Elastic Dynamic Sling on Subluxation of Hemiplegic Shoulder in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
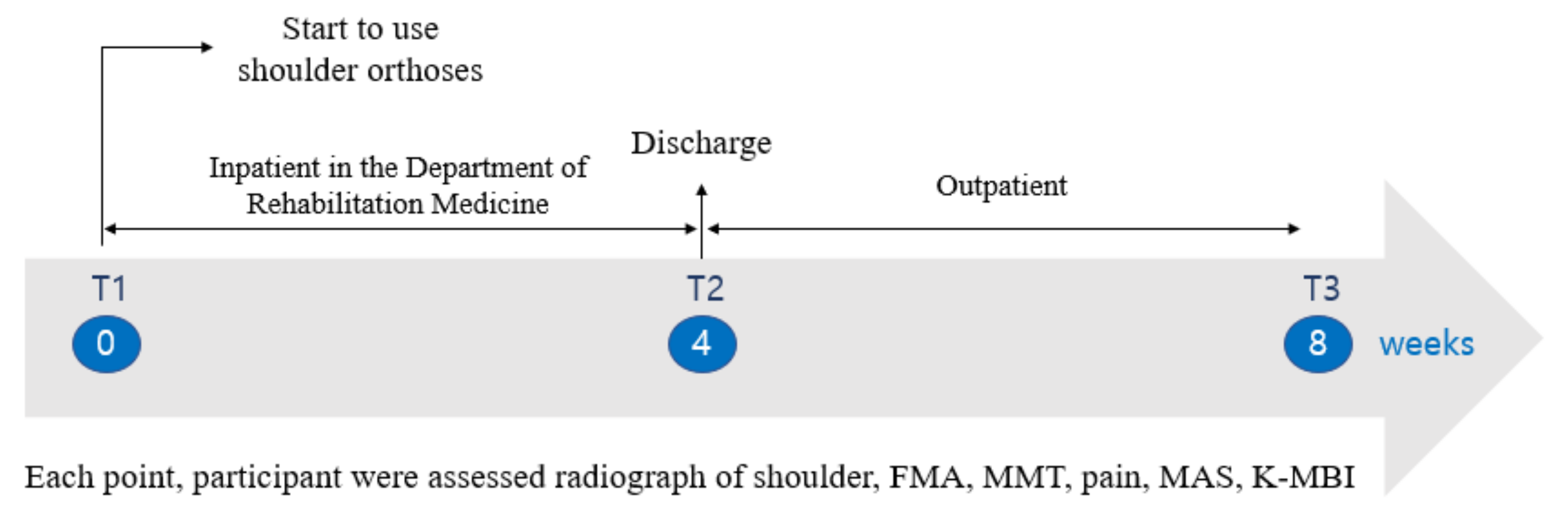
2.1. Design
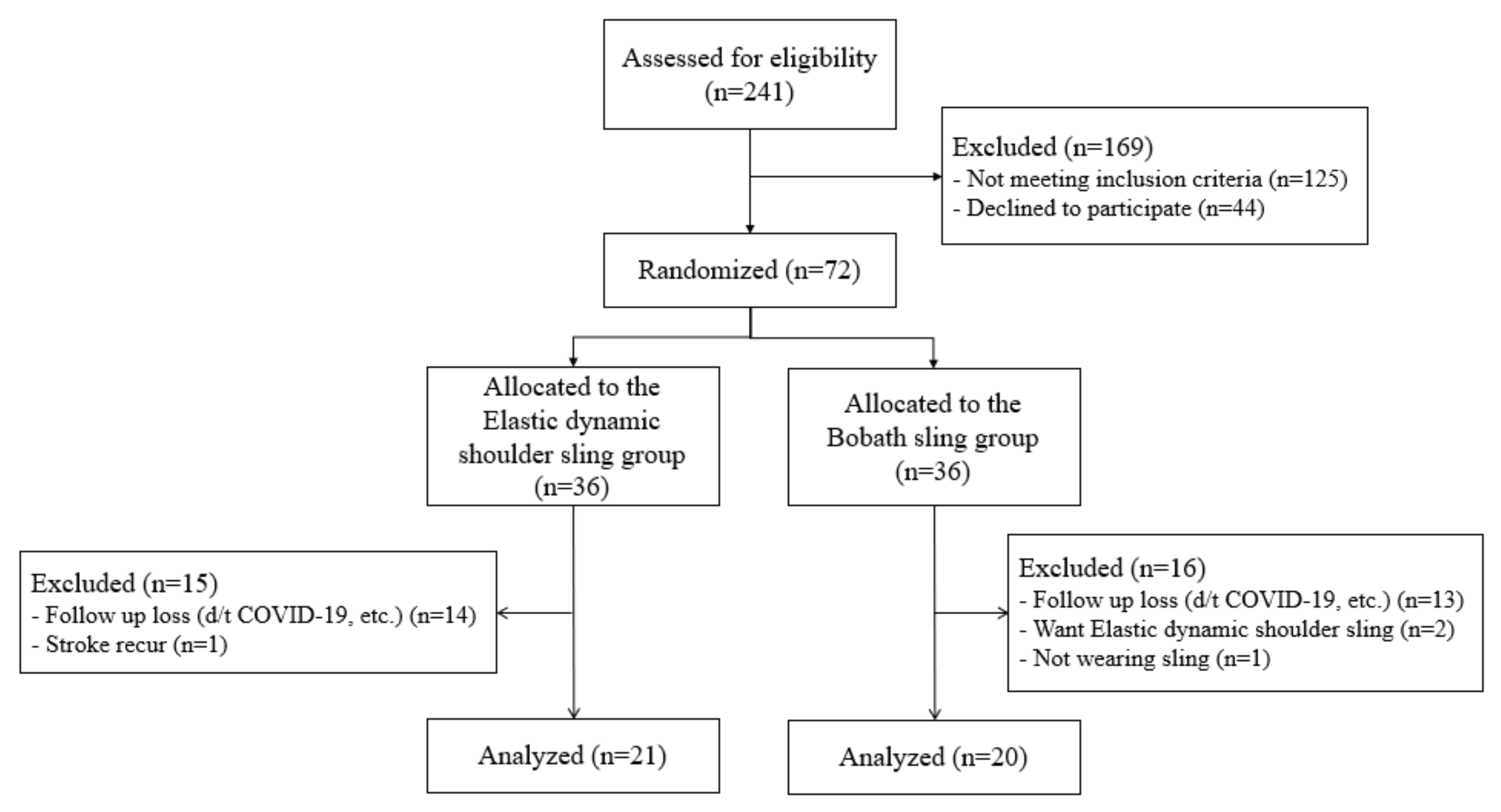
2.2. Randomization
2.3. Participants
2.4. Intervention
- (1)
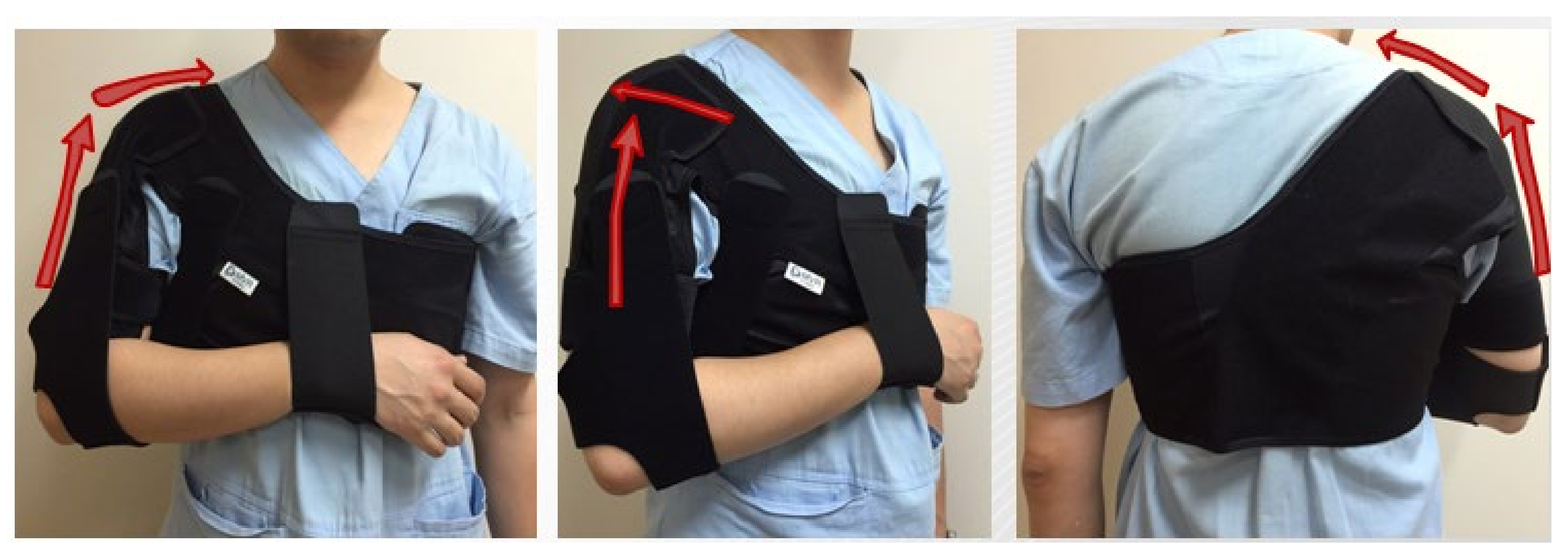
- Elastic dynamic shoulder sling: The shoulder device consists of three main parts: (1) a shoulder belt placed over the affected shoulder, (2) chest belt, and (3) wrist belt on the affected side. It uses elastic material to lift the deltoid and fix the scapula so that it can be adducted and retracted (Figure 1).
- (2)
- Bobath sling: The shoulder device consists of three main parts: (1) a foam roll placed in the axillary region of the affected shoulder, (2) a figure-8 pattern that connects the shoulder blades, and (3) a horizontal strap made of similar material that encircles around the chest (Figure 2).
2.5. Outcomes
- (1)
- Primary outcomes
- (2)
- Secondary outcomes
2.6. Data Analysis
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kumar, P. Hemiplegic shoulder pain in people with stroke: Present and the future. Pain Manag. 2019, 9, 107–110. [Google Scholar] [CrossRef]
- Lindgren, I.; Jönsson, A.-C.; Norrving, B.; Lindgren, A. Shoulder pain after stroke: A prospective population-based study. Stroke 2007, 38, 343–348. [Google Scholar] [CrossRef]
- Anwer, S.; Alghadir, A. Incidence, Prevalence, and Risk Factors of Hemiplegic Shoulder Pain: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 4962. [Google Scholar] [CrossRef]
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.M.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A.N. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Stolzenberg, D.; Siu, G.; Cruz, E. Current and future interventions for glenohumeral subluxation in hemiplegia secondary to stroke. Top. Stroke Rehabil. 2012, 19, 444–456. [Google Scholar] [CrossRef] [PubMed]
- Gamble, G.E.; Barberan, E.; Laasch, H.-U.; Bowsher, D.; Tyrrell, P.J.; Jones, A.K.P. Poststroke shoulder pain: A prospective study of the association and risk factors in 152 patients from a consecutive cohort of 205 patients presenting with stroke. Eur. J. Pain 2002, 6, 467–474. [Google Scholar] [CrossRef]
- Lee, S.C.; Kim, A.R.; Chang, W.H.; Kim, J.-s.; Kim, D.Y. Hemiplegic Shoulder Pain in Shoulder Subluxation after Stroke: Associated with Range of Motion Limitation. Brain Neurorehabilit. 2018, 11, e6. [Google Scholar] [CrossRef]
- Walsh, K. Management of shoulder pain in patients with stroke. Postgrad. Med. J. 2001, 77, 645–649. [Google Scholar] [CrossRef]
- Turner-Stokes, L.; Jackson, D. Shoulder pain after stroke: A review of the evidence base to inform the development of an integrated care pathway. Clin. Rehabil. 2002, 16, 276–298. [Google Scholar] [CrossRef]
- Ada, L.; Foongchomcheay, A.; Canning, C. Supportive devices for preventing and treating subluxation of the shoulder after stroke. Cochrane Database Syst. Rev. 2005, 36, CD003863. [Google Scholar]
- Foongchomcheay, A.; Ada, L.; Canning, C.G. Use of devices to prevent subluxation of the shoulder after stroke. Physiother. Res. Int. 2005, 10, 134–145. [Google Scholar] [CrossRef]
- Pan, R.; Zhou, M.; Cai, H.; Guo, Y.; Zhan, L.; Li, M.; Yang, Z.; Zhu, L.; Zhan, J.; Chen, H. A randomized controlled trial of a modified wheelchair arm-support to reduce shoulder pain in stroke patients. Clin. Rehabil. 2018, 32, 37–47. [Google Scholar] [CrossRef]
- Ravichandran, H.; Balamurugan, J.; Sundaram, S.; Fisseha, B.; Gebreyesus, T.; Gelaw, A.Y. Systematic Review on Effectiveness of shoulder taping in Hemiplegia. J. Stroke Cerebrovasc Dis. 2019, 28, 1463–1473. [Google Scholar] [CrossRef]
- Nadler, M.; Pauls, M. Shoulder orthoses for the prevention and reduction of hemiplegic shoulder pain and subluxation: Systematic review. Clin. Rehabil. 2017, 31, 444–453. [Google Scholar] [CrossRef]
- de Sire, A.; Moggio, L.; Demeco, A.; Fortunato, F.; Spanò, R.; Aiello, V.; Marotta, N.; Ammendolia, A. Efficacy of rehabilitative techniques in reducing hemiplegic shoulder pain in stroke: Systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2021, 65, 101602. [Google Scholar] [CrossRef]
- Ada, L.; Goddard, E.; McCully, J.; Stavrinos, T.; Bampton, J. Thirty minutes of positioning reduces the development of shoulder external rotation contracture after stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2005, 86, 230–234. [Google Scholar] [CrossRef]
- Lannin, N.A.; Horsley, S.A.; Herbert, R.; McCluskey, A.; Cusick, A. Splinting the hand in the functional position after brain impairment: A randomized, controlled trial. Arch. Phys. Med. Rehabil. 2003, 84, 297–302. [Google Scholar] [CrossRef]
- Sullivan, K.J.; Tilson, J.K.; Cen, S.Y.; Rose, D.K.; Hershberg, J.; Correa, A.; Gallichio, J.; McLeod, M.; Moore, C.; Wu, S.S.; et al. Fugl-Meyer assessment of sensorimotor function after stroke: Standardized training procedure for clinical practice and clinical trials. Stroke 2011, 42, 427–432. [Google Scholar] [CrossRef]
- Jung, H.-Y.; Park, B.K.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean version of Modified Barthel Index (K-MBI): Multi-center study for subjects with stroke. J. Korean Acad. Rehabil. Med. 2007, 31, 283–297. [Google Scholar]
- Meseguer-Henarejos, A.-B.; Sánchez-Meca, J.; López-Pina, J.A.; Carles-Hernández, R. Inter-and intra-rater reliability of the Modified Ashworth Scale: A systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 2017, 54, 576–590. [Google Scholar] [CrossRef]
- Cuthbert, S.C.; Goodheart, G.J., Jr. On the reliability and validity of manual muscle testing: A literature review. Chiropr. Osteopat 2007, 15, 4. [Google Scholar] [CrossRef]
- Brooke, M.M.; de Lateur, B.J.; Diana-Rigby, G.C.; Questad, K.A. Shoulder subluxation in hemiplegia: Effects of three different supports. Arch. Phys. Med. Rehabil. 1991, 72, 582–586. [Google Scholar]
- Magezi, D.A. Linear mixed-effects models for within-participant psychology experiments: An introductory tutorial and free, graphical user interface (LMMgui). Front. Psychol. 2015, 6, 2. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Moodie, N.B. Subluxation of the glenohumeral joint in hemiplegia: Evaluation of supportive devices. Physiother. Can. 1986, 38, 151–157. [Google Scholar]
- Morley, A.; Clarke, A.; English, S.; Helliwell, S. Management of the Subluxed Low Tone Shoulder. Physiotherapy 2002, 88, 208–216. [Google Scholar] [CrossRef]
- Zorowitz, R.D.; Idank, D.; Ikai, T.; Hughes, M.B.; Johnston, M.V. Shoulder subluxation after stroke: A comparison of four supports. Arch. Phys. Med. Rehabil. 1995, 76, 763–771. [Google Scholar] [CrossRef]
- Paci, M.; Nannetti, L.; Rinaldi, L.A. Glenohumeral subluxation in hemiplegia: An overview. J. Rehabil. Res. Dev. 2005, 42, 557–568. [Google Scholar] [CrossRef]
- Huang, S.-W.; Liu, S.-Y.; Tang, H.-W.; Wei, T.-S.; Wang, W.-T.; Yang, C.-P. Relationship between severity of shoulder subluxation and soft-tissue injury in hemiplegic stroke patients. J. Rehabil. Med. 2012, 44, 733–739. [Google Scholar] [CrossRef]
- Rost, N.S.; Brodtmann, A.; Pase, M.P.; van Veluw, S.J.; Biffi, A.; Duering, M.; Hinman, J.D.; Dichgans, M. Post-Stroke Cognitive Impairment and Dementia. Circ. Res. 2022, 130, 1252–1271. [Google Scholar] [CrossRef]


| Characteristics | Elastic Dynamic Sling Group (n = 21) | Bobath Sling Group (n = 20) | p Value |
|---|---|---|---|
| Age (years) | 64.76 ± 12.80 | 63.60 ± 14.46 | 0.774 |
| Sex (male) | 13 | 10 | 0.443 |
| K-MBI | 35.00 ± 17.85 | 30.90 ± 20.50 | 0.267 |
| FMA-total | 9.86 ± 9.94 | 8.10 ± 7.08 | 0.579 |
| MMT (of shoulder) | 1.44 ± 0.92 | 1.27 ± 0.76 | 0.413 |
| Underlying disease | |||
| HTN | 81.0% (n = 17) | 65.0% (n = 13) | 0.247 |
| DM | 28.6% (n = 6) | 30.0% (n = 6) | 0.920 |
| Dyslipidemia | 14.3% (n = 3) | 25.0% (n = 5) | 0.387 |
| Lesion | |||
| Brain stem | 4.76% (n = 1) | 5% (n = 1) | 0.972 |
| Non-brain stem | 95.24% (n = 20) | 95% (n = 19) | |
| Stroke | |||
| Infarction | 71.43% (n = 15) | 55% (n = 11) | 0.275 |
| Hemorrhage | 28.57% (n = 6) | 45% (n = 9) |
| Average | p-Value | ||
|---|---|---|---|
| Elastic Dynamic Sling Group (n= 21) | Bobath Sling Group (n = 20) | ||
| VD0 | 42.99 ± 8.41 | 41.44 ± 9.06 | |
| VD1 | 43.66 ± 8.26 | 44.57 ± 7.16 | |
| VD2 | 45.60 ± 9.05 | 42.87 ± 9.16 | |
| ∆VD1 | 0.67 ± 7.76 | 3.05 ± 9.00 | 0.382 |
| ∆VD2 | 2.61 ± 10.95 | 1.43 ± 12.58 | 0.751 |
| Average | p-Value | ||
|---|---|---|---|
| Elastic Dynamic Sling Group (n = 21) | Bobath Sling Group (n = 20) | ||
| HD0 | 28.02 ± 2.66 | 27.44 ± 2.16 | |
| HD1 | 27.13 ± 2.21 | 28.14 ± 2.52 | |
| HD2 | 27.22 ± 2.40 | 29.73 ± 4.08 | |
| ∆HD1 | −0.89 ± 2.46 | 0.48 ± 2.32 | 0.083 |
| ∆HD2 | −0.80 ± 3.11 | 2.28 ± 3.66 | 0.006 |
| Measure | Baseline | 4 Weeks | 8 Weeks | p1-Value | p2-Value |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Elastic Dynamic Sling Group | |||||
| Vertical Distance | 42.99 ± 8.41 | 43.66 ± 8.26 | 45.60 ± 9.05 | 0.7355 a | 0.193 a |
| Horizontal Distance | 28.02 ± 2.66 | 27.13 ± 2.21 | 27.22 ± 2.40 | 0.584 a | 0.3309 a |
| Bobath Group | |||||
| Vertical Distance | 41.44 ± 9.06 | 44.57 ± 7.16 | 42.87 ± 9.16 | 0.1666 a | 0.4203 a |
| Horizontal Distance | 27.44 ± 2.16 | 28.14 ± 2.52 | 29.73 ± 4.08 | 0.0273 a | 0.0023 a |
| Measure | Baseline | 4 Weeks | 8 Weeks | p1-Value | p2-Value |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Elastic Dynamic Sling Group | |||||
| FMA-UE | 7.52 ± 5.62 | 12.24 ± 7.45 | 15.25 ± 8.81 | 0.0001 a | <0.0001 a |
| FMA-Wrist | 1.05 ± 1.94 | 2.05 ± 3.26 | 2.26 ± 4.06 | 0.0691 a | 0.0045 a |
| FMA-Hand | 1.14 ± 3.09 | 1.81 ± 2.89 | 2.85 ± 4.32 | 0.1081 a | 0.0003 a |
| FMA-Co | 0.14 ± 0.65 | 0.33 ± 1.06 | 1.45 ± 2.39 | 0.6379 a | 0.0028 a |
| FMA-Total | 10.05 ± 9.77 | 15.48 ± 13.28 | 22.15 ± 17.10 | 0.0085 a | <0.0001 a |
| MBI | 35.00 ± 17.85 | 46.00 ± 17.98 | 58.80 ± 27.73 | 0.0019 a | <0.001 a |
| Pain (VAS) | 1.52 ± 2.14 | 1.76 ± 2.47 | 1.86 ± 2.46 | 0.6332 a | 0.5046 a |
| MAS | 0.33 ± 0.58 | 0.67 ± 0.70 | 0.76 ± 0.87 | 0.0444 a | 0.0109 a |
| MMT | 1.55 ± 0.95 | 2.71 ± 1.88 | 3.19 ± 1.97 | <0.0001 a | <0.0001 a |
| Bobath Group | |||||
| FMA-UE | 6.70 ± 5.14 | 14.53 ± 8.52 | 16.65 ± 9.39 | 0.0002 a | <0.0001 a |
| FMA-Wrist | 0.90 ± 2.10 | 2.26 ± 3.23 | 2.85 ± 3.38 | 0.0071 a | <0.0001 a |
| FMA-Hand | 0.20 ± 0.62 | 2.58 ± 3.58 | 3.95 ± 4.87 | 0.0109 a | <0.0001 a |
| FMA-Co | 0.30 ± 0.73 | 1.00 ± 1.73 | 1.00 ± 1.75 | 0.0522 a | 0.0420 a |
| FMA-Total | 8.10 ± 7.08 | 20.11 ± 14.91 | 24.60 ± 17.16 | 0.0005 a | <0.0001 a |
| MBI | 30.90 ± 20.50 | 44.70 ± 22.75 | 51.30 ± 27.18 | 0.0004 a | <0.001 a |
| Pain (VAS) | 1.35 ± 2.64 | 1.20 ± 1.82 | 1.70 ± 2.60 | 0.7717 a | 0.4994 a |
| MAS | 0.25 ± 0.53 | 0.48 ± 0.55 | 0.65 ± 0.90 | 0.1840 a | 0.0211 a |
| MMT | 1.35 ± 0.88 | 3.08 ± 1.66 | 3.35 ± 2.30 | <0.0001 a | <0.0001 a |
| Average | p-Value | ||
|---|---|---|---|
| Elastic Dynamic Sling Group (N = 21) Mean ± SD | Bobath Sling Group (N = 20) Mean ± SD | ||
| 4 weeks | |||
| ∆FMA-UE1 | 4.71 ± 4.66 | 7.68 ± 9.40 | 0.448 |
| ∆FMA-Wrist1 | 1.00 ± 2.17 | 1.32 ± 2.00 | 0.437 |
| ∆FMA-Hand1 | 0.67 ± 1.35 | 2.37 ± 3.48 | 0.063 |
| ∆FMA-Co1 | 0.19 ± 0.87 | 0.68 ± 1.63 | 0.146 |
| ∆FMA-Total1 | 5.43 ± 7.63 | 11.79 ± 15.06 | 0.125 |
| ∆MBI1 | 11.00 ± 12.32 | 13.80 ± 16.41 | 0.887 |
| ∆Pain (VAS)1 | 0.24 ± 2.21 | −0.15 ± 1.79 | 0.908 |
| ∆MAS1 | 0.33 ± 0.86 | 0.23 ± 0.47 | 0.621 |
| ∆MMT1 | 1.17 ± 1.37 | 0.40 ± 0.94 | 0.246 |
| 8 weeks | |||
| ∆FMA-UE2 | 7.55 ± 6.71 | 9.95 ± 9.74 | 0.467 |
| ∆FMA-Wrist2 | 1.65 ± 3.25 | 1.95 ± 2.19 | 0.532 |
| ∆FMA-Hand2 | 1.65 ± 2.41 | 3.75 ± 4.84 | 0.329 |
| ∆FMA-Co2 | 1.30 ± 2.39 | 0.70 ± 1.53 | 0.585 |
| ∆FMA-Total2 | 11.80 ± 11.65 | 16.50 ± 16.20 | 0.377 |
| ∆MBI2 | 22.75 ± 17.27 | 20.40 ± 20.51 | 0.601 |
| ∆Pain (VAS)2 | 0.33 ± 2.61 | 0.35 ± 3.05 | 0.999 |
| ∆MAS2 | 0.43 ± 0.76 | 0.40 ± 0.94 | 0.839 |
| ∆MMT2 | 1.64 ± 1.41 | 2.00 ± 2.34 | 0.752 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.G.; Lee, S.A.; Park, E.J.; Choi, M.K.; Kim, J.M.; Sohn, M.K.; Jee, S.J.; Kim, Y.W.; Son, J.E.; Lee, S.J.; et al. Elastic Dynamic Sling on Subluxation of Hemiplegic Shoulder in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 9975. https://doi.org/10.3390/ijerph19169975
Kim MG, Lee SA, Park EJ, Choi MK, Kim JM, Sohn MK, Jee SJ, Kim YW, Son JE, Lee SJ, et al. Elastic Dynamic Sling on Subluxation of Hemiplegic Shoulder in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(16):9975. https://doi.org/10.3390/ijerph19169975
Chicago/Turabian StyleKim, Min Gyun, Seung Ah Lee, Eo Jin Park, Min Kyu Choi, Ji Min Kim, Min Kyun Sohn, Sung Ju Jee, Yeong Wook Kim, Jung Eun Son, Seo Jun Lee, and et al. 2022. "Elastic Dynamic Sling on Subluxation of Hemiplegic Shoulder in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 16: 9975. https://doi.org/10.3390/ijerph19169975
APA StyleKim, M. G., Lee, S. A., Park, E. J., Choi, M. K., Kim, J. M., Sohn, M. K., Jee, S. J., Kim, Y. W., Son, J. E., Lee, S. J., Hwang, K. S., & Yoo, S. D. (2022). Elastic Dynamic Sling on Subluxation of Hemiplegic Shoulder in Patients with Subacute Stroke: A Multicenter Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(16), 9975. https://doi.org/10.3390/ijerph19169975






