.; Zhang, T.; Chen, Y.; Liu, K.; Wang, Z.; Zhong, J. Applying Machine Learning Models to Predict Medication Nonadherence in Crohn’s Disease Maintenance Therapy. Patient Prefer. Adherence 2020, 14, 917–926. [Google Scholar] [CrossRef]
- Koesmahargyo, V.; Abbas, A.; Zhang, L.; Guan, L.; Feng, S.; Yadav, V.; Galatzer-Levy, I.R. Accuracy of Machine Learning-Based Prediction of Medication Adherence in Clinical Research. Psychiatry Res. 2020, 294, 113558. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gil-Guillen, V.F.; Balsa, A.; Bernárdez, B.; Valdés y Llorca, C.; Márquez-Contreras, E.; de la Haba-Rodríguez, J.; Castellano, J.M.; Gómez-Martínez, J. Medication Non-Adherence in Rheumatology, Oncology and Cardiology: A Review of the Literature of Risk Factors and Potential Interventions. Int. J. Environ. Res. Public Health 2022, 19, 12036. https://doi.org/10.3390/ijerph191912036
Gil-Guillen VF, Balsa A, Bernárdez B, Valdés y Llorca C, Márquez-Contreras E, de la Haba-Rodríguez J, Castellano JM, Gómez-Martínez J. Medication Non-Adherence in Rheumatology, Oncology and Cardiology: A Review of the Literature of Risk Factors and Potential Interventions. International Journal of Environmental Research and Public Health. 2022; 19(19):12036. https://doi.org/10.3390/ijerph191912036
Chicago/Turabian StyleGil-Guillen, Vicente F., Alejandro Balsa, Beatriz Bernárdez, Carmen Valdés y Llorca, Emilio Márquez-Contreras, Juan de la Haba-Rodríguez, Jose M. Castellano, and Jesús Gómez-Martínez. 2022. "Medication Non-Adherence in Rheumatology, Oncology and Cardiology: A Review of the Literature of Risk Factors and Potential Interventions" International Journal of Environmental Research and Public Health 19, no. 19: 12036. https://doi.org/10.3390/ijerph191912036
APA StyleGil-Guillen, V. F., Balsa, A., Bernárdez, B., Valdés y Llorca, C., Márquez-Contreras, E., de la Haba-Rodríguez, J., Castellano, J. M., & Gómez-Martínez, J. (2022). Medication Non-Adherence in Rheumatology, Oncology and Cardiology: A Review of the Literature of Risk Factors and Potential Interventions. International Journal of Environmental Research and Public Health, 19(19), 12036. https://doi.org/10.3390/ijerph191912036






