Effects of the Short-Foot Exercise on Foot Alignment and Muscle Hypertrophy in Flatfoot Individuals: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Selection Criteria
2.2. Search Strategy and Study Selection
2.3. Data Extraction
2.4. Methodological Quality Appraisal
2.5. Outcomes
2.6. Statistical Analysis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
3.4. Navicular Drop
3.5. Foot Posture
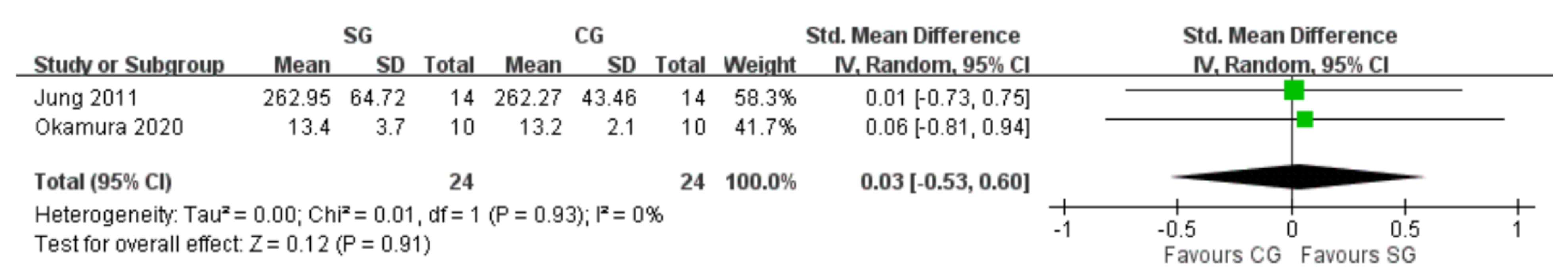
3.6. Muscle Hypertrophy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shibuya, N.; Jupiter, D.C.; Ciliberti, L.J.; VanBuren, V.; La Fontaine, J. Characteristics of adult flatfoot in the United States. J. Foot Ankle Surg. 2010, 49, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.S.; Vanore, J.V.; Thomas, J.L.; Catanzariti, A.R.; Kogler, G.; Kravitz, S.R.; Miller, S.J.; Gassen, S.C. Clinical Practice Guideline Adult Flatfoot Panel. Diagnosis and treatment of adult flatfoot. J. Foot Ankle Surg. 2005, 44, 78–113. [Google Scholar] [CrossRef] [PubMed]
- Buldt, A.K.; Murley, G.S.; Butterworth, P.; Levinger, P.; Menz, H.B.; Landorf, K.B. The relationship between foot posture and lower limb kinematics during walking: A systematic review. Gait Posture 2013, 38, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Tong, J.W.; Kong, P.W. Association between foot type and lower extremity injuries: Systematic literature review with meta-analysis. J. Orthop Sports Phys. Ther. 2013, 43, 700–714. [Google Scholar] [CrossRef]
- Banwell, H.A.; Thewlis, D.; Mackintosh, S. Adults with flexible pes planus and the approach to the prescription of customised foot orthoses in clinical practice: A clinical records audit. Foot (Edinb) 2015, 25, 101–109. [Google Scholar] [CrossRef]
- Desmyttere, G.; Hajizadeh, M.; Bleau, J.; Begon, M. Effect of foot orthosis design on lower limb joint kinematics and kinetics during walking in flexible pes planovalgus: A systematic review and meta-analysis. Clin. Biomech. 2018, 59, 117–129. [Google Scholar] [CrossRef]
- McKeon, P.O.; Hertel, J.; Bramble, D.; Davis, I. The foot core system: A new paradigm for understanding intrinsic foot muscle function. Br. J. Sports Med. 2015, 49, 290. [Google Scholar] [CrossRef]
- Kelly, L.A.; Cresswell, A.G.; Racinais, S.; Whiteley, R.; Lichtwark, G. Intrinsic foot muscles have the capacity to control deformation of the longitudinal arch. J. R. Soc. Interface 2014, 11, 20131188. [Google Scholar] [CrossRef]
- McKeon, P.O.; Fourchet, F. Freeing the foot: Integrating the foot core system into rehabilitation for lower extremity injuries. Clin. Sports Med. 2015, 34, 347–361. [Google Scholar] [CrossRef]
- Jung, D.Y.; Kim, M.H.; Koh, E.K.; Kwon, O.Y.; Cynn, H.S.; Lee, W.H. A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys. Ther. Sport 2011, 12, 30–35. [Google Scholar] [CrossRef]
- Haun, C.; Brown, C.N.; Hannigan, K.; Johnson, S.T. The Effects of the Short Foot Exercise on Navicular Drop: A Critically Appraised Topic. J. Sport Rehabil. 2020, 30, 152–157. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Pisal, S.N.; Chotai, K.; Patil, S. Effectiveness of Short Foot Exercises Versus Towel Curl Exercises to Improve Balance and Foot Posture in Individuals with Flexible Flat Foot. Indian J. Forensic Med. Toxicol. 2020, 14, 653–658. [Google Scholar]
- Tourillon, R.; Gojanovic, B.; Fourchet, F. How to evaluate and improve foot strength in athletes: An update. Front. Sports Act. Living 2019, 1, 46. [Google Scholar] [CrossRef]
- Unver, B.; Erdem, E.U.; Akbas, E. Effects of short-foot exercises on foot posture, pain, disability, and plantar pressure in Pes Planus. J. Sport Rehabil. 2019, 29, 436–440. [Google Scholar] [CrossRef]
- Jung, D.Y.; Koh, E.K.; Kwon, O.Y. Effect of foot orthoses and short-foot exercise on the cross-sectional area of the abductor hallucis muscle in subjects with pes planus: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2011, 24, 225–231. [Google Scholar] [CrossRef]
- Kim, E.K.; Kim, J.S. The effects of short foot exercises and arch support insoles on improvement in the medial longitudinal arch and dynamic balance of flexible flatfoot patients. J. Phys. Ther. Sci. 2016, 28, 3136–3139. [Google Scholar] [CrossRef]
- Kisacik, P.; Tunay, V.B.; Bek, N.; Atay, O.A.; Selfe, J.; Karaduman, A.A. Short foot exercises have additional effects on knee pain, foot biomechanics, and lower extremity muscle strength in patients with patellofemoral pain. J. Back Musculoskelet. Rehabil. 2021, 34, 1093–1104. [Google Scholar] [CrossRef]
- Okamura, K.; Fukuda, K.; Oki, S.; Ono, T.; Tanaka, S.; Kanai, S. Effects of plantar intrinsic foot muscle strengthening exercise on static and dynamic foot kinematics: A pilot randomized controlled single-blind trial in individuals with pes planus. Gait Posture 2020, 75, 40–45. [Google Scholar] [CrossRef]
- Pabon-Carrasco, M.; Castro-Mendez, A.; Vilar-Palomo, S.; Jimenez-Cebrian, A.M.; Garcia-Paya, I.; Palomo-Toucedo, I.C. Randomized Clinical Trial: The Effect of Exercise of the Intrinsic Muscle on Foot Pronation. Int. J. Environ. Res. Public Health 2020, 17, 4882. [Google Scholar] [CrossRef]
- Park, D.J.; Lee, K.S.; Park, S.Y. Effects of Two Foot-Ankle Interventions on Foot Structure, Function, and Balance Ability in Obese People with Pes Planus. Healthcare 2021, 9, 667. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Feuerbach, J.W.; Grabiner, M.D.; Koh, T.J.; Weiker, G.G. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am. J. Sports Med. 1994, 22, 223–229. [Google Scholar] [CrossRef]
- Collaboration, C. 9.4. 5.2 Meta-analysis of change scores. In Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration; John Wiley & Sons: Hoboken, NJ, USA, 2011. [Google Scholar]
- Powers, S.K.; Howley, E.T.; Quindry, J. Exercise Physiology: Theory and Application to Fitness and Performance; McGraw-Hill: New York, NY, USA, 2007. [Google Scholar]
- Seidler, R.D.; Bernard, J.A.; Burutolu, T.B.; Fling, B.W.; Gordon, M.T.; Gwin, J.T.; Kwak, Y.; Lipps, D.B. Motor control and aging: Links to age-related brain structural, functional, and biochemical effects. Neurosci. Biobehav. Rev. 2010, 34, 721–733. [Google Scholar] [CrossRef] [Green Version]



| Author (Year) | Study Design | Inclusion Criteria | Number of Patients (Male, %) | Age, Year, Mean ± SD | BMI, kg/m2, Mean ± SD | Intervention | |
|---|---|---|---|---|---|---|---|
| Jung (2011) | RCT | Bilateral pes planus foot with RCSP ≥4 of eversion and ND exceeding 13 mm | SG: 14 CG: 14 | SG: 22.36 ± 2.41 CG: 21.93 ± 2.73 | Height SG:164.89 ± 8.82 CG: 167.96 ± 7.27 | Weight SG: 57.71 ± 9.65 CG: 58.93 ± 7.84 | SG: Foot orthoses and short-foot exercise twice daily for 8 weeks CG: Foot orthoses for 8 weeks |
| Kim (2016) | RCT | Subjects whose dominant foot had flexible flatfoot according to ND exceeding 10 mm | SG: 7 (85.7) CG: 7 (57.1) | SG: 24.0 ± 1.9 CG: 24.1 ± 1.5 | Height SG: 172.2 ± 6.9 CG: 167.0 ± 6.7 | Weight SG: 68.2 ± 12.9 CG: 63.3 ± 17.6 | SG: Short-foot exercise 30 min at a time, three times per week for 5 weeks CG: Insoles in the shoes and walk 30 min at a time, three times per week for 5 weeks |
| Kısacık (2021) | RCT | Patellofemoral pain patients with pronated foot defined by FPI-6 score ≥ 6 | SG: 15 CG: 15 | SG: 39.60 ± 8.87 CG: 43.60 ± 7.76 | SG: 25.36 ± 5.19 CG: 25.09 ± 3.77 | SG: Supervised hip and knee strengthening and stretching exercises, and short-foot exercise 2 times per week for 6 weeks CG: Supervised hip and knee strengthening and stretching exercises 2 times per week for 6 weeks | |
| Okamura (2020) | RCT | Participants with FPI-6 score ≥ 6 | SG: 10 (10) CG: 10 (20) | SG: 19.7 ± 0.9 CG: 20.2 ± 1.5 | SG: 19.8 ± 1.4 CG: 21.1 ± 2.1 | SG: Short-foot exercise three times per week for 8 weeks CG: No intervention | |
| Pabón-Carrasco (2020) | RCT | FPI-6 score ≥ 6 in both feet to identify pronator individuals | SG: 42 (57.1) CG: 43 (41.9) | SG: 19.45 ± 0.38 CG: 20.92 ± 1.1 | SG: 24.13 ± 4.16 CG: 21.65 ± 3.35 | SG: Short-foot exercise daily for 4 weeks CG: Dorsal and plantar flexion exercise of the metatarsophalangeal joints daily for 4 weeks | |
| Park (2021) | RCT | BMI ≥ 25 kg/m2, ND ≥ 10 mm, and inner longitudinal arch angle ≥ 150 | SG: 12 (58.3) CG: 12 (58.3) | SG: 23.25 ± 1.22 CG: 24.00 ± 1.48 | SG: 29.34 ± 2.81 CG: 29.39 ± 4.57 | SG: Short-foot exercise 3 times a week for 20 min over 4 weeks CG: Proprioceptive neuromuscular facilitation 3 times a week for 20 min over 4 weeks | |
| Author (Year) | Bias Arising from Randomization Process | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|
| Jung (2011) | Some concerns a | Some concerns c | Low risk | Low risk | Low risk | Some concerns |
| Kim (2016) | Some concerns a | Some concerns c | Low risk | Some concerns d | Low risk | High risk |
| Kısacık (2021) | Low risk | Some concerns c | Low risk | Some concerns d | Low risk | Some concerns |
| Okamura (2020) | Some concerns a | Some concerns c | Low risk | Low risk | Some concerns f | High risk |
| Pabón-Carrasco (2020) | Some concerns b | Low risk | Low risk | Low risk | Low risk | Some concerns |
| Park (2021) | Some concerns a | Some concerns c | Low risk | Some concerns e | Low risk | High risk |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C.; Chen, L.-Y.; Liao, Y.-H.; Masodsai, K.; Lin, Y.-Y. Effects of the Short-Foot Exercise on Foot Alignment and Muscle Hypertrophy in Flatfoot Individuals: A Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11994. https://doi.org/10.3390/ijerph191911994
Huang C, Chen L-Y, Liao Y-H, Masodsai K, Lin Y-Y. Effects of the Short-Foot Exercise on Foot Alignment and Muscle Hypertrophy in Flatfoot Individuals: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(19):11994. https://doi.org/10.3390/ijerph191911994
Chicago/Turabian StyleHuang, Ching, Liang-Yu Chen, Yi-Hung Liao, Kunanya Masodsai, and Yi-Yuan Lin. 2022. "Effects of the Short-Foot Exercise on Foot Alignment and Muscle Hypertrophy in Flatfoot Individuals: A Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 19: 11994. https://doi.org/10.3390/ijerph191911994
APA StyleHuang, C., Chen, L.-Y., Liao, Y.-H., Masodsai, K., & Lin, Y.-Y. (2022). Effects of the Short-Foot Exercise on Foot Alignment and Muscle Hypertrophy in Flatfoot Individuals: A Meta-Analysis. International Journal of Environmental Research and Public Health, 19(19), 11994. https://doi.org/10.3390/ijerph191911994






