The Effects of Using a Low-Cost and Easily Accessible Exercise Toolkit Incorporated to the Governmental Health Program on Community-Dwelling Older Adults: A Quasi-Experimental Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Intervention
2.2. Assessments
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Population Ageing 2017. Available online: https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Report.pdf (accessed on 20 May 2022).
- Population Projections for the R.O.C. (Taiwan): 2018–2065. Available online: https://pop-proj.ndc.gov.tw/main_en/dataSearch.aspx?uid=78&pid=78 (accessed on 20 May 2022).
- Cheng, S.J.; Yang, Y.R.; Cheng, F.Y.; Chen, I.H.; Wang, R.Y. The Changes of Muscle Strength and Functional Activities during Aging in Male and Female Populations. Int. J. Gerontol. 2014, 8, 197–202. [Google Scholar] [CrossRef]
- Ishizaki, T.; Furuna, T.; Yoshida, Y.; Iwasa, H.; Shimada, H.; Yoshida, H.; Kumagai, S.; Suzuki, T.; TMIG-LISA Research Group. Declines in Physical Performance by Sex and Age among Nondisabled Community-Dwelling Older Japanese during a 6-year Period. J. Epidemiol. 2011, 21, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Auyeung, T.W.; Lee, S.W.; Leung, J.; Kwok, T.; Woo, J. Age-associated Decline of Muscle Mass, Grip Strength and Gait Speed: A 4-year Longitudinal Study of 3018 Community-Dwelling Older Chinese. Geriatr. Gerontol. Int. 2014, 14, 76–84. [Google Scholar] [CrossRef]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Lee, S.; Lee, S.C.; Harada, K.; Hotta, R.; Nakakubo, S.; Bae, S.; et al. Age-Dependent Changes in Physical Performance and Body Composition in Community-Dwelling Japanese Older Adults. J. Cachexia Sarcopenia Muscle 2017, 8, 607–614. [Google Scholar] [CrossRef]
- Wang, C.Y.; Yeh, C.J.; Wang, C.W.; Wang, C.F.; Lin, Y.L. The Health Benefits Following Regular Ongoing Exercise Lifestyle in Independent Community-Dwelling Older Taiwanese Adults. Australas. J. Ageing 2011, 30, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Makizako, H.; Shimada, H.; Doi, T.; Tsutsumimoto, K.; Suzuki, T. Impact of Physical Frailty on Disability in Community-Dwelling Older Adults: A Prospective Cohort Study. BMJ Open 2015, 5, e008462. [Google Scholar] [CrossRef]
- da Silva, V.D.; Tribess, S.; Meneguci, J.; Sasaki, J.E.; Garcia-Meneguci, C.A.; Virtuoso, J.S., Jr. Association between Frailty and the Combination of Physical Activity Level and Sedentary Behavior in Older Adults. BMC Public Health 2019, 19, 709. [Google Scholar] [CrossRef]
- Río, X.; Larrinaga-Undabarrena, A.; Coca, A.; Guerra-Balic, M. Reference Values for Handgrip Strength in the Basque Country Elderly Population. Biology 2020, 9, 414. [Google Scholar] [CrossRef]
- Cesari, M.; Prince, M.; Thiyagarajan, J.A.; De Carvalho, I.A.; Bernabei, R.; Chan, P.; Gutierrez-Robledo, L.M.; Michel, J.P.; Morley, J.E.; Ong, P.; et al. Frailty: An emerging public health priority. J. Am. Med. Dir. Assoc. 2016, 17, 188–192. [Google Scholar] [CrossRef]
- Ren, P.; Zhang, X.; Du, L.; Pan, Y.; Chen, S.; He, Q. Reallocating Time Spent in Physical Activity, Sedentary Behavior and Its Association with Fear of Falling: Isotemporal Substitution Model. Int. J. Environ. Res. Public Health 2022, 19, 2938. [Google Scholar] [CrossRef]
- Petrescu-Prahova, M.G.; Eagen, T.J.; Fishleder, S.L.; Belza, B. Enhance® Fitness Dissemination and Implementation, 2010–2015: A Scoping Review. Am. J. Prev. Med. 2017, 52, S295–S299. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.S.; Thralls, K.J.; Goble, D.J.; Krippes, T.B. Effects of a Community-Based Exercise Program on Older Adults’ Physical Function, Activities of Daily Living, and Exercise Self-Efficacy: Feeling Fit Club. J. Appl. Gerontol. 2020, 39, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Iwao, Y.; Shigeishi, H.; Takahashi, S.; Uchida, S.; Kawano, S.; Sugiyama, M. Improvement of Physical and Oral Function in Community-Dwelling Older People after a 3-month Long-Term Care Prevention Program Including Physical Exercise, Oral Health Instruction, and Nutritional Guidance. Clin. Exp. Dent. Res. 2019, 5, 611–619. [Google Scholar] [CrossRef]
- Shinkai, S.; Yoshida, H.; Taniguchi, Y.; Murayama, H.; Nishi, M.; Amano, H.; Nofuji, Y.; Seino, S.; Fujiwara, Y. Public Health Approach to Preventing Frailty in the Community and its Effect on Healthy Aging in Japan. Geriatr. Gerontol. Int. 2016, 16, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.Y.; Huang, C.S. Aging in Taiwan: Building a Society for Active Aging and Aging in Place. Gerontologist 2016, 56, 176–183. [Google Scholar] [CrossRef] [PubMed]
- Senior Welfare: Establishing Community Care Stations. Available online: https://www.sfaa.gov.tw/SFAA/Eng/Pages/VDetail.aspx?nodeid=234&pid=3791 (accessed on 20 May 2022).
- Chang, K.S.; Tsai, W.H.; Tsai, C.H.; Yeh, H.I.; Chiu, P.H.; Chang, Y.W.; Chen, H.Y.; Tsai, J.M.; Lee, S.C. Effects of Health Education Programs for the Elders in Community Care Centers–Evaluated by Health Promotion Behaviors. Int. J. Gerontol. 2017, 11, 109–113. [Google Scholar] [CrossRef]
- Liang, C.C.; Change, Q.X.; Hung, Y.C.; Chen, C.C.; Lin, C.H.; Wei, Y.C.; Chen, J.C. Effects of a Community Care Station Program with Structured Exercise Intervention on Physical Performance and Balance in Community-Dwelling Older Adults: A Prospective 2-Year Observational Study. J. Aging Phys. Act. 2017, 25, 596–603. [Google Scholar] [CrossRef]
- Valdés-Badilla, P.A.; Gutiérrez-García, C.; Pérez-Gutiérrez, M.; Vargas-Vitoria, R.; López-Fuenzalida, A. Effects of Physical Activity Governmental Programs on Health Status in Independent Older Adults: A Systematic Review. J. Aging Phys. Act. 2019, 27, 265–275. [Google Scholar] [CrossRef]
- Fien, S.; Linton, C.; Mitchell, J.S.; Wadsworth, D.P.; Szabo, H.; Askew, C.D.; Schaumberg, M.A. Characteristics of Community-Based Exercise Programs for Community-Dwelling Older Adults in Rural/Regional Areas: A Scoping Review. Aging Clin. Exp. Res. 2022, 34, 1511–1528. [Google Scholar] [CrossRef]
- Aartolahti, E.; Lönnroos, E.; Hartikainen, S.; Häkkinen, A. Long-Term Strength and Balance Training in Prevention of Decline in Muscle Strength and Mobility in Older Adults. Aging Clin. Exp. Res. 2020, 32, 59–66. [Google Scholar] [CrossRef]
- Chan, S.Y.; Kuo, C.C.; Chen, K.M.; Tseng, W.S.; Huang, H.T.; Li, C.H. Health Promotion Outcomes of a Newly Developed Elastic Band Exercise Program for Older Adults in the Community: A Pilot Test. J. Nurs. Res. 2016, 24, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.M.; Chen, M.H.; Hong, S.M.; Chao, H.C.; Lin, H.S.; Li, C.H. Physical Fitness of Older Adults in Senior Activity Centres After 24-Week Silver Yoga Exercises. J. Clin. Nurs. 2008, 17, 2634–2646. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Chen, K.M.; Tsai, H.Y.; Huang, H.T.; Cheng, Y.Y.; Tsai, A.Y. Self-Perceived Health and Sleep Quality of Community Older Adults after Acupunch Exercises. Am. J. Geriatr. Psychiatry 2018, 26, 511–520. [Google Scholar] [CrossRef]
- Wang, J.; Chen, C.Y.; Lai, L.J.; Chen, M.L.; Chen, M.Y. The Effectiveness of a Community-Based Health Promotion Program for Rural Elders: A Quasi-Experimental Design. Appl. Nurs. Res. 2014, 27, 181–185. [Google Scholar] [CrossRef]
- Gonçalves, A.K.; Griebler, E.M.; da Silva, W.A.; Sant Helena, D.P.; da Silva, P.C.; Possamai, V.D.; Martins, V.F. Does a Multicomponent Exercise Program Improve Physical Fitness in Older Adults? Findings from A 5-Year Longitudinal Study. J. Aging Phys. Act. 2021, 29, 814–821. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Macera, C.A.; Castaneda-Sceppa, C. Physical Activity and Public Health in Older Adults: Recommendation from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1435–1445. [Google Scholar] [CrossRef] [PubMed]
- Monteagudo, P.; Cordellat, A.; Roldán, A.; Gómez-Cabrera, M.C.; Pesce, C.; Blasco-Lafarga, C. Exploring Potential Benefits of Accumulated Multicomponent-Training in Non-Active Older Adults: From Physical Fitness to Mental Health. Int. J. Environ. Res. Public Health 2021, 18, 9645. [Google Scholar] [CrossRef]
- Pfeiffer, E. A Short Portable Mental Status Questionnaire for the Assessment of Organic Brain Deficit in Elderly Patients. J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Berg, K.; Wood-Dauphinee, S.; Williams, J.I.; Gayton, D. Measuring Balance in the Elderly: Preliminary Development of an Instrument. Physiother. Can. 1989, 41, 304–311. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical Bases of Perceived Exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful Change and Responsiveness in Common Physical Performance Measures in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
- Vellas, B.J.; Rubenstein, L.Z.; Ousset, P.J.; Faisant, C.; Kostek, V.; Nourhashemi, F.; Allard, M.; Albarede, J.L. One-Leg Standing Balance and Functional Status in a Population of 512 Community-Living Elderly Persons. Aging Clin. Exp. Res. 1997, 9, 95–98. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.R.; Hwang, H.F.; Hu, M.H.; Wu, H.D.; Wang, Y.W.; Huang, F.C. Psychometric Comparisons of The Timed Up and Go, One-Leg Stand, Functional Reach, and Tinetti Balance Measures in Community-Dwelling Older People. J. Am. Geriatr. Soc. 2004, 52, 1343–1348. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Schaubert, K. Long-Term Reliability of the Timed Up-and-Go Test among Community-Dwelling Elders. J. Phys. Ther. Sci. 2005, 17, 93–96. [Google Scholar] [CrossRef][Green Version]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the Reliability and Validity of a Shorter Walk Test Compared with the 10-Meter Walk Test for Measurements of Gait Speed in Healthy, Older Adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short Physical Performance Battery and All-Cause Mortality: Systematic Review and Meta-Analysis. BMC Med. 2016, 14, 215. [Google Scholar] [CrossRef]
- Franco, M.R.; Tong, A.; Howard, K.; Sherrington, C.; Ferreira, P.H.; Pinto, R.Z.; Ferreira, M.L. Older People’s Perspectives on Participation in Physical Activity: A Systematic Review and Thematic Synthesis of Qualitative Literature. Br. J. Sports Med. 2015, 49, 1268–1276. [Google Scholar] [CrossRef]
- Borde, R.; Hortobágyi, T.; Granacher, U. Dose-Response Relationships of Resistance Training in Healthy Old Adults: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 1693–1720. [Google Scholar] [CrossRef]
- Layne, J.E.; Sampson, S.E.; Mallio, C.J.; Hibberd, P.L.; Griffith, J.L.; Das, S.K.; Flanagan, W.J.; Castaneda-Sceppa, C. Successful Dissemination of a Community-Based Strength Training Program for Older Adults by Peer and Professional Leaders: The People Exercising Program. J. Am. Geriatr. Soc. 2008, 56, 2323–2329. [Google Scholar] [CrossRef]
- Lim, S.E.R.; Cox, N.J.; Tan, Q.Y.; Ibrahim, K.; Roberts, H.C. Volunteer-Led Physical Activity Interventions to Improve Health Outcomes for Community-Dwelling Older People: A Systematic Review. Aging Clin. Exp. Res. 2021, 33, 843–853. [Google Scholar] [CrossRef]

| Name of the Test | Objective | Skill Evaluated or Conditional Capacity | Relevant Clinical Cutoff Values |
|---|---|---|---|
| Short Physical Performance Battery (SPPB) | to evaluate lower extremity strength and physical mobility | Balance test: close feet, semi-tandem to tandem position without support Lower extremity strength: sit to stand X 5-time Gait ability: timed for walk 4 m | scores at or below 9 indicating mobility disability [34], all-cause mortality as cutoff 10 [39] |
| The one-leg stance (OLS) test | to assess postural steadiness while standing and screening for low functional level and frailty | to test one leg standing with flexing the opposite knee to allow the foot to clear the floor as long as possible | time < 5 s indicating more difficulty in transportation, high risk of functional dependency and frailty [35,36] |
| Functional reach (FR) | to evaluate the postural control and balance ability | the distance between the length of the middle-fingers’ tips and a maximal forward reach while maintaining 90° shoulder flexion and straight arms in the standing position | distance > 16 cm indicating low risk of fall and ADL disability [36] |
| The Timed Up and Go (TUG) | to determine the dynamic balance and fall risk | timed the individual rose from a chair, walked 3 m at a comfortable and safe pace, turned around, walked back to the chair, and sat down again | <13 s indicating high risk of fall; >16.5 s indicating high risk of ADL disability [36] |
| The 10 m walk test | functional mobility and walking ability | to record the time needed to walk to the mid-point of 10 m excluding the 5 m of each acceleration/deceleration phases | the Minimal Detectable Change values (MDC): 0.01–0.02 m/s; [38] cutoff for sarcopenia and frailty: 1 m/s [5,11] |
| Variables | Intervention Group (n = 42) | Control Group (n = 41) | p Value |
|---|---|---|---|
| Age (y) | 76.9 ± 7.3 | 77 ± 6.3 | 0.95 |
| Height (cm) | 153.5 ± 7.9 | 153.0 ± 7.8 | 0.78 |
| Weight (kg) | 59.3 ± 12.4 | 58.0 ± 9.8 | 0.61 |
| Body mass index | 25.0 ± 4.0 | 24.7 ± 2.9 | 0.68 |
| Gender | 0.85 | ||
| Female | 11 (26) | 10 (24) | |
| Male | 31 (74) | 31 (76) | |
| Education | 0.1 | ||
| Illiterate | 21 (50) | 12 (29) | |
| Elementary school | 17 (40) | 20 (49) | |
| Junior height school and above | 4 (10) | 9 (22) | |
| Chronic disease | |||
| Hypertension | 23 (55) | 22 (54) | 0.92 |
| Diabetes | 14 (33) | 12 (29) | 0.69 |
| Heart disease | 10 (24) | 12 (29) | 0.57 |
| Arthritis | 9 (21) | 7 (17) | 0.62 |
| Stroke | 4 (10) | 0 (0) | 0.12 |
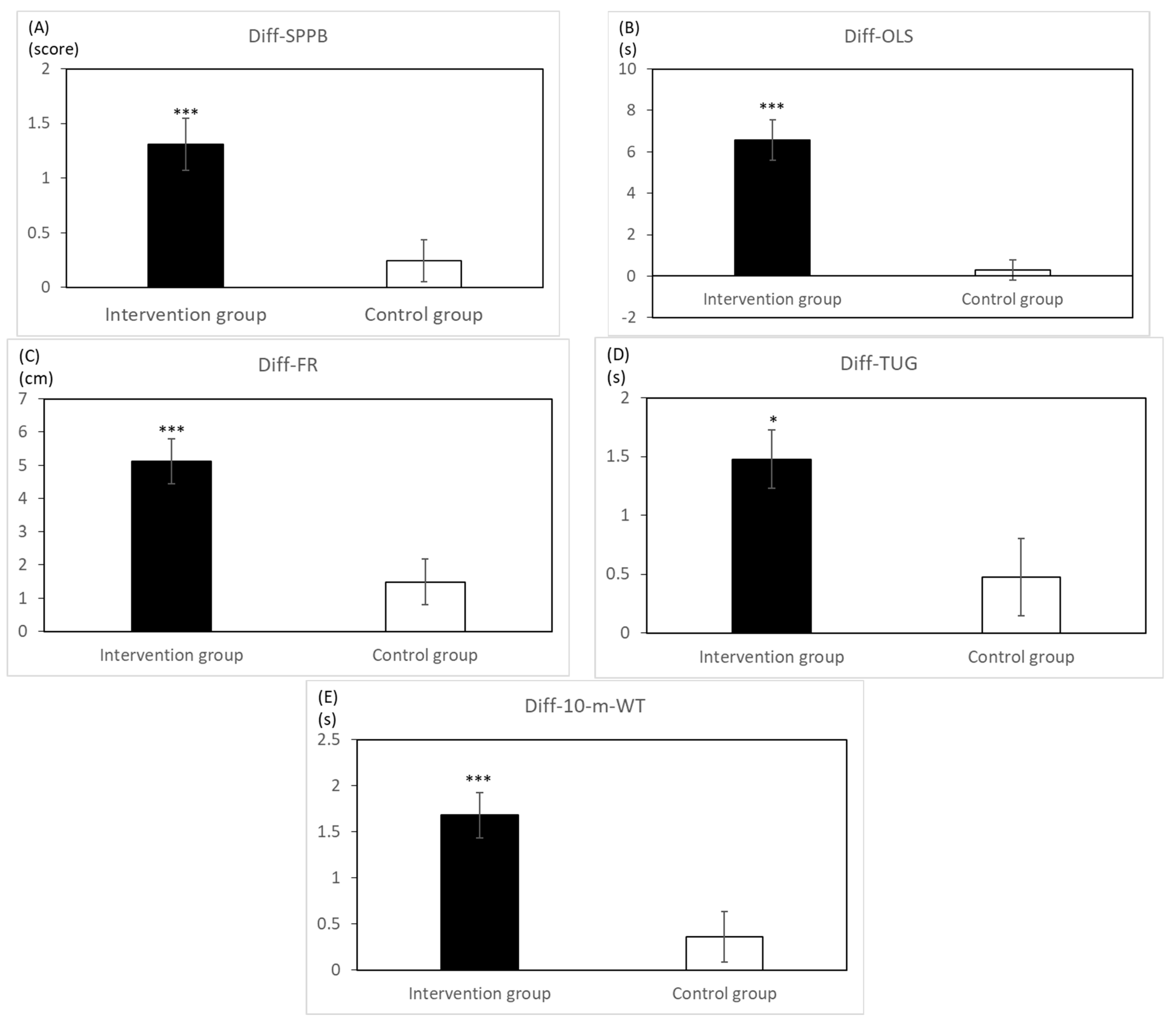
| Variables | Intervention Group (n = 42) | Control Group (n = 41) | Main Effect (Group) | Main Effect (Time) | Interaction (Group × Time) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Pre-Test | Post-Test | |||||||||||
| Mean | (SD) | Mean | (SD) | Mean | (SD) | Mean | (SD) | F | p | F | p | F | p | |
| SPPB | 10.0 | (1.9) | 11.3 | (1.4) | 9.7 | (2.3) | 9.9 | (2.5) | 3.60 | 0.06 | 26.24 | <0.01 | 12.35 | <0.01 |
| One leg stance (s) | 6.0 | (5.4) | 12.5 | (8.6) | 9.5 | (10.6) | 9.8 | (10.7) | 0.05 | 0.83 | 40.09 | <0.01 | 33.49 | <0.01 |
| Forward reach (cm) | 14.8 | (5.3) | 19.9 | (4.5) | 15.0 | (6.7) | 16.5 | (5.2) | 2.23 | 0.14 | 48.22 | <0.01 | 14.50 | <0.01 |
| TUG (s) | 11.1 | (3.3) | 9.6 | (3.1) | 11.8 | (4.5) | 11.3 | (4.5) | 2.16 | 0.15 | 23.24 | <0.01 | 6.15 | 0.02 |
| 10-m WT (s) | 10.6 | (2.9) | 8.9 | (2.3) | 11.0 | (3.9) | 10.6 | (4.1) | 2.25 | 0.14 | 31.43 | <0.01 | 13.28 | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, S.-H.; Chang, Q.-X.; Liang, C.-C.; Chen, J.-C. The Effects of Using a Low-Cost and Easily Accessible Exercise Toolkit Incorporated to the Governmental Health Program on Community-Dwelling Older Adults: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2022, 19, 9614. https://doi.org/10.3390/ijerph19159614
Yang S-H, Chang Q-X, Liang C-C, Chen J-C. The Effects of Using a Low-Cost and Easily Accessible Exercise Toolkit Incorporated to the Governmental Health Program on Community-Dwelling Older Adults: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9614. https://doi.org/10.3390/ijerph19159614
Chicago/Turabian StyleYang, Shih-Hsien, Qi-Xing Chang, Chung-Chao Liang, and Jia-Ching Chen. 2022. "The Effects of Using a Low-Cost and Easily Accessible Exercise Toolkit Incorporated to the Governmental Health Program on Community-Dwelling Older Adults: A Quasi-Experimental Study" International Journal of Environmental Research and Public Health 19, no. 15: 9614. https://doi.org/10.3390/ijerph19159614
APA StyleYang, S.-H., Chang, Q.-X., Liang, C.-C., & Chen, J.-C. (2022). The Effects of Using a Low-Cost and Easily Accessible Exercise Toolkit Incorporated to the Governmental Health Program on Community-Dwelling Older Adults: A Quasi-Experimental Study. International Journal of Environmental Research and Public Health, 19(15), 9614. https://doi.org/10.3390/ijerph19159614






