Subclinical Hearing Deficits in Noise-Exposed Firefighters
Abstract
:1. Introduction
2. Materials and Method
2.1. Design
2.2. Participants
2.3. Procedures
2.4. Statistical Methods
3. Results
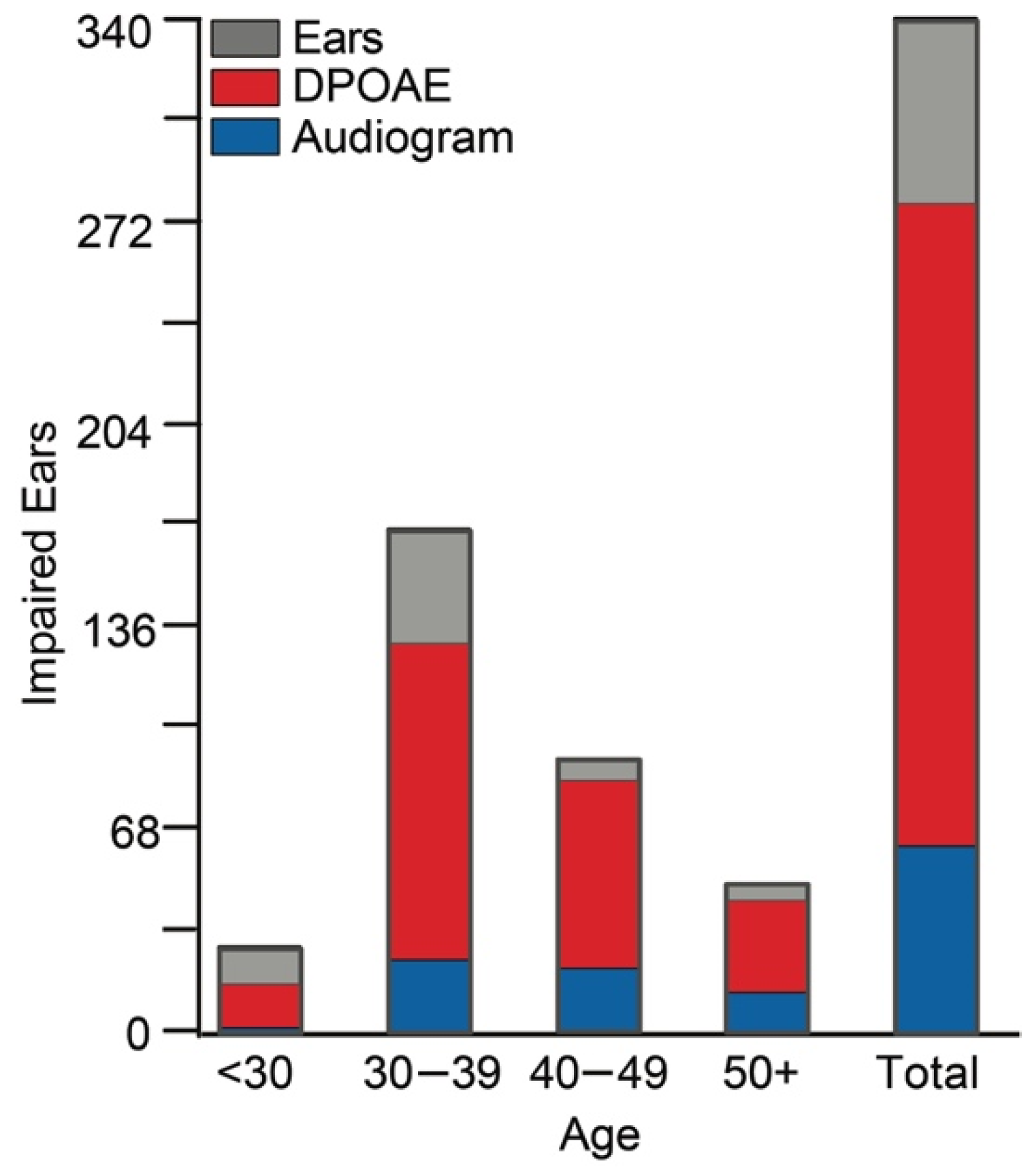
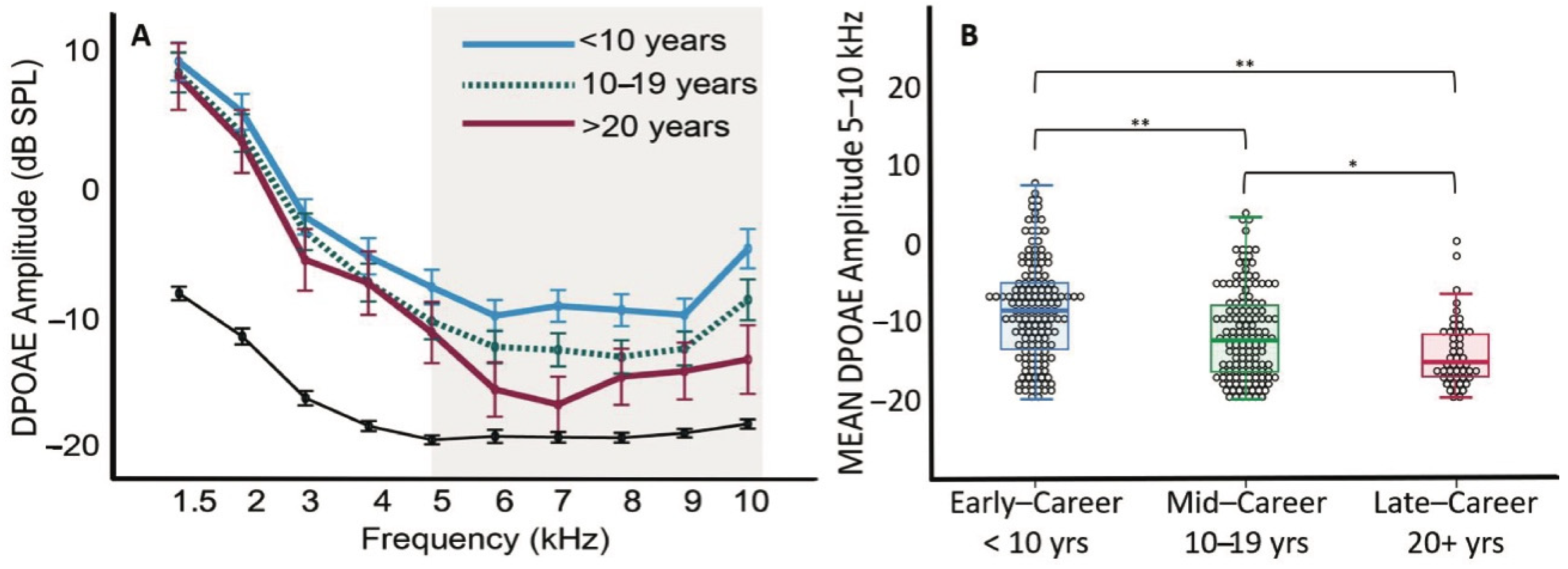
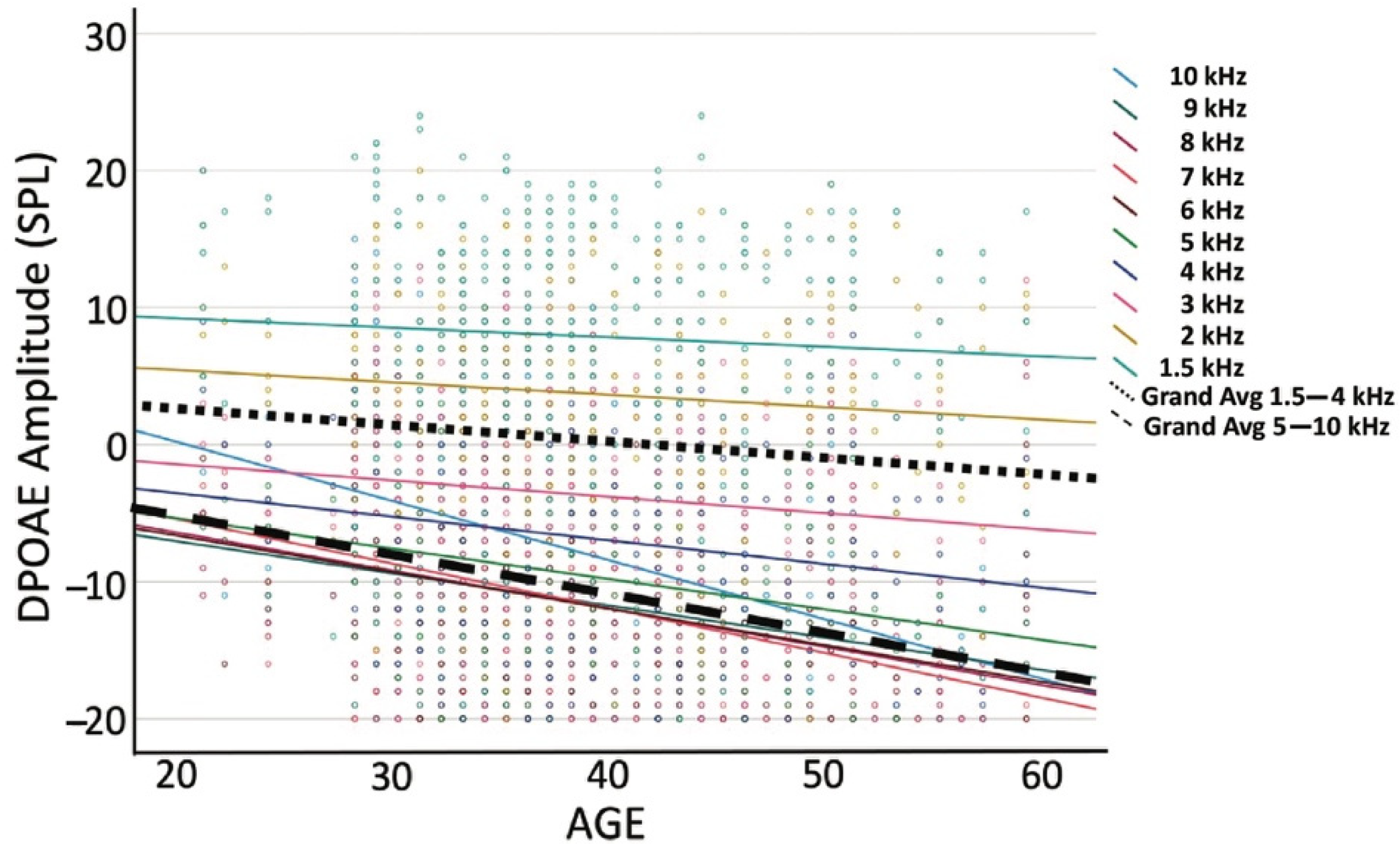
3.1. Functional Assessment Findings
3.2. Reported Outcomes
3.3. Relation between Self-Report Concerns about Hearing Loss and Functional Assessments
4. Discussion
5. Conclusions
- The characterization of DPOAE in a group of relatively young firefighters suggests that firefighters are at risk of NIHL due to their repeated exposure to hazardous noise during their service.
- Findings indicate that noise injury occurs early and is not detected by standard surveillance methods.
- The significant associations between subclinical hearing deficits and number of years in service highlight the importance of early detection measures and the need to address the role of a critical modifiable risk factor, noise overexposure, in mitigating hearing loss and reducing the prevalence of cognitive impairment in aging adults.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Deafness and Hearing Loss. 2019. Available online: http://www.who.int/en/news-room/fact-sheets/detail/deafness-and-hearing-loss (accessed on 1 July 2019).
- Kujawa, S.G.; Liberman, M.C. Acceleration of age-related hearing loss by early noise exposure: Evidence of a misspent youth. J. Neurosci. 2006, 26, 2115–2123. [Google Scholar] [CrossRef] [PubMed]
- Kujawa, S.G.; Liberman, M.C. Translating animal models to human therapeutics in noise-induced and age-related hearing loss. Hear. Res. 2019, 377, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Kujawa, S.G.; Liberman, M.C. Synaptopathy in the noise-exposed and aging cochlea: Primary neural degeneration in acquired sensorineural hearing loss. Hear. Res. 2015, 330, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Kujawa, S.G.; Liberman, M.C. Adding insult to injury: Cochlear nerve degeneration after "temporary" noise-induced hearing loss. J. Neurosci. 2009, 29, 14077–14085. [Google Scholar] [CrossRef]
- Fernandez, K.A.; Jeffers, P.W.; Lall, K.; Liberman, M.C.; Kujawa, S.G. Aging after noise exposure: Acceleration of cochlear synaptopathy in "recovered" ears. J. Neurosci. 2015, 35, 7509–7520. [Google Scholar] [CrossRef]
- Gates, G.A.; Schmid, P.; Kujawa, S.G.; Nam, B.; D’Agostino, R. Longitudinal threshold changes in older men with audiometric notches. Hear. Res. 2000, 141, 220–228. [Google Scholar] [CrossRef]
- Rosenhall, U. The influence of ageing on noise-induced hearing loss. Noise Health 2003, 5, 47–53. [Google Scholar]
- Rabinowitz, P.M. Noise-induced hearing loss. Am. Fam. Physician 2000, 61, 2749–2756, 2759–2760. [Google Scholar]
- Crowson, M.G.; Schulz, K.; Tucci, D.L. Access to Health Care and Hearing Evaluation in US Adults. Ann. Otol. Rhinol. Laryngol. 2016, 125, 716–721. [Google Scholar] [CrossRef]
- Tan, H.E.; Lan, N.S.R.; Knuiman, M.W.; Divitini, M.L.; Swanepoel, D.W.; Hunter, M.; Brennan-Jones, C.G.; Hung, J.; Eikelboom, R.H.; Santa Maria, P.L. Associations between cardiovascular disease and its risk factors with hearing loss-A cross-sectional analysis. Clin. Otolaryngol. 2018, 43, 172–181. [Google Scholar] [CrossRef]
- Lawrence, B.J.; Jayakody, D.M.P.; Bennett, R.J.; Eikelboom, R.H.; Gasson, N.; Friedland, P.L. Hearing Loss and Depression in Older Adults: A Systematic Review and Meta-analysis. Gerontologist 2020, 60, e137–e154. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.B.; Zhang, Y.; Chang, Y.; Ryu, S.; Choi, Y.; Kwon, M.J.; Moon, I.J.; Deal, J.A.; Lin, F.R.; Guallar, E.; et al. Diabetes mellitus and the incidence of hearing loss: A cohort study. Int. J. Epidemiol. 2017, 46, 717–726. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, F.R.; Ferrucci, L.; An, Y.; Goh, J.O.; Doshi, J.; Metter, E.J.; Davatzikos, C.; Kraut, M.A.; Resnick, S.M. Association of hearing impairment with brain volume changes in older adults. Neuroimage 2014, 90, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Ferrucci, L.; Metter, E.J.; An, Y.; Zonderman, A.B.; Resnick, S.M. Hearing loss and cognition in the Baltimore Longitudinal Study of Aging. Neuropsychology 2011, 25, 763–770. [Google Scholar] [CrossRef]
- Lin, F.R.; Metter, E.J.; O’Brien, R.J.; Resnick, S.M.; Zonderman, A.B.; Ferrucci, L. Hearing loss and incident dementia. Arch. Neurol. 2011, 68, 214–220. [Google Scholar] [CrossRef]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; Aboyans, V.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2163–2196. [Google Scholar] [CrossRef]
- NIDCD. Noise-Induced Hearing Loss. 2022. Available online: https://www.nidcd.nih.gov/health/noise-induced-hearing-loss (accessed on 7 January 2022).
- Engdahl, B.; Kemp, D.T. The effect of noise exposure on the details of distortion product otoacoustic emissions in humans. J. Acoust. Soc. Am. 1996, 99, 1573–1587. [Google Scholar] [CrossRef]
- Attias, J.; Bresloff, I. Noise induced temporary otoacoustic emission shifts. J. Basic. Clin. Physiol. Pharmacol. 1996, 7, 221–233. [Google Scholar] [CrossRef]
- Attias, J.; Bresloff, I.; Reshef, I.; Horowitz, G.; Furman, V. Evaluating noise induced hearing loss with distortion product otoacoustic emissions. Br. J. Audiol. 1998, 32, 39–46. [Google Scholar] [CrossRef]
- Attias, J.; Furst, M.; Furman, V.; Reshef, I.; Horowitz, G.; Bresloff, I. Noise-induced otoacoustic emission loss with or without hearing loss. Ear Hear. 1995, 16, 612–618. [Google Scholar] [CrossRef]
- Lonsbury-Martin, B.L.; Whitehead, M.L.; Martin, G.K. Distortion-product otoacoustic emissions in normal and impaired ears: Insight into generation processes. Prog. Brain Res. 1993, 97, 77–90. [Google Scholar] [CrossRef] [PubMed]
- Marshall, L.; Lapsley Miller, J.A.; Heller, L.M.; Wolgemuth, K.S.; Hughes, L.M.; Smith, S.D.; Kopke, R.D. Detecting incipient inner-ear damage from impulse noise with otoacoustic emissions. J. Acoust. Soc. Am. 2009, 125, 995–1013. [Google Scholar] [CrossRef] [Green Version]
- Seixas, N.S.; Goldman, B.; Sheppard, L.; Neitzel, R.; Norton, S.; Kujawa, S.G. Prospective noise induced changes to hearing among construction industry apprentices. Occup. Environ. Med. 2005, 62, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Lapsley Miller, J.A.; Marshall, L.; Heller, L.M.; Hughes, L.M. Low-level otoacoustic emissions may predict susceptibility to noise-induced hearing loss. J. Acoust. Soc. Am. 2006, 120, 280–296. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.E.; Holt, A.G.; Altschuler, R.A.; Cacace, A.T.; Hall, C.D.; Murnane, O.D.; King, W.M.; Akin, F.W. Effects of Noise Exposure on the Vestibular System: A Systematic Review. Front. Neurol. 2020, 11, 593919. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.M.; Perez, C.F.; Hoffer, M.E. The implications of physical injury on otovestibular and cognitive symptomatology following blast exposure. Otolaryngol. Head Neck Surg. 2014, 150, 437–440. [Google Scholar] [CrossRef]
- Lien, S.; Dickman, J.D. Vestibular Injury After Low-Intensity Blast Exposure. Front. Neurol. 2018, 9, 297. [Google Scholar] [CrossRef]
- Stewart, C.E.; Kanicki, A.C.; Bauer, D.S.; Altschuler, R.A.; King, W.M. Exposure to Intense Noise Causes Vestibular Loss. Mil. Med. 2020, 185 (Suppl. S1), 454–461. [Google Scholar] [CrossRef]
- Wang, Y.P.; Young, Y.H. Vestibular-evoked myogenic potentials in chronic noise-induced hearing loss. Otolaryngol. Head Neck Surg. 2007, 137, 607–611. [Google Scholar] [CrossRef]
- Akin, F.W.; Murnane, O.D.; Tampas, J.W.; Clinard, C.; Byrd, S.; Kelly, J.K. The effect of noise exposure on the cervical vestibular evoked myogenic potential. Ear Hear. 2012, 33, 458–465. [Google Scholar] [CrossRef]
- Asakura, S.; Kamogashira, T. Sudden bilateral hearing loss after vestibular-evoked myogenic potentials. Clin. Case Rep. 2021, 9, e05025. [Google Scholar] [CrossRef] [PubMed]
- Dlugaiczyk, J. Ocular Vestibular Evoked Myogenic Potentials: Where Are We Now? Otol. Neurotol. 2017, 38, e513–e521. [Google Scholar] [CrossRef] [PubMed]
- Hong, O.; Samo, D.; Hulea, R.; Eakin, B. Perception and attitudes of firefighters on noise exposure and hearing loss. J. Occup. Environ. Hyg. 2008, 5, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Broyles, G.; Kardous, C.A.; Shaw, P.B.; Krieg, E.F. Noise exposures and perceptions of hearing conservation programs among wildland firefighters. J. Occup. Environ. Hyg. 2019, 16, 775–784. [Google Scholar] [CrossRef]
- Ide, C.W. Hearing losses in wholetime firefighters occurring early in their careers. Occup. Med. 2011, 61, 509–511. [Google Scholar] [CrossRef]
- Kales, S.N.; Freyman, R.L.; Hill, J.M.; Polyhronopoulos, G.N.; Aldrich, J.M.; Christiani, D.C. Firefighters’ hearing: A comparison with population databases from the International Standards Organization. J. Occup. Environ. Med. 2001, 43, 650–656. [Google Scholar] [CrossRef]
- Pepe, P.E.; Jerger, J.; Miller, R.H.; Jerger, S. Accelerated hearing loss in urban emergency medical services firefighters. Ann. Emerg. Med. 1985, 14, 438–442. [Google Scholar] [CrossRef]
- NIOSH. Criteria for a Recommended Standard: Occupational Noise Exposure, Revised Criteria. In National Institute for Occupational Safety and Health 1998; NIOSH: Cincinnati, OH, USA, 1998; pp. 98–126. [Google Scholar]
- Hong, O.; Chin, D.L.; Ronis, D.L. Predictors of hearing protection behavior among firefighters in the United States. Int. J. Behav. Med. 2013, 20, 121–130. [Google Scholar] [CrossRef]
- Millet, B.; Harris, K.; Rajguru, S.; Snapp, H. Noise exposure and hearing health among US Firefighters. Health Saf. Work. 2022, 13, S281. [Google Scholar] [CrossRef]
- Snapp, H.A.; Coto, J.; Solle, N.; Khan, U.; Millet, B.; Rajguru, S.M. Risk propensity as a risk factor for noise induced hearing loss in the general population. Int. J. Audiol. 2022; in press. [Google Scholar] [CrossRef]
- ANSI. American National Standards Specification for Audiometers; American National Standards Institute: New York, NY, USA, 1999. [Google Scholar]
- Lee, J.; Kim, J. The maximum permissible ambient noise and frequency-specific averaging time on the measurement of distortion product otoacoustic emissions. Audiology 1999, 38, 19–23. [Google Scholar] [CrossRef]
- Carhart, R.; Jerger, J. Preferred Methods for Clinical Determination of Pure-Tone Thresholds. J. Speech Hear. Res. 1959, 24, 330–345. [Google Scholar] [CrossRef]
- Stevens, G.; Flaxman, S.; Brunskill, E.; Mascarenhas, M.; Mathers, C.D.; Finucane, M.; Global Burden of Disease Hearing Loss Expert Group. Global and regional hearing impairment prevalence: An analysis of 42 studies in 29 countries. Eur. J. Public Health 2013, 23, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Lonsbury-Martin, B.L.; Cutler, W.M.; Martin, G.K. Evidence for the influence of aging on distortion-product otoacoustic emissions in humans. J. Acoust. Soc. Am. 1991, 89, 1749–1759. [Google Scholar] [CrossRef]
- Abdala, C.; Visser-Dumont, L. Distortion Product Otoacoustic Emissions: A Tool for Hearing Assessment and Scientific Study. Volta Rev. 2001, 103, 281–302. [Google Scholar] [PubMed]
- Wagner, W.; Heppelmann, G.; Vonthein, R.; Zenner, H.P. Test-retest repeatability of distortion product otoacoustic emissions. Ear Hear. 2008, 29, 378–391. [Google Scholar] [CrossRef] [PubMed]
- Gorga, M.P.; Neely, S.T.; Dorn, P.A. Distortion product otoacoustic emission test performance for a priori criteria and for multifrequency audiometric standards. Ear Hear. 1999, 20, 345–362. [Google Scholar] [CrossRef]
- Uchida, Y.; Ando, F.; Shimokata, H.; Sugiura, S.; Ueda, H.; Nakashima, T. The effects of aging on distortion-product otoacoustic emissions in adults with normal hearing. Ear Hear. 2008, 29, 176–184. [Google Scholar] [CrossRef]
- Abdala, C.; Dhar, S. Maturation and aging of the human cochlea: A view through the DPOAE looking glass. J. Assoc. Res. Otolaryngol. 2012, 13, 403–421. [Google Scholar] [CrossRef]
- Henley, C.M.; Weatherly, R.A.; Martin, G.K.; Lonsbury-Martin, B. Sensitive developmental periods for kanamycin ototoxic effects on distortion-product otoacoustic emissions. Hear. Res. 1996, 98, 93–103. [Google Scholar] [CrossRef]
- Kapoor, N.; Mani, K.V.; Shukla, M. Distortion product oto-acoustic emission: A superior tool for hearing assessment than pure tone audiometry. Noise Health 2019, 21, 164–168. [Google Scholar] [CrossRef]
- Helleman, H.W.; Eising, H.; Limpens, J.; Dreschler, W.A. Otoacoustic emissions versus audiometry in monitoring hearing loss after long-term noise exposure—A systematic review. Scand. J. Work Environ. Health 2018, 44, 585–600. [Google Scholar] [CrossRef] [PubMed]
- Hunter, L.L.; Monson, B.B.; Moore, D.R.; Dhar, S.; Wright, B.A.; Munro, K.J.; Zadeh, L.M.; Blankenship, C.M.; Stiepan, S.M.; Siegel, J.H. Extended high frequency hearing and speech perception implications in adults and children. Hear. Res. 2020, 397, 107922. [Google Scholar] [CrossRef] [PubMed]
- Attias, J.; Horovitz, G.; El-Hatib, N.; Nageris, B. Detection and Clinical Diagnosis of Noise-Induced Hearing Loss by Otoacoustic Emissions. Noise Health 2001, 3, 19–31. [Google Scholar] [PubMed]
- Baradarnfar, M.H.; Karamifar, K.; Mehrparvar, A.H.; Mollasadeghi, A.; Gharavi, M.; Karimi, G.; Vahidy, M.R.; Baradarnfar, A.; Mostaghaci, M. Amplitude changes in otoacoustic emissions after exposure to industrial noise. Noise Health 2012, 14, 28–31. [Google Scholar] [CrossRef]
- Attias, J.; Karawani, H.; Shemesh, R.; Nageris, B. Predicting hearing thresholds in occupational noise-induced hearing loss by auditory steady state responses. Ear Hear. 2014, 35, 330–338. [Google Scholar] [CrossRef]
- Prasher, D.; Sulkowski, W. The role of otoacoustic emissions in screening and evaluation of noise damage. Int. J. Occup. Med. Environ. Health 1999, 12, 183–192. [Google Scholar]
- Seixas, N.S.; Kujawa, S.G.; Norton, S.; Sheppard, L.; Neitzel, R.; Slee, A. Predictors of hearing threshold levels and distortion product otoacoustic emissions among noise exposed young adults. Occup. Environ. Med. 2004, 61, 899–907. [Google Scholar] [CrossRef]
- Mirza, R.; Kirchner, D.B.; Dobie, R.A.; Crawford, J. Occupational Noise-Induced Hearing Loss. J. Occup. Environ. Med. 2018, 60, e498–e501. [Google Scholar] [CrossRef]
- Brown, M.N.; Char, R.; Henry, S.O.; Tanigawa, J.; Yasui, S. The effect of firefighter personal protective equipment on static and dynamic balance. Ergonomics 2019, 62, 1193–1201. [Google Scholar] [CrossRef]
- Kim, H.D.; An, Y.S.; Kim, D.H.; Jeong, K.S.; Ahn, Y.S. An overview of compensated work-related injuries among Korean firefighters from 2010 to 2015. Ann. Occup. Environ. Med. 2018, 30, 57. [Google Scholar] [CrossRef]
- Phelps, S.M.; Drew-Nord, D.C.; Neitzel, R.L.; Wallhagen, M.I.; Bates, M.N.; Hong, O.S. Characteristics and Predictors of Occupational Injury Among Career Firefighters. Workplace Health Saf. 2018, 66, 291–301. [Google Scholar] [CrossRef] [PubMed]
- Krishnamurti, S. Sensorineural hearing loss associated with occupational noise exposure: Effects of age-corrections. Int. J. Environ. Res. Public Health 2009, 6, 889–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prince, M.M. Distribution of risk factors for hearing loss: Implications for evaluating risk of occupational noise-induced hearing loss. J. Acoust. Soc. Am. 2002, 112, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Angara, P.; Tsang, D.C.; Hoffer, M.E.; Snapp, H.A. Self-Perceived Hearing Status Creates an Unrealized Barrier to Hearing Healthcare Utilization. Laryngoscope 2020, 131, E289–E295. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, C.; Chen, G.; Hu, B.H.; Chi, L.; Li, M.; Zheng, G.; Bielefeld, E.C.; Jamesdaniel, S.; Coling, D.; Henderson, D. The effects of acoustic environment after traumatic noise exposure on hearing and outer hair cells. Hear. Res. 2009, 250, 10–18. [Google Scholar] [CrossRef]
- Wang, J.; Puel, J.L. Presbycusis: An Update on Cochlear Mechanisms and Therapies. J. Clin. Med. 2020, 9, 218. [Google Scholar] [CrossRef]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]

| Variable | Mean | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| 1. Ringing/buzzing ITE | 1.71 | 0.965 | ||||
| 2. Muffled hearing AEHN | 1.65 | 0.830 | 0.419 * | |||
| 3. Changes in hearing AEHN | 1.69 | 0.823 | 0.211 * | 0.31 * | ||
| 4. Ringing or buzzing ITE AEHN | 1.74 | 0.868 | 0.284 * | 0.334 * | 0.784 * | |
| 5. DPOAE amplitude 5–10 kHz | −10.71 | 6.176 | −0.095 | −0.057 | −0.085 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Snapp, H.A.; Schaefer Solle, N.; Millet, B.; Rajguru, S.M. Subclinical Hearing Deficits in Noise-Exposed Firefighters. Int. J. Environ. Res. Public Health 2022, 19, 11028. https://doi.org/10.3390/ijerph191711028
Snapp HA, Schaefer Solle N, Millet B, Rajguru SM. Subclinical Hearing Deficits in Noise-Exposed Firefighters. International Journal of Environmental Research and Public Health. 2022; 19(17):11028. https://doi.org/10.3390/ijerph191711028
Chicago/Turabian StyleSnapp, Hillary A., Natasha Schaefer Solle, Barbara Millet, and Suhrud M. Rajguru. 2022. "Subclinical Hearing Deficits in Noise-Exposed Firefighters" International Journal of Environmental Research and Public Health 19, no. 17: 11028. https://doi.org/10.3390/ijerph191711028
APA StyleSnapp, H. A., Schaefer Solle, N., Millet, B., & Rajguru, S. M. (2022). Subclinical Hearing Deficits in Noise-Exposed Firefighters. International Journal of Environmental Research and Public Health, 19(17), 11028. https://doi.org/10.3390/ijerph191711028






