Home- and Community-Based Interventions for Physical Activity and Early Child Development: A Systematic Review of Effective Strategies
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Quality Assessment of Studies
2.5. Effect Measures
3. Results
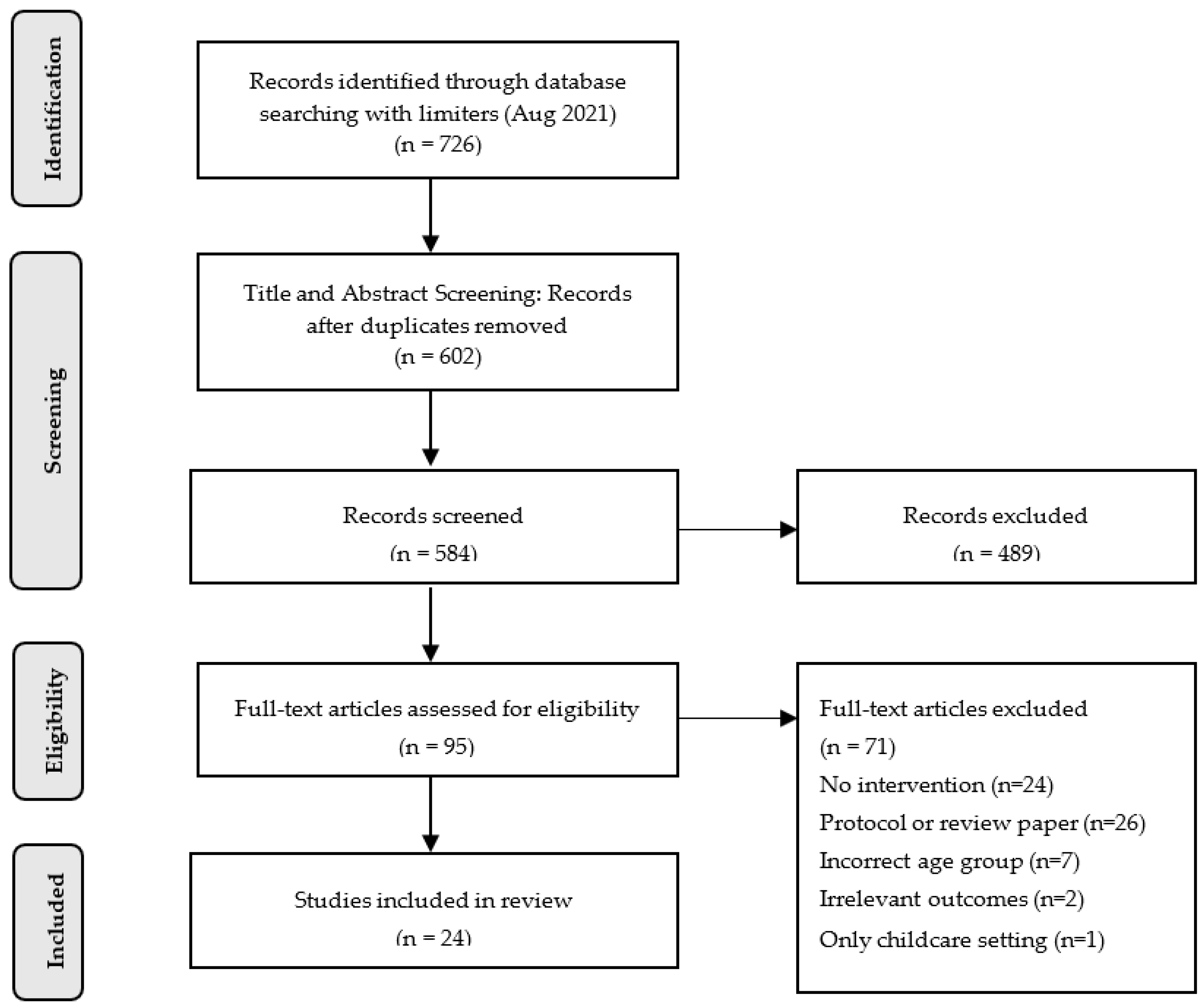
3.1. Study Selection and Characteristics
3.2. Effect Estimates of Studies
3.3. Effects of Home/Family-Based Interventions on Outcomes
3.4. Effects of Community-Based Intervention on Outcomes
3.5. Summary of Identified Recommended Strategies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018 Key findings Data from the National Health and Nutrition Examination Survey. HCHS Data Brief 2017, 360, 1–8. [Google Scholar]
- Lee, O.; Lee, D.-C.; Lee, S.; Kim, Y.S. Associations between physical activity and obesity defined by waist-to-height ratio and body mass index in the Korean population. PLoS ONE 2016, 11, e0158245. [Google Scholar] [CrossRef] [PubMed]
- Ward, Z.J.; Long, M.W.; Resch, S.C.; Giles, C.M.; Cradock, A.L.; Gortmaker, S.L. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N. Engl. J. Med. 2017, 377, 2145–2153. [Google Scholar] [CrossRef] [PubMed]
- Pulgarón, E.R. Childhood Obesity: A Review of Increased Risk for Physical and Psychological Comorbidities. Clin. Ther. 2013, 35, A18–A32. [Google Scholar] [CrossRef] [PubMed]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Screening for Obesity in Children and Adolescents. JAMA 2017, 317, 2417. [Google Scholar] [CrossRef] [PubMed]
- Timmons, B.W.; Leblanc, A.G.; Carson, V.; Connor Gorber, S.; Dillman, C.; Janssen, I.; Kho, M.E.; Spence, J.C.; Stearns, J.A.; Tremblay, M.S. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 773–792. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P. The physical activity levels of preschool-aged children: A systematic review. Early Child. Res. Q. 2008, 23, 547–558. [Google Scholar] [CrossRef]
- McArthur, B.A.; Volkova, V.; Tomopoulos, S.; Madigan, S. Global Prevalence of Meeting Screen Time Guidelines Among Children 5 Years and Younger. JAMA Pediatrics 2022, 176, 373–383. [Google Scholar] [CrossRef]
- Bellman, M.; Byrne, O.; Sege, R. Developmental assessment of children. BMJ 2013, 346, e8687. [Google Scholar] [CrossRef]
- Basman, A.J. Assessment criteria of fundamental movement skills for various age groups: A systematic review. J. Phys. Educ. Sport 2019, 19, 722–732. [Google Scholar]
- Gu, X. Fundamental motor skill, physical activity, and sedentary behavior in socioeconomically disadvantaged kindergarteners. Psychol. Health Med. 2016, 21, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Gu, X.; Zhang, T.; Caçola, P.; Wang, J. Are movement behaviors and fundamental motor skills associated with fitness and fatness in early childhood? Findings from the 2012 NHANES National Youth Fitness Survey. Pediatric Exerc. Sci. 2020, 32, 9–15. [Google Scholar] [CrossRef]
- Ali, A.; McLachlan, C.; Mugridge, O.; McLaughlin, T.; Conlon, C.; Clarke, L. The effect of a 10-week physical activity programme on fundamental movement skills in 3–4-year-old children within early childhood education centres. Children 2021, 8, 440. [Google Scholar] [CrossRef]
- Brian, A.; Goodway, J.D.; Logan, J.A.; Sutherland, S. SKIPing with teachers: An early years motor skill intervention. Phys. Educ. Sport Pedagog. 2017, 22, 270–282. [Google Scholar] [CrossRef]
- Capio, C.M.; Sit, C.H.; Eguia, K.F.; Abernethy, B.; Masters, R.S. Fundamental movement skills training to promote physical activity in children with and without disability: A pilot study. J. Sport Health Sci. 2015, 4, 235–243. [Google Scholar] [CrossRef]
- Jones, R.A.; Riethmuller, A.; Hesketh, K.; Trezise, J.; Batterham, M.; Okely, A.D. Promoting fundamental movement skill development and physical activity in early childhood settings: A cluster randomized controlled trial. Pediatric Exerc. Sci. 2011, 23, 600–615. [Google Scholar] [CrossRef]
- Kipping, R.R.; Howe, L.D.; Jago, R.; Campbell, R.; Wells, S.; Chittleborough, C.R.; Mytton, J.; Noble, S.M.; Peters, T.J.; Lawlor, D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014, 348, g3256. [Google Scholar] [CrossRef] [PubMed]
- Marinšek, M.; Denac, O. The effects of an integrated programme on developing fundamental movement skills and rhythmic abilities in early childhood. Early Child. Educ. J. 2020, 48, 751–758. [Google Scholar]
- Sallis, J.F.; Owen, N.; Fisher, E.B. Ecological Models of Health Behavior. In Health Behavior and Health Education: Theory, Research, and Practice; Jossey-Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Loprinzi, P.D.; Cardinal, B.J.; Loprinzi, K.L.; Lee, H. Benefits and Environmental Determinants of Physical Activity in Children and Adolescents. Obes. Facts 2012, 5, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Copeland, K.A.; Khoury, J.C.; Kalkwarf, H.J. Child care center characteristics associated with preschoolers’ physical activity. Am. J. Prev. Med. 2016, 50, 470–479. [Google Scholar] [CrossRef]
- Henderson, K.E.; Grode, G.M.; O’Connell, M.L.; Schwartz, M.B. Environmental factors associated with physical activity in childcare centers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 43. [Google Scholar] [CrossRef]
- Vanderloo, L.M.; Tucker, P.; Johnson, A.M.; Burke, S.M.; Irwin, J.D. Environmental influences on Preschoolers’ physical activity levels in various early-learning facilities. Res. Q. Exerc. Sport 2015, 86, 360–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, H.; Wen, L.M.; Rissel, C. Associations of Parental Influences with Physical Activity and Screen Time among Young Children: A Systematic Review. J. Obes. 2015, 2015, 546925. [Google Scholar] [CrossRef] [PubMed]
- Brown, H.E.; Atkin, A.J.; Panter, J.; Wong, G.; Chinapaw, M.J.M.; van Sluijs, E.M.F. Family-based interventions to increase physical activity in children: A systematic review, meta-analysis and realist synthesis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2016, 17, 345–360. [Google Scholar] [CrossRef] [PubMed]
- Tonge, K.L.; Jones, R.A.; Okely, A.D. Correlates of children’s objectively measured physical activity and sedentary behavior in early childhood education and care services: A systematic review. Prev. Med. 2016, 89, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Yao, C.A.; Rhodes, R.E. Parental correlates in child and adolescent physical activity: A meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 10. [Google Scholar] [CrossRef]
- Valadi, S.; Gabbard, C. The effect of affordances in the home environment on children’s fine-and gross motor skills. Early Child Dev. Care 2020, 190, 1225–1232. [Google Scholar] [CrossRef]
- Smith, J.D.; Cruden, G.H.; Rojas, L.M.; Van Ryzin, M.; Fu, E.; Davis, M.M.; Landsverk, J.; Brown, C.H. Parenting interventions in pediatric primary care: A systematic review. Pediatrics 2020, 146, e20193548. [Google Scholar] [CrossRef] [PubMed]
- Knowlden, A.P.; Sharma, M. Systematic review of family and home-based interventions targeting paediatric overweight and obesity. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2012, 13, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009, 62, e1–e34. [Google Scholar] [CrossRef] [PubMed]
- Montori, V.M.; Wilczynski, N.L.; Morgan, D.; Haynes, R.B. Optimal search strategies for retrieving systematic reviews from Medline: Analytical survey. BMJ 2005, 330, 68. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.H.; Ciliska, D.; Dobbins, N.; Micucci, S. A process for systematically reveiwing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid. Based Nurs. 2004, 3, 176–184. [Google Scholar] [CrossRef]
- Armijo-Olivo, S.; Stiles, C.R.; Hagen, N.A.; Biondo, P.D.; Cummings, G.G. Assessment of study quality for systematic reviews: A comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: Methodological research. J. Eval. Clin. Pract. 2012, 18, 12–18. [Google Scholar] [CrossRef]
- Crutzen, R. Adding effect sizes to a systematic review on interventions for promoting physical activity among European teenagers. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 29. [Google Scholar] [CrossRef]
- De Craemer, M.; De Decker, E.; Verloigne, M.; De Bourdeaudhuij, I.; Manios, Y.; Cardon, G. The effect of a kindergarten-based, family-involved intervention on objectively measured physical activity in Belgian preschool boys and girls of high and low SES: The ToyBox-study. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 38. [Google Scholar] [CrossRef]
- Laukkanen, A.; Pesola, A.J.; Finni, T.; Sääkslahti, A. Parental Support and Objectively Measured Physical Activity in Children: A Yearlong Cluster-Randomized Controlled Efficacy Trial. Res. Q. Exerc. Sport 2017, 88, 293–306. [Google Scholar] [CrossRef]
- Ray, C.; Figuereido, R.; Vepsäläinen, H.; Lehto, R.; Pajulahti, R.; Skaffari, E.; Sainio, T.; Hiltunen, P.; Lehto, E.; Korkalo, L.; et al. Effects of the Preschool-Based Family-Involving DAGIS Intervention Program on Children’s Energy Balance-Related Behaviors and Self-Regulation Skills: A Clustered Randomized Controlled Trial. Nutrients 2020, 12, 2599. [Google Scholar] [CrossRef] [PubMed]
- Puder, J.J.; Marques-Vidal, P.; Schindler, C.; Zahner, L.; Niederer, I.; Bürgi, F.; Ebenegger, V.; Nydegger, A.; Kriemler, S. Effect of multidimensional lifestyle intervention on fitness and adiposity in predominantly migrant preschool children (Ballabeina): Cluster randomised controlled trial. BMJ 2011, 343, d6195. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Brookes, D.S.K. Effectiveness of a novel digital application to promote fundamental movement skills in 3- to 6-year-old children: A randomized controlled trial. J. Sports Sci. 2021, 39, 453–459. [Google Scholar] [CrossRef]
- Zask, A.; Adams, J.K.; Brooks, L.O.; Hughes, D.F.; Zask, A.; Adams, J.K.; Brooks, L.O.; Hughes, D.F. Tooty Fruity Vegie: An obesity prevention intervention evaluation in Australian preschools. Health Promot. J. Aust. 2012, 23, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Haines, J.; McDonald, J.; O’Brien, A.; Sherry, B.; Bottino, C.J.; Schmidt, M.E.; Taveras, E.M. Healthy Habits, Happy Homes: Randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatrics 2013, 167, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Haines, J.; Douglas, S.; Mirotta, J.A.; O’Kane, C.; Breau, R.; Walton, K.; Krystia, O.; Chamoun, E.; Annis, A.; Darlington, G.A.; et al. Guelph Family Health Study: Pilot study of a home-based obesity prevention intervention. Can. J. Public Health 2018, 109, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Knowlden, A.; Sharma, M. One-Year Efficacy Testing of Enabling Mothers to Prevent Pediatric Obesity Through Web-Based Education and Reciprocal Determinism (EMPOWER) Randomized Control Trial. Health Educ. Behav. Off. Publ. Soc. Public Health Educ. 2016, 43, 94–106. [Google Scholar] [CrossRef]
- Koulouglioti, C.; Cole, R.; McQuillan, B.; Moskow, M.; Kueppers, J.; Pigeon, W. Feasibility of an Individualized, Home-Based Obesity Prevention Program for Preschool-Age Children. Child. Health Care 2013, 42, 134–152. [Google Scholar] [CrossRef]
- Latomme, J.; Cardon, G.; De Bourdeaudhuij, I.; Iotova, V.; Koletzko, B.; Socha, P.; Moreno, L.; Androutsos, O.; Manios, Y.; De Craemer, M. Effect and process evaluation of a kindergarten-based, family-involved intervention with a randomized cluster design on sedentary behaviour in 4- to 6- year old European preschool children: The ToyBox-study. PLoS ONE 2017, 12, e0172730. [Google Scholar] [CrossRef]
- Quattrin, T.; Roemmich, J.N.; Paluch, R.; Yu, J.; Epstein, L.H.; Ecker, M.A. Efficacy of family-based weight control program for preschool children in primary care. Pediatrics 2012, 130, 660–666. [Google Scholar] [CrossRef]
- Stark, L.J.; Clifford, L.M.; Towner, E.K.; Filigno, S.S.; Zion, C.; Bolling, C.; Rausch, J. A pilot randomized controlled trial of a behavioral family-based intervention with and without home visits to decrease obesity in preschoolers. J. Pediatric Psychol. 2014, 39, 1001–1012. [Google Scholar] [CrossRef]
- Taverno Ross, S.E.; Barone Gibbs, B.; Documet, P.I.; Pate, R.R. ANDALE Pittsburgh: Results of a promotora-led, home-based intervention to promote a healthy weight in Latino preschool children. BMC Public Health 2018, 18, 360. [Google Scholar] [CrossRef]
- Tomayko, E.J.; Prince, R.J.; Cronin, K.A.; Adams, A.K. The Healthy Children, Strong Families intervention promotes improvements in nutrition, activity and body weight in American Indian families with young children. Public Health Nutr. 2016, 19, 2850–2859. [Google Scholar] [CrossRef]
- Wen, L.M.; Baur, L.A.; Simpson, J.M.; Rissel, C.; Wardle, K.; Flood, V.M. Effectiveness of home based early intervention on children’s BMI at age 2: Randomised controlled trial. BMJ 2012, 344, e3732. [Google Scholar] [CrossRef]
- Bonvin, A.; Barral, J.; Kakebeeke, T.H.; Kriemler, S.; Longchamp, A.; Schindler, C.; Marques-Vidal, P.; Puder, J.J. Effect of a governmentally-led physical activity program on motor skills in young children attending child care centers: A cluster randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 90. [Google Scholar] [CrossRef]
- Fitzgibbon, M.L.; Stolley, M.R.; Schiffer, L.; Kong, A.; Braunschweig, C.L.; Gomez-Perez, S.L.; Odoms-Young, A.; Van Horn, L.; Christoffel, K.K.; Dyer, A.R. Family-based hip-hop to health: Outcome results. Obesity 2013, 21, 274–283. [Google Scholar] [CrossRef] [Green Version]
- Keita, A.D.; Risica, P.M.; Drenner, K.L.; Adams, I.; Gorham, G.; Gans, K.M. Feasibility and acceptability of an early childhood obesity prevention intervention: Results from the healthy homes, healthy families pilot study. J. Obes. 2014, 2014, 378501. [Google Scholar] [CrossRef]
- Van de Kolk, I.; Gerards, S.M.P.L.; Harms, L.S.E.; Kremers, S.P.J.; Gubbels, J.S. The Effects of a Comprehensive, Integrated Obesity Prevention Intervention Approach (SuperFIT) on Children’s Physical Activity, Sedentary Behavior, and BMI Z-Score. Int. J. Environ. Res. Public Health 2019, 16, 5016. [Google Scholar] [CrossRef]
- Yin, Z.; Ullevig, S.L.; Sosa, E.; Liang, Y.; Olmstead, T.; Howard, J.T.; Errisuriz, V.L.; Estrada, V.M.; Martinez, C.E.; He, M.; et al. Study protocol for a cluster randomized controlled trial to test “¡Míranos! Look at Us, We Are Healthy!”—An early childhood obesity prevention program. BMC Pediatrics 2019, 19, 190. [Google Scholar] [CrossRef]
- Walton, K.; Filion, A.J.; Gross, D.; Morrongiello, B.; Darlington, G.; Randall Simpson, J.; Hou, S.; Haines, J. Parents and Tots Together: Pilot randomized controlled trial of a family-based obesity prevention intervention in Canada. Can. J. Public Health 2015, 106, e555–e562. [Google Scholar] [CrossRef]
- Davison, K.K.; Edmunds, L.S.; Wyker, B.A.; Young, L.M.; Sarfoh, V.S.; Sekhobo, J.P. Feasibility of increasing childhood outdoor play and decreasing television viewing through a family-based intervention in WIC, New York State, 2007–2008. Prev. Chronic Dis. 2011, 8, A54. [Google Scholar]
- Barkin, S.L.; Gesell, S.B.; Po’e, E.K.; Escarfuller, J.; Tempesti, T. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics 2012, 130, 445–456. [Google Scholar]
- Yin, Z.; Parra-Medina, D.; Cordova, A.; He, M.; Trummer, V.; Sosa, E.; Gallion, K.J.; Sintes-Yallen, A.; Huang, Y.; Wu, X.; et al. Míranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child. Obes. 2012, 8, 429–439. [Google Scholar] [CrossRef]
- Engel, A.C.; Broderick, C.R.; Van Doorn, N.; Hardy, L.L.; Parmenter, B.J. Exploring the Relationship Between Fundamental Motor Skill Interventions and Physical Activity Levels in Children: A Systematic Review and Meta-analysis. Sports Med. 2018, 48, 1845–1857. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar]
- Hall, C.M.; Bierman, K.L. Technology-assisted interventions for parents of young children: Emerging practices, current research, and future directions. Early Child. Res. Q. 2015, 33, 21–32. [Google Scholar]
- Ullmann, G.; Kedia, S.K.; Homayouni, R.; Akkus, C.; Schmidt, M.; Klesges, L.M.; Ward, K.D. Memphis FitKids: Implementing a mobile-friendly web-based application to enhance parents’ participation in improving child health. BMC Public Health 2018, 18, 1068. [Google Scholar]
- Heredia, N.I.; Ranjit, N.; Warren, J.L.; Evans, A.E. Association of parental social support with energy balance-related behaviors in low-income and ethnically diverse children: A cross-sectional study. BMC Public Health 2016, 16, 1182. [Google Scholar] [CrossRef]
- Shen, B.; Centeio, E.; Garn, A.; Martin, J.; Kulik, N.; Somers, C.; McCaughtry, N. Parental social support, perceived competence and enjoyment in school physical activity. J. Sport Health Sci. 2018, 7, 346–352. [Google Scholar]
- Gardner, B.; Arden, M.A.; Brown, D.; Eves, F.F.; Green, J.; Hamilton, K.; Hankonen, N.; Inauen, J.; Keller, J.; Kwasnicka, D. Developing habit-based health behaviour change interventions: Twenty-one questions to guide future research. Psychol. Health 2021, 1–23. [Google Scholar]
- Pereira, J.R.; Cliff, D.P.; Sousa-Sá, E.; Zhang, Z.; Santos, R. Prevalence of objectively measured sedentary behavior in early years: Systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2019, 29, 308–328. [Google Scholar]
- Chang, M.; Gu, X. The role of executive function in linking fundamental motor skills and reading proficiency in socioeconomically disadvantaged kindergarteners. Learn. Individ. Differ. 2018, 61, 250–255. [Google Scholar] [CrossRef]
- Gonzalez, S.L.; Alvarez, V.; Nelson, E.L. Do gross and fine motor skills differentially contribute to language outcomes? A systematic review. Front. Psychol. 2019, 10, 2670. [Google Scholar]
- Lee, E.-Y.; Spence, J.C.; Carson, V. Television viewing, reading, physical activity and brain development among young South Korean children. J. Sci. Med. Sport 2017, 20, 672–677. [Google Scholar] [CrossRef]
- Veldman, S.L.C.; Santos, R.; Jones, R.A.; Sousa-Sá, E.; Okely, A.D. Associations between gross motor skills and cognitive development in toddlers. Early Hum. Dev. 2019, 132, 39–44. [Google Scholar] [CrossRef]
- Sim, A.L.; Bowes, L.; Maignant, S.; Magber, S.; Gardner, F. Acceptability and Preliminary Outcomes of a Parenting Intervention for Syrian Refugees. Res. Soc. Work Pract. 2021, 31, 14–25. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| Domain Rating | |||||||
|---|---|---|---|---|---|---|---|
| Articles | Selection Bias | Study Design | Confounders | Blinding | Data Collection Methods | Withdrawals and Dropouts | Global Rating |
| Barkin et al., 2013 | Strong | Strong | Weak | Weak | Moderate | Moderate | Weak |
| Bonvin et al., 2013 | Weak | Strong | Strong | Weak | Strong | Strong | Moderate |
| Davison et al., 2011 | Weak | Weak | Moderate | Moderate | Strong | Weak | Weak |
| De Craemer et al., 2014 | Moderate | Strong | Strong | Weak | Strong | Moderate | Moderate |
| Ftizgibbon et al., 2013 | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Haines et al., 2013 | Weak | Strong | Weak | Weak | Moderate | Strong | Weak |
| Haines et al., 2018 | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Keita et al., 2014 | Weak | Moderate | Weak | Weak | Strong | Moderate | Weak |
| Knowlden & Sharma et al., 2016 | Moderate | Weak | Weak | Weak | Strong | Moderate | Weak |
| Koulouglioti et al., 2013 | Weak | Moderate | Weak | Weak | Strong | Strong | Weak |
| Latomme et al., 2017 | Moderate | Strong | Strong | Weak | Strong | Weak | Weak |
| Laukkanen et al., 2017 | Weak | Strong | Strong | Weak | Strong | Weak | Weak |
| Puder et al., 2011 | Strong | Strong | Strong | Moderate | Strong | Strong | Strong |
| Quattrin et al., 2012 | Strong | Strong | Strong | Moderate | Moderate | Strong | Strong |
| Ray et al., 2020 | Weak | Strong | Strong | Weak | Strong | Strong | Weak |
| Stark et al., 2014 | Weak | Strong | Moderate | Weak | Strong | Moderate | Weak |
| Taverno Ross et al., 2018 | Strong | Moderate | Weak | Weak | Strong | Strong | Weak |
| Tomayko et al., 2016 | Weak | Strong | Weak | Moderate | Weak | Moderate | Weak |
| Trost & Brookes et al., 2021 | Strong | Strong | Weak | Moderate | Strong | Strong | Moderate |
| Van de Kolk et a., 2019 | Weak | Moderate | Strong | Weak | Strong | Moderate | Weak |
| Walton et al., 2015 | Weak | Strong | Strong | Weak | Weak | Strong | Weak |
| Wen et al., 2012 | Strong | Strong | Moderate | Moderate | Strong | Moderate | Moderate |
| Yin et al., 2012 | Strong | Moderate | Strong | Weak | Moderate | Strong | Moderate |
| Zask et al., 2012 | Moderate | Strong | Strong | Weak | Moderate | Strong | Moderate |
| Articles | Outcome Measures Effect Size | |||
|---|---|---|---|---|
| PA | SB/Screen Time | BMI | Motor Skills | |
| Barkin et al., 2013 | - | |||
| Bonvin et al., 2013 | 0.19 | 0.08 | 0 | |
| Davison et al., 2011 | - | - | ||
| De Craemer et al., 2014 | 0.16 | |||
| Fitzgibbon et al., 2013 | 1.24 | 0.20 | ||
| Haines et al., 2018 | 0.65 to 0.64 | −1.46 to 0.17 | −1.30 to −3.54 | |
| Haines et al., 2013 | 0.37 | 0.15 | ||
| Keita et al., 2014 | 0.43 | 0.40 | 0.05 | |
| Knowlden & Sharma et al., 2013 | 0.04 | 0.02 | ||
| Latomme et al., 2017 | 0.11 | |||
| Laukkanen et al., 2017 | 0.10 | 0.21 | ||
| Puder et al., 2011 | 0.01 | 0.26 | 0.06 | |
| Quattrin et al., 2012 | 0.42 | |||
| Ray et al., 2020 | 0.08 | 0.08 | ||
| Stark et al., 2014 | −1.64 to −0.088 | |||
| Taverno Ross et al., 2018 | 0 | 0.03 | 0.04 | |
| Tomayko et al., 2016 | 0.24 | 0.03 | 0.19 | |
| Trost & Brookes, 2021 | 0.06 | 0.61 to 1.1 | ||
| Van de Kolk et al., 2019 | −0.19 to −0.24 | 0.21 to 0.33 | ||
| Walton et al., 2015 | 0.60 | 0.10 | 0.07 | |
| Wen et al., 2012 | - | - | 0.22 | |
| Yin et al., 2012 | 0.02 to 0.12 | 0.69 to 0.80 | ||
| Zask et al., 2012 | 1.70 | 2.33 to 5.15 | ||
| Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Location | N (Age) | Design | Intervention Protocol | PA | SB/Screen Time | BMI | Motor Skills |
| Bonvin et al. (2013) | Switzerland | 648 children (M = 3.3 years) | 9-month RCT |
| X 0 | X 0 | X 0 | |
| De Craemer et al. (2014) | Belgium | 472 children (M = 4.4 years) | 24-week RCD |
| X * | |||
| Fitzgibbon et al. (2013) | United States | 157 children (M = 4.5 years) | 14-week RCT |
| X 0 | X 0 | X 0 | |
| Haines et al. (2018) | Canada | 55 children (M = 3.0 years) | 6-month RCT |
| X 0 | X 0 | X * | |
| Haines et al. (2013) | United States | 111 children (M = 4.1 years) | 6-month RCT |
| X * | X * | ||
| Keita et al. (2014) | United States | 39 children (M = 3.7 years) | 4-month Prospective Design |
| X * (-) | X * | X 0 | |
| Knowlden & Sharma (2016) | United States | 44 children (M = 5.2 years) | 8-week Mixed between- subjects design |
| X 0 | X * | ||
| Koulouglioti et al. (2013) | United States | 11 children (3–5 years old) | 6-week Single group pre-post design |
| X * | |||
| Latomme et al. (2017) | Belgium, Bulgaria, Germany, Greece, Poland, and Spain | 2434 children (M = 4.7 years) | 24-week RCD |
| X * | |||
| Laukkanen et al. (2017) | Finland | 44 children (M = 6.1 years) | 6-month RCT |
| X * | X * | ||
| Puder et al. (2011) | Switzerland | 652 children (M = 5.2 years) | 12-month RCT |
| X 0 | X * | X 0 | X * |
| Quattrin et al. (2012) | United States | 96 children (M = 4.6 years) | 12-week RCT |
| X * | |||
| Ray et al. (2020) | Finland | 802 children (M = 5.1 years) | 4-month RCT |
| X * | X 0 | ||
| Stark et al. (2014) | United States | 18 children (M = 4.6 years) | 6-month RCT |
| X 0 | X * | ||
| Taverno Ross et al. (2018) | United States | 49 children (M = 3.9 years) | 10-week Single group pre-post design |
| X 0 | X * | X * | |
| Tomayko et al. (2016) | United States | 150 children (M = 4.0 years) | 24-month RCT |
| X 0 | X * | X * | |
| Trost & Brookes (2021) | Australia | 34 children (M = 5.3 years) | 8-week RCT |
| X 0 | X * | ||
| Wen et al. (2012) | Australia | 667 children (Range: 2 years) | 24-month RCT |
| X 0 | X * | X * | |
| Zask et al. (2012) | Australia | 560 children (M = 4.5 years) | 10-month RCT |
| X * | X * | ||
| Outcomes | ||||||||
|---|---|---|---|---|---|---|---|---|
| Author | Location | N (Age) | Design | Intervention Protocol | PA | SB/Screen Time | BMI | Motor Skills |
| Barkin et al. (2012) | United States | 106 children (M = 4.1 years) | 12-week RCT |
| X * | |||
| Bonvin et al. (2013) * | Switzerland | 648 children (M = 3.3 years) | 9-month RCT |
| X 0 | X 0 | X 0 | |
| Davison et al. (2011) | United States | 422 children (M = 3.4 years) | 12-month Pre- post measured (nonpaired quasi experimental) |
| X * | X * | ||
| Fitzgibbon et al. (2013) * | United States | 157 children (M = 4.5 years) | 14-week RCT |
| X 0 | X 0 | X 0 | |
| Laukkanen et al. (2017) * | Finland | 44 children (M = 6.1 years) | 6-month RCT |
| X * | X * | X 0 | |
| Puder et al. (2011) * | Switzerland | 652 children (M = 5.2 years) | 12-month RCT |
| X 0 | X * | X 0 | X * |
| Quattrin et al. (2012) * | United States | 96 children (M = 4.6 years) | 12-week RCT |
| X * | |||
| Stark et al. (2014) * | United States | 18 children (M = 4.6 years) | 6-month RCT |
| X 0 | X * | ||
| Trost & Brookes (2021) * | Australia | 34 children (M = 5.3 years) | 8-week RCT |
| X 0 | X * | ||
| Tomayko et al. (2016) * | United States | 150 children (M = 4.0 years) | 24-month RCT |
| X 0 | X * | X * | |
| Van de Kolk et al. (2019) | Netherlands | 191 children (M = 3.1 years) | 3-month Quasi- experimental design |
| X * | X * | X 0 | |
| Walton et al. (2015) | Canada | 48 children (M = 3.0 years) | 9-week RCT |
| X 0 | X 0 | X 0 | |
| Yin et al. (2012) | United States | 384 children (M = 4.1 years) | 18-week Quasi- experimental pretest/posttest design |
| X * | X 0 | X * | X * |
| Zask et al. (2012) * | Australia | 560 children (M = 4.5 years) | 10-month RCT |
| X * | X * | ||
| Target Change Outcome: Physical Activity | |
|---|---|
| Recommended Strategy | Citation |
| Distribute Educational Material: Provide parents with knowledge-based printed (or web-based) materials with information, interactive activities, and suggestions on how to integrate healthy behaviors into home life. | De Craemer et al., 2014; Ray et al., 2020 |
| Direct Contact with Parents: Call parents via telephone to discuss barriers, actions, and goals to enhance PA behaviors. Host individual discussions with parents tailored to their family to identify where and how PA may be increased in their daily life. | Laukkanen et al., 2017 |
| Promote Community Resources: Provide families with information on physical activity opportunities within their neighborhoods with relevant details (i.e., hours of operation, pictures, parking availability) and a community event calendar through their local neighborhood to encourage physical activity participation with peers. | Davison et al., 2011; Van de Kolk et al., 2019 |
| Encourage Community Engagement: Organize group seminars/lectures with parents and families providing education, interactive games, incorporating motivational techniques, and take home activities. | Laukkanen et al., 2017; Van de Kolk et al., 2019 |
| Peer Education: Utilize peer educators (other parents willing to be trained) to deliver presentations and group seminars. | Yin et al., 2012 |
| Target Change Outcome: Sedentary Behavior/Screen Time | |
|---|---|
| Recommended Strategy | Citation |
| Home Visits: Researchers visit the physical homes of families to first observe normal routines/behaviors. After the initial visit, researchers can individually discuss goals with parents and strategize tailored techniques to achieve those goals. Families will also receive culturally sensitive toolkits/materials engrained with knowledge-based content and family activities to do in place of engaging in sedentary behaviors. | Haines et al., 2013; Koulouglioti et al., 2013; Taverno-Ross et al., 2018; Tomayko et al., 2016; Wen et al., 2012 |
| Distribute Educational Material: Parents receive either printed, web-based educational materials and activities highlighting sedentary behaviors/screen time and to reinforce already established goals. Parents may also participate in individualized and educational discussions with the research team. | Haines et al., 2013; Keita et al., 2014; Knowlden & Sharma, 2016; Laukkanen et al., 2017; Puder et al., 2011; Tomayko et al., 2016; Wen et al., 2012 |
| Direct Contact with Parents: Call and text parents to check-in on progress and to reinforce behaviors and goals previously established. During phone calls, incorporate motivational interviewing to promote behavior change. | Haines et al., 2013; Keita et al., 2014 |
| Parent Participation: Parents receive a family exercise video that is conducive for the whole family to participate in. Families also receive a TV monitor that connects to their TVs to restrict screen time. | Keita et al., 2014 |
| Promote Community Resources: Provide families with information on physical activity opportunities within their neighborhoods with relevant details (i.e., hours of operation, pictures, parking availability) and a community event calendar through their local neighborhood to encourage physical activity participation with peers. | Davison et al., 2011; Van de Kolk et al., 2019 |
| Encourage Community Engagement: Schedule parental group sessions targeting encouragement of PA participation, strategies how parents can role model these behaviors, information on TV use, general parenting tips, and demonstrate co-activities that can be reproduced at home. | Laukkanen et al., 2017; Puder et al., 2011; Van de Kolk et al., 2019 |
| Target Change Outcome: BMI/Weight Status | |
|---|---|
| Recommended Strategy | Citation |
| Home Visits: Researchers schedule visits to families’ homes that is incorporates monitoring familial behaviors, setting behavioral goals, monitoring progress, and delivering intervention components (i.e., materials, discussions, activities). | Haines et al., 2013; Haines et al., 2018; Stark et al., 2014; Taverno-Ross et al., 2018; Tomayko et al., 2016; Wen et al., 2012 |
| Distribute Educational Material: Provide families with printed, individualized educational materials or tool kits targeting their specific goals previously established with the researchers along with information and strategies targeting PA and other activities they can incorporate in their daily life. | Haines et al., 2013; Latomme et al., 2017; Puder et al., 2011; Wen et al., 2012; Zask et al., 2012 |
| Direct Contact with Parents: Parents receive tailored behavior change emails, telephone calls, and text messages specific towards check-ins, reinforcement, and encouragement. One-on-one meetings assisting in behavior goal shaping can be scheduled as needed. | Haines et al., 2013; Haines et al., 2018; Quattrin et al., 2012 |
| Encourage Community Engagement: Scheduling group informational sessions focusing on PA promotion, TV use, overall sedentary behavior, FMS promotion, and parenting skills. Parents may also be assigned to social groups throughout the duration of the intervention for enhanced peer support. Children can also participate in group activity sessions with their peers. | Barkin et al., 2012; Puder et al., 2011; Quattrin et al., 2012; Stark et al., 2014; Zask et al., 2012 |
| Peer Education: Utilize peer educators (other parents willing to be trained) to deliver presentations and group seminars. | Yin et al., 2012 |
| Target Change Outcome: Motor Skills | |
|---|---|
| Recommended Strategy | Citation |
| Distributing Educational Material: Parents receive printed and interactive materials pertaining to overall child health promotion. | Puder et al., 2011; Zask et al., 2012 |
| Direct Contact with Parents: Parents download a specific mobile app designed to promote FMS in young children through games and activities, in which parents would receive texts and emails for technological troubleshooting support and to confirm adherence. Parents were also able to share achievements with other family and friends virtually. | Trost & Brookes, 2021 |
| Community Engagement: Schedule group discussions and informational activity sessions about PA and sedentary behavior, and how to teach FMS at home. | Puder et al., 2011; Zask et al., 2012 |
| Peer Education: Utilize peer educators (other parents willing to be trained) to deliver presentations and group seminars. | Yin et al., 2012 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moss, S.; Gu, X. Home- and Community-Based Interventions for Physical Activity and Early Child Development: A Systematic Review of Effective Strategies. Int. J. Environ. Res. Public Health 2022, 19, 11968. https://doi.org/10.3390/ijerph191911968
Moss S, Gu X. Home- and Community-Based Interventions for Physical Activity and Early Child Development: A Systematic Review of Effective Strategies. International Journal of Environmental Research and Public Health. 2022; 19(19):11968. https://doi.org/10.3390/ijerph191911968
Chicago/Turabian StyleMoss, Samantha, and Xiangli Gu. 2022. "Home- and Community-Based Interventions for Physical Activity and Early Child Development: A Systematic Review of Effective Strategies" International Journal of Environmental Research and Public Health 19, no. 19: 11968. https://doi.org/10.3390/ijerph191911968





