Effects of Group Music Intervention on Depression for Elderly People in Nursing Homes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Participants and Setting
2.3. Intervention and Procedure
2.4. Ethical Consideration
2.5. Measures
2.5.1. Demographics
2.5.2. Geriatric Depression Scale—Short Form
2.5.3. Salivary Cortiso
2.6. Data Collection and Data Analysis
2.6.1. Data Collection
2.6.2. Data Analysis
3. Results
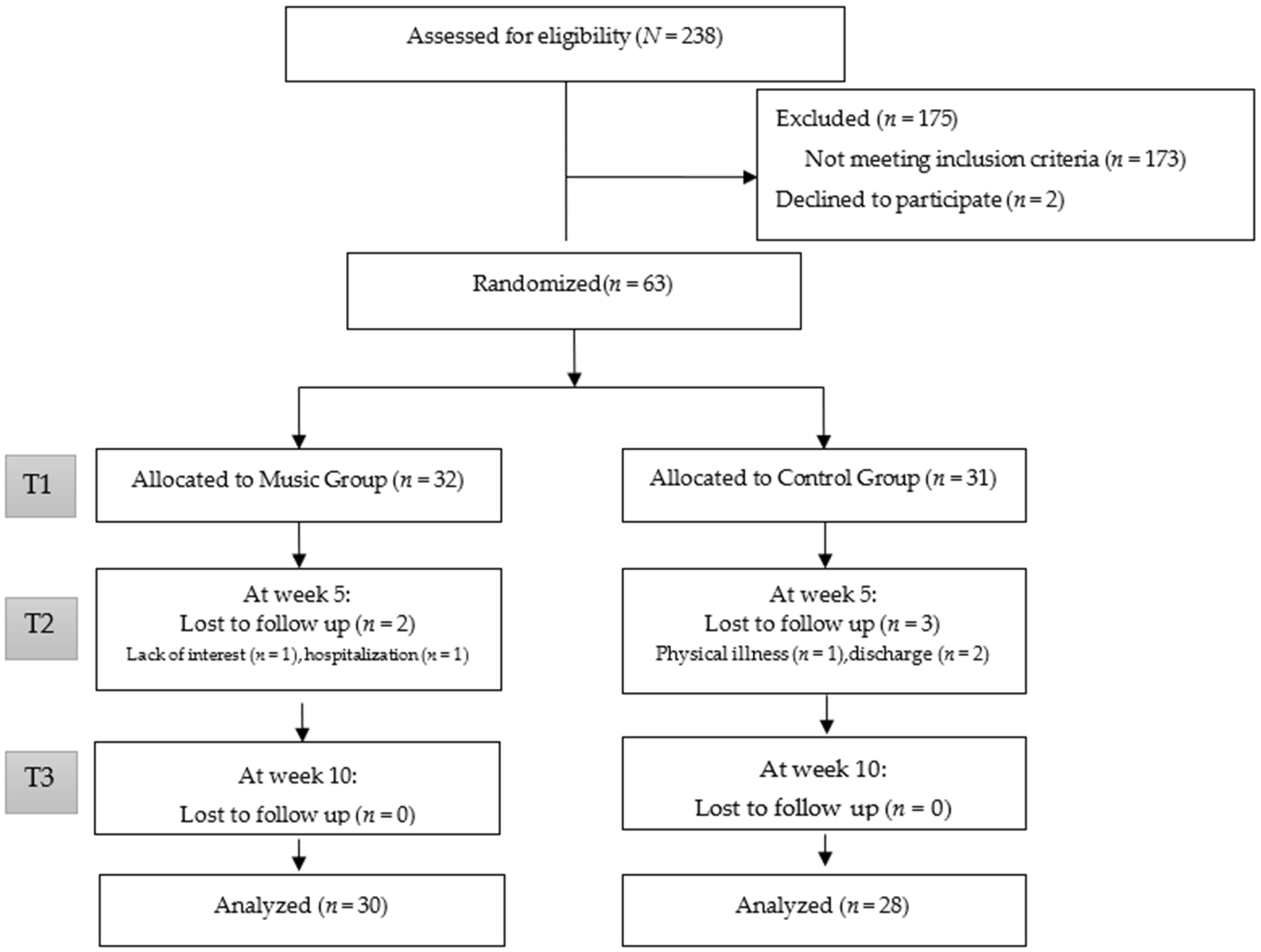
3.1. Participant Flow
3.2. Demographic Information
3.3. Result on Outcome Measures
4. Discussion
4.1. Effects on Depression
4.2. Effects on Salivary Cortisol
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. Global Issues: Ageing. Available online: https://www.un.org/en/global-issues/ageing (accessed on 8 June 2022).
- Wu, C.S.; Yu, S.H.; Lee, C.Y.; Tseng, H.Y.; Chiu, Y.F.; Hsiung, C.A. Prevalence of and risk factors for minor and major depression among community-dwelling older adults in Taiwan. Int. Psychogeriatr. 2017, 29, 1113–1121. [Google Scholar] [CrossRef] [PubMed]
- Nazemi, L.; Skoog, I.; Karlsson, I.; Hosseini, S.; Hosseini, M.; Hosseinzadeh, M.J.; Mohammadi, M.R.; Pouransari, Z.; Chamari, M.; Baikpour, M. Depression, prevalence and some risk factors in elderly nursing homes in Tehran, Iran. Iran. J. Public Health 2013, 42, 559–569. [Google Scholar] [PubMed]
- Barua, A.; Ghosh, M.K.; Kar, N.; Basilio, M.A. Prevalence of depressive disorders in the elderly. Ann. Saudi Med. 2011, 31, 620–624. [Google Scholar] [CrossRef] [Green Version]
- Kowalska, J.; Bojko, E.; Szczepańska-Gieracha, J.; Rymaszewska, J.; Rożek-Piechura, K. Occurrence of Depressive Symptoms Among Older Adults after a Stroke in the Nursing Home Facility. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nurses 2016, 41, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Tiong, W.W.; Yap, P.; Huat Koh, G.C.; Phoon Fong, N.; Luo, N. Prevalence and risk factors of depression in the elderly nursing home residents in Singapore. Aging Ment. Health 2013, 17, 724–731. [Google Scholar] [CrossRef]
- Ramamurthy, G.; Danasu; Tamilselvi, P. A study to assess the prevalence of depression among elderly residing in selected old age home, Kancheepuram District, Tamil Nadu, 2015. Asian J. Nur. Edu. Res. 2015, 5, 381–384. [Google Scholar] [CrossRef]
- Cong, L.; Dou, P.; Chen, D.; Cai, L. Depression and Associated Factors in the Elderly Cadres in Fuzhou, China: A Community-Based Study. Int. J. Gerontol. 2015, 9, 29–33. [Google Scholar] [CrossRef] [Green Version]
- Boyce, R.D.; Hanlon, J.T.; Karp, J.F.; Kloke, J.; Saleh, A.; Handler, S.M. A review of the effectiveness of antidepressant medications for depressed nursing home residents. J. Am. Med Dir. Assoc. 2012, 13, 326–331. [Google Scholar] [CrossRef] [Green Version]
- American Music Therapy Association. What Is Music Therapy? Available online: https://www.musictherapy.org/about/musictherapy/ (accessed on 8 June 2022).
- De Witte, M.; Spruit, A.; van Hooren, S.; Moonen, X.; Stams, G.J. Effects of music interventions on stress-related outcomes: A systematic review and two meta-analyses. Health Psychol. Rev. 2020, 14, 294–324. [Google Scholar] [CrossRef]
- Grynderup, M.B.; Kolstad, H.A.; Mikkelsen, S.; Andersen, J.H.; Bonde, J.P.; Buttenschøn, H.N.; Kærgaard, A.; Kærlev, L.; Rugulies, R.; Thomsen, J.F.; et al. A two-year follow-up study of salivary cortisol concentration and the risk of depression. Psychoneuroendocrinology 2013, 38, 2042–2050. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Yang, C.Y.; Lin, Y.; Ou, K.L.; Lee, T.Y.; O’Brien, A.P.; Chou, K.R. The impact of group music therapy on depression and cognition in elderly persons with dementia: A randomized controlled study. Biol. Res. Nurs. 2014, 16, 209–217. [Google Scholar] [CrossRef] [PubMed]
- De la Rubia Ortí, J.E.; García-Pardo, M.P.; Iranzo, C.C.; Madrigal, J.J.C.; Castillo, S.S.; Rochina, M.J.; Gascó, V.J.P. Does Music Therapy Improve Anxiety and Depression in Alzheimer’s Patients? J. Altern. Complement Med. 2018, 24, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Guétin, S.; Portet, F.; Picot, M.C.; Pommié, C.; Messaoudi, M.; Djabelkir, L.; Olsen, A.L.; Cano, M.M.; Lecourt, E.; Touchon, J. Effect of music therapy on anxiety and depression in patients with Alzheimer’s type dementia: Randomised, controlled study. Dement. Geriatry Cogn. Disord. 2009, 28, 36–46. [Google Scholar] [CrossRef]
- Li, H.C.; Wang, H.H.; Lu, C.Y.; Chen, T.B.; Lin, Y.H.; Lee, I. The effect of music therapy on reducing depression in people with dementia: A systematic review and meta-analysis. Geriatry Nurs. 2019, 40, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.D.; Götell, E. The Use of Music and Music Therapy in Ameliorating Depression Symptoms and Improving Well-Being in Nursing Home Residents with Dementia. Front. Med. 2018, 5, 287. [Google Scholar] [CrossRef] [PubMed]
- Werner, J.; Wosch, T.; Gold, C. Effectiveness of group music therapy versus recreational group singing for depressive symptoms of elderly nursing home residents: Pragmatic trial. Aging Ment. Health 2017, 21, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Särkämö, T.; Tervaniemi, M.; Laitinen, S.; Numminen, A.; Kurki, M.; Johnson, J.K.; Rantanen, P. Cognitive, emotional, and social benefits of regular musical activities in early dementia: Randomized controlled study. Gerontologist 2014, 54, 634–650. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allison, T.A.; Smith, A.K. “Now I Write Songs”: Growth and Reciprocity After Long-Term Nursing Home Placement. Gerontologist 2020, 60, 135–144. [Google Scholar] [CrossRef]
- Perez-Ros, P.; Cubero-Plazas, L.; Mejias-Serrano, T.; Cunha, C.; Martinez-Arnau, F.M. Preferred Music Listening Intervention in Nursing Home Residents with Cognitive Impairment: A Randomized Intervention Study. J. Alzheimers Dis. 2019, 70, 431–440. [Google Scholar] [CrossRef]
- Kwak, J.; Anderson, K.; Valuch, K.O. Findings from a Prospective Randomized Controlled Trial of an Individualized Music Listening Program for Persons with Dementia. J. Appl. Gerontol. 2020, 39, 567–575. [Google Scholar] [CrossRef]
- Janus, S.I.M.; Kosters, J.; van den Bosch, K.A.; Andringa, T.C.; Zuidema, S.U.; Luijendijk, H.J. Sounds in nursing homes and their effect on health in dementia: A systematic review. Int. Psychogeriatr. 2021, 33, 627–644. [Google Scholar] [CrossRef] [PubMed]
- Ridder, H.M.; Stige, B.; Qvale, L.G.; Gold, C. Individual music therapy for agitation in dementia: An exploratory randomized controlled trial. Aging Ment. Health 2013, 17, 667–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weise, L.; Topfer, N.F.; Deux, J.; Wilz, G. Feasibility and effects of individualized recorded music for people with dementia: A pilot RCT study. Nord. J. Music Ther. 2020, 29, 39–56. [Google Scholar] [CrossRef]
- Onieva-Zafra, M.D.; Hernández-Garcia, L.; Gonzalez-Del-Valle, M.T.; Parra-Fernández, M.L.; Fernandez-Martinez, E. Music Intervention with Reminiscence Therapy and Reality Orientation for Elderly People with Alzheimer Disease Living in a Nursing Home: A Pilot Study. Holist. Nurs. Pract. 2018, 32, 43–50. [Google Scholar] [CrossRef]
- Moghaddasifar, I.; Fereidooni-Moghadam, M.; Fakharzadeh, L.; Haghighi-Zadeh, M.H. Investigating the effect of multisensory stimulation on depression and anxiety of the elderly nursing home residents: A randomized controlled trial. Perspect. Psychiatry Care 2019, 55, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Raglio, A.; Bellandi, D.; Baiardi, P.; Gianotti, M.; Ubezio, M.C.; Zanacchi, E.; Granieri, E.; Imbriani, M.; Stramba-Badiale, M. Effect of Active Music Therapy and Individualized Listening to Music on Dementia: A Multicenter Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1534–1539. [Google Scholar] [CrossRef]
- Sakamoto, M.; Ando, H.; Tsutou, A. Comparing the effects of different individualized music interventions for elderly individuals with severe dementia. Int. Psychogeriatr. 2013, 25, 775–784. [Google Scholar] [CrossRef]
- Wilkins, R.W.; Hodges, D.A.; Laurienti, P.J.; Steen, M.; Burdette, J.H. Network science and the effects of music preference on functional brain connectivity: From Beethoven to Eminem. Sci. Rep. 2014, 4, 6130. [Google Scholar] [CrossRef] [Green Version]
- Reybrouck, M.; Vuust, P.; Brattico, E. Brain Connectivity Networks and the Aesthetic Experience of Music. Brain Sci. 2018, 8, 107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chin, W.-C.; Liu, C.-Y.; Lee, C.-P.; Chu, C.-L. Validation of Five Short Versions of the Geriatric Depression Scale in the Elder Population in Taiwan. Taiwan. J. Psychiatry 2014, 28, 156–163. [Google Scholar]
- Harris, T.O.; Borsanyi, S.; Messari, S.; Stanford, K.; Cleary, S.E.; Shiers, H.M.; Brown, G.W.; Herbert, J. Morning cortisol as a risk factor for subsequent major depressive disorder in adult women. Br. J. Psychiatry J. Ment. Sci. 2000, 177, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Herbert, J.; Ban, M.; Brown, G.W.; Harris, T.O.; Ogilvie, A.; Uher, R.; Craig, T.K. Interaction between the BDNF gene Val/66/Met polymorphism and morning cortisol levels as a predictor of depression in adult women. Br. J. Psychiatry J. Ment. Sci. 2012, 201, 313–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Music Group (n = 32) | Control Group (n = 31) | p Value | |
|---|---|---|---|---|
| Gender | Male | 10 (31.3%) | 18 (58.1%) | <0.05 |
| Female | 22 (68.7%) | 13 (41.9%) | ||
| Marital status | Married | 5 (15.6%) | 12 (38.7%) | 0.07 |
| Widowed/divorced | 27 (84.4%) | 19 (61.3%) | ||
| Religion | No | 1 (3.1%) | 2 (6.5%) | 0.62 |
| Taoism | 28 (87.5%) | 24 (77.4%) | ||
| Buddhism | 3 (9.4%) | 4 (12.9%) | ||
| Christian | 0 (0%) | 1 (3.2%) | ||
| Education | Illiterate | 15 (46.9%) | 15 (48.4%) | 0.51 |
| literate | 2 (6.3%) | 1 (3.2%) | ||
| Primary | 12 (37.5%) | 7 (22.6%) | ||
| junior | 1 (3.1%) | 2 (6.5%) | ||
| High school | 2 (6.3%) | 5 (16.1%) | ||
| College | 0 (0%) | 1 (3.2%) | ||
| Health status | None | 1 (3.1%) | 0 (0%) | 0.65 |
| One item | 10 (31.3%) | 9 (29.0%) | ||
| Two item | 10 (31.3%) | 12 (38.7%) | ||
| Three item | 11 (34.4%) | 9 (29.0%) | ||
| >Four item | 0 (0%) | 1 (3.2%) | ||
| Mean age (SD) | 80.30 ± 6.88 | 79.03 ± 7.71 | 0.19 | |
| Mean length of stay years (SD) | 3.16 ± 3.26 | 2.49 ± 3.20 | 0.40 | |
| GDS-SF(baseline) | 8.65 ± 3.38 | 10.16 ± 2.91 | 0.054 | |
| Salivary cortisol(pg/mL) (baseline) | 585.13 ± 573.74 | 567.66 ± 541.49 | 0.317 | |
| Variable | Time 1 (N = 63) | Time 2 (N = 58) | Time 3 (N = 58) | |||
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||||
| Music Group | Control Group | Music Group | Control Group | Music Group | Control Group | |
| GDS-SF | 8.65 (3.38) | 10.16 (2.91) | 3.96 (1.54) | 10.39 (2.87) | 2.96 (1.29) | 10.17 (2.77) |
| Salivary cortisol | 585.13 (573.74) | 567.66 (541.49) | 765.16 (746.18) | 866.67 (728.43) | 645.61 (668.74) | 647.00 (759.34) |
| Depression(GDS-SF) | Salivary Cortisol | |||||
|---|---|---|---|---|---|---|
| Effect | Wald χ2 | df | p | Wald χ2 | df | p |
| Intercept | 4.43 | 1 | <0.001 | 680.92 | 1 | 0.051 |
| Group | −4.84 | 1 | <0.0001 | −272.21 | 1 | 0.511 |
| Time | −0.21 | 1 | 0.092 | −219.67 | 1 | 0.23 |
| Group × Time | −0.78 | 1 | <0.0001 | 100.12 | 1 | 0.686 |
| Baseline | −0.45 | 1 | <0.0001 | −0.86 | 1 | <0.0001 |
| Variable | Type III Sum of Squares | df | Mean Squares | F | p Value | Effect Size Cohen d |
|---|---|---|---|---|---|---|
| Effect on depression (GDS-SF) | ||||||
| 5th weekly | ||||||
| Intercept | 1.87 | 1 | 1.87 | 1.21 | 0.274 | |
| GDS (baseline) | 83.54 | 1 | 83.54 | 54.32 | <0.0001 | |
| Gender | 2.16 | 1 | 2.16 | 1.41 | 0.24 | |
| Group | 385.16 | 1 | 385.16 | 250.48 | <0.0001 | 2.75 |
| Error | 83.03 | 54 | 1.53 | |||
| 10th weekly | ||||||
| Intercept | 5.29 | 1 | 5.29 | 2.29 | 0.136 | |
| GDS (baseline) | 146.42 | 1 | 146.42 | 63.41 | <0.0001 | |
| Gender | 2.28 | 1 | 2.28 | 0.99 | 0.324 | |
| Group | 536.43 | 1 | 536.43 | 232.32 | <0.0001 | 2.51 |
| Error | 124.68 | 54 | 2.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, A.-L.; Lo, S.-F.; Chen, P.-Y.; Lu, S.-F. Effects of Group Music Intervention on Depression for Elderly People in Nursing Homes. Int. J. Environ. Res. Public Health 2022, 19, 9291. https://doi.org/10.3390/ijerph19159291
Yu A-L, Lo S-F, Chen P-Y, Lu S-F. Effects of Group Music Intervention on Depression for Elderly People in Nursing Homes. International Journal of Environmental Research and Public Health. 2022; 19(15):9291. https://doi.org/10.3390/ijerph19159291
Chicago/Turabian StyleYu, Ai-Ling, Shu-Fen Lo, Pei-Yu Chen, and Shiou-Fang Lu. 2022. "Effects of Group Music Intervention on Depression for Elderly People in Nursing Homes" International Journal of Environmental Research and Public Health 19, no. 15: 9291. https://doi.org/10.3390/ijerph19159291
APA StyleYu, A.-L., Lo, S.-F., Chen, P.-Y., & Lu, S.-F. (2022). Effects of Group Music Intervention on Depression for Elderly People in Nursing Homes. International Journal of Environmental Research and Public Health, 19(15), 9291. https://doi.org/10.3390/ijerph19159291





