Clinical Efficacy of 1% CHX Gluconate Gel and 0.12% CHX Solution: A Randomized Controlled Trial
Abstract
1. Introduction
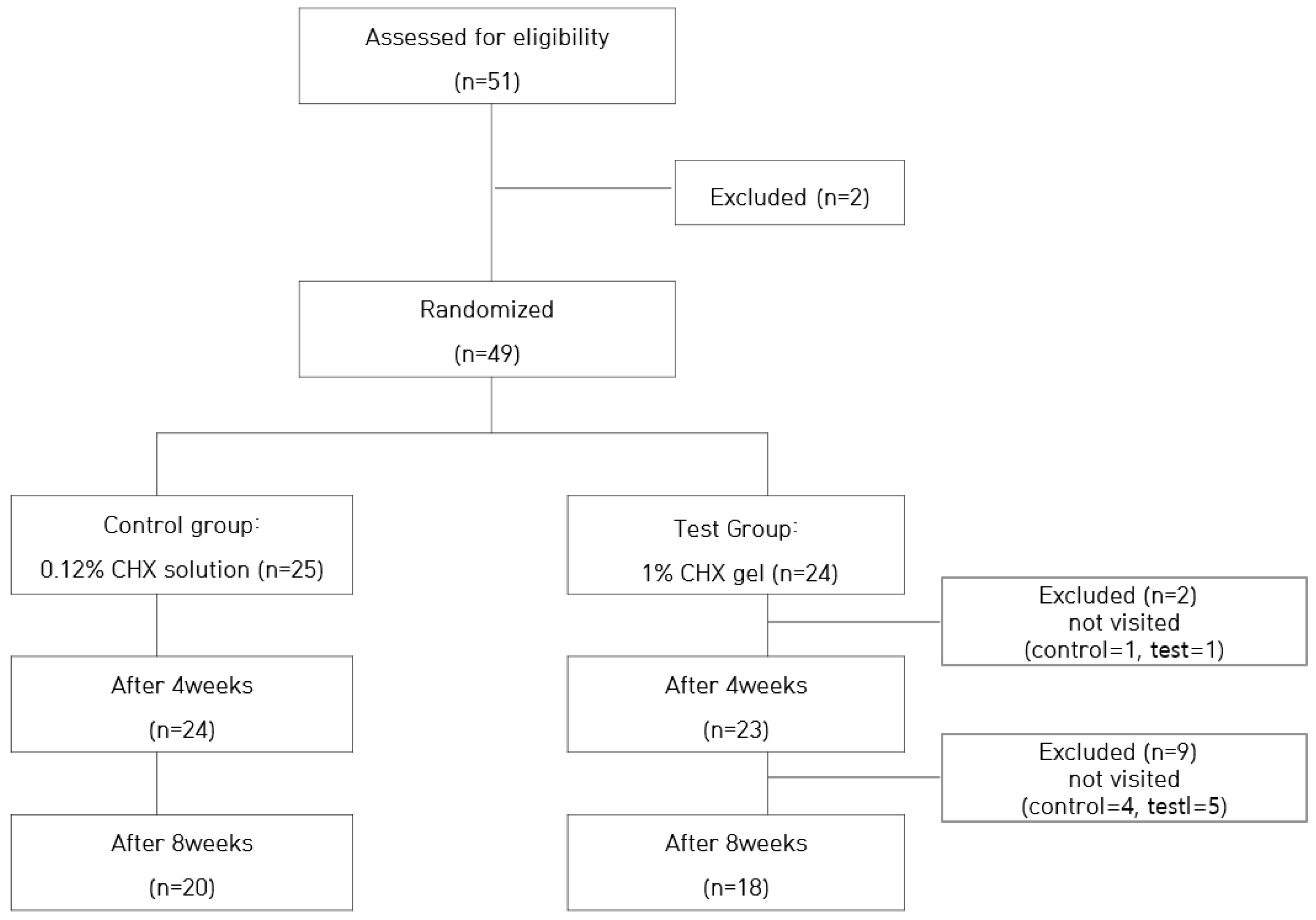
2. Materials and Methods
2.1. Study Design and Subjects
- adults of both sexes over 20 years,
- medically healthy subjects,
- at least 20 teeth remaining,
- understanding of the content and purpose of the study.
- poor oral hygiene,
- an allergic reaction to chlorhexidine,
- ≥5 mm periodontal pocket depth (PPD).
2.2. Clinical Protocol
2.3. Clinical Measurements
2.4. Statistical Analysis
3. Results
3.1. Changes of TQHPI and GI According to Treatment Period
3.2. Comparison between Groups by ∆Value of before and after Treatment
3.3. Bacterial Changes Pre -Intervention and Post-Intervention through BANA Test
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Darveau, R.P.; Tanner, A.; Page, R.C. The microbial challenge in periodontitis. Periodontol. 2000 1997, 14, 12–32. [Google Scholar] [CrossRef]
- Highfield, J. Diagnosis and classification of periodontal disease. Aust. Dent. J. 2009, 54, S11–S26. [Google Scholar] [CrossRef] [PubMed]
- Petersilka, G.J.; Ehmke, B.; Flemming, T.F. Antimicrobial effects of mechanical debridement. Periodontol. 2000 2002, 28, 56–71. [Google Scholar] [CrossRef] [PubMed]
- Gunsolley, J.C. Clinical efficacy of antimicrobial mouthrinses. J. Dent. 2010, 38, S6–S10. [Google Scholar] [CrossRef]
- Setu, M.; Tanu, M.; Rahul, S.; Rohit, K. Chlorhexidine: The gold standard in chemical plaque control. Natl. J. Physiol. Pharm. Pharmacol. 2011, 1, 45–50. [Google Scholar]
- Stanevičiūtė, E.; Builytė, I.U.; Ridziauskas, M.; Besusparis, J.; Kirkliauskienė, A.; Zabulis, V.; Davainis, L.; Valiūnaitė, G.; Triponis, V.; Sirvydis, V. Efficacy of antiseptic solutions in treatment of staphylococcus aureus infected surgical wounds with patches of vascular graft: An experimental study in rats. Medicina 2019, 55, 106. [Google Scholar] [CrossRef]
- Serra, E.; Hidalgo-Bastida, L.A.; Verran, J.; Williams, D.; Malic, S. Antifungal activity of commercial essential oils and biocides against Candida Albicans. Pathogens 2018, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- James, P.; Worthington, H.V.; Parnell, C.; Harding, M.; Lamont, T.; Cheung, A.; Whelton, H.; Riley, P. Chlorhexidine mouthrinse as an adjunctive treatment for gingival health. Cochrane Database Syst. Rev. 2017, 3, CD008676. [Google Scholar] [CrossRef] [PubMed]
- Chatzigiannidou, I.; Teughels, W.; Wiele, T.V.; Boon, N. Oral biofilms exposure to chlorhexidine results in altered microbial composition and metabolic profile. NPJ Biofilms Microbiomes 2020, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Calderini, A.; Pantoleo, G.; Rossi, A.; Gazzolo, D.; Polizzi, E. Adjunctive effect of chlorhexidine antiseptics in mechanical periodontal treatment: First results of a preliminary case series. Int. J. Dent. Hyg. 2013, 11, 180–185. [Google Scholar] [CrossRef]
- Berchier, C.E.; Slot, D.E.; Weijden, G.A. The efficacy of 0.12% chlorhexidine mouthrinse compared with 0.2% on plaque accumulation and periodontal parameters: A systematic review. J. Clin. Periodontol. 2010, 37, 829–839. [Google Scholar] [CrossRef]
- Stoeken, J.E.; Versteeg, P.A.; Rosema, N.A.M.; Timmerman, M.F.; Velden, U.; Weijden, G.A. Inhibition of “De Novo” plaque formation with 0.12% chlorhexidine spray compared to 0.2%s and 0.2% chlorhexidine mouthwash. J. Periodontol. 2007, 78, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Supranoto, S.C.; Slot, D.E.; Addy, M.; Weijden, G.A. The effect of chlorhexidine dentifrice or gel versus chlorhexidine mouthwash on plaque, gingivitis, bleeding and tooth discoloration: A systematic review. Int. J. Dent. Hyg. 2015, 13, 83–92. [Google Scholar] [CrossRef]
- Haraji, A.; Rakhshan, V. Single-dose intra-alveolar chlorhexidine gel application, easier surgeries and younger ages are associated with reduced dry socket risk. J. Oral. Maxillofac. Surg. 2014, 72, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Heitz-Mayfield, L.J.A.; Salvi, G.E.; Botticelli, D.; Mombelli, A.; Faddy, M.; Lang, N.P. Anti-infective treatment of peri-implant mucositis: A randomised controlled clinical trial. Clin. Oral. Implant. Res. 2011, 22, 237–241. [Google Scholar] [CrossRef] [PubMed]
- He, T.; Mazor, S.; Zou, Y.; Grender, J.; Farrell, S.; Sagel, P.; Biesbrock, A.R.; Timm, H.; Zini, A. Randomized clinical trial assessing anti-gingivitis efficacy of two stannous fluoride dentifrices and zinc/arginine dentifrice. Am. J. Dent. 2021, 34, 110–115. [Google Scholar] [PubMed]
- Loesche, W.J.; Bretz, W.A.; Kerschensteiner, D.; Stoll, J.; Socransky, S.S.; Hujoel, P.; Lopatin, D.E. Development of a diagnostic test for anaerobic periodontal infections based on plaque hydrolysis of benzoyl-DL-arginine-naphthylamide. J. Clin. Microbiol. 1990, 28, 1551–1559. [Google Scholar] [CrossRef]
- McCoy, L.C.; Wehler, C.J.; Rich, S.E.; Garcia, R.I.; Miller, D.R.; Jones, J.A. Adverse events associated with chlorhexidine use: Results from the Department of Veterans Affairs Dental Diabetes Study. J. Am. Dent. Assoc. 2008, 139, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Asbi, T.; Hussein, H.A.; Horwitz, J.; Gabay, E.; Machtei, E.E.; Giladi, H.Z. A single application of chlorhexidine gel reduces gingival inflammation and interleukin 1-β following one-stage implant placement: A randomized controlled study. Clin. Implant. Dent. Relat. Res. 2021, 23, 726–734. [Google Scholar] [CrossRef] [PubMed]
- Löe, H.; Silness, J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol. Scand. 1963, 21, 533–551. [Google Scholar] [CrossRef] [PubMed]
- Cugini, M.A.; Thompson, M.; Warren, P.R. Correlations between two plaque indices in assessment of toothbrush effectiveness. J. Contemp. Dent. Pract. 2006, 7, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Richards, D. Chlorhexidine mouthwash more effective than dentifrice or gel. Evid. Based Dent. 2015, 16, 59. [Google Scholar] [CrossRef] [PubMed]
- Siena, F.D.; Francetti, L.; Corbella, S.; Taschieri, S.; Fabbro, M.D. Topical application of 1% chlorhexidine gel versus 0.2% mouthwash in the treatment of peri-implant mucositis. An observational study. Int. J. Dent. Hyg. 2013, 11, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Slot, D.E.; Rosema, N.A.M.; Hennequin-Hoenderdos, N.L.; Versteeg, P.A.; Van Der Velden, U.; Van Der Weijden, G.A. The effect of 1% chlorhexidine gel and 0.12% dentifrice gel on plaque accumulation: A 3-day non-brushing model. Int. J. Dent. Hyg. 2010, 8, 294–300. [Google Scholar] [CrossRef]
- Wang, C.S.; Arnold, R.R.; Trope, M.; Teixeira, F.B. Clinical efficiency of 2% chlorhexidine gel in reducing intracanal bacteria. J. Endod. 2007, 33, 1283–1289. [Google Scholar] [CrossRef]
- Komorowski, R.; Grad, H.; Wu, X.Y.; Friedman, S. Antimicrobial substantivity of chlorhexidine treated bovine root dentin. J. Endod. 2000, 6, 315–317. [Google Scholar] [CrossRef]
- Woodland Hills Compounding Pharmacy. 2022. Available online: https://www.woodlandhillspharmacy.com/compounds/dentistry/chlorhexidine/ (accessed on 23 June 2022).
- Ferraz, C.C.; Gomes, B.P.; Zaia, A.A.; Teixeira, F.B.; Souza-Filho, F.J. In vitro assessment of the antimicrobial action and mechanical ability or chlorhexidine gel as an endodontic irrigant. J. Endod. 2001, 27, 452–455. [Google Scholar] [CrossRef]
- Gomes, B.P.F.A.; Souza, S.F.C.; Ferraz, C.C.R.; Teixeira, F.B.; Zaia, A.A.; Valdrighi, L.; Souza-Filho, F.J. Effectiveness of 2% chlorhexidine gel and calcium hydroxide against Enterococcus faecalis in bovine root dentine in vitro. Int. Endod. J. 2003, 36, 267–275. [Google Scholar] [CrossRef]
- Lorez, K.; Bruhn, G.; Netuschil, L.; Heumann, C.; Hoffmann, T. How to select study designs and parameters to investigate the effect of mouthrinses? Part I: Rationale and background. J. Physiol. Pharmacol. 2009, 60, 77–83. [Google Scholar]
- de Andrade, J.A.; Feres, M.; de Figueiredo, L.C.; Salvador, S.L.; Cortelli, S.C. The ability of the BANA test to detect different levels of P. gingivalis, T. denticola and T. forsythia. Braz. Oral. Res. 2010, 24, 224–230. [Google Scholar] [CrossRef][Green Version]
- Dhalla, N.; Patil, S.; Chaubey, K.K.; Narula, I.S. The detection of BANA micro-organisms in adult periodontitis before and after scaling and root planing by BANA-Enzymatic™ test kit: An in vivo study. J. Indian Soc. Periodontol. 2015, 19, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Hita-Iglesias, P.; Torres-Lagares, D.; Flores-Ruiz, R.; Magallanes-Abad, N.; Basallote-Gonzalez, M.; Gutierrez-Perez, J.L. Effectiveness of chlorhexidine gel versus chlorhexidine rinse in reducing alveolar osteitis in mandibular third molar sugery. J. Oral. Maxillofac. Surg. 2008, 66, 441–445. [Google Scholar] [CrossRef] [PubMed]
- Souza-Filho, F.J.; Soares, A.J.; Vianna, M.E.; Zaia, A.A.; Ferraz, C.C.R.; Gomes, B.P.F.A. Antimicrobial effect and pH of chlorhexidine gel and calcium hydroxide alone and associated with other materials. Braz. Dent. J. 2008, 19, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Chlorhexidine gel use in the oral district: A systematic review. Gels 2019, 5, 31. [Google Scholar] [CrossRef] [PubMed]
| Group | N | Baseline | 4 Weeks | 8 Weeks | p | |
|---|---|---|---|---|---|---|
| TQHPI | Control | 20 | 1.04 ± 0.29 | 0.59 ± 0.32 | 0.76 ± 0.22 | <0.001 |
| Test | 18 | 1.00 ± 0.29 | 0.46 ± 0.24 | 0.58 ± 0.26 | ||
| GI | Control | 20 | 1.77 ± 0.25 | 1.23 ± 0.20 | 1.36 ± 0.23 | <0.001 |
| Test | 18 | 1.91 ± 0.15 | 1.21 ± 0.13 | 1.26 ± 0.27 |
| Group | N | ∆Value of 4 Weeks—Baseline | ∆Value of 8 Weeks—Baseline | |
|---|---|---|---|---|
| TQHPI | Control | 20 | 0.44 ± 0.31 | 0.27 ± 0.36 |
| Test | 18 | 0.53 ± 0.30 | 0.41 ± 0.37 | |
| p | 0.40 | 0.26 | ||
| GI | Control | 20 | 0.54 ± 0.22 | 0.41 ± 0.34 |
| Test | 18 | 0.70 ± 0.15 | 0.65 ± 0.29 | |
| p | 0.01 | 0.03 |
| Group | N | Baseline | 8 Weeks | p * |
|---|---|---|---|---|
| Control | 20 | 1.25 ± 0.71 | 1.05 ± 0.51 | <0.001 |
| Test | 18 | 1.28 ± 0.82 | 0.44 ± 0.61 | <0.001 |
| p ** | 0.91 | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-Y.; Nam, E.-J. Clinical Efficacy of 1% CHX Gluconate Gel and 0.12% CHX Solution: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 9358. https://doi.org/10.3390/ijerph19159358
Lee S-Y, Nam E-J. Clinical Efficacy of 1% CHX Gluconate Gel and 0.12% CHX Solution: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(15):9358. https://doi.org/10.3390/ijerph19159358
Chicago/Turabian StyleLee, Su-Young, and Eun-Joo Nam. 2022. "Clinical Efficacy of 1% CHX Gluconate Gel and 0.12% CHX Solution: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 15: 9358. https://doi.org/10.3390/ijerph19159358
APA StyleLee, S.-Y., & Nam, E.-J. (2022). Clinical Efficacy of 1% CHX Gluconate Gel and 0.12% CHX Solution: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(15), 9358. https://doi.org/10.3390/ijerph19159358






