Effects of a Mixed Exercise Program on Overweight and Obese Children and Adolescents: A Pilot, Uncontrolled Study
Abstract
:1. Introduction
2. Materials and Methods
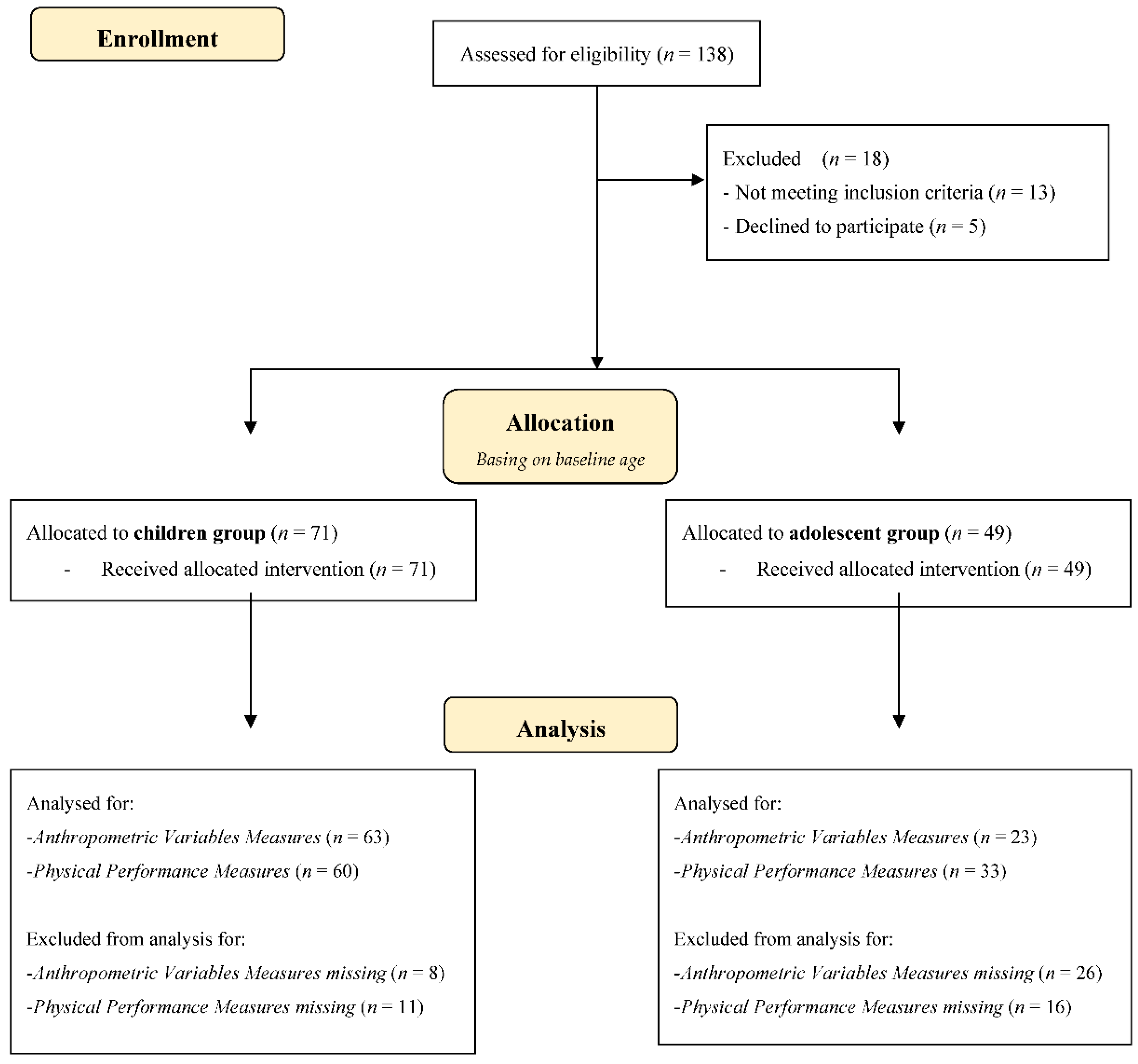
2.1. Participants
2.2. Intervention
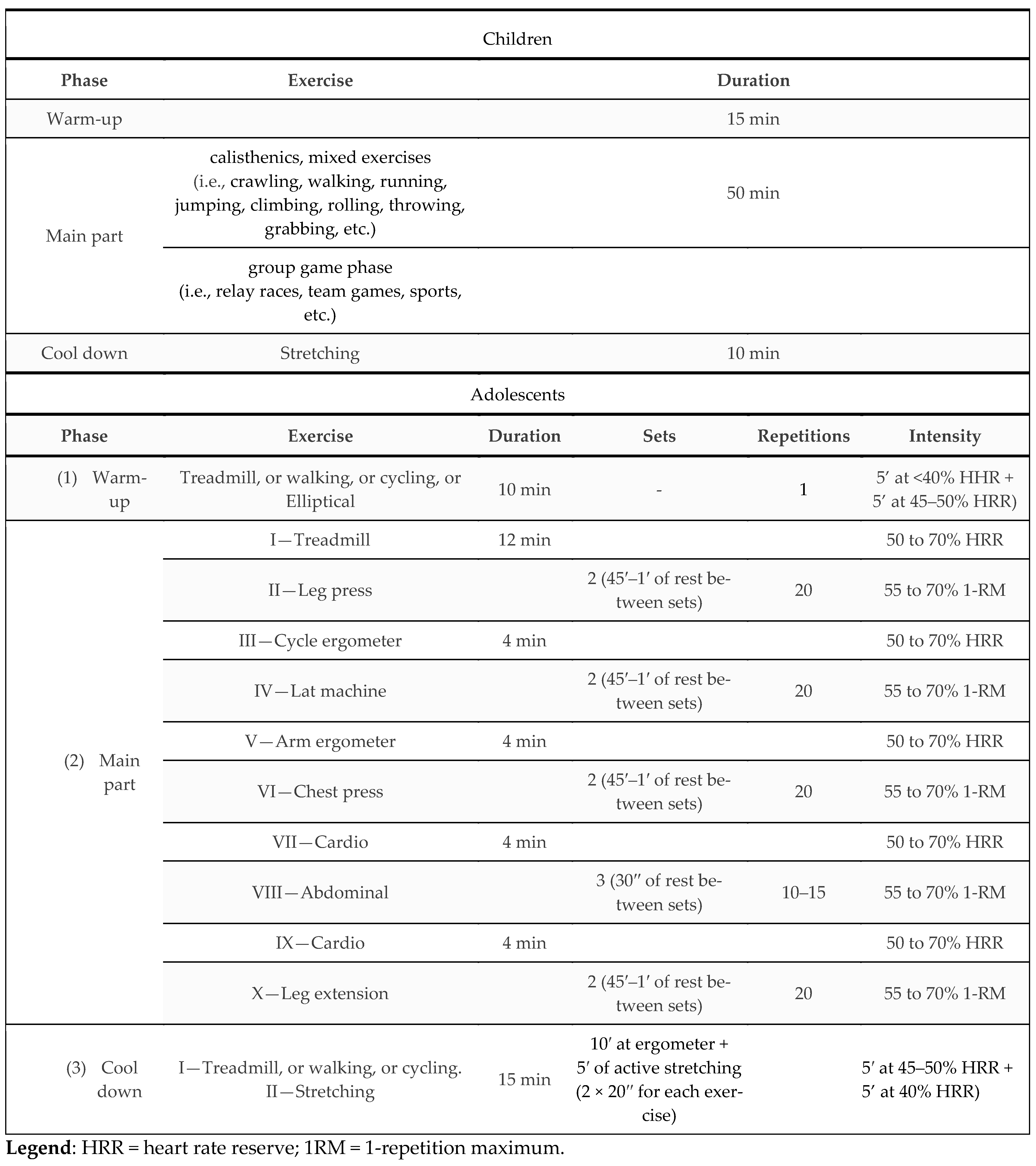
2.2.1. Exercise Intervention
2.3. Measures
2.3.1. Anthropometric Variables Measures
2.3.2. Physical Performance Measures
2.4. Statistical Analysis
2.5. Sample Size Calculation
3. Results
3.1. Baseline Ressults
3.2. Exercise Program Effects
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sabin, M.A.; Kao, K.T.; Juonala, M.; Baur, L.A.; Wake, M. Viewpoint article: Childhood obesity--looking back over 50 years to begin to look forward. J. Paediatr. Child Health 2015, 51, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.R.; Lovejoy, J.C.; Greenway, F.; Ryan, D.; DeJonge, L.; de la Bretonne, J.; Volafova, J.; Bray, G.A. Contributions of total body fat, abdominal subcutaneous adipose tissue compartments, and visceral adipose tissue to the metabolic complications of obesity. Metabolism 2001, 50, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Bass, R.; Eneli, I. Severe childhood obesity: An under-recognised and growing health problem. Postgrad. Med. J. 2015, 91, 639–645. [Google Scholar] [CrossRef]
- Busnatu, S.S.; Serbanoiu, L.I.; Lacraru, A.E.; Andrei, C.L.; Jercalau, C.E.; Stoian, M.; Stoian, A. Effects of Exercise in Improving Cardiometabolic Risk Factors in Overweight Children: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 82. [Google Scholar] [CrossRef]
- Rajjo, T.; Almasri, J.; Al Nofal, A.; Farah, W.; Alsawas, M.; Ahmed, A.T.; Mohammed, K.; Kanwar, A.; Asi, N.; Wang, Z.; et al. The Association of Weight Loss and Cardiometabolic Outcomes in Obese Children: Systematic Review and Meta-regression. J. Clin. Endocrinol. Metab. 2017, 102, 758–762. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Vélez, R.; Ramírez-Campillo, R.; Peterson, M.D.; Martínez-Vizcaíno, V. Concurrent aerobic plus resistance exercise versus aerobic exercise alone to improve health outcomes in paediatric obesity: A systematic review and meta-analysis. Br. J. Sports Med. 2018, 52, 161–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, D.; Chen, P. The Effects of Different Exercise Modalities in the Treatment of Cardiometabolic Risk Factors in Obese Adolescents with Sedentary Behavior-A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Children 2021, 8, 1062. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guillem, C.M.; Loaiza-Betancur, A.F.; Rebullido, T.R.; Faigenbaum, A.D.; Chulvi-Medrano, I. The Effects of Resistance Training on Blood Pressure in Preadolescents and Adolescents: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7900. [Google Scholar] [CrossRef]
- Ortega, F.B.; Silventoinen, K.; Tynelius, P.; Rasmussen, F. Muscular strength in male adolescents and premature death: Cohort study of one million participants. BMJ 2012, 20, e7279. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Campos, R.; Andruske, C.L.; Arruda, M.D.; Sulla-Torres, J.; Pacheco-Carrillo, J.; Urra-Albornoz, C.; Cossio-Bolaños, M. Normative data for handgrip strength in children and adolescents in the Maule Region, Chile: Evaluation based on chronological and biological age. PLoS ONE 2018, 13, e0201033. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Ramírez-Campillo, R.; Izquierdo, M. Is muscular fitness associated with future health benefits in children and adolescents? A systematic review and meta-analysis of longitudinal studies. Sports Med. 2019, 49, 1079–1094. [Google Scholar] [CrossRef]
- García-Hermoso, A.; Sánchez-López, M.; Martínez-Vizcaíno, V. Effects of Aerobic Plus Resistance Exercise on Body Composition Related Variables in Pediatric Obesity: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pediatr. Exerc. Sci. 2015, 27, 431–440. [Google Scholar] [CrossRef]
- Mendonça, F.R.; Ferreira de Faria, W.; Marcio da Silva, J.; Massuto, R.B.; Castilho Dos Santos, G.; Correa, R.C.; Dos Santos, C.F.; Sasaki, J.E.; Neto, A.S. Effects of aerobic exercise combined with resistance training on health-related physical fitness in adolescents: A randomized controlled trial. J. Exerc. Sci. Fit. 2022, 20, 182–189. [Google Scholar] [CrossRef]
- Enríquez-del-Castillo, L.A.; Ornelas-López, A.; De León, L.G.; Cervantes-Hernández, N.; Quintana-Mendias, E.; Flores, L.A. Strength and VO2 max Changes by Exercise Training According to Maturation State in Children. Children 2022, 9, 938. [Google Scholar] [CrossRef]
- Izzicupo, P.; Di Blasio, A.; Di Credico, A.; Ghinassi, B.; Capranica, L.; Napolitano, G.; Di Baldassarre, A.; Modestini, E.; Di Pietro, M. Objectively Measured Physical Activity Increases Only in Males During a Summer Camp for Obese Children. Front. Sports Act. Living 2021, 3, 624449. [Google Scholar] [CrossRef]
- Ranucci, C.; Pippi, R.; Buratta, L.; Aiello, C.; Gianfredi, V.; Piana, N.; Reginato, E.; Tirimagni, A.; Chiodini, E.; Sbroma Tomaro, E.; et al. Effects of an Intensive Lifestyle Intervention to Treat Overweight/Obese Children and Adolescents. Biomed. Res. Int. 2017, 2017, 8573725. [Google Scholar] [CrossRef] [Green Version]
- Cacciari, E.; Milani, S.; Balsamo, A.; Dammacco, F.; De Luca, F.; Chiarelli, F.; Pasquino, A.M.; Tonini, G.; Vanelli, M. Italian cross-sectional growth charts for height, weight and BMI (6–20 y). Eur. J. Clin. Nutr. 2002, 56, 171–180. [Google Scholar] [CrossRef] [Green Version]
- Mazzeschi, C.; Pazzagli, C.; Laghezza, L.; Battistini, D.; Reginato, E.; Perrone, C.; Ranucci, C.; Fatone, C.; Pippi, R.; Giaimo, M.D.; et al. Description of the EUROBIS Program: A combination of an epode community-based and a clinical care intervention to improve the lifestyles of children and adolescents with overweight or obesity. Biomed. Res. Int. 2014, 2014, 546262. [Google Scholar] [CrossRef] [Green Version]
- De Feo, P.; Fatone, C.; Burani, P.; Piana, N.; Pazzagli, C.; Battistini, D.; Capezzali, D.; Pippi, R.; Chipi, B.; Mazzeschi, C. An innovative model for changing the lifestyles of persons with obesity and/or type 2 diabetes mellitus. J. Endocrinol. Investig. 2011, 34, e349–e354. [Google Scholar]
- Pippi, R.; Buratta, L.; Perna, F.; Aiello, C.; Ranucci, C.; Mazzeschi, C.; Fanelli, C. Evaluation of maximum oxygen consumption in obese adolescents before and after a multidisciplinary lifestyle intervention. Gazz. Med. Ital. Arch. Per Le Sci. Med. 2020, 179, 154–161. [Google Scholar] [CrossRef]
- S.I.O. Società Italiana dell’Obesità. Standard Italiana per la cura dell’Obesità 2012–2013. Available online: https://www.obesityday.org/usr_files/biblioteca/Standard_SIOADI.pdf (accessed on 10 June 2022).
- S.I.O. Società Italiana dell’Obesità. Standard Italiana per la cura dell’Obesità 2016–2017. Available online: https://www.sio-obesita.org/wp-content/uploads/2017/09/STANDARD-OBESITA-SIO-ADI.pdf (accessed on 10 June 2022).
- Marta, C.C.; Marinho, D.A.; Izquierdo, M.; Marques, M.C. Differentiating maturational influence on training-induced strength and endurance adaptations in prepubescent children. Am. J. Hum. Biol. 2014, 26, 469–475. [Google Scholar] [CrossRef]
- Cervantes Hernández, N.; Enríquez del Castillo, L.A.; Flores Olivares, L.A.; Candia Luján, R.; Domínguez Esparza, S. Entrenamiento De Flexibilidad Integradora Para Mejorar La Movilidad Articular Y El Rango De Movimiento En Bailarinas De Jazz. Sportis Sci. J. 2021, 7, 425–447. [Google Scholar] [CrossRef]
- Benjamin, H.J.; Glow, K.M. Strength training for children and adolescents: What can physicians recommend? Phys. Sportsmed. 2003, 31, 19–26. [Google Scholar] [CrossRef]
- Dahab, K.S.; McCambridge, T.M. Strength Training in Children and Adolescents: Raising the Bar for Young Athletes? Sports Health 2009, 1, 223–226. [Google Scholar] [CrossRef] [Green Version]
- Seca Portable Stadiometer Height Rod 0–205 cm. Capes Medical Ltd. 2011. Available online: https://www.capesmedical.co.nz/media/seca-213-seca-mobile-measuring-board-10-100cm.pdf (accessed on 23 March 2022).
- Nuñez, C.; Kovera, A.J.; Pietrobelli, A.; Heshka, S.; Horlick, M.; Kehayias, J.J.; Wang, Z.; Heymsfield, S.B. Body composition in children and adults by air displacement plethysmography. Eur. J. Clin. Nutr. 1999, 53, 382–387. [Google Scholar] [CrossRef] [Green Version]
- Soliman, H.; Ahmed, S.; Ibrahim, A. Waist-to-height ratio as a clinical predictor for cardiovascular risks and insulin resistance in children and adolescents with exogenous obesity. Gaz. Egypt. Paediatr. Assoc. 2021, 69, 38. [Google Scholar] [CrossRef]
- Morinder, G.; Mattsson, E.; Sollander, C.; Marcus, C.; Larsson, U.E. Six-minute walk test in obese children and adolescents: Reproducibility and validity. Physiother. Res. Int. 2009, 14, 91–104. [Google Scholar] [CrossRef]
- Fanelli, E.; Abate Daga, F.; Pappaccogli, M.; Eula, E.; Astarita, A.; Mingrone, G.; Fasano, C.; Magnino, C.; Schiavone, D.; Rabbone, I.; et al. A structured physical activity program in an adolescent population with overweight or obesity: A prospective interventional study. Appl. Physiol. Nutr. Metab. 2022, 47, 253–260. [Google Scholar] [CrossRef]
- Fit Mate User Manual, XIV ed.; COSMED Srl: Roma, Italy, 2012.
- Borys, J.M.; Le Bodo, Y.; Jebb, S.A.; Seidell, J.C.; Summerbell, C.; Richard, D.; De Henauw, S.; Moreno, L.A.; Romon, M.; Visscher, T.L.S.; et al. EPODE approach for childhood obesity prevention: Methods, progress and international development. Obes. Rev. 2012, 13, 299–315. [Google Scholar] [CrossRef] [Green Version]
- Chen, P.S.; Chang, K.C.; Chang, C.H.; Chen, Y.T.; Huang, H.W.; Tsai, S.M.; Yang, H.R.; Tung, Y.C.; Wu, W.W.; Chen, H.L. The effect of a multidisciplinary lifestyle modification program for obese and overweight children. J. Formos. Med. Assoc. 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Tessaris, D.; Matarazzo, P.; Tuli, G.; Tuscano, A.; Rabbone, I.; Spinardi, A.; Lezo, A.; Fenocchio, G.; Buganza, R.; de Sanctis, L. Multidisciplinary Approach for Hypothalamic Obesity in Children and Adolescents: A Preliminary Study. Children 2021, 8, 531. [Google Scholar] [CrossRef] [PubMed]
- Bharath, L.P.; Choi, W.W.; Cho, J.M.; Skobodzinski, A.A.; Wong, A.; Sweeney, T.E.; Park, S.Y. Combined resistance and aerobic exercise training reduces insulin resistance and central adiposity in adolescent girls who are obese: Randomized clinical trial. Eur. J. Appl. Physiol. 2018, 118, 1653–1660. [Google Scholar] [CrossRef] [PubMed]
- Ells, L.J.; Rees, K.; Brown, T.; Mead, E.; Al-Khudairy, L.; Azevedo, L.; McGeechan, G.J.; Baur, L.; Loveman, E.; Clements, H. Interventions for treating children and adolescents with overweight and obesity: An overview of Cochrane reviews. Int. J. Obes. 2018, 42, 1823–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, J.C.K.; Fewtrell, M.S. Is body composition important for paediatricians? Arch. Dis. Child. 2008, 93, 168–172. [Google Scholar] [CrossRef]
- Lindholm, A.; Roswall, J.; Alm, B.; Almquist-Tangen, G.; Bremander, A.; Dahlgren, J.; Staland-Nyman, C.; Bergman, S. Body mass index classification misses to identify children with an elevated waist-toheight ratio at 5 years of age. Pediatric. Res. 2019, 85, 30–32. [Google Scholar] [CrossRef]
- Adom, T.; De Villiers, A.; Puoane, T.; Kengne, A.P. School-based interventions targeting nutrition and physical activity, and body weight status of african children: A systematic review. Nutrients 2019, 12, 95. [Google Scholar] [CrossRef] [Green Version]
- Fredriksen, P.M.; Skår, A.; Mamen, A. Waist circumference in 6–12-year-old children: The Health Oriented Pedagogical Project (HOPP). Scand. J. Public Health 2018, 46, 12–20. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, H.D.; Ashwell, M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message-‘keep your waist circumference to less than half your height’. Int. J. Obes. 2006, 30, 988–992. [Google Scholar] [CrossRef] [Green Version]
- Ali, O.; Cerjak, D.; Kent, J.W.; James, R.; Blangero, J.; Zhang, Y. Obesity, central adiposity and cardiometabolic risk factors in children and adolescents: A family-based study. Pediatric. Obes. 2014, 9, e58–e62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, E.G. Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk. Korean J. Pediatr. 2016, 59, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.; Kuh, D.; Hardy, R. Mortality Review Group; FALCon and HALCyon Study Teams. Objectively measured physical capability levels and mortality: Systematic review and meta-analysis. BMJ 2010, 341, c4467. [Google Scholar] [CrossRef] [Green Version]
- Thivel, D.; Ring-Dimitriou, S.; Weghuber, D.; Frelut, M.; O’Malley, G. Muscle Strength and Fitness in Pediatric Obesity: A Systematic Review from the European Childhood Obesity Group. Obes. Facts. 2016, 9, 52–63. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Fu, A.; Cobley, S.; Sanders, R.H. Effectiveness of exercise intervention on improving fundamental movement skills and motor coordination in overweight/obese children and adolescents: A systematic review. J. Sci. Med. Sport 2018, 21, 89–102. [Google Scholar] [CrossRef]
- Bonney, E.; Ferguson, G.; Burgess, T.; Smits-Engelsman, B. Benefits of Activity-Based Interventions Among Female Adolescents Who Are Overweight and Obese. Pediatr. Phys. Ther. 2019, 31, 338–345. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Wiemer, D.M.; Federman, S.M. Grip and pinch strength: Norms for 6- to 19-years-olds. Am. J. Occup. Ther. 1986, 40, 705–711. [Google Scholar] [CrossRef] [Green Version]
- Sartorio, A.; Lafortuna, C.L.; Pogliaghi, S.; Trecate, L. The impact of gender, body dimension and body composition on hand-grip strength in healthy children. J. Endocrinol. Investig. 2002, 25, 431–435. [Google Scholar] [CrossRef]
- Link, L.; Lukens, S.; Bush, M.A. Spherical grip strength in children 3 to 6 years of age. Am. J. Occup. Ther. 1995, 49, 318–326. [Google Scholar] [CrossRef] [Green Version]
- Montalcini, T.; Ferro, Y.; Salvati, M.A.; Romeo, S.; Miniero, R.; Pujia, A. Gender difference in handgrip strength of Italian children aged 9 to 10 years. Ital. J. Pediatr. 2016, 42, 16. [Google Scholar] [CrossRef] [Green Version]
- Karpowicz, K. Interrelation of selected factors determining the effectiveness of training in young basketball players. Hum. Mov. 2006, 7, 130–146. [Google Scholar]
- Kemper, H.C.G. Change in the mindset of a paediatric exercise physiologist: A review of fifty years research. Int. J. Environ. Res. Public Health 2020, 17, 2888. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacchetti, R.; Ceciliani, A.; Garulli, A.; Masotti, A.; Poletti, G.; Beltrami, P.; Leoni, E. Physical fitness of primary school children in relation to overweight prevalence and physical activity habits. J. Sports Sci. 2012, 30, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Vizcaíno, V.; Pozuelo-Carrascosa, D.P.; García-Prieto, J.C.; Cavero-Redondo, I.; Solera-Martínez, M.; Garrido-Miguel, M.; Díez-Fernández, A.; Ruiz-Hermosa, A.; Sánchez-López, M. Effectiveness of a school-based physical activity intervention on adiposity, fitness and blood pressure: MOVI-KIDS study. Br. J. Sports Med. 2020, 54, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Magnani, B.; Rizzardini, M.; Gemelli, T.; Cusella De Angelis, G. Attività sport-specifica nel pre-adolescente: Un approccio sperimentale. Sport Anat. 2016, 1, 8–13. [Google Scholar]
| Children | Gender Group Category | ||||
| Girls | Boys | Boys vs. Girls | |||
| Mn ± SD | Mn ± SD | Mn ± SD | F | p | |
| Weight (kg) | 61.64 ± 13.33 | 64.32 ± 11.54 | 58.73 ± 14.65 | 3.219 | 0.077 |
| Fat mass (%) | 40.06 ± 4.99 | 40.48 ± 3.79 | 39.61 ± 6.07 | 0.534 | 0.468 |
| Fat-free mass (kg) | 25.10 ± 7.34 | 26.12 ± 5.76 | 23.99 ± 8.70 | 2.154 | 0.147 |
| BMI (kg/m2) | 28.81 ± 3.8 | 28.77 ± 2.41 | 28.85 ± 4.05 | 0.11 | 0.916 |
| WC (cm) | 94.09 ± 8.58 | 94.12 ± 8.50 | 94.05 ± 8.91 | 0.001 | 0.980 |
| WHTR | 0.63 ± 0.04 | 0.63 ± 0.05 | 0.64 ± 0.04 | 0.197 | 0.660 |
| MBT forward (cm) | 4.49 ± 1.02 | 4.53 ± 1.04 | 4.45 ± 1.02 | 0.103 | 0.749 |
| MBT backward (cm) | 4.70 ± 1.34 | 4.79 ± 1.46 | 4.62 ± 1.23 | 0.223 | 0.639 |
| ST (kg) | 20.28 ± 6.80 | 22.04 ± 7.25 | 18.64 ± 6.02 | 3.524 | 0.066 |
| HG test for right hand (kg) | 16.48 ± 4.51 | 16.90 ± 5.21 | 15.79 ± 3,14 | 0.556 | 0.461 |
| HG test for left hand (kg) | 14.53 ± 3.42 | 14.15 ± 3.32 | 15.24 ± 3.63 | 0.841 | 0.365 |
| 6 MWT (m) | 712.27 ± 96.41 | 717.25 ± 99.40 | 707.13 ± 94.52 | 0.177 | 0.676 |
| 30 mt speed (s) | 1.13 ± 4.33 | 6.69 ± 1.13 | 7.00 ± 1.12 | 1228 | 0.272 |
| VB (cm) | −3.42 ± 7.97 | 1.09 ± 6.21 | −8.06 ± 6.89 | 31.707 | <0.001 |
| HB (cm) | 32.36 ± 7.83 | 35.81 ± 6.31 | 29.04 ± 7.80 | 12.506 | 0.001 |
| Adolescents | Gender Group Category | ||||
| Girls | Boys | Boys vs. Girls | |||
| Mn ± SD | Mn ± SD | Mn ± SD | F | p | |
| Weight (kg) | 90.12 ± 17.52 | 83.23 ± 14.89 | 99.30 ± 16.79 | 12.520 | 0.001 |
| Fat mass (%) | 39.05 ± 7.55 | 40.20 ± 6.42 | 37.51 ± 8.78 | 1.541 | 0.221 |
| Fat-free mass (kg) | 53.43 ± 9.36 | 48.53 ± 6.06 | 59.73 ± 9.17 | 25.874 | <0.001 |
| BMI (kg/m2) | 32.88 ± 5.09 | 31.58 ± 4.99 | 34.61 ± 4.80 | 4.562 | 0.038 |
| WC (cm) | 106.79 ± 12.42 | 103.52 ± 11.76 | 111.26 ± 12.19 | 4.615 | 0.037 |
| WHTR | 0.65 ± 0.07 | 0.64 ± 0.07 | 0.66 ± 0.07 | 1.283 | 0.264 |
| Lat machine (kg) | 36.20 ± 9.54 | 32.05 ± 5.14 | 40.97 ± 11.23 | 11.707 | 0.001 |
| Chest press (kg) | 28.54 ± 9.43 | 24.06 ± 6.04 | 33.70 ± 10.10 | 14.877 | <0.001 |
| Leg press (kg) | 168.26 ± 53.34 | 156.78 ± 39.52 | 181.46 ± 64.32 | 2.365 | 0.132 |
| Leg extension (kg) | 34.79 ± 13.33 | 30.94 ± 12.42 | 39.45 ± 13.21 | 4.608 | 0.038 |
| HG test for right hand (kg) | 22.90 ± 8.93 | 20.22 ± 10.34 | 26.34 ± 5.70 | 1.969 | 0.182 |
| HG test for left hand (kg) | 20.64 ± 8.59 | 17.99 ± 9.06 | 24.05 ± 7.14 | 2.106 | 0.169 |
| VB (cm) | −6.06 ± 9.53 | −3.89 ± 12.09 | −8.22 ± 6.02 | 0.927 | 0.350 |
| HB (cm) | 29.28 ± 9.75 | 31.11 ± 10.78 | 27.44 ± 8.85 | 0.622 | 0.442 |
| VO2 max (mL/min/kg) | 28.96 ± 5.25 | 26.05 ± 3.89 | 32.19 ± 4.77 | 9.540 | 0.007 |
| Children | T0 | T1 | Time T0 vs. T1 | Time * Gender Group Category | ||
| Mn ± SD | Mn ± SD | p | Partial η2 | p | Partial η2 | |
| Weight (kg) | 62.04 ± 12.15 | 62.94 ± 11.76 | 0.092 | 0.046 | 0.310 | 0.017 |
| Fat mass (%) | 40.29 ± 4.46 | 36.63 ± 5.38 | <0.001 | 0.507 | 0.559 | 0.006 |
| Fat-free mass (kg) | 36.79 ± 7.08 | 39.62 ± 6.86 | <0.001 | 0.482 | 0.217 | 0.025 |
| BMI (kg/m2) | 28.59 ± 2.80 | 27.97 ± 2.84 | 0.012 | 0.106 | 0.790 | 0.001 |
| WC (cm) | 94.62 ± 8.15 | 91.03 ± 7.88 | <0.001 | 0.449 | 0.935 | <0.001 |
| WHtR | 0.64 ± 0.04 | 0.53 ± 0.21 | 0.004 | 0.261 | 0.882 | 0.001 |
| MBT forward (cm) | 4.52. ± 1.04 | 4.98 ± 1.07 | <0.001 | 0.326 | 0.584 | 0.005 |
| MBT backward (cm) | 4.76 ± 1.36 | 5.48 ± 1.71 | <0.001 | 0.388 | 0.554 | 0.007 |
| ST (kg) | 20.83 ± 7.21 | 24.22 ± 7.64 | <0.001 | 0.340 | 0.637 | 0.005 |
| HG test for right hand (kg) | 16.65 ± 4.57 | 18.15 ± 5.43 | 0.042 | 0.113 | 0.175 | 0.052 |
| HG test for left hand (kg) | 14.40 ± 3.54 | 15.33 ± 5.13 | 0.214 | 0.048 | 0.560 | 0.011 |
| 6 MWT (m) | 715.34 ± 97.86 | 775.50 ± 126.91 | <0.001 | 0.371 | 0.392 | 0.013 |
| 30 mt speed (s) | 6.80 ± 1.18 | 6.19 ± 0.95 | <0.001 | 0.577 | 0.650 | 0.004 |
| VB (cm) | −3.48 ± 8.22 | −1.81 ± 8.16 | 0.006 | 0.127 | 0.123 | 0.041 |
| HB (cm) | 32.41 ± 8.05 | 34.16 ± 8.39 | 0.016 | 0.117 | 0.778 | 0.002 |
| Adolescents | T0 | T1 | Time T0 vs. T1 | Time * Gender Group Category | ||
| Mn ± SD | Mn ± SD | p | Partial η2 | p | Partial η2 | |
| Weight (kg) | 90.23 ± 16.52 | 88.13 ± 17.51 | 0.014 | 0.255 | 0.646 | 0.10 |
| Fat mass (%) | 40.57 ± 6.83 | 36.97 ± 7.41 | <0.001 | 0.526 | 0.198 | 0.078 |
| Fat-free mass (kg) | 52.96 ± 7.13 | 54.83 ± 8.58 | 0.020 | 0.233 | 0.119 | 0.112 |
| BMI (kg/m2) | 32.71 ± 5.41 | 31.67 ± 5.78 | <0.001 | 0.461 | 0.791 | 0.003 |
| WC (cm) | 105.913 ± 12.80 | 101.87 ± 11.25 | 0.001 | 0.445 | 0.956 | <0.001 |
| WHtR | 0.64 ± 0.08 | 0.61 ± 0.07 | <0.001 | 0.497 | 0.764 | 0.004 |
| Lat machine (kg) | 38.23 ± 9.69 | 46.82 ± 11.09 | <0.001 | 0.780 | 0.320 | 0.032 |
| Chest press (kg) | 30.77 ± 9.50 | 40.33 ± 12.51 | <0.001 | 0.733 | 0.214 | 0.049 |
| Leg press (kg) | 174.73 ± 57.26 | 215.48 ± 66.13 | <0.001 | 0.548 | 0.732 | 0.004 |
| Leg extension (kg) | 37.10 ± 12.53 | 54.13 ± 14.70 | <0.001 | 0.712 | 0.691 | 0.005 |
| HG test for right hand (kg) | 23.18 ± 8.60 | 18.05 ± 6.15 | 0.016 | 0.370 | 0.407 | 0.054 |
| HG test for left hand (kg) | 21.52 ± 8.13 | 16.54 ± 5.94 | 0.018 | 0.359 | 0.367 | 0.063 |
| VB (cm) | −6.06 ± 9.53 | −4.22 ± 10.51 | 0.145 | 0.128 | 0.964 | <0.001 |
| HB (cm) | 29.28 ± 9.75 | 30.61 ± 10.40 | 0.165 | 0.117 | 0.553 | 0.022 |
| VO2 max | 28.97 ± 5.40 | 30.16 ± 6.11 | 0.169 | 0.115 | 0.852 | 0.002 |
| (a) | ||||||
| Boys | Girls | |||||
| Δ Mean ± SD | t | p | Δ Mean ± SD | t | p | |
| Weight (kg) | 0.35 ± 3.04 | 0.636 | 0.530 | 1.40 ± 4.79 | 1.678 | 0.103 |
| Height (cm) | 2.81 ± 3.15 | 4.892 | <0.001 | 3.48 ± 2.68 | 7.455 | <0.001 |
| Fat mass (%) | −3.53 ± 3.67 | −5.901 | <0.001 | −3.40 ± 3.70 | −5.288 | <0.001 |
| Fat mass (kg) | −1.66 ± 4.00 | −2.270 | 0.031 | −1.58 ± 3.70 | −2.459 | 0.020 |
| Fat-free mass (kg) | 2.35 ± 2.72 | 4.731 | <0.001 | 3.28 ± 3.16 | 5.958 | <0.001 |
| BMI (kg/m2) | −0.69 ± 1.84 | −2.022 | 0.053 | −0.56 ± 1.85 | −1.660 | 0.108 |
| WC (cm) | −3.53 ± 3.20 | −4.542 | <0.001 | −3.64 ± 4.57 | −3.730 | 0.001 |
| WHtR | −0.12 ± 0.22 | −2.058 | 0.060 | −0.11 ± 0.18 | −2.407 | 0.029 |
| MBT forward (cm) | 0.41 ± 0.77 | 2.934 | 0.006 | 0.51 ± 0.56 | 4.958 | <0.001 |
| MBT backward (cm) | 0.79 ± 0.94 | 4.305 | <0.001 | 0.64 ± 0.89 | 3.512 | 0.002 |
| ST (kg) | 3.08 ± 5.38 | 2.860 | 0.009 | 3.76 ± 4.12 | 4.182 | <0.001 |
| HG test for right hand (kg) | 2.84 ± 5.45 | 2.020 | 0.063 | 0.59 ± 4.42 | 0.630 | 0.535 |
| HG test for left hand (kg) | 0.45 ± 3.78 | 0.432 | 0.674 | 1.24 ± 3.77 | 1.502 | 0.149 |
| 6 MWT (m) | 69.03 ± 85.17 | 4.440 | <0.001 | 51.28 ± 73.78 | 3.807 | 0.001 |
| 30 mt speed (s) | −0.64 ± 0.59 | −5.823 | <0.001 | 0.58 ± 0.48 | 6.450 | <0.001 |
| VB (cm) | 2.59 ± 4.85 | 2.871 | 0.008 | 0.77 ± 4.06 | 1.035 | 0.309 |
| HB (cm) | 1.56 ± 4.40 | 1.774 | 0.089 | 1.96 ± 5.42 | 1.771 | 0.090 |
| (b) | ||||||
| Boys | Girls | |||||
| Δ Mean ± SD | t | p | Δ Mean ± SD | t | p | |
| Weight (kg) | −1.67 ± 3.75 | −1.337 | 0.218 | −2.37 ± 3.39 | −2.621 | 0.021 |
| Height (cm) | 1.5 ± 1.04 | 4.310 | 0.003 | 0.26 ± 0.95 | 1.046 | 0.314 |
| Fat mass (%) | −4.89 ± 5.09 | −2.881 | 0.020 | −2.78 ± 2.53 | −4.107 | 0.001 |
| Fat mass (kg) | −3.12 ± 4.33 | −2.161 | 0.063 | −3.19 ± 2.36 | −5.045 | <0.001 |
| Fat-free mass (kg) | 3.57 ± 5.09 | 2.108 | 0.068 | 0.77 ± 3.21 | 0.898 | 0.386 |
| BMI (kg/m2) | −1.12 ± 0.99 | −3.388 | 0.010 | −0.99 ± 1.26 | −2.940 | 0.011 |
| WC (cm) | −4.11 ± 2.62 | −4.709 | 0.002 | −4.00 ± 5.51 | −2.719 | 0.018 |
| WHtR | −0.29 ± 0.02 | −5.942 | <0.001 | −0.03 ± 0.03 | −2.828 | 0.014 |
| Lat (kg) | 9.28 ± 4.11 | 9.828 | <0.001 | 7.65 ± 5.17 | 5.533 | <0.001 |
| Chest (kg) | 10.65 ± 6.86 | 6.766 | <0.001 | 8.08 ± 3.73 | 8.105 | <0.001 |
| Leg (kg) | 38.79 ± 41.51 | 4.073 | 0.001 | 43.52 ± 31.76 | 4.940 | <0.001 |
| Legext (kg) | 17.67 ± 12.57 | 6.126 | <0.001 | 16.10 ± 7.73 | 7.509 | <0.001 |
| HG test for right hand (kg) | −7.58 ± 5.75 | −3.485 | 0.013 | −3.99 ± 9.65 | −1.168 | 0.281 |
| HG test for left hand (kg) | −6.86 ± 6.58 | −2.759 | 0.033 | −3.33 ± 7.86 | −1.198 | 0.270 |
| VB (cm) | 1.78 ± 6.18 | 0.863 | 0.413 | 1.89 ± 3.66 | 1.550 | 0.160 |
| HB (cm) | 1.89 ± 3.06 | 1.852 | 0.101 | 0.78 ± 4.68 | 0.510 | 0.624 |
| VO2 max | 1.33 ± 4.28 | 0.934 | 0.378 | 1.02 ± 2.40 | 1.279 | 0.237 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pippi, R.; Mascherini, G.; Izzicupo, P.; Bini, V.; Fanelli, C.G. Effects of a Mixed Exercise Program on Overweight and Obese Children and Adolescents: A Pilot, Uncontrolled Study. Int. J. Environ. Res. Public Health 2022, 19, 9258. https://doi.org/10.3390/ijerph19159258
Pippi R, Mascherini G, Izzicupo P, Bini V, Fanelli CG. Effects of a Mixed Exercise Program on Overweight and Obese Children and Adolescents: A Pilot, Uncontrolled Study. International Journal of Environmental Research and Public Health. 2022; 19(15):9258. https://doi.org/10.3390/ijerph19159258
Chicago/Turabian StylePippi, Roberto, Gabriele Mascherini, Pascal Izzicupo, Vittorio Bini, and Carmine Giuseppe Fanelli. 2022. "Effects of a Mixed Exercise Program on Overweight and Obese Children and Adolescents: A Pilot, Uncontrolled Study" International Journal of Environmental Research and Public Health 19, no. 15: 9258. https://doi.org/10.3390/ijerph19159258
APA StylePippi, R., Mascherini, G., Izzicupo, P., Bini, V., & Fanelli, C. G. (2022). Effects of a Mixed Exercise Program on Overweight and Obese Children and Adolescents: A Pilot, Uncontrolled Study. International Journal of Environmental Research and Public Health, 19(15), 9258. https://doi.org/10.3390/ijerph19159258








