Exploring the Associated Factors of Depression, Anxiety, and Stress among Healthcare Shift Workers during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
2.2. Ethical Aspects of the Study
2.3. Questionnaires and Data Collection
2.4. Statistical Analysis
3. Results
3.1. Background of the Participants
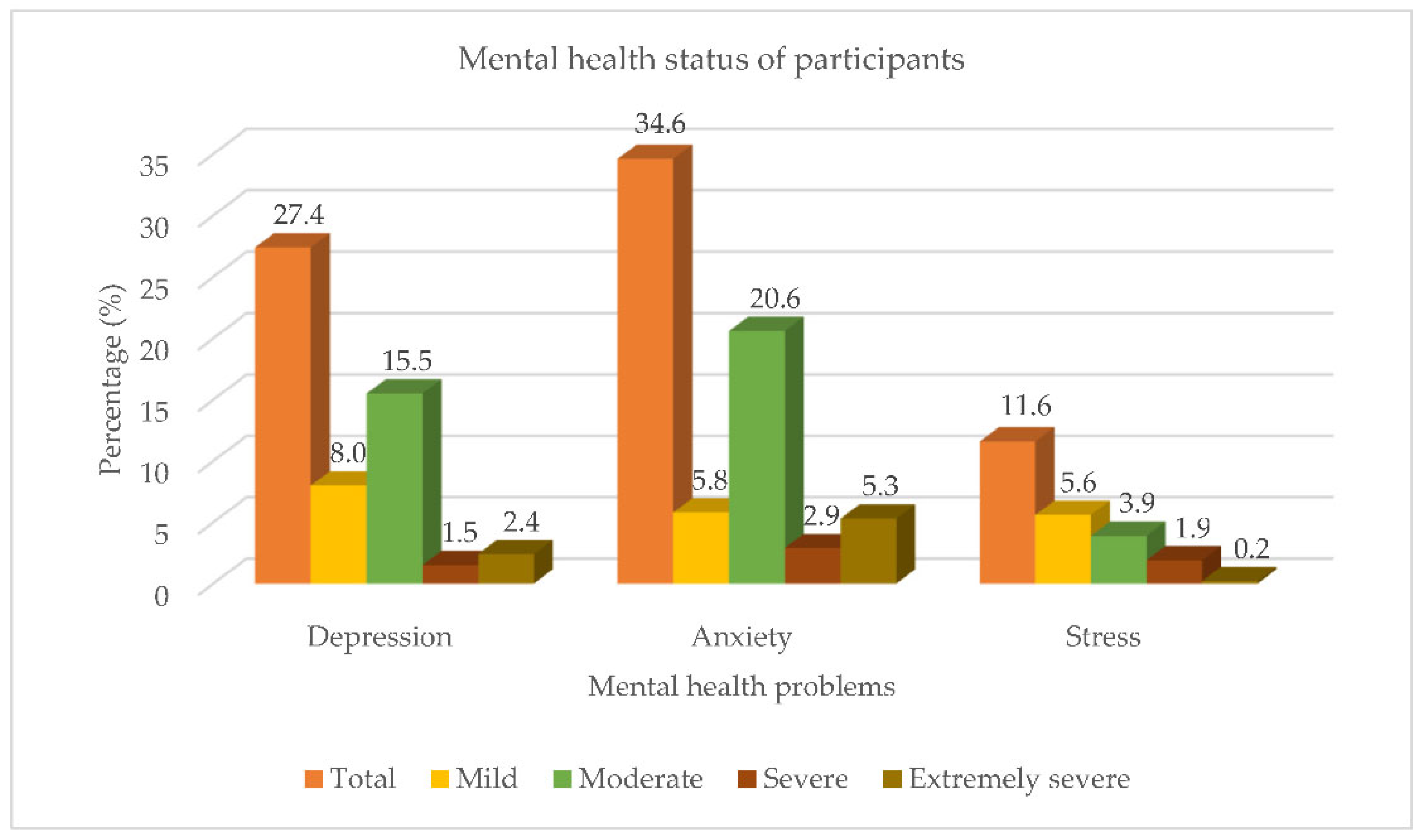
3.2. Mental Health Status
3.3. Sleep Quality, Physical Activities and Eating Habits of the Participants
3.4. Factors Associated with Depression, Anxiety and Stress of the Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mohd Azmi, N.A.S.; Juliana, N.; Mohd Fahmi Teng, N.I.; Azmani, S.; Das, S.; Effendy, N. Consequences of Circadian Disruption in Shift Workers on Chrononutrition and their Psychosocial Well-Being. Int. J. Environ. Res. Public Health 2020, 17, 2043. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Cao, D.; Huang, Y.; Chen, Z.; Wang, R.; Dong, Q.; Wei, Q.; Liu, L. Sleep duration and health outcomes: An umbrella review. Sleep Breath. 2021. [Google Scholar] [CrossRef] [PubMed]
- Roslan, N.S.; Yusoff, M.S.B.; Asrenee, A.R.; Morgan, K. Burnout prevalence and its associated factors among Malaysian healthcare workers during COVID-19 pandemic: An embedded mixed-method study. Healthcare 2021, 9, 90. [Google Scholar] [CrossRef] [PubMed]
- Sahimi, H.M.S.; Mohd Daud, T.I.; Chan, L.F.; Shah, S.A.; Rahman, F.H.A.; Nik Jaafar, N.R. Depression and Suicidal Ideation in a Sample of Malaysian Healthcare Workers: A Preliminary Study During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 658174. [Google Scholar] [CrossRef] [PubMed]
- Azuddin, A.; Razak, Z.; Omar, N. A Year of Living under COVID-19. Part 1: How the Year-Long Pandemic Impacted Malaysians’ Overall Mental and Physical Well-Being. 2021. Available online: https://www.centre.my/post/covid-19-physical-mental-health (accessed on 10 June 2022).
- Fancourt, D.; Steptoe, A.; Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. Lancet Psychiatry 2021, 8, 141–149. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Huang, H. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kapetanos, K.; Mazeri, S.; Constantinou, D.; Vavlitou, A.; Karaiskakis, M.; Kourouzidou, D. Exploring the factors associated with the mental health of frontline healthcare workers during the COVID-19 pandemic in Cyprus. PLoS ONE 2021, 16, e0258475. [Google Scholar] [CrossRef]
- Izzudin, M.P.B.E.; Al-Bedri, A.; Subramaniam, V.; Matthews, P.; Theng, C.A. Prevalence and related factors of depression among healthcare personnel at primary healthcare centers. Depression 2018, 6, 4–5. [Google Scholar]
- Maidstone, R.; Anderson, S.G.; Ray, D.W.; Rutter, M.K.; Durrington, H.J.; Blaikley, J.F. Shift work is associated with positive COVID-19 status in hospitalised patients. Thorax 2021, 76, 601–606. [Google Scholar] [CrossRef]
- Rowlands, A.V.; Gillies, C.; Chudasama, Y.; Davies, M.J.; Islam, N.; Kloecker, D.E.; Khunti, K. Association of working shifts, inside and outside of healthcare, with severe COVID-19: An observational study. BMC Public Health 2021, 21, 773. [Google Scholar] [CrossRef] [PubMed]
- İlhan, B.; Küpeli, İ. Secondary traumatic stress, anxiety, and depression among emergency healthcare workers in the middle of the COVID-19 outbreak: A cross-sectional study. Am. J. Emerg. Med. 2022, 52, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Teo, I.; Nadarajan, G.D.; Ng, S.; Bhaskar, A.; Sung, S.C.; Cheung, Y.B.; Pan, F.T.; Haedar, A.; Gaerlan, F.J.; Ong, S.F.; et al. The Psychological Well-Being of Southeast Asian Frontline Healthcare Workers during COVID-19: A Multi-Country Study. Int. J. Environ. Res. Public Health 2022, 19, 6380. [Google Scholar] [CrossRef] [PubMed]
- Subhas, N.; Pang, N.T.-P.; Chua, W.-C.; Kamu, A.; Ho, C.-M.; David, I.S.; Goh, W.W.-L.; Gunasegaran, Y.I.; Tan, K.-A. The Cross-Sectional Relations of COVID-19 Fear and Stress to Psychological Distress among Frontline Healthcare Workers in Selangor, Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 10182. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.R.B.; Mussi, F.C.; Mota, T.N.; Lua, I.; Macedo, T.T.S.; Souza, A.R.; de Araújo, T.M. Psychosocial risk factors at work associated with the level of physical activity among motorcycle taxi drivers. Arch. Environ. Occup. Health 2020, 75, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Chu, A.H.Y.; Moy, F.M. Reliability and Validity of the Malay International Physical Activity Questionnaire (IPAQ-M) Among a Malay Population in Malaysia. Asia Pac. J. Public Health 2012, 27, NP2381–NP2389. [Google Scholar] [CrossRef]
- Subramaniam, K.; Low, W.Y.; Chinna, K.; Chin, K.F.; Krishnaswamy, S. Psychometric properties of the Malay version of the Dutch Eating Behaviour Questionnaire (DEBQ) in a sample of Malaysian adults attending a health care facility. Malays. J. Med. Sci. 2017, 24, 64–73. [Google Scholar] [CrossRef]
- Farah, N.M.; Saw Yee, T.; Mohd Rasdi, H.F. Self-Reported Sleep Quality Using the Malay Version of the Pittsburgh Sleep Quality Index (PSQI-M) in Malaysian Adults. Int. J. Environ. Res. Public Health 2019, 16, 4750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rusli, N.; Amrina, K.; Trived, S.; Loh, K.P.; Shashi, M. Construct validity and internal consistency reliability of the Malay version of the 21-item depression anxiety stress scale (Malay-DASS-21) among male outpatient clinic attendees in Johor. Med. J. Malays. 2017, 72, 264–270. [Google Scholar]
- Sweeney, E.; Cui, Y.; Yu, Z.M.; Dummer, T.J.B.; DeClercq, V.; Forbes, C.; Grandy, S.A.; Keats, M.R.; Adisesh, A. The association between mental health and shift work: Findings from the Atlantic PATH study. Prev. Med. 2021, 150, 106697. [Google Scholar] [CrossRef] [PubMed]
- Matarazzo, T.; Bravi, F.; Valpiani, G.; Morotti, C.; Martino, F.; Bombardi, S.; Bozzolan, M.; Longhitano, E.; Bardasi, P.; Roberto, D.V.; et al. CORONAcrisis—An Observational Study on the Experience of Healthcare Professionals in a University Hospital during a Pandemic Emergency. Int. J. Environ. Res. Public Health 2021, 18, 4250. [Google Scholar] [CrossRef]
- Lee, A.; Myung, S.-K.; Cho, J.J.; Jung, Y.-J.; Yoon, J.L.; Kim, M.Y. Night Shift Work and Risk of Depression: Meta-analysis of Observational Studies. J. Korean Med. Sci. 2017, 32, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Booker, L.A.; Barnes, M.; Alvaro, P.; Collins, A.; Chai-Coetzer, C.L.; McMahon, M.; Lockley, S.W.; Rajaratnam, S.M.W.; Howard, M.E.; Sletten, T.L. The role of sleep hygiene in the risk of Shift Work Disorder in nurses. Sleep 2019, 43, zsz228. [Google Scholar] [CrossRef]
- Zakaria, M.I.; Remeli, R.; Ahmad Shahamir, M.F.; Md Yusuf, M.H.; Azizah Ariffin, M.A.; Noor Azhar, A.M. Assessment of burnout among emergency medicine healthcare workers in a teaching hospital in Malaysia during COVID-19 pandemic. Hong Kong J. Emerg. Med. 2021, 28, 254–259. [Google Scholar] [CrossRef]
- Kit, L.P.; Abu Saad, H.; Jamaluddin, R.; Phing, C.H. Prevalence of Overweight and Obesity among Primary Healthcare Workers In Perak, Malaysia. IIUM Med. J. Malays. 2020, 19. [Google Scholar] [CrossRef]
- Singh, N.K.D.; Loo, J.L.; Ko, A.M.N.; Husain, S.S.; Dony, J.F.; Sharizman, S.A.R.S. Obesity and mental health issues among healthcare workers: A cross-sectional study in Sabah, Malaysia. J. Health Res. 2021. [Google Scholar] [CrossRef]
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritising the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef] [PubMed]
- Elbay, R.Y.; Kurtulmuş, A.; Arpacıoğlu, S.; Karadere, E. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res. 2020, 290, 113–130. [Google Scholar] [CrossRef]
- Arafa, A.; Mohammed, Z.; Mahmoud, O.; Elshazley, M.; Ewis, A. Depressed, anxious, and stressed: What have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J. Affect. Disord. 2021, 278, 365–371. [Google Scholar] [CrossRef]
- Shanafelt, T.D.; West, C.P.; Sinsky, C.; Trockel, M.; Tutty, M.; Satele, D.V. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin. Proc. 2019, 94, 1681–1694. [Google Scholar] [CrossRef] [Green Version]
- Vizheh, M.; Qorbani, M.; Arzaghi, S.M.; Muhidin, S.; Javanmard, Z.; Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020, 19, 1967–1978. [Google Scholar] [CrossRef]
- Alnazly, E.; Khraisat, O.M.; Al-Bashaireh, A.M.; Bryant, C.L. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. PLoS ONE 2021, 16, e0247679. [Google Scholar] [CrossRef] [PubMed]
- Salaton, N.F.; Bulgiba, A. Depression, Anxiety, and Stress Among Frontline Primary Health Care Workers During the COVID-19 Pandemic. Asia Pac. J. Public Health 2022, 34, 416–419. [Google Scholar] [CrossRef]
- Li, Y.; Scherer, N.; Felix, L.; Kuper, H. Prevalence of depression, anxiety and posttraumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246454. [Google Scholar]
- James, S.M.; Honn, K.A.; Gaddameedhi, S.; Van Dongen, H.P.A. Shift Work: Disrupted Circadian Rhythms and Sleep-Implications for Health and Well-Being. Curr. Sleep Med. Rep. 2017, 3, 104–112. [Google Scholar] [CrossRef]
- Dai, C.; Qiu, H.; Huang, Q.; Hu, P.; Hong, X.; Tu, J.; Xie, Q.; Li, H.; Ren, W.; Ni, S.; et al. The effect of night shift on sleep quality and depressive symptoms among Chinese nurses. Neuropsychiatr. Dis. Treat. 2019, 15, 435–440. [Google Scholar] [CrossRef] [Green Version]
- Feng, H.L.; Qi, X.X.; Xia, C.L.; Xiao, S.Q.; Fan, L. Association between night shift and sleep quality and health among Chinese nurses: A cross-sectional study. J. Nurs. Manag. 2021, 29, 2123–2131. [Google Scholar] [CrossRef]
- Mohd Azmi, N.A.S.; Juliana, N.; Azmani, S.; Mohd Effendy, N.; Abu, I.F.; Mohd Fahmi Teng, N.I.; Das, S. Cortisol on Circadian Rhythm and Its Effect on Cardiovascular System. Int. J. Environ. Res. Public Health 2021, 18, 676. [Google Scholar] [CrossRef]
- Tsuno, N.; Besset, A.; Ritchie, K.; Clin, J. Sleep and depression. J. Clin. Psychiatry 2005, 66, 1254–1269. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.M.; Kim, H.Y.; Na, H.K.; Cho, K.H.; Chu, M.K. The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: A population-based study. Front. Neurol. 2019, 10, 849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnavita, N.; Tripepi, G.; Di Prinzio, R.R. Symptoms in Health Care Workers during the COVID-19 Epidemic. A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 5218. [Google Scholar] [CrossRef]
- Antunes, H.K.M.; Leite, G.S.F.; Lee, K.S.; Barreto, A.T.; Santos, R.V.T.; dos Souza, H. Exercise deprivation increases negative mood in exercise-addicted subjects and modifies their biochemical markers. Physiol. Behav. 2016, 156, 182–190. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Silva, L.R.B.; Seguro, C.S.; de Oliveira, C.G.A.; Santos, P.O.S.; de Oliveira, J.C.M.; de Souza Filho, L.F.M.; de Paula Júnior, C.A.; Gentil, P.; Rebelo, A.C.S. Physical Inactivity is Associated With Increased Levels of Anxiety, Depression, and Stress in Brazilians During the COVID-19 Pandemic: A Cross-Sectional Study. Front. Psychiatry 2020, 11, 565291. [Google Scholar] [CrossRef] [PubMed]
- Moussa, O.M.; Ardissino, M.; Kulatilake, P.; Faraj, A.; Muttoni, E.; Darzi, A.; Ziprin, P.; Scholtz, S.; Purkayastha, S. Effect of body mass index on depression in a UK cohort of 363,037 obese patients: A longitudinal analysis of transition. Clin. Obes. 2019, 9, e12305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, S.; Sun, Q.; Zhai, L.; Bai, Y.; Wei, W.; Jia, L. The Prevalence of Depression and Anxiety Symptoms among Overweight/Obese and Non-Overweight/Non-Obese Children/Adolescents in China: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 340. [Google Scholar] [CrossRef] [Green Version]
- Farsani, Z.K.; Khabazi, M. The Psychological Consequences of Obesity in Adolescent Girls: A Causal-Comparative Study. J. Kermanshah Univ. Med. Sci. 2020, 24, e102339. [Google Scholar]
- Luppino, F.S.; De Wit, L.M.; Bouvy, P.F. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry 2010, 67, 220–229. [Google Scholar] [CrossRef] [PubMed]
- De Wit, L.M.; Van Straten, A.; Van Herten, M.; Penninx, B.W.; Cuijpers, P. Depression and body mass index, a U-shaped association. BMC Public Health 2009, 9, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vittengl, J.R. Mediation of the bidirectional relations between obesity and depression among women. Psychiatry Res. 2018, 264, 254–259. [Google Scholar] [CrossRef]
- Anversa, R.G.; Muthmainah, M.; Sketriene, D.; Gogos, A.; Sumithran, P.; Brown, R.M. A review of sex differences in the mechanisms and drivers of overeating. Front. Neuroendocrinol. 2021, 63, 100941. [Google Scholar] [CrossRef] [PubMed]
- Herhaus, B.; Petrowski, K. The effect of restrained eating on acute stress-induced food intake in people with obesity. Appetite 2021, 159, 105045. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Adjepong, M.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Keaver, L.; Lee, H.; Ludy, M.-J.; Shen, W.; et al. Gender Differences in the Relationships between Perceived Stress, Eating Behaviors, Sleep, Dietary Risk, and Body Mass Index. Nutrients 2022, 14, 1045. [Google Scholar] [CrossRef] [PubMed]
- Moyo, I.; Ndou-Mammbona, A.A.; Mavhandu-Mudzusi, A.H. Challenges faced by healthcare workers at a central hospital in Zimbabwe after contracting COVID-19: An interpretive phenomenological analysis study. S. Afr. Fam. Pract. 2022, 64, a5428. [Google Scholar] [CrossRef] [PubMed]
| n | % | |
|---|---|---|
| Age | ||
| <40 years old | 368 | 89.1 |
| ≥40 years old | 43 | 10.4 |
| Gender | ||
| Men | 78 | 18.9 |
| Women | 335 | 81.1 |
| Ethnicity | ||
| Malays | 337 | 81.6 |
| Chinese | 12 | 2.9 |
| Indians | 47 | 11.4 |
| Others | 17 | 4.1 |
| Educational status | ||
| Secondary education | 27 | 6.5 |
| Post-secondary education | 12 | 2.9 |
| Diploma | 231 | 55.9 |
| Bachelor/postgraduate | 143 | 34.6 |
| Marital status | ||
| Single | 135 | 32.7 |
| Married | 275 | 66.6 |
| Divorced/separated/widowed | 3 | 0.7 |
| Household income *1 | ||
| Low (<MYR 4850) | 192 | 46.5 |
| Middle (MYR 4850–RM 10,959) | 207 | 50.1 |
| High (≥MYR 10,960) | 14 | 3.4 |
| Healthcare position | ||
| House officer | 47 | 11.4 |
| Medical officer | 91 | 22 |
| Nurse | 251 | 60.8 |
| Paramedics | 24 | 5.8 |
| Department | ||
| Emergency and trauma | 175 | 42.4 |
| Medical-based | 125 | 30.3 |
| Surgical-based | 113 | 27.4 |
| Part-time job involvement *2 | ||
| No | 369 | 89.3 |
| Yes | 44 | 10.7 |
| Comorbidities | ||
| No | 353 | 85.5 |
| Yes | 60 | 14.5 |
| Smoking/vaping status | ||
| No | 390 | 94.4 |
| Yes | 23 | 5.6 |
| Alcohol consumption | ||
| No | 399 | 96.6 |
| Yes | 14 | 3.4 |
| Body mass index (BMI) *3 | ||
| Underweight | 30 | 7.3 |
| Normal | 202 | 48.9 |
| Overweight | 107 | 25.9 |
| Obese | 74 | 17.9 |
| Mental Health Status | n (%) | Mean ± S.D. |
|---|---|---|
| DASS-21 | ||
| Depression | ||
| Mild (10–13) | 33 (8.0) | 15.61 ± 5.7 |
| Moderate (14–20) | 64 (15.5) | |
| Severe (21–27) | 6 (1.5) | |
| Extremely severe (28+) | 10 (2.4) | |
| Anxiety | ||
| Mild (8–9) | 24 (5.8) | 13.89 ± 5.5 |
| Moderate (10–14) | 85 (20.6) | |
| Severe (15–19) | 12 (2.9) | |
| Extremely severe (20+) | 22 (5.3) | |
| Stress | ||
| Mild (15–18) | 23 (5.6) | 21.04 ± 5.3 |
| Moderate (19–25) | 16 (3.9) | |
| Severe (26–33) | 8 (1.9) | |
| Extremely severe (34+) | 1 (0.2) |
| Factors (n) | DASS-21 Depression | |||||
|---|---|---|---|---|---|---|
| Normal (n) | Depression (n) | Crude OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Age group | ||||||
| <40 years old | 260 (70.8%) | 107 (29.2%) | 2.54 (1.0–6.2) | p = 0.041 * | 1.63 (0.6–4.3) | p = 0.319 |
| ≥40 years old | 37 (86.0%) | 6 (14.0%) | Ref | Ref | ||
| Gender | ||||||
| Male | 57 (73.1%) | 21 (26.9%) | Ref | Ref | ||
| Female | 242 (72.5%) | 92 (27.5%) | 1.03 (0.6–1.8) | p = 0.912 | 1.39 (0.7–2.9) | p = 0.374 |
| Marital status | ||||||
| Married | 209 (76.3%) | 65 (23.7%) | Ref | Ref | ||
| Single | 87 (64.4%) | 48 (35.6%) | 1.77 (1.1–2.8) | p = 0.012 * | 1.41 (0.8–2.4) | p = 0.207 |
| Divorced/separated/widowed | 3 (100.0%) | 0 (0.0%) | 0.00 (0.0–0.0) | p = 0.999 | 0.00 (0.0–0.0) | p = 0.999 |
| Healthcare position | ||||||
| Medical officer | 57 (62.6%) | 34 (37.4%) | Ref | Ref | ||
| House officer | 29 (61.7%) | 18 (38.3%) | 1.04 (0.5–2.1) | p = 0.914 | 1.16 (0.5–2.6) | p = 0.711 |
| Nurse | 193 (77.2%) | 57 (22.8%) | 0.50 (0.3–0.8) | p = 0.008 * | 0.63 (0.3–1.2) | p = 0.162 |
| Paramedics | 20 (83.3%) | 4 (16.7%) | 0.34 (0.1–1.1) | p = 0.064 | 0.40 (0.1–1.5) | p = 0.162 |
| Body mass index (BMI) | ||||||
| Underweight | 20 (66.7%) | 10 (33.3%) | 1.48 (0.7–3.4) | p = 0.350 | 1.51 (0.6–3.8) | p = 0.380 |
| Overweight | 80 (75.5%) | 26 (24.5%) | 0.96 (0.6–1.7) | p = 0.890 | 1.24 (0.7–2.3) | p = 0.479 |
| Obese | 48 (64.9%) | 26 (35.1%) | 1.60 (0.9–2.8) | p = 0.106 | 2.18 (1.1–4.2) | p = 0.018 * |
| Normal | 151 (74.8%) | 51 (25.2%) | Ref | Ref | ||
| Category of physical activity (IPAQ) | ||||||
| Inactive | 81 (61.8%) | 50 (38.2%) | 2.35 (1.3–4.3) | p = 0.005 * | 2.16 (1.1–4.1) | p = 0.019 * |
| Minimally active | 137 (76.5%) | 42 (23.5%) | 1.17 (0.6–2.1) | p = 0.607 | 1.16 (0.6–2.2) | p = 0.652 |
| HEPA active | 80 (79.2%) | 21 (20.8%) | Ref | Ref | ||
| Emotional eating habit (DEBQ) | ||||||
| Low score | 265 (74.0%) | 93 (26.0%) | Ref | Ref | ||
| High score | 34 (63.0%) | 20 (37.0%) | 1.68 (0.9–3.1) | p = 0.092 | 1.54 (0.8–3.0) | p = 0.207 |
| External eating habit (DEBQ) | ||||||
| Low score | 72 (79.1%) | 19 (20.9%) | Ref | Ref | ||
| High score | 227 (70.7%) | 94 (29.3%) | 1.57 (0.9–2.7) | p = 0.115 | 1.62 (0.8–3.1) | p = 0.146 |
| Restraint eating habit (DEBQ) | ||||||
| Low score | 106 (70.2%) | 45 (29.8%) | Ref | Ref | ||
| High score | 193 (73.9%) | 68 (26.1%) | 0.83 (0.5–1.3) | p = 0.412 | 0.76 (0.4–1.3) | p = 0.292 |
| Sleep quality (PSQI) | ||||||
| Good | 141 (82.5%) | 30 (17.5%) | Ref | Ref | ||
| Poor | 157 (65.4%) | 83 (34.6%) | 2.49 (1.5–4.0) | p < 0.001 * | 2.33 (1.4–3.9) | p = 0.001 * |
| Factors (n) | DASS-21 Anxiety | |||||
|---|---|---|---|---|---|---|
| Normal (n) | Anxiety (n) | Crude OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Age group | ||||||
| <40 years old | 230 (62.7%) | 137 (37.3%) | 3.67 (1.5–8.9) | p = 0.004 * | 3.29 (1.3–8.5) | p = 0.014 * |
| ≥40 years old | 37 (86.0%) | 6 (14.0%) | Ref | Ref | ||
| Gender | ||||||
| Male | 59 (75.6%) | 19 (24.4%) | Ref | Ref | ||
| Female | 210 (62.9%) | 124 (37.1%) | 1.83 (1.0–3.2) | p = 0.035 * | 1.65 (0.8–3.4) | p = 0.177 |
| Marital status | ||||||
| Married | 186 (67.9%) | 88 (32.1%) | Ref | Ref | ||
| Single | 80 (59.3%) | 55 (40.7%) | 1.45 (0.9–2.2) | p = 0.086 | 1.24 (0.7–2.1) | p = 0.414 |
| Divorced/separated/widowed | 3 (100.0%) | 0 (0.0%) | 0.00 (0.0–0.0) | p = 0.999 | 0.00 (0.0–0.0) | p = 0.999 |
| Healthcare position | ||||||
| Medical officer | 61 (67.0%) | 30 (33.0%) | Ref | Ref | ||
| House officer | 26 (55.3%) | 21 (44.7%) | 1.64 (0.8–3.4) | p = 0.178 | 1.53 (0.7–3.4) | p = 0.287 |
| Nurse | 162 (64.8%) | 88 (35.2%) | 1.11 (0.7–1.8) | p = 0.701 | 1.37 (0.7–2.6) | p = 0.338 |
| Paramedics | 20 (83.3%) | 4 (16.7%) | 0.41 (0.1–1.3) | p = 0.128 | 0.59 (0.2–2.1) | p = 0.423 |
| Body mass index (BMI) | ||||||
| Underweight | 16 (53.3%) | 14 (46.7%) | 1.51 (0.7–3.3) | p = 0.293 | 1.67 (0.7–4.0) | p = 0.251 |
| Overweight | 81 (76.4%) | 25 (23.6%) | 0.53 (0.3–0.9) | p = 0.021 * | 0.62 (0.4–1.1) | p = 0.107 |
| Obese | 44 (59.5%) | 30 (40.5%) | 1.18 (0.7–2.0) | p = 0.553 | 1.52 (0.8–2.8) | p = 0.175 |
| Normal | 128 (63.4%) | 74 (36.6%) | Ref | Ref | ||
| Category of physical activity (IPAQ) | ||||||
| Inactive | 79 (60.3%) | 52 (39.7%) | 1.80 (1.0–3.2) | p = 0.040 * | 2.00 (1.1–3.7) | p = 0.029 * |
| Minimally active | 115 (64.2%) | 64 (35.8%) | 1.53 (0.9–2.6) | p = 0.123 | 1.60 (0.9–2.9) | p = 0.112 |
| HEPA active | 74 (73.3%) | 27 (26.7%) | Ref | Ref | ||
| Emotional eating habit (DEBQ) | ||||||
| Low score | 242 (67.6%) | 116 (32.4%) | Ref | Ref | ||
| High score | 27 (50.0%) | 27 (50.0%) | 2.09 (1.2–3.7) | p = 0.013 * | 1.78 (0.9–3.4) | p = 0.074 |
| External eating habit (DEBQ) | ||||||
| Low score | 68 (74.7%) | 23 (25.3%) | Ref | Ref | ||
| High score | 201 (62.6%) | 120 (37.4%) | 1.77 (1.0–3.0) | p = 0.034 * | 1.66 (0.9–3.0) | p = 0.096 |
| Restraint eating habit (DEBQ) | ||||||
| Low score | 97 (64.2%) | 54 (35.8%) | Ref | Ref | ||
| High score | 172 (65.9%) | 89 (34.1%) | 0.93 (0.6–1.4) | p = 0.733 | 0.84 (0.5–1.4) | p = 0.486 |
| Sleep quality (PSQI) | ||||||
| Good | 127 (74.3%) | 44 (25.7%) | Ref | Ref | ||
| Poor | 141 (58.8%) | 99 (41.3%) | 2.03 (1.3–3.1) | p = 0.001 * | 2.09 (1.3–3.3) | p = 0.002 * |
| Factors (n) | DASS-21 Stress | |||||
|---|---|---|---|---|---|---|
| Normal (n) | Stress (n) | Crude OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Age group | ||||||
| <40 years old | 321 (87.5%) | 46 (12.5%) | 2.94 (0.7–12.6) | p = 0.146 | 1.21 (0.3–5.7) | p = 0.814 |
| ≥40 years old | 41 (95.3%) | 2 (4.7%) | Ref | Ref | ||
| Gender | ||||||
| Male | 67 (85.9%) | 11 (14.1%) | Ref | Ref | ||
| Female | 297 (88.9%) | 37 (11.1%) | 0.76 (0.4–1.6) | p = 0.455 | 1.11 (0.4–2.8) | p = 0.828 |
| Marital status | ||||||
| Married | 252 (92.0%) | 22 (8.0%) | Ref | Ref | ||
| Single | 109 (80.7%) | 26 (19.3%) | 2.73 (1.5–5.0) | p = 0.001 * | 2.05 (1.0–4.2) | p = 0.050 |
| Divorced/separated/widowed | 3 (100.0%) | 0 (0.0%) | 0.00 (0.0–0.0) | p = 0.999 | 0.00 (0.0–0.0) | p = 0.999 |
| Healthcare position | ||||||
| Medical officer | 76 (83.5%) | 15 (16.5%) | Ref | Ref | ||
| House officer | 37 (78.7%) | 10 (21.3%) | 1.37 (0.6–3.3) | p = 0.489 | 1.72 (0.6–4.7) | p = 0.287 |
| Nurse | 229 (91.6%) | 21 (8.4%) | 0.47 (0.2–0.9) | p = 0.035 * | 0.74 (0.3–1.8) | p = 0.500 |
| Paramedics | 22 (91.7%) | 2 (8.3%) | 0.46 (0.1–2.2) | p = 0.327 | 0.36 (0.1–2.1) | p = 0.255 |
| Body mass index (BMI) | ||||||
| Underweight | 25 (83.3%) | 5 (16.7%) | 1.64 (0.6–4.7) | p = 0.361 | 1.56 (0.5–5.0) | p = 0.456 |
| Overweight | 95 (89.6%) | 11 (10.4%) | 0.95 (0.4–2.0) | p = 0.890 | 1.47 (0.6–3.4) | p = 0.377 |
| Obese | 64 (86.5%) | 10 (13.5%) | 1.28 (0.6–2.8) | p = 0.547 | 2.11 (0.8–5.3) | p = 0.110 |
| Normal | 180 (89.1%) | 22 (10.9%) | Ref | Ref | ||
| Category of physical activity (IPAQ) | ||||||
| Inactive | 108 (82.4%) | 23 (17.6%) | 1.74 (0.8–3.8) | p = 0.158 | 1.44 (0.6–3.4) | p = 0.405 |
| Minimally active | 165 (92.2%) | 14 (7.8%) | 0.69 (0.3–1.6) | p = 0.389 | 0.61 (0.2–1.5) | p = 0.282 |
| HEPA active | 90 (89.1%) | 11 (10.9%) | Ref | Ref | ||
| Emotional eating habit (DEBQ) | ||||||
| Low score | 318 (88.8%) | 40 (11.2%) | Ref | Ref | ||
| High score | 46 (85.2%) | 8 (14.8%) | 1.38 (0.6–3.1) | p = 0.439 | 1.35 (0.5–3.4) | p = 0.522 |
| External eating habit (DEBQ) | ||||||
| Low score | 82 (90.1%) | 9 (9.9%) | Ref | Ref | ||
| High score | 282 (87.9%) | 39 (12.1%) | 1.26 (0.6–2.7) | p = 0.554 | 1.76 (0.7–4.3) | p = 0.215 |
| Restraint eating habit (DEBQ) | ||||||
| Low score | 124 (82.1%) | 27 (17.9%) | Ref | Ref | ||
| High score | 240 (92.0%) | 21 (8.0%) | 0.40 (0.2–0.7) | p = 0.003 * | 0.34 (0.2–0.7) | p = 0.003 * |
| Sleep quality (PSQI) | ||||||
| Good | 163 (95.3%) | 8 (4.7%) | Ref | Ref | ||
| Poor | 200 (83.3%) | 40 (16.7%) | 4.08 (1.9–9.0) | p < 0.001 * | 3.96 (1.7–9.1) | p = 0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Juliana, N.; Mohd Azmi, N.A.S.; Effendy, N.; Mohd Fahmi Teng, N.I.; Azmani, S.; Baharom, N.; Mohamad Yusuff, A.S.; Abu, I.F. Exploring the Associated Factors of Depression, Anxiety, and Stress among Healthcare Shift Workers during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 9420. https://doi.org/10.3390/ijerph19159420
Juliana N, Mohd Azmi NAS, Effendy N, Mohd Fahmi Teng NI, Azmani S, Baharom N, Mohamad Yusuff AS, Abu IF. Exploring the Associated Factors of Depression, Anxiety, and Stress among Healthcare Shift Workers during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(15):9420. https://doi.org/10.3390/ijerph19159420
Chicago/Turabian StyleJuliana, Norsham, Nor Amira Syahira Mohd Azmi, Nadia Effendy, Nur Islami Mohd Fahmi Teng, Sahar Azmani, Nizam Baharom, Aza Sherin Mohamad Yusuff, and Izuddin Fahmy Abu. 2022. "Exploring the Associated Factors of Depression, Anxiety, and Stress among Healthcare Shift Workers during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 15: 9420. https://doi.org/10.3390/ijerph19159420
APA StyleJuliana, N., Mohd Azmi, N. A. S., Effendy, N., Mohd Fahmi Teng, N. I., Azmani, S., Baharom, N., Mohamad Yusuff, A. S., & Abu, I. F. (2022). Exploring the Associated Factors of Depression, Anxiety, and Stress among Healthcare Shift Workers during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(15), 9420. https://doi.org/10.3390/ijerph19159420








