A Prospective Comparative Analysis Regarding the Assessment of Oral Mucosal Disease Using a Validated Questionnaire to Improve the Teaching of Dental Students
Abstract
:1. Introduction
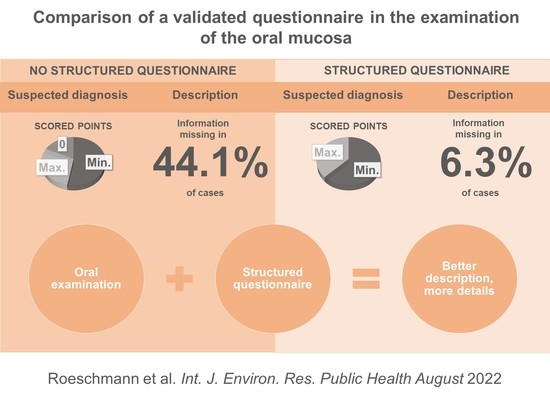
2. Experimental Section
2.1. Study Design and Setup
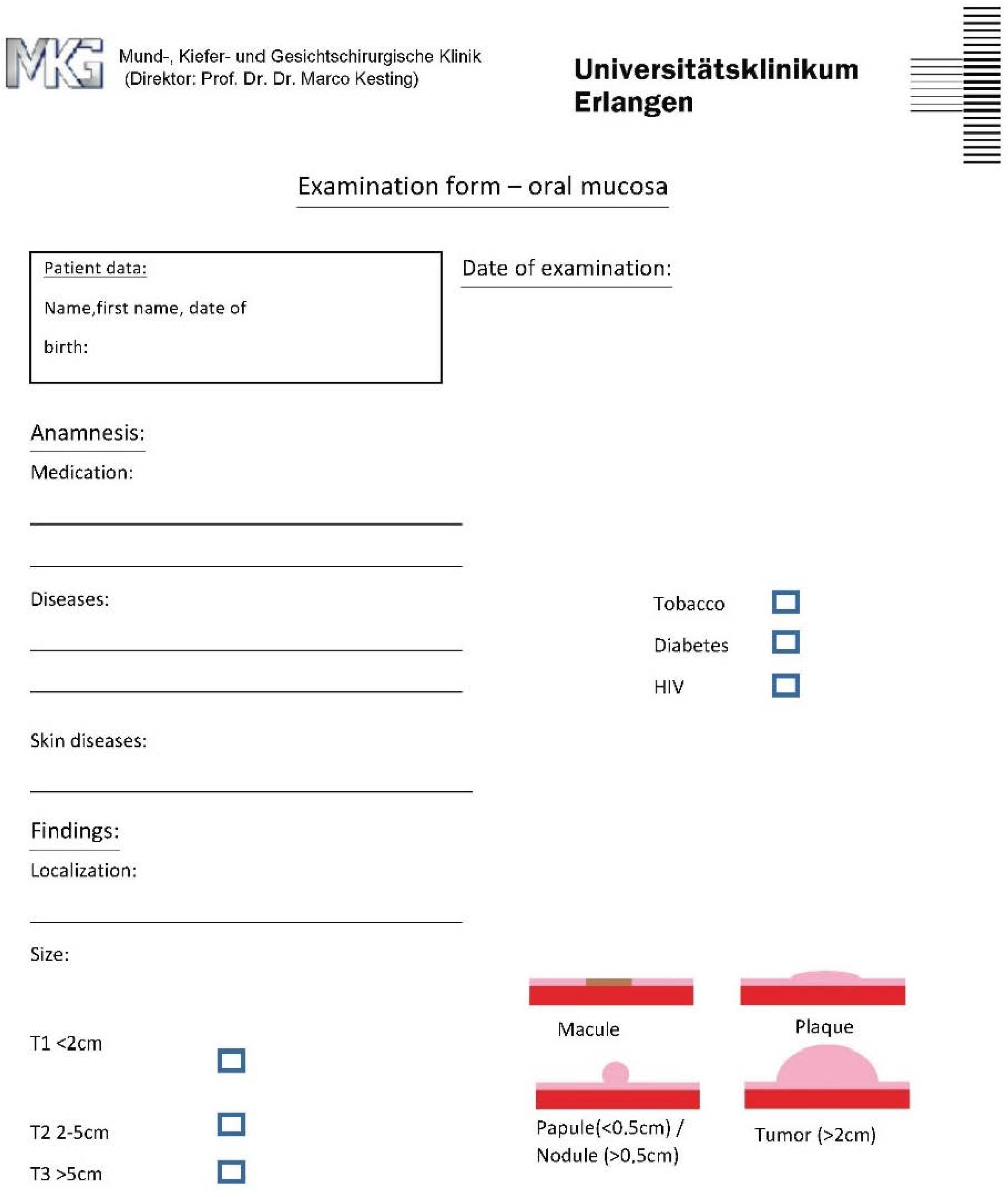
2.2. Design of the Questionnaire for Group 2
2.3. Data Extraction and Examination
- Localization.
- Size.
- Type of lesion (according to the inclusion criteria).
- Surface and margin condition.
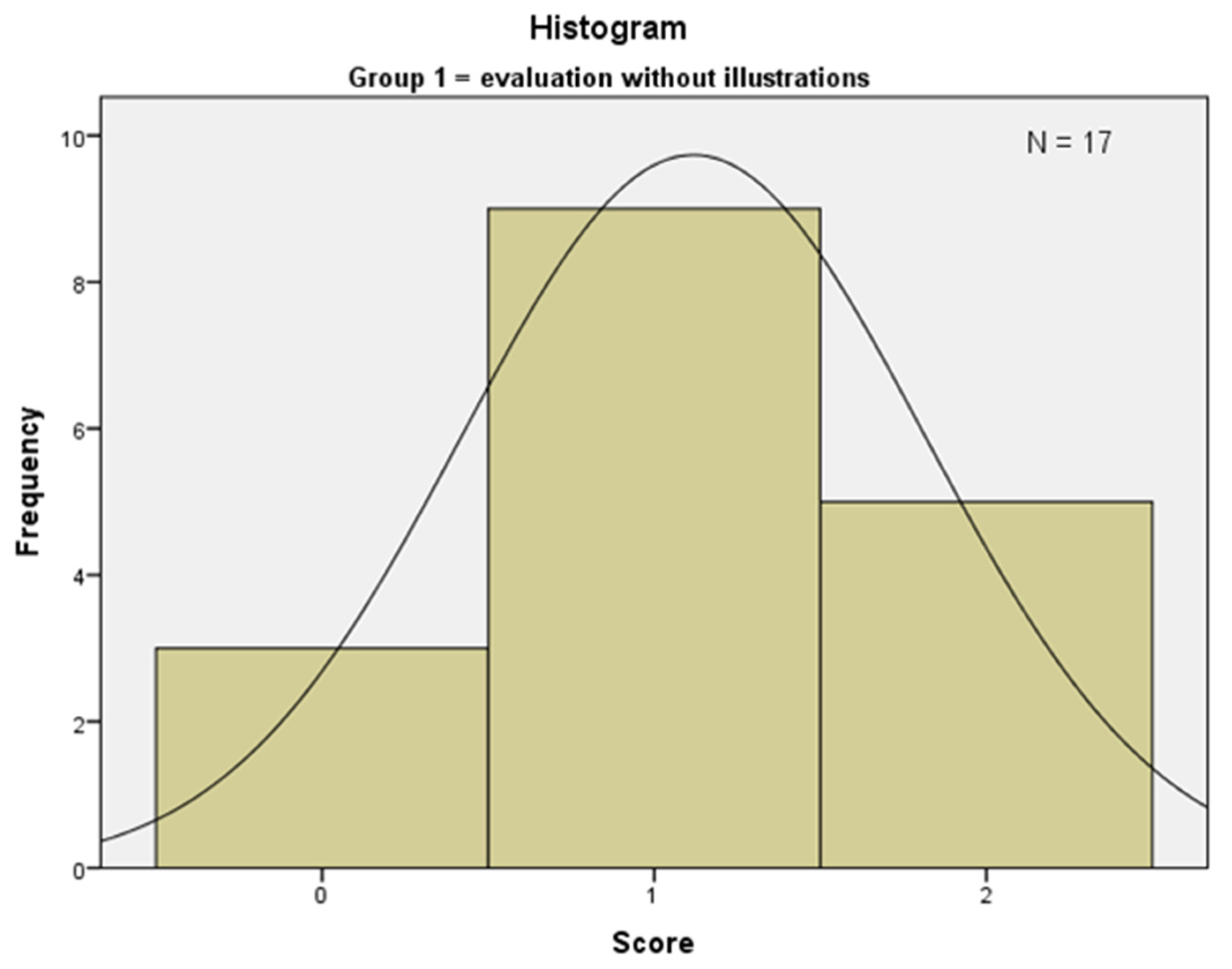
2.4. Outcomes
2.5. Data and Statistical Analysis
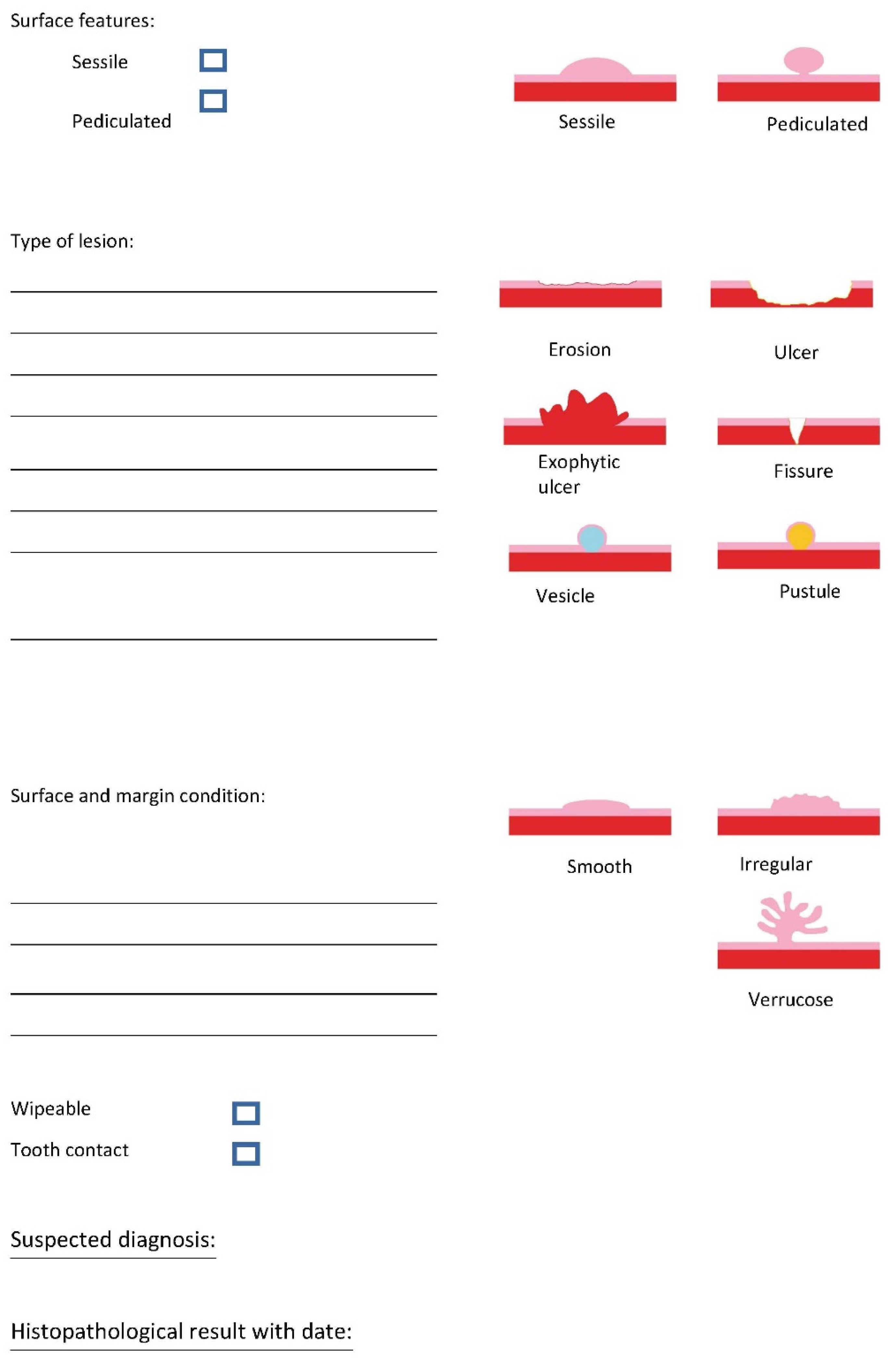
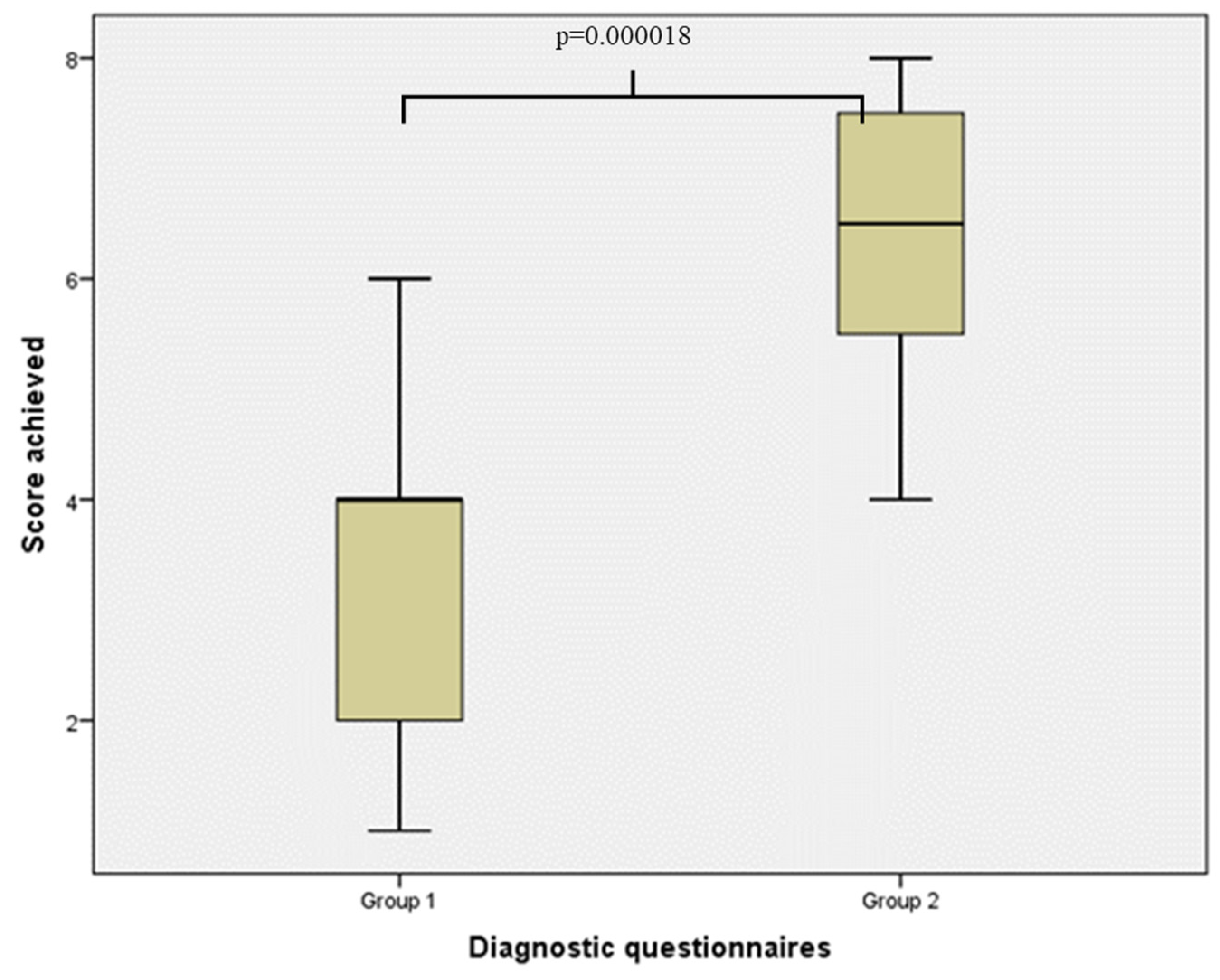
3. Results
3.1. Participant Cohorts
3.2. Primary Outcome—Diagnosis
3.3. Secondary Outcome—Description
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shulman, J.D.; Beach, M.M.; Rivera-Hidalgo, F. The prevalence of oral mucosal lesions in U.S. adults: Data from the Third National Health and Nutrition Examination Survey, 1988–1994. J. Am. Dent. Assoc. 2004, 135, 1279–1286. [Google Scholar] [CrossRef]
- Carrard, V.; Haas, A.; Rados, P.; Filho, M.; Oppermann, R.; Albandar, J.M.; Susin, C. Prevalence and risk indicators of oral mucosal lesions in an urban population from South Brazil. Oral Dis. 2010, 17, 171–179. [Google Scholar] [CrossRef]
- Robert Koch-Institut, Zentrum für Krebsregisterdaten. Datenbankabfrage mit Schätzung der Inzidenz, Prävalenz und des Überlebens von Krebs in Deutschland auf Basis der Epidemiologischen Landeskrebsregisterdaten 2021. Mortalitätsdaten Bereitgestellt vom Statistischen Bundesamt. Available online: www.krebsdaten.de/abfrage (accessed on 23 June 2021).
- Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft DK, AWMF). S3-Leitlinie Diagnostik und Therapie des Mundhöhlenkarzinoms: Leitlinienprogramm Onkologie. Langversion 3.0:AWMF Registernummer: 007/100OL. 2021. Available online: https://www.leitlinienprogramm-onkologie.de/leitlinien/mundhoehlenkarzinom/ (accessed on 23 June 2021).
- Muir, C.; Weiland, L. Upper aerodigestive tract cancers. Cancer 1995, 75, 147–153. [Google Scholar] [CrossRef]
- Howaldt, H.P.; Vorast, H.; Blecher, J.C.; Reicherts, M.; Kainz, M. Ergebnisse aus dem DÖSAK-Tumorregister. Mund Kiefer Gesichtschirurgie 2000, 4, S216–S225. [Google Scholar] [CrossRef]
- Howaldt, H.-P.; Schmelzeisen, R. Einführung in die Mund-, Kiefer-, Gesichtschirurgie, 2nd ed.; Deutscher Ärzteverlag: Cologne, Germany, 2015. [Google Scholar]
- Allon, I.; Kaplan, I.; Gal, G.; Chaushu, G.; Allon, D. The clinical characteristics of benign oral mucosal tumors. Med. Oral Patol. Oral Cir. Bucal 2014, 19, e438–e443. [Google Scholar] [CrossRef]
- Fattahi, S.; Vosoughhosseini, S.; Khiavi, M.M.; Mostafazadeh, S.; Gheisar, A. Consistency Rates of Clinical Diagnosis and Histopathological Reports of Oral Lesions: A Retrospective Study. J. Dent. Res. Dent. Clin. Dent. Prospect. 2014, 8, 111–113. [Google Scholar]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Silverman, S. Early diagnosis of oral cancer. Cancer 1988, 62, 1796–1799. [Google Scholar] [CrossRef]
- Abati, S.; Bramati, C.; Bondi, S.; Lissoni, A.; Trimarchi, M. Oral Cancer and Precancer: A Narrative Review on the Relevance of Early Diagnosis. Int. J. Environ. Res. Public Health 2020, 17, 9160. [Google Scholar] [CrossRef] [PubMed]
- Pitiphat, W.; Diehl, S.R.; Laskaris, G.; Cartsos, V.; Douglass, C.W.; Zavras, A. Factors associated with delay in the diagnosis of oral cancer. J. Dent. Res. 2002, 81, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.J.; de Silva, H.L.; Tong, D.C.; Love, R.M. Concordance Between Clinical and Histopathologic Diagnoses of Oral Mucosal Lesions. J. Oral Maxillofac. Surg. 2011, 69, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Pakravan, F.; Abbasi, F.; Garshasbi, M.A.; Isfahani, M.N. Relationship between oral cancer stage and elapsed time from the onset of signs and symptoms to diagnosis and treatment. Cancer Treat. Res. Commun. 2021, 28, 100428. [Google Scholar] [CrossRef] [PubMed]
- Warnakulasuriya, S.; Kujan, O.; Aguirre-Urizar, J.M.; Bagan, J.V.; González-Moles, M.; Kerr, A.R.; Lodi, G.; Mello, F.W.; Monteiro, L.; Ogden, G.R.; et al. Oral potentially malignant disorders: A consensus report from an international seminar on nomenclature and classification, convened by the WHO Collaborating Centre for Oral Cancer. Oral Dis. 2020, 27, 1862–1880. [Google Scholar] [CrossRef] [PubMed]
- Silverman, S.; Kerr, A.R.; Epstein, J.B. Oral and Pharyngeal Cancer Control and Early Detection. J. Cancer Educ. 2010, 25, 279–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lapiedra, R.C.; Esparza-Gómez, G.C.; la Cruz, L.C.-D.; Domínguez-Gordillo, A.A.; Corral-Linaza, C.; Seoane-Romero, J.M. Ability of Dental Students in Spain to Identify Potentially Malignant Disorders and Oral Cancer. J. Dent. Educ. 2015, 79, 959–964. [Google Scholar] [CrossRef]
- Keser, G.; Pekiner, F.N. Assessing Oral Cancer Awareness Among Dental Students. J. Cancer Educ. 2018, 34, 512–518. [Google Scholar] [CrossRef]
- Srivastava, R.; Wazir, S.S.; Jyoti, B.; Kushwah, S.; Pradhan, D.; Priyadarshi, P. Perception and outcome of oral cancer awareness among clinical undergraduate dental students of Tertiary health care centre at Kanpur city: A cross-sectional study. Natl. J. Maxillofac. Surg. 2020, 11, 89–93. [Google Scholar] [CrossRef]
- Gaballah, K.; Faden, A.; Fakih, F.; Alsaadi, A.; Noshi, N.; Kujan, O. Diagnostic Accuracy of Oral Cancer and Suspicious Malignant Mucosal Changes among Future Dentists. Healthcare 2021, 9, 263. [Google Scholar] [CrossRef]
- Zimmermann, C.; Meurer, M.I.; de Lacerda, J.T.; de Mello, A.L.S.F.; Grando, L.J. The use of tools to support oral lesion description in oral medicine referrals. Braz. Oral Res. 2017, 31, e93. [Google Scholar] [CrossRef] [Green Version]
- Meurer, M.I.; Zimmermann, C.; Grando, L.J. Proposta de um roteiro de apoio à descrição de lesões bucais como instrumentalização para a comunicação profissional. Rev. Abeno 2015, 15, 2–15. [Google Scholar] [CrossRef]
- Hassona, Y.; Scully, C.; Abu Tarboush, N.; Baqain, Z.; Ismail, F.; Hawamdeh, S.; Sawair, F. Oral Cancer Knowledge and Diagnostic Ability Among Dental Students. J. Cancer Educ. 2015, 32, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Frola, M.I.; Barrios, R. Knowledge and Attitudes About Oral Cancer Among Dental Students After Bologna Plan Implementation. J. Cancer Educ. 2016, 32, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Roxo-Gonçalves, M.; Martins, M.A.T.; Martins, M.D.; Schmitz, C.A.A.; Moro, R.G.D.; D’Avila, O.P.; Rados, D.R.V.; Umpierre, R.N.; Gonçalves, M.R.; Carrard, V.C. Perceived usability of a store and forward telehealth platform for diagnosis and management of oral mucosal lesions: A cross-sectional study. PLoS ONE 2020, 15, e0233572. [Google Scholar] [CrossRef] [PubMed]
- Inquimbert, C.; Balacianu, I.; Huyghe, N.; Pasdeloup, J.; Tramini, P.; Meroueh, F.; Montal, S.; Bencharit, S.; Giraudeau, N. Applications of teledentistry in a French inmate population: A one-year observational study. PLoS ONE 2021, 16, e0247778. [Google Scholar] [CrossRef] [PubMed]
- Pei, L.; Wu, H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ. Online 2019, 24, 1666538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hew, K.F.; Lo, C.K. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soltanimehr, E.; Bahrampour, E.; Imani, M.M.; Rahimi, F.; Almasi, B.; Moattari, M. Effect of virtual versus traditional education on theoretical knowledge and reporting skills of dental students in radiographic interpretation of bony lesions of the jaw. BMC Med Educ. 2019, 19, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Luke, A.M.; Mathew, S.; Kuriadom, S.T.; George, J.M.; Karobari, M.I.; Marya, A.; Pawar, A.M. Effectiveness of Problem-Based Learning versus Traditional Teaching Methods in Improving Acquisition of Radiographic Interpretation Skills among Dental Students—A Systematic Review and Meta-Analysis. BioMed Res. Int. 2021, 2021, 1–19. [Google Scholar] [CrossRef]
- Approbationsordnung für Zahnärzte und Zahnärztinnen (ZApprO). 2019. Available online: https://www.gesetze-im-internet.de/zappro/BJNR093310019.html (accessed on 23 June 2021).

| Category | Scoring System | Maximum Score |
|---|---|---|
| Localization | 1 point for description | 1 |
| Size | 1 point for description | 2 |
| 1 point for classification | ||
| Type of lesion | 1 point for description | 2 |
| 1 point for classification | ||
| Surface and margin condition | 1 point for color description | 4 |
| 1 point for margin description | ||
| 1 point for surface description | ||
| 1 point for shape description | ||
| Total | 9 |
| Patient Number | Group | Students Diagnosis | Pathological Diagnosis |
|---|---|---|---|
| 1 | 1 | None | Aphtous stomatitis |
| 2 | 2 | Aphtous stomatitis | Oral lichen planus |
| 3 | 2 | Oral lichen planus | Oral leukoplakia |
| 4 | 2 | Oral lichen planus | Oral herpes simplex |
| 5 | 1 | Oral lichen planus | Oral herpes simplex |
| 6 | 1 | Oral lichen planus | Oral lichen planus |
| 7 | 1 | Oral squamous cell carcinoma | Oral leukoplakia |
| 8 | 2 | Oral leukoplakia | Oral leukoplakia |
| 9 | 1 | Fibrous tumor | Irritation fibroma |
| 10 | 1 | Oral leukoplakia | Oral herpes simplex |
| 11 | 2 | Oral lichen planus | Oral lichen planus |
| 12 | 1 | Oral squamous cell carcinoma | Oral leukoplakia |
| 13 | 2 | Oral lichen erosivus | Oral squamous cell carcinoma |
| 14 | 1 | Oral candidiasis | Oral leukoplakia |
| 15 | 1 | Oral leukoplakia | Oral leukoplakia |
| 16 | 1 | Oral lichen planus | Oral lichen planus |
| 17 | 2 | Oral leukoplakia | Oral lichen planus |
| 18 | 1 | Oral lichen planus | Oral graft-versus-host disease |
| 19 | 2 | Oral lichen erosivus | Oral lichen erosivus |
| 20 | 1 | Oral squamous cell carcinoma | Oral squamous cell carcinoma |
| 21 | 2 | Oral leukoplakia | Oral leukoplakia |
| 22 | 1 | None | Oral leukoplakia |
| 23 | 2 | Acute necrotizing ulcerative periodontitis | Oral lichen planus |
| 24 | 1 | Oral squamous cell carcinoma | Trauma of oral mucosa |
| 25 | 1 | Oral leukoplakia | Oral lichen planus |
| 26 | 2 | Oral squamous cell carcinoma | Oral squamous cell carcinoma |
| 27 | 1 | Oral squamous cell carcinoma | Oral squamous cell carcinoma |
| 28 | 2 | Oral leukoplakia | Oral squamous cell carcinoma |
| 29 | 1 | None | Oral lichen planus |
| 30 | 1 | Oral squamous cell carcinoma | Oral leukoplakia |
| 31 | 2 | Oral lichen planus | Oral lichen planus |
| 32 | 2 | Lupus erythematosus | Oral lichen planus |
| 33 | 1 | Oral erythroplakia | Oral lichen planus |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roeschmann, N.; Rau, A.; Kesting, M.R.; Maier, E.; Buchbender, M. A Prospective Comparative Analysis Regarding the Assessment of Oral Mucosal Disease Using a Validated Questionnaire to Improve the Teaching of Dental Students. Int. J. Environ. Res. Public Health 2022, 19, 9663. https://doi.org/10.3390/ijerph19159663
Roeschmann N, Rau A, Kesting MR, Maier E, Buchbender M. A Prospective Comparative Analysis Regarding the Assessment of Oral Mucosal Disease Using a Validated Questionnaire to Improve the Teaching of Dental Students. International Journal of Environmental Research and Public Health. 2022; 19(15):9663. https://doi.org/10.3390/ijerph19159663
Chicago/Turabian StyleRoeschmann, Nico, Andrea Rau, Marco R. Kesting, Eva Maier, and Mayte Buchbender. 2022. "A Prospective Comparative Analysis Regarding the Assessment of Oral Mucosal Disease Using a Validated Questionnaire to Improve the Teaching of Dental Students" International Journal of Environmental Research and Public Health 19, no. 15: 9663. https://doi.org/10.3390/ijerph19159663
APA StyleRoeschmann, N., Rau, A., Kesting, M. R., Maier, E., & Buchbender, M. (2022). A Prospective Comparative Analysis Regarding the Assessment of Oral Mucosal Disease Using a Validated Questionnaire to Improve the Teaching of Dental Students. International Journal of Environmental Research and Public Health, 19(15), 9663. https://doi.org/10.3390/ijerph19159663