Ageing and Long-Term Informal Care: The Reality of Two Countries in Europe: Denmark and Portugal
Abstract
1. Introduction
- (a)
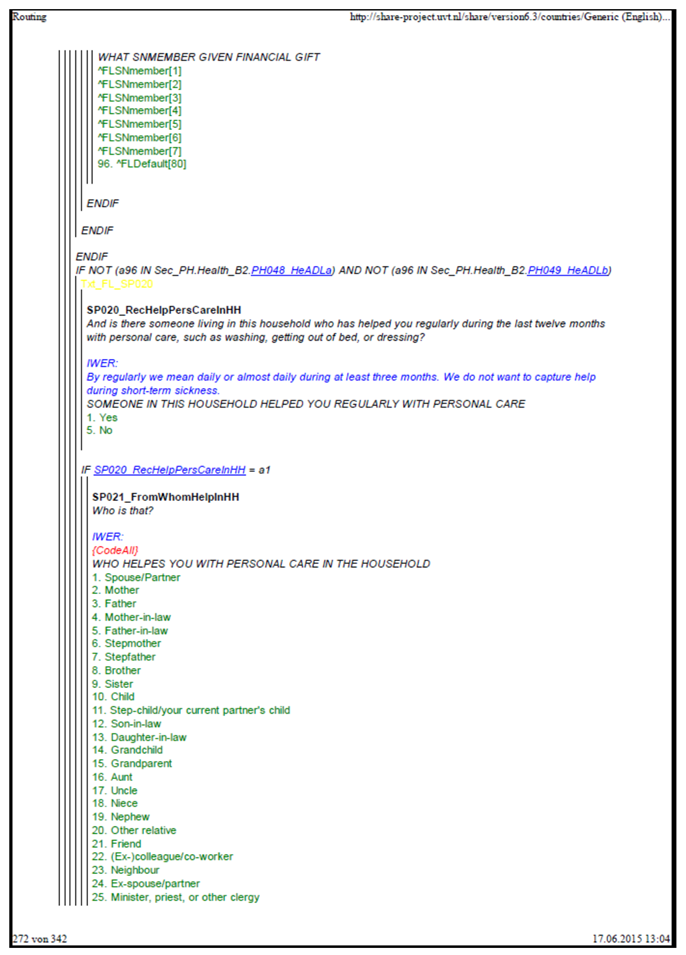
- How is long-term informal care received by older people in both countries, concerning personal care by informal caregivers who are part of their household?
- (b)
- How is long-term informal care received by older people in both countries, concerning personal care by informal caregivers who do not live with them?
2. Materials and Methods
2.1. Sample and Data
2.2. Measures of Variables
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic, Economic, and Health Participants’ Characteristics
3.2. Long-Term Informal Care Characteristics Received by Older People Relative to Personal Care
3.3. Ability of Older People to Receive Long-Term Informal Care, Related to Personal Care
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


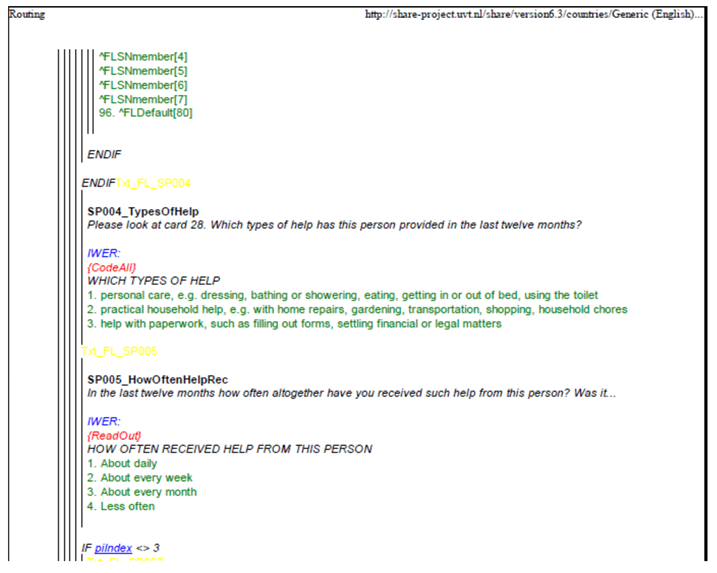
Appendix B
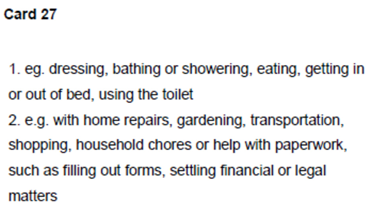
- “Personal care: e.g., dressing, bathing or showering, eating, getting in or out of bed, using the toilet”.
- For example, with gardening, transportation, shopping, household chores or help with paperwork, home repairs, such as filling out forms, and the settling of financial or legal matters.
Appendix C
References
- OECD. Health at a Glance 2019: OECD Indicators; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- European Commission; Directorate-General for Employment; Social Affairs and Inclusion. Study on Exploring the Incidence and Costs of Long-Term Informal Care in the EU; Publications Office of the European Union: Luxembourg, 2021. Available online: https://data.europa.eu/doi/10.2767/06382 (accessed on 25 January 2022).
- European Commission; Directorate-General for Research and Innovation. Population Ageing in Europe: Facts, Implications and Policies: Outcomes of EU-Funded Research; Publications Office: Luxembourg, 2014. [CrossRef]
- Spasova, S.; Baeten, R.; Coster, S.; Ghailani, D.; Peña-Casas, R.; Vanhercke, B. Challenges in Long-Term Care in Europe. A Study of National Policies; European Social Policy Network (ESPN), European Commission: Brussels, Belgium, 2018. [Google Scholar]
- do Rosário Oliveira Martins, M.; Rodrigues, I.; Rodrigues, T. Projecting Health Outcomes for Portuguese Ageing Population: Challenges and Opportunities. Health 2014, 6, 1874–1882. [Google Scholar] [CrossRef][Green Version]
- INE. Indicadores Sociais 2010; Instituto Nacional de Estatistica IP: Lisboa, Portugal, 2011.
- Colombo, F.; Llena-Nozal, A.; Mercier, J.; Tjadens, F. Help Wanted? Providing and Paying for Long-Term Care; OECD Health Policies Studies, OECD Publishing: Paris, France, 2011. [Google Scholar] [CrossRef]
- OECD/European Observatory on Health Systems and Policies. Denmark: Country Health Profile 2021; State of Health in the EU, OECD Publishing: Paris, France, 2021. [Google Scholar] [CrossRef]
- Barbosa, F.; Voss, G.; Delerue Matos, A. Health impact of providing informal care in Portugal. BMC Geriatr. 2020, 20, 440. [Google Scholar] [CrossRef] [PubMed]
- Entidade Reguladora da Saúde. Acesso, Qualidade e Concorrência nos Cuidados Continuados e Paliativos. 2015. Available online: https://www.ers.pt/uploads/writer_file/document/1647/ERS_-_Estudo_Cuidados_Continuados_-_vers_o_final.pdf (accessed on 25 October 2021).
- Barbosa, F.; Matos, A.D. Informal support in Portugal by individuals aged 50+. Eur. J. Ageing. 2014, 11, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Rudkjøbing, A.; Olejaz, M.; Birk, H.O.; Nielsen, A.J.; Hernández-Quevedo, C.; Krasnik, A. Integrated care: A Danish perspective. BMJ 2012, 345, e4451. [Google Scholar] [CrossRef] [PubMed]
- Solipaca, A.; Iezzi, D.F.; Farelli, V.; Damiani, G.; Anselmi, A.; Ricciardi, W.; Iezzi, D.F.; Ricciardi, W. Patterns of Long Term Care in 29 European countries: Evidence from an exploratory study. BMC Health Serv. Res. 2011, 11, 316. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Country Case Study on the Integrated Delivery of Long-Term Care: Denmark; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2019; Available online: https://apps.who.int/iris/handle/10665/352847 (accessed on 1 November 2021).
- World Health Organization; Regional Office for Europe. Country Case Study on the Integrated Delivery of Long-Term Care: Portugal; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2020; Available online: https://apps.who.int/iris/handle/10665/352857 (accessed on 1 November 2021).
- European Commission; Directorate-General for Employment; Social Affairs and Inclusion. Long-Term Care Report: Trends, Challenges and Opportunities in an Ageing Society. Volume II, Country Profiles; Publications Office: Luxembourg, 2021. Available online: https://data.europa.eu/doi/10.2767/183997 (accessed on 25 January 2022).
- Kent, E.E.; Ornstein, K.A.; Dionne-Odom, J.N. The Family Caregiving Crisis Meets an Actual Pandemic. J. Pain Symptom Manag. 2020, 60, e66–e69. [Google Scholar] [CrossRef]
- Budnick, A.; Hering, C.; Eggert, S.; Teubner, C.; Suhr, R.; Kuhlmey, A. Informal caregivers during the COVID-19 pandemic perceive additional burden: Findings from an ad-hoc survey in Germany. BMC Health Serv. Res. 2021, 21, 353. [Google Scholar] [CrossRef]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Schaan, B.; Stuck, S.; Zuber, S.; SHARE Central Coordination Team. Data Resource Profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef]
- SHARE: Survey of Health, Ageing and Retirement in Europe. Available online: http://www.share-project.org/organisation/share-eric.html (accessed on 24 October 2021).
- Malter, F.; Börsch-Supan, A. (Eds.) SHARE Wave 6: Panel Innovations and Collecting Dried Blood Spots; MEA, Max Planck Institute for Social Law and Social Policy: Munich, Germany, 2017. [Google Scholar]
- Börsch-Supan, A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 6. Release Version: 6.1.1. SHARE-ERIC. Data Set. 2018. Available online: https://doi.org/10.6103/SHARE.w6.611 (accessed on 24 October 2021). [CrossRef]
- Bergmann, M.; Kneip, T.; De Luca, G.; Scherpenzeel, A. Survey Participation in the Survey of Health, Ageing and Retirement in Europe (SHARE), Wave 1-7. Based on Release 7.0.0; SHARE Working Paper Series (41-2019); Munich Center for the Economics of Aging (MEA): Munich, Germany, 2019. [Google Scholar]
- Malter, F.; Börsch-Supan, A. SHARE Compliance Profiles—Wave 6; Munich Center for the Economics of Aging: Munich, Germany, 2016. [Google Scholar]
- SHARE. Questionnaires Wave 6. Available online: http://www.share-project.org/data-documentation/questionnaires/questionnaire-wave-6.html (accessed on 24 October 2021).
- Eurostat. Ageing Europe- Looking at the Lives of Older People in the EU; Eurostat: Brussels, Belgium, 2019. [Google Scholar] [CrossRef]
- Mehrbrodt, T.; Gruber, S.; Wagner, M. SHARE: Scales and Multi-Item Indicators; Max Planck Institute for Social Law and Social Policy: Munich, Germany, 2017. [Google Scholar]
- Marôco, J. Análise Estatística com o SPSS Statistics, 7th ed.; ReportNumber: Pêro Pinheiro, Portugal, 2018. [Google Scholar]
- Verbakel, E.; Tamlagsronning, S.; Winstone, L.; Fjaer, E.L.; Eikemo, T.A. Informal care in Europe: Findings from the European Social Survey (2014) special module on the social determinants of health. Eur. J. Public Health 2017, 27, 90–95. [Google Scholar] [CrossRef]
- Pego, M.A.; Nunes, C. Aging, Disability, and Informal Caregivers: A Cross-sectional Study in Portugal. Front Med. 2018, 4, 255. [Google Scholar] [CrossRef]
- INE. População Residente com 15 e Mais anos de Idade que Presta Cuidados Informais [Residents 15 Years or Older Providing Informal Care]; INE: Lisbon, Portugal, 2019.
- Dixe, M.d.A.C.R.; da Conceição Teixeira, L.F.; Areosa, T.J.T.C.C.; Frontini, R.C.; de Jesus Almeida Peralta, T.; Querido, A.I.F. Needs and skills of informal caregivers to care for a dependent person: A cross-sectional study. BMC Geriatr. 2019, 19, 255. [Google Scholar] [CrossRef]
- Ciccarelli, N.; Van Soest, A. Informal Caregiving, Employment Status and Work Hours of the 50+ Population in Europe. Economist 2018, 166, 363–396. [Google Scholar] [CrossRef] [PubMed]
- Gaertner, B.; Busch, M.A.; Scheidt-Nave, C.; Fuchs, J. Limitations in activities of daily living in old age in Germany and the EU—Results from the European Health Interview Survey (EHIS) 2. J. Health Monit. 2019, 4, 48–56, Correction in J. Health Monit. 2020, 4, 56. [Google Scholar] [CrossRef]
- Verbakel, E. How to understand informal caregiving patterns in Europe? The role of formal long-term care provisions and family care norms. Scand. J. Public Health 2018, 46, 436–447. [Google Scholar] [CrossRef]
- Muir, T. Measuring social protection for long-tre. In OECD Health Working Papers; No. 93; OECD Publishing: Paris, France, 2017. [Google Scholar] [CrossRef]
- de Labra, C.; Millán-Calenti, J.C.; Buján, A.; Núñez-Naveira, L.; Jensen, A.M.; Peersen, M.C.; Mojs, E.; Samborski, W.; Maseda, A. Predictors of caregiving satisfaction in informal caregivers of people with dementia. Arch. Gerontol. Geriatr. 2015, 60, 380–388. [Google Scholar] [CrossRef]
- Solé-Auró, A.; Crimmins, E.M. Who cares? A comparison of informal and formal care provision in Spain, England and the USA. Ageing Soc. 2014, 34, 495–517. [Google Scholar] [CrossRef]
- Dahlberg, L.; McKee, K.J. Living on the Edge: Social exclusion and the receipt of informal care in older people. J. Aging Res. 2016, 2016, 6373101. [Google Scholar] [CrossRef] [PubMed]
- Ulmanen, P.; Szebehely, M. From the state to the family or to the market? Consequences of reduced residential elder care in Sweden. Int. J. Soc. Welf. 2015, 24, 81–92. [Google Scholar] [CrossRef]
- Verhaak, P.F.; Dekker, J.H.; de Waal, M.W.; van Marwijk, H.W.; Comijs, H.C. Depression, disability and somatic diseases among elderly. J. Affect. Disord. 2014, 167, 187–191. [Google Scholar] [CrossRef]
- Astudillo, G.C. Depresión como predictor de discapacidad en adultos mayores. Rev. la Univ. Ind. Santander. Salud. 2017, 49, 438–449. [Google Scholar] [CrossRef][Green Version]
- Johnsen, N.F.; Davidsen, M.; Michelsen, S.I.; Juel, K. Health profile for Danish adults with activity limitation: A cross-sectional study. BMC Public Health 2017, 18, 46. [Google Scholar] [CrossRef] [PubMed][Green Version]
- United Nations General Assembly. Global Indicator Framework for the Sustainable Development Goals and targets of the 2030 Agenda for Sustainable Development; Work of the Statistical Commission pertaining to the 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2020; pp. 1–21. Available online: https://unstats.un.org/sdgs/indicators/indicators-list/ (accessed on 12 February 2022).
- Diaz, T.; Strong, K.L.; Cao, B.; Guthold, R.; Moran, A.C.; Moller, A.B.; Requejo, J.; Sadana, R.; Thiyagarajan, J.A.; Adebayo, E.; et al. A call for standardised age-disaggregated health data. Lancet Healthy Longev. 2021, 2, e436–e443, Erratum in Lancet Healthy Longev. 2021, 2, e458. [Google Scholar] [CrossRef]
- Todd, O.M.; Burton, J.K.; Dodds, R.M.; Hollinghurst, J.; Lyons, R.A.; Quinn, T.J.; Schneider, A.; Walesby, K.E.; Wilkinson, C.; Conroy, S.; et al. New horizons in the use of routine data for ageing research. Age Ageing. 2020, 49, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Câmara, G.; Arriaga, M.T.D.; Nogueira, P.; Miguel, J.P. Active and Healthy Aging After COVID-19 Pandemic in Portugal and Other European Countries: Time to Rethink Strategies and Foster Action. Front. Public Health 2019, 9, 700279. [Google Scholar] [CrossRef]
| Variables | Categories |
|---|---|
| Older people Age Age class | Years 65–69; 70–74; 75–79; 80–84; 85–89; ≥90 (years) |
| Gender | Female; male |
| Marital status | Married and living together with a spouse; registered partnership; married, separated from a spouse a; never married a; divorced a; widowed a |
| Educational level (Isced-97) | None a; code-1: primary education; code-2: secondary education a; code-3: upper secondary education; code-4: post-secondary education/non-tertiary education a; code-5: the first stage of tertiary education; code-6: the second stage of tertiary education a |
| Annual household income | Low (<14,844.36 €); medium (≥14,844.36 € to <29,236.09 €); high (≥29,236.09 €) |
| Country | Denmark; Portugal |
| Chronic diseases | Less than two; two or more |
| Depression | Not depressed; depressed |
| Limitation in ADLs | No limitations; one or more than one limitation |
| Limitation in IADLs | No limitations; one or more than one limitation |
| Long-term informal care received from non-household caregivers | |
| Occurrence | Yes; no |
| Kinship of informal caregiver | Partner/Spouse; Child (son/daughter; stepchild/current partner´s child; son-in-law; daughter-in-law; grandchild); friends; neighbors; other relatives (niece; nephew; ex-spouse/partner) |
| Frequency | Almost day; almost every week; almost every month b; less often b |
| Long-term informal care received from household caregivers | |
| Occurrence | Yes; no |
| Kinship of informal caregiver | Partner/Spouse; Child (son/daughter; stepchild/current partner´s child; son-in-law; daughter-in-law; grandchild); friends; neighbors; other relatives (niece; nephew; ex-spouse/partner) |
| N | Denmark | Portugal | T/χ2 | p-Value | Cohen’s d/φ//V | |
|---|---|---|---|---|---|---|
| N = 1878 | N = 1013 | |||||
| Age, years (mean, SD) Age, classes (years) (%) | 2891 | 77.7(1.23) | 83.0(0.82) | 3.58 | p = 0.001 | 0.93 * |
| 65–69 | 997 | 33.5 | 28.6 | 24.8 | p = 0.007 | 0.09 + |
| 70–74 | 785 | 25.6 | 25.2 | |||
| 75–79 | 494 | 17.1 | 17.5 | |||
| 80–84 | 347 | 12.5 | 17.3 | |||
| 85–89 | 181 | 7.3 | 9.2 | |||
| ≥90 | 87 | 4.0 | 2.2 | |||
| Gender (%) | ||||||
| Female | 1520 | 54.0 | 58.3 | 4.8 | p = 0.006 | 0.04 |
| Male | 1371 | 46.0 | 41.7 | |||
| Marital status (%) | ||||||
| Married, living with a spouse | 1952 | 65.0 | 72.3 | 126.6 | p < 0.001 | 0.21 ++ |
| Registered partnership | 16 | 0.2 | 1.2 | |||
| Married, not living with a spouse | 28 | 0.7 | 1.4 | |||
| Never married | 104 | 4.0 | 2.9 | |||
| Divorced | 233 | 10.4 | 3.7 | |||
| Widowed | 558 | 19.6 | 18.7 | |||
| Educational level (ISCED-1997) (%) | ||||||
| None | 92 | 0.1 | 9.9 | 1013.8 | p = 0.000 | 0.59 +++ |
| Isced-97 code 1 | 952 | 15.9 | 63.4 | |||
| Isced-97 code 2 | 219 | 7.1 | 8.7 | |||
| Isced-97 code 3 | 845 | 40.8 | 7.5 | |||
| Isced-97 code 4 | 9 | 0.3 | 0.2 | |||
| Isced-97 code 5 | 765 | 36.0 | 10.1 | |||
| Isced-97 code 6 | 9 | 0.2 | 0.2 | |||
| Annual household income (%) | ||||||
| Low | 954 | 14.1 | 71.0 | 987.0 | p = 0.000 | 0.58 +++ |
| Medium | 954 | 42.5 | 23.5 | |||
| High | 983 | 43.5 | 5.5 | |||
| Chronic Diseases (%) | ||||||
| Less than two | 430 | 44.6 | 26.0 | 102.6 | p < 0.001 | 0.19 * |
| Two or more | 2461 | 55.4 | 74.0 | |||
| Depression (%) | ||||||
| Not depressed | 660 | 60.2 | 51.3 | 20.5 | p < 0.001 | 0.08 |
| Depressed | 2331 | 39.8 | 48.7 | |||
| Limitations in ADLs (%) | ||||||
| No limitations | 2419 | 93.0 | 81.2 | 70.9 | p < 0.001 | 0.16 * |
| One or more than one | 472 | 7.0 | 18.8 | |||
| Limitations in IADLs (%) | ||||||
| No limitations | 2200 | 84.6 | 76.2 | |||
| One or more than one | 691 | 15.4 | 23.8 | 27.7 | p < 0.0001 | 0.10 * |
| N | Denmark | Portugal | χ2 | p-Value | φ | |
|---|---|---|---|---|---|---|
| N = 1878 | N = 1013 | |||||
| Long-term informal care received from non-household caregivers | ||||||
| Occurrence (%) | ||||||
| No | 2798 | 97.3 | 94.4 | 11.9 | p < 0.001 | 0.06 |
| Yes | 93 | 2.7 | 5.6 | |||
| Kinship of informal caregiver (%) | ||||||
| -Partner/spouse | ||||||
| No | 2875 | 99.6 | 99.6 | 0.1 | p = 0.367 | 0.01 |
| Yes | 16 | 0.4 | 0.4 | |||
| -Child | ||||||
| No | 2837 | 98.4 | 96.8 | 6.1 | p < 0.001 | 0.05 |
| Yes | 54 | 1.6 | 3.2 | |||
| -Friends/Other relatives/Neighbors | ||||||
| No | 2842 | 98.3 | 97.3 | 2.9 | p < 0.001 | 0.03 |
| Yes | 49 | 1.7 | 2.7 | |||
| Frequency (%) | ||||||
| -Almost every day | ||||||
| No | 2830 | 98.5 | 94.7 | 23.5 | p < 0.001 | 0.09 |
| Yes | 61 | 1.5 | 5.3 | |||
| -Almost every week | ||||||
| No | 2860 | 98.7 | 99.6 | 7.1 | p < 0.001 | 0.05 |
| Yes | 31 | 1.3 | 0.4 | |||
| -Almost every month/Less often | ||||||
| No | 2858 | 98.6 | 99.4 | 5.1 | p < 0.001 | 0.04 |
| Yes | 33 | 1.4 | 0.6 | |||
| Long-term informal care received from household caregivers | ||||||
| Occurrence (%) | ||||||
| No | 2752 | 97.9 | 87.4 | 85.2 | p < 0.001 | 0.17 * |
| Yes | 139 | 2.1 | 12.6 | |||
| Kinship of informal caregiver (%) | ||||||
| -Partner/spouse | ||||||
| No | 2786 | 98.1 | 95.2 | 13.9 | p < 0.001 | 0.06 |
| Yes | 105 | 1.9 | 4.8 | |||
| -Child | ||||||
| No | 2867 | 99.9 | 94.7 | 51.1 | p < 0.001 | 0.13 * |
| Yes | 27 | 0.1 | 5.3 | |||
| -Friends/Other relatives/Neighbors | ||||||
| No | 2881 | 99.8 | 99.5 | 0.8 | p = 0.034 | 0.02 |
| Yes | 10 | 0.2 | 0.5 | |||
| Ability to Receive Long-Term Informal Care from Non-Household Caregivers | Ability to Receive Long-Term Informal Care from Household Caregivers | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |||||||||
| OR | 95% IC | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Age, years | 1.04 | 1.01–1.07 | * | 1.01 | 0.96–1.05 | 1.08 | 1.05–1.12 | *** | 1.06 | 1.01–1.11 | * | |
| Gender | ||||||||||||
| Female (ref.) | ||||||||||||
| Male | 0.91 | 0.56–1.47 | 0.93 | 0.57–1.51 | 1.26 | 0.82–1.93 | 1.29 | 0.84–1.98 | ||||
| Marital Status | ||||||||||||
| Live with spouse (ref.) | ||||||||||||
| Does not live with a spouse | 1.82 | 1.09–3.02 | * | 1.74 | 1.05–2.90 | * | 0.17 | 0.10–0.31 | *** | 0.17 | 0.13–0.30 | *** |
| Educational level | ||||||||||||
| None-Isced code 2 (ref.) | ||||||||||||
| Isced code 3- Isced code 6 | 1.30 | 0.75–2.26 | 1.18 | 0.67–2.08 | 2.02 | 1.18–3.48 | * | 1.96 | 1.13–3.40 | * | ||
| Annual Household Income | ||||||||||||
| Lower (ref.) | ||||||||||||
| Medium | 0.87 | 0.48–1.56 | 0.86 | 0.47–1.56 | 1.32 | 0.74–2.36 | 1.381 | 0.76–2.50 | ||||
| Higher | 0.22 | 0.07–0.69 | * | 0.18 | 0.06–0.58 | ** | 2.23 | 1.06–4.67 | * | 2.13 | 0.99–4.56 | * |
| Country Denmark (ref.) | ||||||||||||
| Portugal Country*Age | 1.40 | 0.74–2.63 | 0.01 | 0.00–0.79 | * | 7.35 | 4.05–13.33 | *** | 0.34 | 0.00–31.37 | ||
| 1.07 | 1.01–1.13 | * | 1.04 | 0.98–1.10 | ||||||||
| Number of Chronic Diseases | ||||||||||||
| Fewer than two (ref.) | ||||||||||||
| Two or more | 2.19 | 1.20–3.98 | * | 2.21 | 1.21–4.04 | * | 1.54 | 0.94–2.51 | 0.94 | 1.00–2.51 | ||
| Depression (Euro-D) | ||||||||||||
| Not depressed (ref.) | ||||||||||||
| Depressed | 1.13 | 0.71–1.80 | 1.12 | 0.70–1.78 | 1.60 | 1.05–2.44 | * | 1.63 | 1.07–2.49 | * | ||
| Limitations in ADLs | ||||||||||||
| No limitations (ref) | ||||||||||||
| One or more than one | 3.08 | 1.86–5.09 | *** | 3.10 | 1.87–5.14 | *** | 6.18 | 3.95–9.66 | *** | 6.19 | 3.96–9.69 | *** |
| limitation in IADLs | ||||||||||||
| No limitations (ref.) | ||||||||||||
| One or more than one | 2.90 | 1.76–4.78 | *** | 2.94 | 1.78–4.87 | *** | 8.09 | 5.15–12.71 | *** | 8.26 | 5.26–12.99 | *** |
| Likelihood Ratio Test:χ2(11) = 151.68, p < 0.001 Hosmer–Lemeshow Test: χ2(8) = 3.70, p = 0.883 Nagelkerke R2 = 0.218 | Likelihood Ratio Test: χ2(12) = 156.65, p < 0.001 Hosmer–Lemeshow Test: χ2(8) = 6.75, p = 0.564 Nagelkerke R2 = 0.225 | Likelihood Ratio Test: χ2(11) = 377.64, p < 0.001 Hosmer–Lemeshow Test: χ2(8) = 9.45, p = 0.305 Nagelkerke R2 = 0.393 | Likelihood Ratio Test: χ2(12) = 379.44, p < 0.001 Hosmer–Lemeshow Test: χ2(8) = 9.43, p = 0.308 Nagelkerke R2 = 0.395 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maia, A.C.; Nogueira, P.; Henriques, M.A.; Farinha, C.; Costa, A. Ageing and Long-Term Informal Care: The Reality of Two Countries in Europe: Denmark and Portugal. Int. J. Environ. Res. Public Health 2022, 19, 10859. https://doi.org/10.3390/ijerph191710859
Maia AC, Nogueira P, Henriques MA, Farinha C, Costa A. Ageing and Long-Term Informal Care: The Reality of Two Countries in Europe: Denmark and Portugal. International Journal of Environmental Research and Public Health. 2022; 19(17):10859. https://doi.org/10.3390/ijerph191710859
Chicago/Turabian StyleMaia, Ana Catarina, Paulo Nogueira, Maria Adriana Henriques, Carla Farinha, and Andreia Costa. 2022. "Ageing and Long-Term Informal Care: The Reality of Two Countries in Europe: Denmark and Portugal" International Journal of Environmental Research and Public Health 19, no. 17: 10859. https://doi.org/10.3390/ijerph191710859
APA StyleMaia, A. C., Nogueira, P., Henriques, M. A., Farinha, C., & Costa, A. (2022). Ageing and Long-Term Informal Care: The Reality of Two Countries in Europe: Denmark and Portugal. International Journal of Environmental Research and Public Health, 19(17), 10859. https://doi.org/10.3390/ijerph191710859









