Effects of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Selection Criteria
2.3.1. Inclusion Criteria
2.3.2. Exclusion Criteria
2.4. Study Selection and Data Extraction
2.5. Risk of Bias
2.6. Data Analysis and Synthesis
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk-of-Bias Assessment
3.4. Meta-Analysis
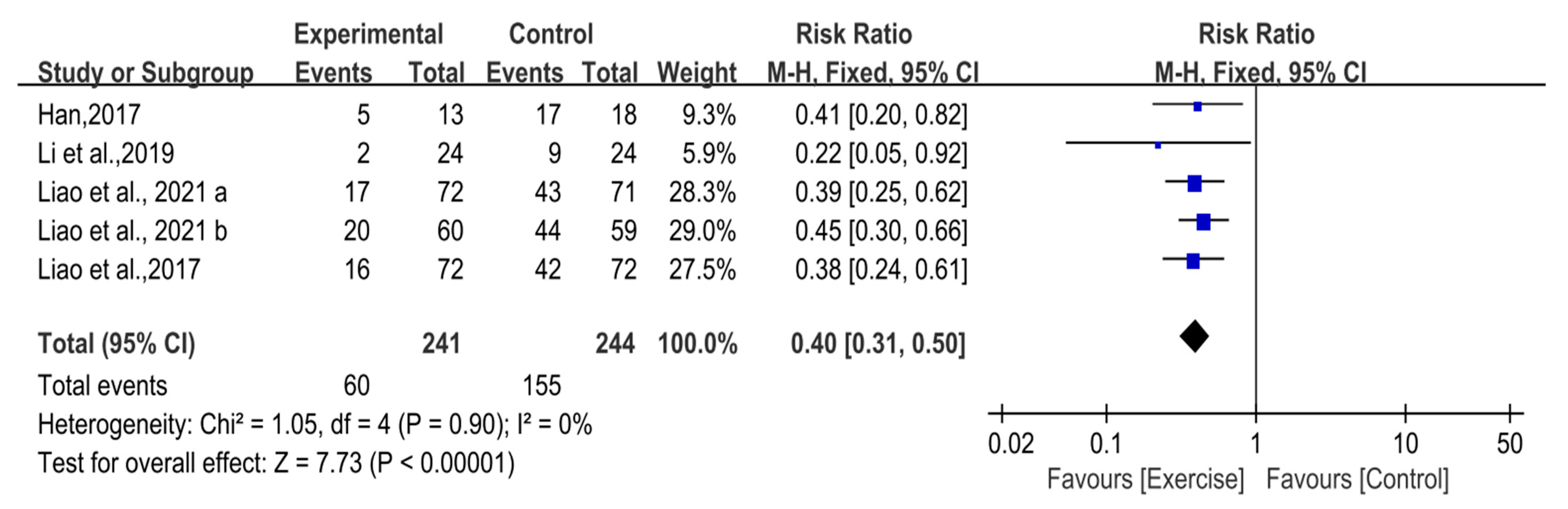
3.4.1. Asymmetry Functional Patterns
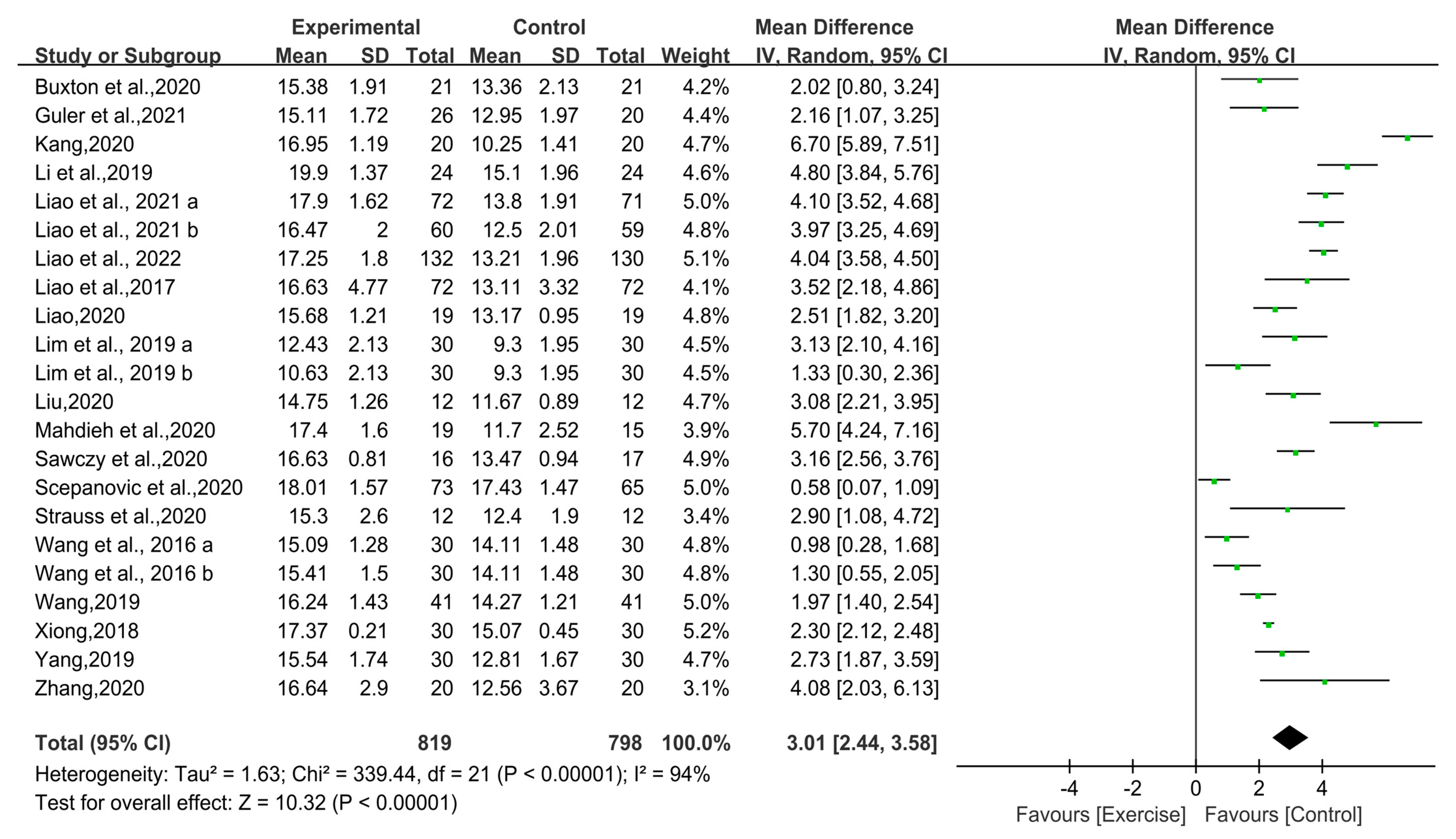
3.4.2. FMS Composite Scores
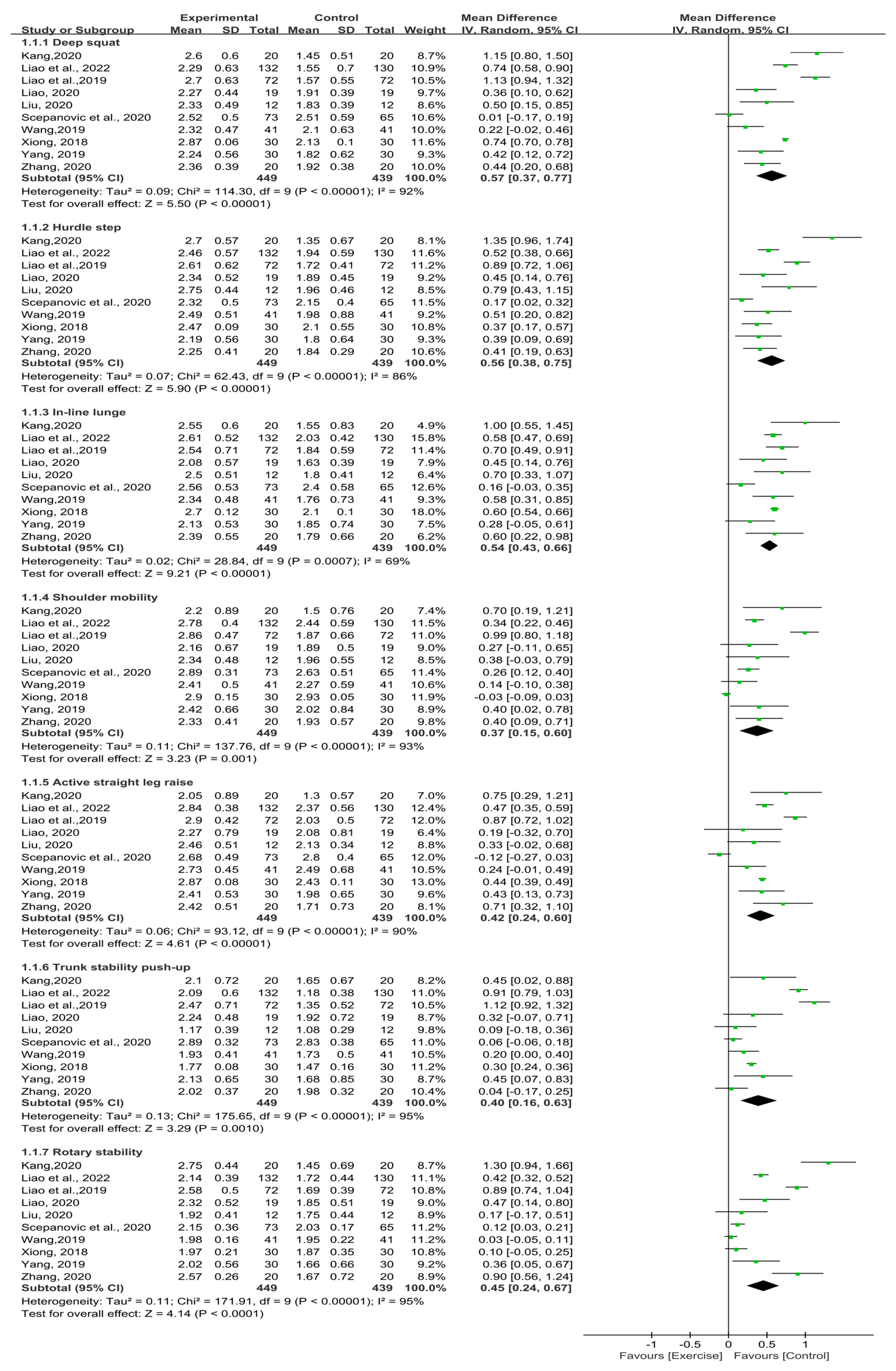
3.4.3. FMS Individual Scores
3.5. Subgroup Analysis
3.6. Sensitivity Analysis
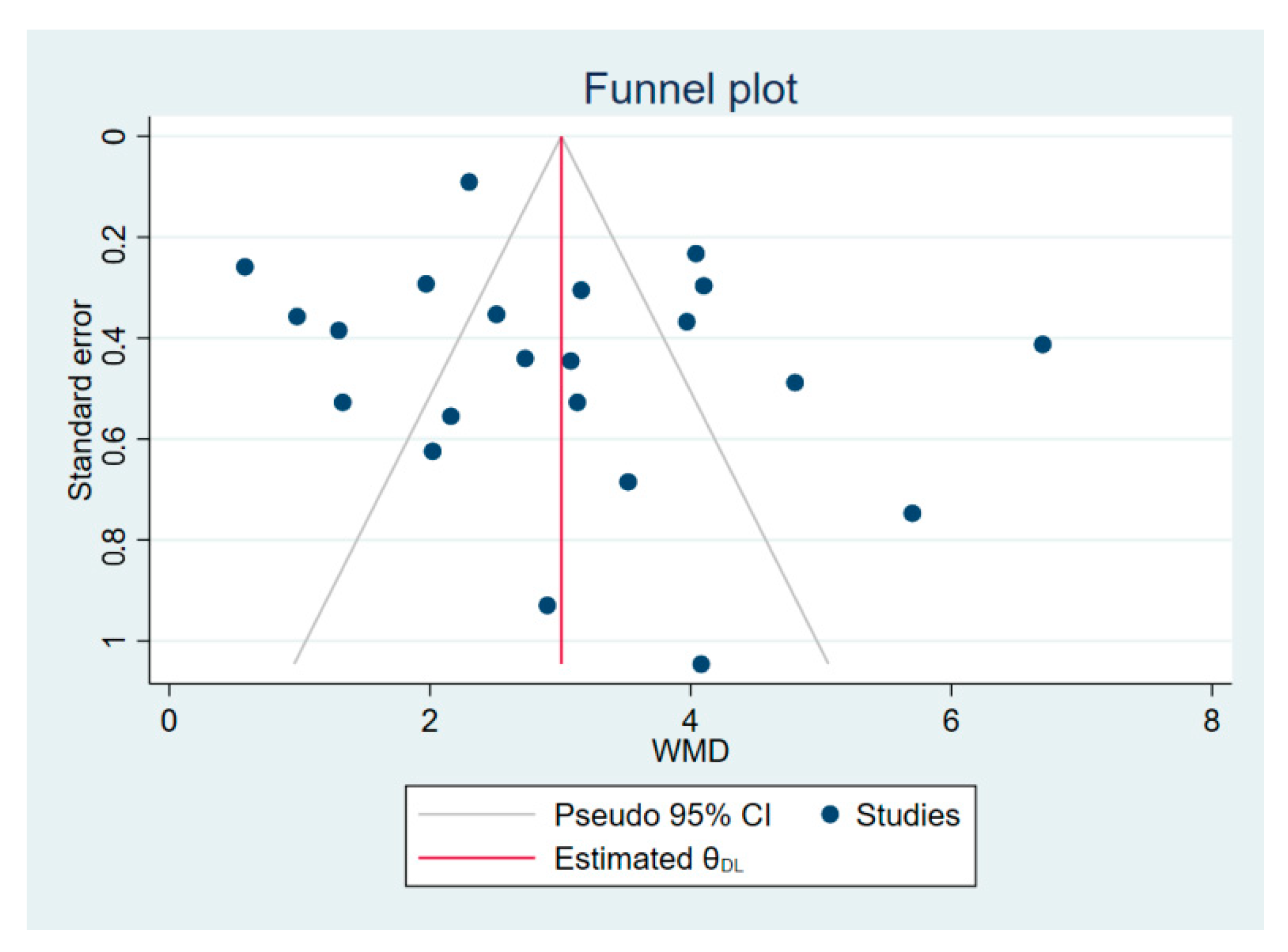
3.7. Publication Bias
4. Discussion
4.1. Effect of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations
4.2. Subgroup Analysis of FMS Composite Scores
4.3. Sensitivity Analysis
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 1. Int. J. Sports Phys. Ther. 2014, 9, 396–409. [Google Scholar] [PubMed]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional movement screening: The use of fundamental movements as an assessment of function—Part 2. Int. J. Sports Phys. Ther. 2014, 9, 549–563. [Google Scholar]
- O’Brien, W.; Khodaverdi, Z.; Bolger, L.; Tarantino, G.; Philpott, C.; Neville, R.D. The Assessment of Functional Movement in Children and Adolescents: A Systematic Review and Meta-Analysis. Sports Med. 2022, 52, 37–53. [Google Scholar] [CrossRef]
- Patel, D.R.; Nelson, T.L. Sports injuries in adolescents. Med. Clin. N. Am. 2000, 84, 983–1007. [Google Scholar] [CrossRef]
- Boden, B.P.; Dean, G.S.; Feagin, J.J.; Garrett, W.J. Mechanisms of anterior cruciate ligament injury. Orthopedics 2000, 23, 573–578. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Kiesel, K.; Bryant, M.; Torine, J. Movement: Functional Movement Systems: Screening, Assessment, and Corrective Strategies; On Target Publications: Santa Cruz, CA, USA, 2010; Volume 24, pp. 123–127. [Google Scholar]
- Sahrmann, S. Diagnosis and Treatment of Movement Impairment Syndromes; Elsevier Health Sciences: Alpharetta, CA, USA, 2002; pp. 107–112. [Google Scholar]
- Mahdieh, L.; Zolaktaf, V.; Karimi, M.T. Effects of dynamic neuromuscular stabilization (DNS) training on functional movements. Hum. Mov. Sci. 2020, 70, 102568. [Google Scholar] [CrossRef]
- Cook, G.; Burton, L.; Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 1. N. Am. J. Sports Phys. Ther. 2006, 1, 62–72. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 2. N. Am. J. Sports Phys. Ther. 2006, 1, 132–139. [Google Scholar] [PubMed]
- Bonazza, N.A.; Smuin, D.; Onks, C.A.; Silvis, M.L.; Dhawan, A. Reliability, Validity, and Injury Predictive Value of the Functional Movement Screen: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2017, 45, 725–732. [Google Scholar] [CrossRef]
- Scudamore, E.M.; Stevens, S.L.; Fuller, D.K.; Coons, J.M.; Morgan, D.W. Use of Functional Movement Screen Scores to Predict Dynamic Balance in Physically Active Men and Women. J. Strength Cond. Res. 2019, 33, 1848–1854. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.W.; Pavlovic, A.; Barlow, C.E.; Leonard, D.; DeFina, J.R.; Willis, B.L.; DeFina, L.F.; Haskell, W.L. Functional Movement Screening Performance and Association With Key Health Markers in Older Adults. J. Strength Cond. Res. 2021, 35, 3021–3027. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.; Rodrigues, L.P.; Clemente, F.M.; Cancela, J.M.; Bezerra, P. Association between motor competence and Functional Movement Screen scores. PeerJ 2019, 7, e7270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, M.; Youm, C.; Noh, B.; Park, H. Low composite functional movement screen score associated with decline of gait stability in young adults. PeerJ 2021, 9, e11356. [Google Scholar] [CrossRef] [PubMed]
- Bodden, J.G.; Needham, R.A.; Chockalingam, N. The Effect of an Intervention Program on Functional Movement Screen Test Scores in Mixed Martial Arts Athletes. J. Strength Cond. Res. 2015, 29, 219–225. [Google Scholar] [CrossRef] [Green Version]
- Dinc, E.; Kilinc, B.E.; Bulat, M.; Erten, Y.T.; Bayraktar, B. Effects of special exercise programs on functional movement screen scores and injury prevention in preprofessional young football players. J. Exerc. Rehabil. 2017, 13, 535–540. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiesel, K.; Plisky, P.; Butler, R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand. J. Med. Sci. Sports 2011, 21, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Basar, M.J.; Stanek, J.M.; Dodd, D.D.; Begalle, R.L. The Influence of Corrective Exercises on Functional Movement Screen and Physical Fitness Performance in Army ROTC Cadets. J. Sport Rehabil. 2019, 28, 360–367. [Google Scholar] [CrossRef] [Green Version]
- Jafari, M.; Zolaktaf, V.; Ghasemi, G. Functional Movement Screen Composite Scores in Firefighters: Effects of Corrective Exercise Training. J. Sport Rehabil. 2020, 29, 102–106. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, C.; Chen, S.; Zhao, Y. Effects of functional correction training on injury risk of athletes: A systematic review and meta-analysis. PeerJ 2021, 9, e11089. [Google Scholar] [CrossRef]
- Shim, Y.; Choi, H.; Shin, W. Aerobic training with rhythmic functional movement: Influence on cardiopulmonary function, functional movement and Quality of life in the elderly women. J. Hum. Sport Exerc. 2019, 14, 748–756. [Google Scholar] [CrossRef]
- Roh, S.Y. A functional movement screening of college students performing Pilates exercise. J. Cosmet. Med. 2019, 3, 33–37. [Google Scholar] [CrossRef]
- Wright, M.D.; Portas, M.D.; Evans, V.J.; Weston, M. The Effectiveness of 4 Weeks of Fundamental Movement Training on Functional Movement Screen and Physiological Performance in Physically Active Children. J. Strength Cond. Res. 2015, 29, 254–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Impellizzeri, F.M.; Bizzini, M. Systematic review and meta-analysis: A primer. Int. J. Sports Phys. Ther. 2012, 7, 493–503. [Google Scholar] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Higgins, J.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.; Welch, V. Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021). Available online: www.training.cochrane.org/handbook (accessed on 8 April 2022).
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [Green Version]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Egger, M.; Smith, G.D. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001, 323, 101–105. [Google Scholar] [CrossRef]
- Kang, Z.C. An empirical Study on the Influence of Functional Training on Physical Fitness of Children Aged 8–12 Years; Northwest Normal University: Lanzhou, China, 2020. [Google Scholar]
- Wang, P. Experimental Study on the Correction of College Students’ bad Action Patterns by Fitness Yoga; Henan University: Zhengzhou, China, 2019. [Google Scholar]
- Liu, J.W. Experimental Study on the Influence of Wu Qinxi on FMS Results of the Elderly; Hebei Normal University: Shijiazhuang, China, 2020. [Google Scholar]
- Xiong, H. The Effect of Yoga Practice on the Basic Athletic Ability of Middle-Aged Women; Hunan Normal University: Changsha, China, 2018. [Google Scholar]
- Liao, T.; Li, L.; Wang, Y.T. Effects of Functional Strength Training Program on Movement Quality and Fitness Performance Among Girls Aged 12–13 Years. J. Strength Cond. Res. 2019, 33, 1534–1541. [Google Scholar] [CrossRef]
- Strauss, A.T.; Parr, A.J.; Desmond, D.J.; Vargas, A.T.; Baker, R.T. The Effect of Total Motion Release on Functional Movement Screen Composite Scores: A Randomized Controlled Trial. J. Sport Rehabil. 2020, 29, 1106–1114. [Google Scholar] [CrossRef] [PubMed]
- Sawczyn, M. Effects of a periodized functional strength training program (FST) on Functional Movement Screen (FMS) in physical education students. Phys. Educ. Stud. 2020, 24, 162–167. [Google Scholar] [CrossRef]
- Guler, O.; Tuncel, O.; Bianco, A. Effects of Functional Strength Training on Functional Movement and Balance in Middle-Aged Adults. Sustainability 2021, 13, 1074. [Google Scholar] [CrossRef]
- Buxton, J.D.; Prins, P.J.; Miller, M.G.; Moreno, A.; Welton, G.L.; Atwell, A.D.; Talampas, T.R.; Elsey, G.E. The Effects of a Novel Quadrupedal Movement Training Program on Functional Movement, Range of Motion, Muscular Strength, and Endurance. J. Strength Cond Res. 2020. preprint. [Google Scholar] [CrossRef] [PubMed]
- Liao, S.J. Research on the impact of elastic band resistance training on functional exercise ability of office sedentary people. J. Jilin Sport Univ. 2020, 36, 43–48. [Google Scholar]
- Lim, E.J.; Park, J.E. The effects of Pilates and yoga participant’s on engagement in functional movement and individual health level. J. Exerc. Rehabil. 2019, 15, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Wei, A.; Lu, Y.; Yu, B.; Chen, W.; Lu, Y.; Liu, Y.; Yu, D.; Zou, L. Simplified Tai Chi Program Training versus Traditional Tai Chi on the Functional Movement Screening in Older Adults. Evid.-Based Complement. Altern. 2016, 2016, 5867810. [Google Scholar] [CrossRef] [Green Version]
- Liao, T.; Yang, Q.W.; Cheng, X. Effects of a Progressive Functional Strength Training Program on Functional Movement Quality in Middle and High School Students. J. Wuhan Inst. of Phys. Educ. 2021, 55, 85–92. [Google Scholar]
- Liao, T.; Duhig, S.J.; Du, G.; Luo, B.; Wang, Y.T. The Effect of a Functional Strength Training Intervention on Movement Quality and Physical Fitness in Adolescents. Percept. Mot. Skills 2022, 129, 176–194. [Google Scholar] [CrossRef]
- Li, Y.H.; He, Y.; Li, Y.K. Effect of 24 style Taijiquan typical movements on FMS test. J. Beijing Sport Univ. 2019, 42, 81–87. [Google Scholar]
- Zhang, Z.X.; Yu, Q.C.; Sheng, Z.J.; Cai, J. Intervention research of traditional Chinese medicine guiding exercise prescription on the functional movement capability of sedentary college students. J. Changchun Norm. Univ. 2020, 39, 89–91. [Google Scholar]
- Yang, X.L. Research on the Application of Functional Movement Training in Level 2 Student Physique Development—Take Sanyuanli Primary School in Guangzhou as an Example; Guangzhou Sport University: Guangzhou, China, 2019. [Google Scholar]
- Šćepanović, T.; Protić-Gava, B.; Sporiš, G.; Rupčić, T.; Miljković, Z.; Liapikos, K.; Mačak, D.; Madić, D.M.; Trajković, N. Short-Term Core Strengthening Program Improves Functional Movement Score in Untrained College Students. Int. J. Environ. Res. Public Health 2020, 17, 8669. [Google Scholar] [CrossRef]
- Han, L. Research of Health Qigong Yi Jinjing to Improve College Students’ Physical Movement Function; Beijing Sport University: Beijing, China, 2017. [Google Scholar]
- Ge, L.; Zheng, Q.; Liao, Y.; Tan, J.; Xie, Q.; Rask, M. Effects of traditional Chinese exercises on the rehabilitation of limb function among stroke patients: A systematic review and meta-analysis. Complement. Ther. Clin. 2017, 29, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Yeung, A.; Zeng, N.; Wang, C.; Sun, L.; Thomas, G.; Wang, H. Effects of Mind-Body Exercises for Mood and Functional Capabilities in Patients with Stroke: An Analytical Review of Randomized Controlled Trials. Int. J. Environ. Res. Public Health 2018, 15, 721. [Google Scholar] [CrossRef] [Green Version]
- Moore, E.; Chalmers, S.; Milanese, S.; Fuller, J.T. Factors Influencing the Relationship Between the Functional Movement Screen and Injury Risk in Sporting Populations: A Systematic Review and Meta-analysis. Sports Med. 2019, 49, 1449–1463. [Google Scholar] [CrossRef]
- Laurent, C.W.S.; Masteller, B.; Sirard, J. Effect of a Suspension-Trainer-Based Movement Program on Measures of Fitness and Functional Movement in Children: A Pilot Study. Pediatr. Exerc. Sci. 2018, 30, 364–375. [Google Scholar] [CrossRef]
- Duncan, M.J.; Stanley, M. Functional movement is negatively associated with weight status and positively associated with physical activity in british primary school children. J. Obes. 2012, 2012, 697563. [Google Scholar] [CrossRef]
- Mitchell, U.H.; Johnson, A.W.; Vehrs, P.R.; Feland, J.B.; Hilton, S.C. Performance on the Functional Movement Screen in older active adults. J. Sport Health Sci. 2016, 5, 119–125. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perry, F.T.; Koehle, M.S. Normative data for the functional movement screen in middle-aged adults. J. Strength Cond. Res. 2013, 27, 458–462. [Google Scholar] [CrossRef] [Green Version]
- Karuc, J.; Mišigoj-Duraković, M.; Marković, G.; Hadžić, V.; Duncan, M.J.; Podnar, H.; Sorić, M. Movement quality in adolescence depends on the level and type of physical activity. Phys. Ther. Sport 2020, 46, 194–203. [Google Scholar] [CrossRef]
- Li, Y.; Wang, X.; Chen, X.; Dai, B. Exploratory factor analysis of the functional movement screen in elite athletes. J. Sports Sci. 2015, 33, 1166–1172. [Google Scholar] [CrossRef]
- Silva, B.; Clemente, F.; Camões, M.; Bezerra, P. Functional Movement Screen Scores and Physical Performance among Youth Elite Soccer Players. Sports 2017, 5, 16. [Google Scholar] [CrossRef] [Green Version]
- Silva, B.; Clemente, F.M.; Martins, F.M. Associations between functional movement screen scores and performance variables in surf athletes. J. Sports Med. Phys. Fit. 2018, 58, 583–590. [Google Scholar] [CrossRef]
- Armstrong, R.; Greig, M. Injury identification: The efficacy of the functional movement screen in female and male rugby union players. Int. J. Sports Phys. Ther. 2018, 13, 605–617. [Google Scholar] [CrossRef] [Green Version]
- Mitchell, U.H.; Johnson, A.W.; Adamson, B. Relationship between functional movement screen scores, core strength, posture, and body mass index in school children in Moldova. J. Strength Cond. Res. 2015, 29, 1172–1179. [Google Scholar] [CrossRef]
- Wang, H.; Yu, B.; Chen, W.; Lu, Y.; Yu, D. Simplified Tai Chi Resistance Training versus Traditional Tai Chi in Slowing Bone Loss in Postmenopausal Women. Evid.-Based Complement. Altern. 2015, 2015, 379451. [Google Scholar] [CrossRef]
- Zhang, Y.P.; Hu, R.X.; Han, M.; Lai, B.Y.; Liang, S.B.; Chen, B.J.; Robinson, N.; Chen, K.; Liu, J.P. Evidence Base of Clinical Studies on Qi Gong: A Bibliometric Analysis. Complement. Ther. Med. 2020, 50, 102392. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, C.; Zou, L.; Liu, X.; Song, W. The Effects of Mind-Body Exercise on Cognitive Performance in Elderly: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2018, 15, 2791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boyle, M. New Functional Training for Sports, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2016; pp. 30–34. [Google Scholar]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081–1093. [Google Scholar] [CrossRef] [Green Version]

| Authors, Year | Study Design | Participants (n) | Age (Years) (±SD) | Experimental Group | Control Group | Duration/Frequency /Period | Outcomes (Measures) |
|---|---|---|---|---|---|---|---|
| Buxton et al. (2020) [39] | RCT | College students (42) (EG: 21; CG: 21) | EG (19.38 ± 1.36); CG (20.14 ± 2.63) | Quadrupedal movement training | Waiting list | 60 min, 2 times per week, 8 weeks | FMS composite score |
| Guler et al. (2021) [38] | RCT | Middle-aged adults (46) (EG: 26; CG: 20) | EG (51.55 ± 3.73); CG (52.85 ± 4.01) | Functional strength training | Traditional strength training | 60 min, 3 times per week, 8 weeks | FMS composite score |
| Han (2017) [49] | Non-RCT | College students (31) (EG: 13; CG: 18) | NR | Yi Jinjing | Routine exercise | 90 min, 3 times per week, 12 weeks | Asymmetry functional patterns |
| Kang (2020) [31] | RCT | Children (40) (EG: 20; CG: 20) | EG (9.45 ± 1.36); CG (9.50 ± 1.15) | Functional training | Routine exercise | 90 min, once a week, 14 weeks | FMS composite score; FMS individual score |
| Li et al. (2019) [45] | Non-RCT | Male college students (48) (EG: 24; CG: 24) | 18.88 ± 0.68 | Simplified 24-form Tai Chi | Waiting list | 20 min, 2 times per week, 8 weeks | FMS composite score; Asymmetry functional patterns |
| Liao et al. (2019) [35] | RCT | Girls (144) (EG: 72; CG: 72) | 12.47 ± 0.57 | Functional strength training | Traditional strength training | 45 min, 3 times per week, 12 weeks | FMS composite score; FMS individual score; Asymmetry functional patterns |
| Liao (2020) [40] | RCT | Office sedentary people (38) (EG: 19; CG: 19) | EG (28.15 ± 1.9); CG (27.10 ± 2.1) | Elastic band resistance training | Waiting list | 50–60 min, 3 times per week, 12 weeks | FMS composite score; FMS individual score |
| Liao et al. (2021) [43] | RCT | Adolescents (266) (EG1: 72; CG1: 72; EG2: 61; CG2: 61) | 13–16 | Functional strength training | Physical education | 45 min, 3 times per week, 12 weeks | FMS composite score; Asymmetry functional patterns |
| Liao et al. (2022) [44] | RCT | Adolescents (266) (EG: 133; CG: 133) | EG (14.37 ± 0.55); CG (14.03 ± 0.59) | Functional strength training | Physical education | 45 min, 3 times per week, 12 weeks | FMS composite score; FMS individual score |
| Lim et al. (2019) [41] | RCT | Adults (90) (EG1: 30; EG2: 30; CG: 30) | 30–40 | EG1:Pilates EG2:Yoga | Waiting list | 60 min, 3 times per week, 8 weeks | FMS composite score |
| Liu (2020) [33] | RCT | Elderly adults (24) (EG: 12; CG: 12) | EG (65.25 ± 3.93); CG (65.42 ± 3.94) | Wu Qinxi | Waiting list | 60 min, 6 times per week, 12 weeks | FMS composite score; FMS individual score |
| Mahdieh et al. (2020) [8] | RCT | Female students (34) (EG: 19; CG: 15) | EG (18.8 ± 0.68); CG (18.9 ± 0.91) | Dynamic neuromuscular stabilization training | Routine exercise | 50 min, 3 times per week, 6 weeks | FMS composite score |
| Sawczy et al. (2020) [37] | RCT | College students (33) (EG: 16; CG: 17) | 21.6 ± 1.3 | Functional strength training | Routine exercise | 60 min, 4 times per week (1–6 wk)/2 times per week (7–12 wk), 12 weeks | FMS composite score |
| Scepanovic et al.(2020) [48] | Non-RCT | Male college students (138) (EG: 73; CG: 65) | EG (20 ± 0.5); CG (20 ± 0.7) | Core stabilization training | Routine exercise | 30 min, 3 times per week, 6 weeks | FMS composite score; FMS individual score |
| Strauss et al. (2020) [36] | RCT | Active young population (24) (EG: 12; CG: 12) | EG (25.7 ± 4.70); CG (27.4 ± 5.50) | Total Motion Release | Waiting list | 2 sets of 15 repetitions | FMS composite score |
| Wang et al. (2016) [42] | RCT | Older adults (90) (EG1: 30; EG2: 30; CG: 30) | EG1 (65.2 ± 5.0); EG2 (65.3 ± 4.3); CG (65.3 ± 4.4) | EG1:Traditional Tai Chi EG2:Simplified Tai Chi | Routine activity | 60 min, 4 times per week, 12 weeks | FMS composite score |
| Wang (2019) [32] | RCT | Female college students (82) (EG: 41; CG: 41) | NR | Modified yoga | Regular yoga | 90 min, once a week, 12 weeks | FMS composite score; FMS individual score |
| Xiong (2018) [34] | RCT | Middle-aged women (60) (EG: 30; CG: 30) | 50 ± 3.21 | Yoga | Waiting list | 60 min, 3 times per week, 12 weeks | FMS composite score; FMS individual score |
| Yang (2019) [47] | Non-RCT | Primary school students (60) (EG: 30; CG: 30) | 8–10 | Functional training | Waiting list | 45 min, 2 times per week, 12 weeks | FMS composite score; FMS individual score |
| Zhang (2020) [46] | Non-RCT | College students (40) (EG: 20; CG: 20) | NR | Dao Yin | Routine exercise | 90 min, 5 times per week, 24 weeks | FMS composite score; FMS individual score |
| Authors, Year | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Buxton et al. (2020) [39] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Guler et al. (2021) [38] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Kang (2020) [31] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Liao et al. (2019) [35] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Liao (2020) [40] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Liao et al. (2021) [43] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Liao et al. (2022) [44] | Y | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7/10 |
| Lim et al. (2019) [41] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Liu (2020) [33] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Mahdieh et al. (2020) [8] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 5/10 |
| Sawczy et al. (2020) [37] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Strauss et al. (2020) [36] | Y | Y | Y | Y | N | Y | N | Y | Y | Y | Y | 8/10 |
| Wang et al. (2016) [42] | Y | Y | N | Y | N | N | Y | Y | Y | Y | Y | 7/10 |
| Wang (2019) [32] | N | Y | N | Y | Y | Y | N | Y | Y | Y | Y | 8/10 |
| Xiong (2018) [34] | Y | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Authors, Year | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Han (2017) [49] | 2 | 1 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 15/24 |
| Li et al. (2019) [45] | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 16/24 |
| Scepanovic et al. (2020) [48] | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 18/24 |
| Yang (2019) [47] | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 16/24 |
| Zhang (2020) [46] | 1 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 2 | 2 | 15/24 |
| Group | Subgroup | N | MD | 95% CI | p | I2 |
|---|---|---|---|---|---|---|
| Age (year) | Under 18 | 6 | 4.20 | 3.27, 5.12 | <0.00001 | 90% |
| 18–30 | 9 | 2.99 | 1.97, 4.01 | <0.00001 | 92% | |
| More than 50 | 5 | 1.95 | 1.28, 2.62 | <0.00001 | 82% | |
| Intervention | Specific sports | 9 | 2.42 | 1.80, 3.04 | <0.00001 | 87% |
| Functional training program | 13 | 3.38 | 2.47, 4.30 | <0.00001 | 95% | |
| Time (min) | Under 60 min | 8 | 3.64 | 2.45, 4.83 | <0.00001 | 95% |
| 60 min | 9 | 2.17 | 1.67, 2.67 | <0.00001 | 79% | |
| More than 60 min | 3 | 4.25 | 0.71, 7.79 | 0.02 | 98% | |
| Frequency (time/week) | Under 3 times/week | 5 | 3.65 | 1.74, 5.56 | 0.0002 | 96% |
| 3 times/week | 12 | 3.13 | 2.39, 3.87 | <0.00001 | 94% | |
| More than 3 times/week | 4 | 2.15 | 0.94, 3.35 | 0.0005 | 85% | |
| Period (week) | 6 weeks | 2 | 3.09 | −1.92, 8.11 | 0.23 | 98% |
| 8 weeks | 5 | 2.71 | 1.45, 3.96 | <0.0001 | 86% | |
| 12 weeks | 12 | 2.80 | 2.24, 3.35 | <0.00001 | 92% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Zhong, M.; Wang, J. Effects of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 9353. https://doi.org/10.3390/ijerph19159353
Huang J, Zhong M, Wang J. Effects of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(15):9353. https://doi.org/10.3390/ijerph19159353
Chicago/Turabian StyleHuang, Jiafu, Mengting Zhong, and Jinghao Wang. 2022. "Effects of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 15: 9353. https://doi.org/10.3390/ijerph19159353
APA StyleHuang, J., Zhong, M., & Wang, J. (2022). Effects of Exercise-Based Interventions on Functional Movement Capability in Untrained Populations: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(15), 9353. https://doi.org/10.3390/ijerph19159353