Big Data to Knowledge Analytics Reveals the Zika Virus Epidemic as Only One of Multiple Factors Contributing to a Year-Over-Year 28-Fold Increase in Microcephaly Incidence
Abstract
:1. Introduction
Understanding the Complex Associations between a Zika Virus (ZIKV) Outbreak, Environmental Exposure to Chemical and Non-Chemical Stressors, and ZIKV-Related and Non-Zika-Related Microcephaly
2. Methods
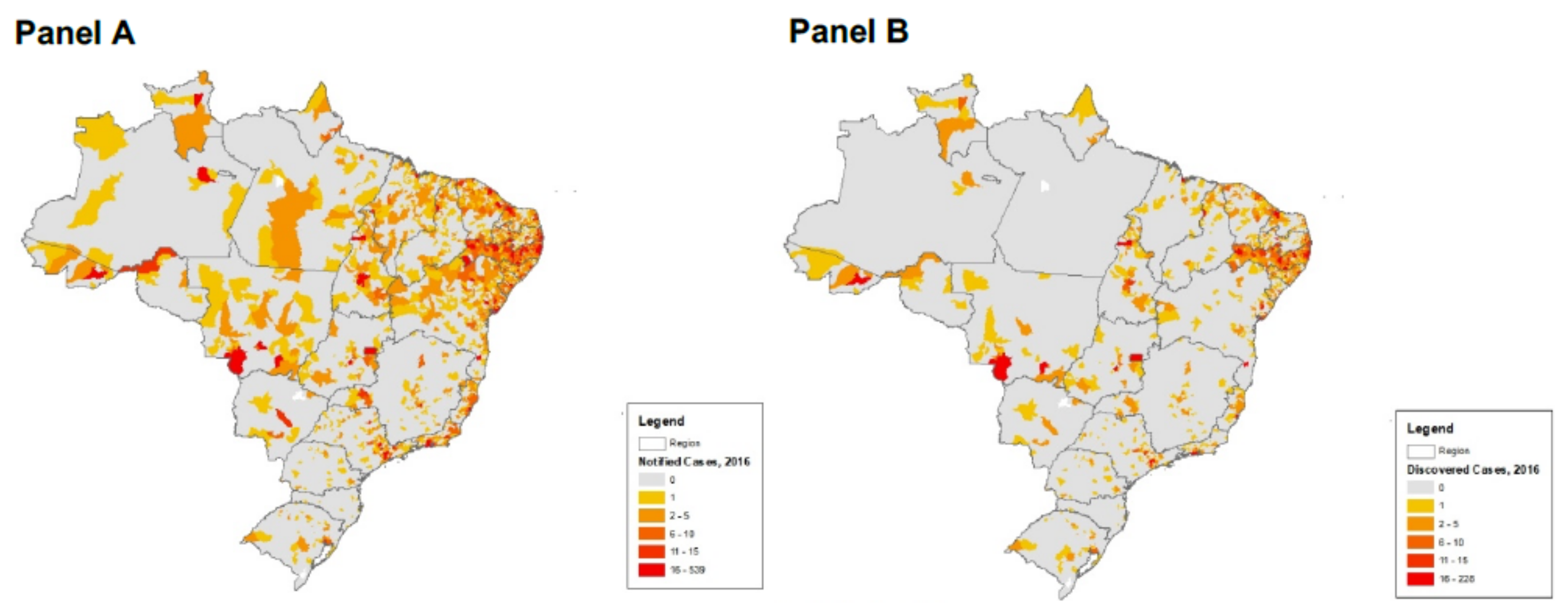
2.1. Data Collection, Integration, and Preprocessing
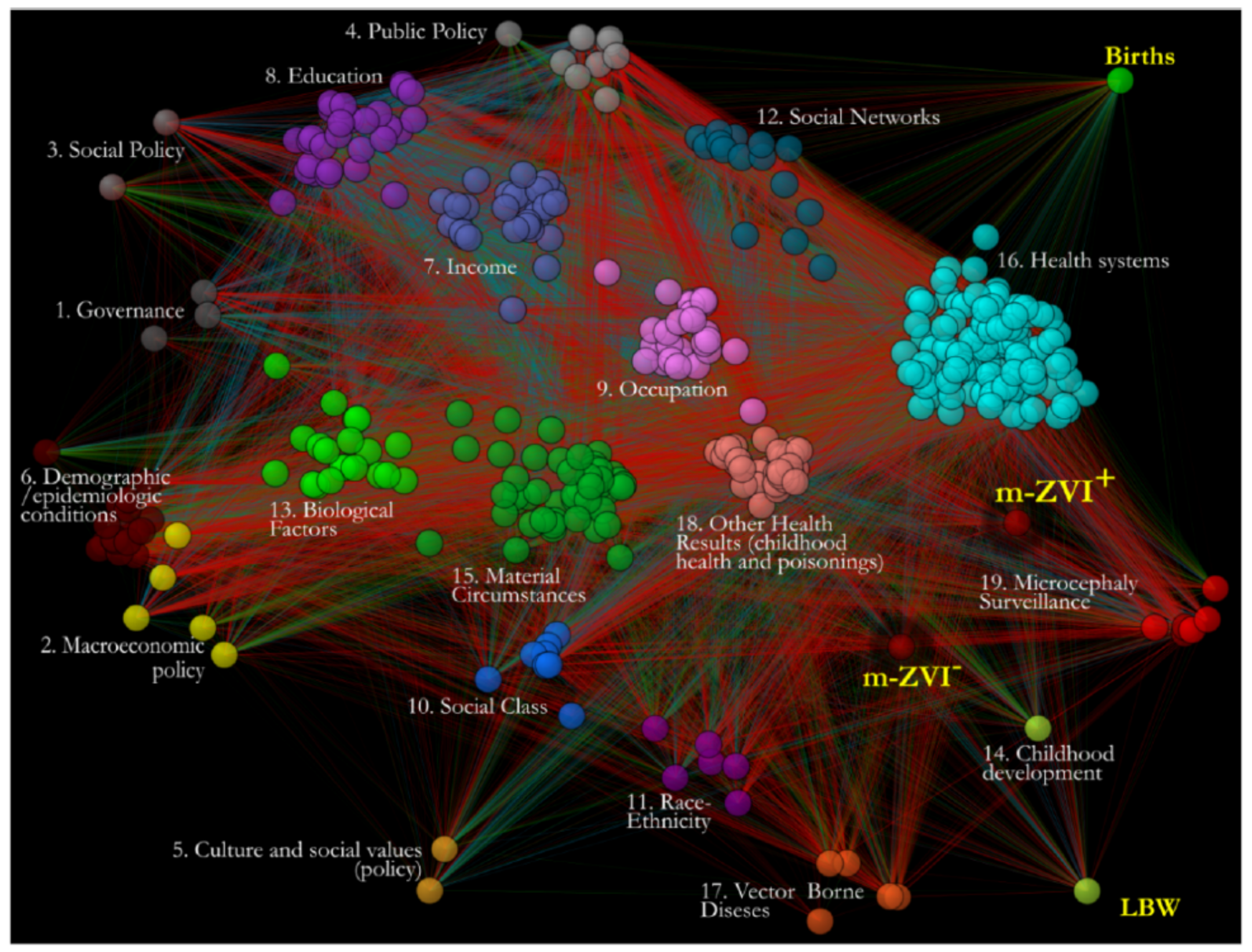
2.2. Network Generation
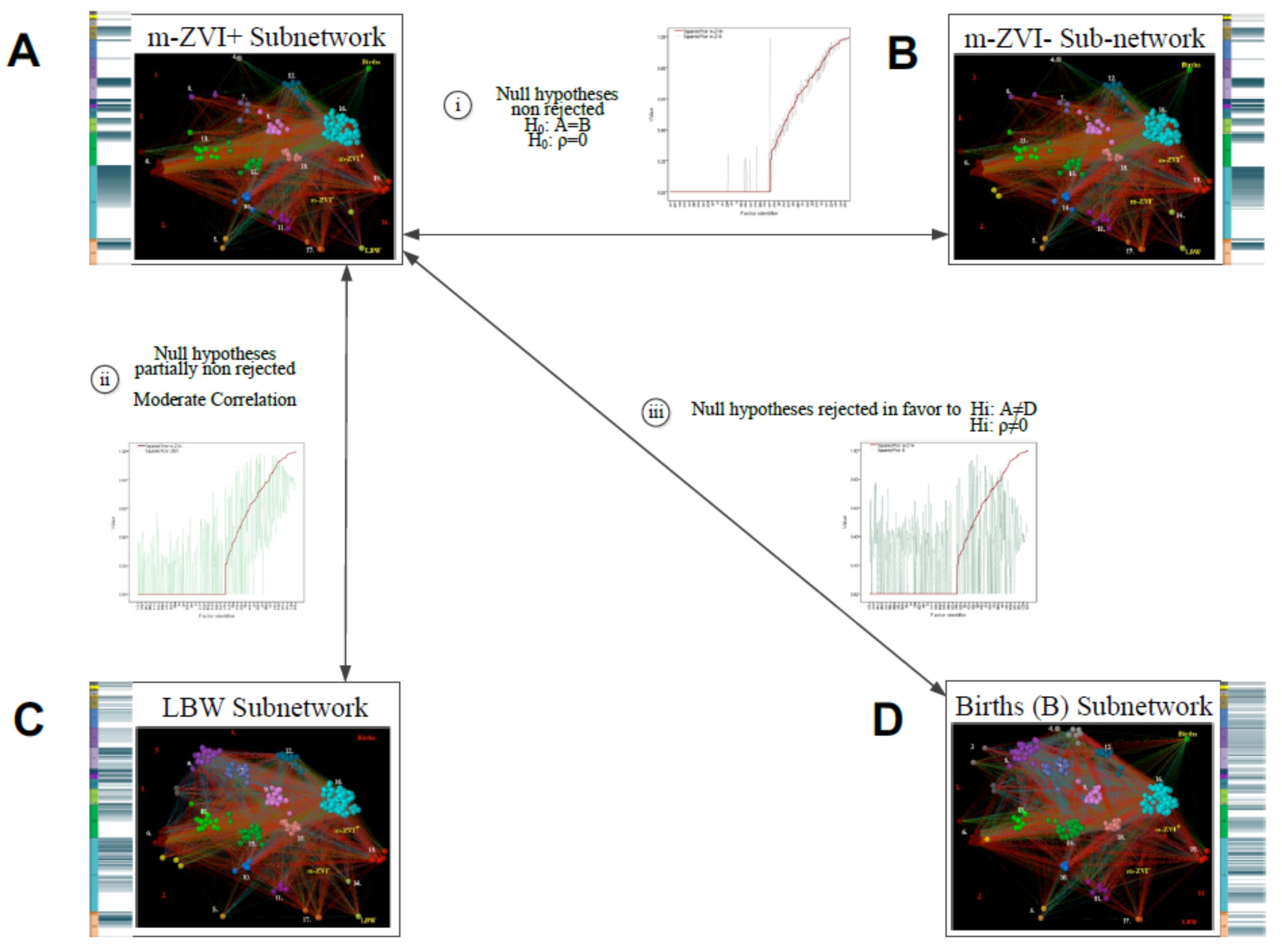
2.3. Inferential Network Analysis by Subnetwork Comparison
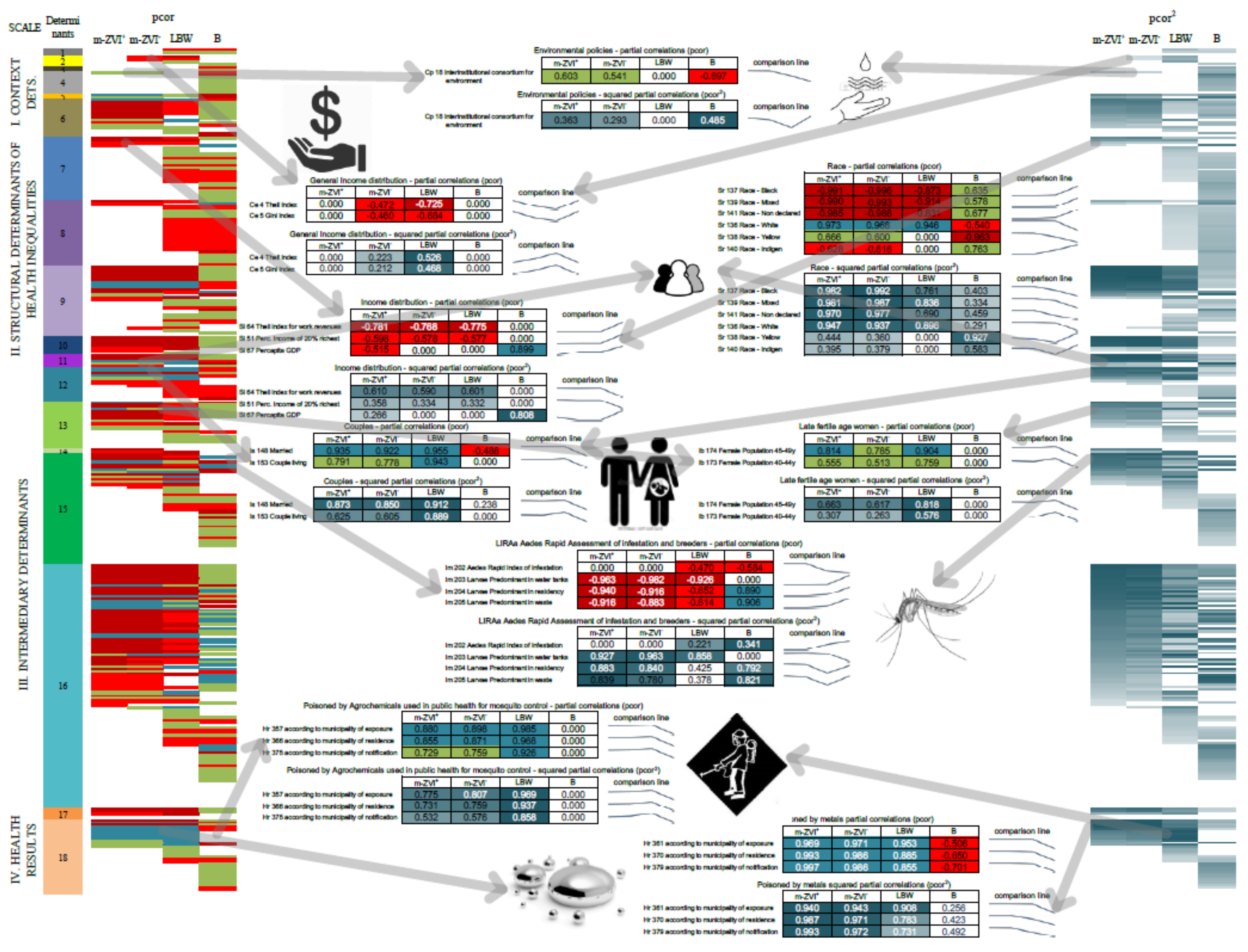
3. Results
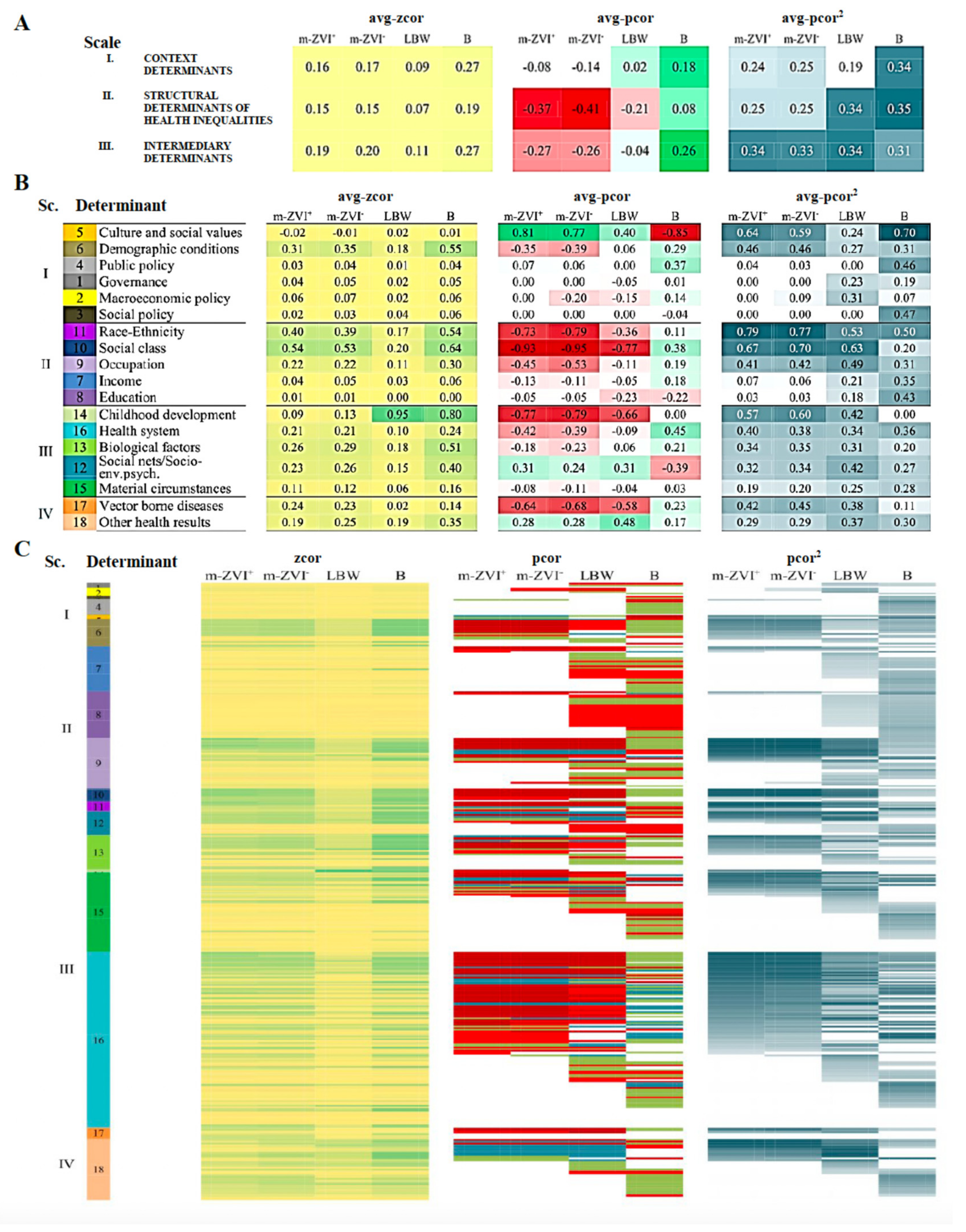
3.1. General Pattern of Factors Associated with Microcephaly Is Not Specific for m-ZIKV+
3.2. Factors That Explained the Non-Specific Pattern of Associations of m-ZIKV+
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Zika Virus Outbreak Global Response. 2016. Available online: http://www.who.int/emergencies/zika-virus/response/en/ (accessed on 16 March 2017).
- Brady, O.J.; Osgood-Zimmerman, A.; Kassebaum, N.J.; Ray, S.E.; de Araújo, V.E.M.; da Nóbrega, A.A.; Frutuoso, L.C.V.; Lecca, R.C.R.; Stevens, A.; de Oliveira, B.Z.; et al. The association between Zika virus infection and microcephaly in Brazil 2015–2017: An observational analysis of over 4million births. PLoS Med. 2019, 16, e1002755. [Google Scholar] [CrossRef] [PubMed]
- Plourde, A.R.; Bloch, E.M. A Literature Review of Zika Virus. Emerg. Infect. Dis. 2016, 22, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Oliveira, W.K.; Cortez-escalante, J.; Tenório, W.; Holanda, G.; Madeleine, G. Increase in reported prevalence of microcephaly in infants born to women living in areas with confirmed Zika virus transmission during the first trimester of pregnancy—Brazil, 2015. Morb. Mortal. Wkly. Rep. 2016, 65, 242–247. [Google Scholar] [CrossRef] [PubMed]
- WHO. Zika Virus and Complications. WHO Webpage 2016. Available online: http://www.who.int/emergencies/zika-virus/en/ (accessed on 16 March 2017).
- WHO. WHO Director-General Summarizes the Outcome of the Emergency Committee Regarding Clusters of Microcephaly and Guillain-Barré Syndrome. 2016. Available online: http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/ (accessed on 16 March 2017).
- WHO. The History of Zika Virus. 2016. Available online: http://www.who.int/emergencies/zika-virus/history/en/) (accessed on 16 March 2017).
- WHO. Situation Report: Zika Virusn Microcephaly, Guillain-Barré Syndrome. 30 June 2016. Available online: http://www.who.int/emergencies/zika-virus/situation-report/30-june-2016/en/ (accessed on 16 March 2017).
- COES. Informe Epidemiológico N° 32-SE 25/2016. Monitoramento dos Casos de Microcefalia no Brasil. 2016. Available online: http://combateaedes.saude.gov.br/images/pdf/informe_microcefalia_epidemiologico_32.pdf (accessed on 16 March 2017).
- Kim, S. ppcor: An R Package for a Fast Calculation to Semi-partial Correlation Coefficients. Commun. Stat. Appl. Methods. 2015, 22, 665–674. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grayo, S. Is the ZIKV congenital syndrome and microcephaly due to syndemism latent virus coinfection? Viruses 2021, 13, 669. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Larroque, A.; Kranjec, E.; Drapeau, P.; Samarut, E. The larvicide pyriproxyfen blamed during the Zika virus outbreak does not cause microcephaly in zebrafish embryos. Nat. Publ. Gr. 2017, 7, 40067. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Truong, L.; Gonnerman, G.; Simonich, M.T.; Tanguay, R.L. Assessment of the developmental and neurotoxicity of the mosquito control larvicide, pyriproxyfen, using embryonic zebrafish. Environ. Pollut. 2016, 218, 1089–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parens, R.; Yam, Y.B. Zika and Other Potential Causes of Microcephaly in Brazil; New England Complex Systems Institute: Cambridge, MA, USA, 2016. [Google Scholar]
- Bar-Yam, Y.; Costa, F.; Parens, R.; Morales, A.J.; Nijhout, F. Determining the Rate and Week of Infection of Zika Caused Microcephaly from Colombian and Brazilian Data; Status Report 1 August 2016; New England Complex Systems Institute: Cambridge, MA, USA, 2016; pp. 1–7. [Google Scholar]
- Butler, D. Brazil asks whether Zika acts alone to cause birth defects. Nature. 2016, 535, 475–476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Lancet Global Health. The right(s) approach to Zika. Lancet Glob. Health 2016, 4, e427. [Google Scholar] [CrossRef] [Green Version]
- Stettler, K.; Beltramello, M.; Espinosa, D.A.; Graham, V.; Cassotta, A.; Bianchi, S.; Vanzetta, F.; Minola, A.; Jaconi, S.; Mele, F.; et al. Specificity, cross-reactivity and function of antibodies elicited by Zika virus infection. Science 2016, 353, 823–826. [Google Scholar] [CrossRef] [Green Version]
- WHO. WHO—Dispelling Rumours around Zika and Complications. WHO. 2016. Available online: http://www.who.int/emergencies/zika-virus/articles/rumours/en/ (accessed on 16 March 2017).
- da Saúde, M. Ministério da Saúde divulga novos dados de microcefalia. Portal da Saude SUS Bras. 2016. [Google Scholar]
- Harris, S.R. Measuring head circumference. Update on infant microcephaly. Can. Fam. Phys. 2015, 61, 680–684. [Google Scholar]
- Simmins, C.H., Jr. Establishing base levels of microcephaly in Brazil prior to the arrival of Zika viral illnesses. Bull. World Health Organ. Open 2016, 1–8. [Google Scholar] [CrossRef]
- Gullo, G.; Scaglione, M.; Cucinella, G.; Riva, A.; Coldebella, D.; Cavaliere, A.F.; Signore, F.; Buzzaccarini, G.; Spagnol, G.; Laganà, A.S.; et al. Congenital Zika syndrome: Genetic avenues for diagnosis and therapy, possible management and long-term outcomes. J. Clin. Med. 2022, 11, 1351. [Google Scholar] [CrossRef] [PubMed]
- Miller, G.W. The Exposome: A Primer; Elsevier: Waltham, MA, USA, 2013; Available online: http://books.google.com.au/books?id=USKcAAAAQBAJ (accessed on 16 March 2017).
- Rappaport, S.M.; Smith, M.T. Environment and Disease Risks. Science 2010, 330, 460–461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juarez, P.D.; Matthews-Juarez, P.; Hood, D.B.; Im, W.; Levine, R.S.; Kilbourne, B.J.; Langston, M.A.; Al-Hamdan, M.Z.; Crosson, W.L.; Estes, M.G.; et al. The public health exposome: A population-based, exposure science approach to health disparities research. Int. J. Environ. Res. Public Health 2014, 11, 12866–12895. [Google Scholar] [CrossRef]
- Cifuentes, P.; Reichard, J.; Im, W.; Smith, S.; Colen, C.; Giurgescu, C.; Williams, K.P.; Gillespie, S.; Juarez, P.D.; Hood, D.B. Application of the Public Health Exposome Framework to Estimate Phenotypes of Resilience in a Model Ohio African-American Women’s Cohort. J. Urban. Health. 2019, 96 (Suppl. S1), 57–71. [Google Scholar] [CrossRef] [PubMed]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of HEALTH. Social Determinants of Health Discussion Paper 2; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- IBGE. Cartografia; IBGE: Rio de Janeiro, Brazil, 2016. [Google Scholar]
- Kim, S. ppcor: An R Package for a Fast Calculation to Semi-partial Correlation Coefficients. Commun. Stat. Appl. Methods 2015, 22, 665–674. [Google Scholar]
- Scutari, M. Learning Bayesian Networks with the bnlearn R Package. J. Stat. Softw. 2010, 35, 1–22. [Google Scholar] [CrossRef] [Green Version]
- Pržulj, N.; Corneil, D.G.; Jurisica, I. Modeling interactome: Scale-free or geometric? Bioinformatics 2004, 20, 3508–3515. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yaveroğlu, Ö.N.; Malod-Dognin, N.; Davis, D.; Levnajic, Z.; Janjic, V.; Karapandza, R.; Stojmirovic, A.; Pržulj, N. Revealing the Hidden Language of Complex Networks. Sci. Rep. 2014, 4, 4547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mrvar, A.; Batagelj, V. Analysis and visualization of large networks with program package Pajek. Complex Adapt Syst Model 2016, 4, 6. [Google Scholar] [CrossRef] [Green Version]
- Pržulj, N. Biological network comparison using graphlet degree distribution. Bioinformatics 2007, 23, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Sheskin, D.J. Handbook of Parametric and Nonparametric Statistical Procedures; Chapman & Hall/CRC: New York, NY, USA, 2004; Available online: http://books.google.es/books?id=YDd2cgAACAAJ (accessed on 20 April 2018).
- Jacob, C.; Cohen, P.; West, S.G.; Aiken, L.S. Applied Multiple Regression/Correaltion Analysis for Behavioral Sciences, 3rd ed.; Laurence Erlbaum Associates: Mahwah, NJ, USA, 2003. [Google Scholar]
- Schwartz, D.A. The Origins and Emergence of Zika Virus, the Newest TORCH Infection: What’s Old Is New Again. Arch. Pathol. Lab. Med. 2017, 141, 18–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chua, A.; Prat, I.; Nuebling, C.M.; Wood, D.; Moussy, F. Update on Zika Diagnostic Tests and WHO’s Related Activities. PLoS Negl. Trop. Dis. 2017, 11, e0005269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, M.M.; da Cunha, A.J.L.A.; Robaina, J.R.; Raymundo, C.E.; Barbosa, A.P.; Medronho, R.A. Fetal, neonatal, and infant outcomes associated with maternal Zika virus infection during pregnancy: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246643. [Google Scholar] [CrossRef] [PubMed]
- Dutta, S.; Celestine, M.J.; Khanal, S.; Huddleston, A.; Simms, C.; Arca, J.F.; Mitra, A.; Heller, L.; Kraj, P.J.; Ledizet, M.; et al. Coordination of different ligands to copper (II) and cobalt (III) metal centers enhances Zika virus and dengue virus loads in both arthropod cells and human keratinocytes. Biochim. Biophys. Acta Gen. Subj. 2018, 1862, 40–50. [Google Scholar] [CrossRef] [Green Version]
- Alomar, A.A.; Eastmond, B.H.; Alto, B.W. The effects of exposure to pyriproxyfen and predation on Zika virus infection and transmission in Aedes aegypti. PLoS Negl. Trop. Dis. 2020, 14, e0008846. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Jamieson, D.J.; Honein, M.A.; Petersen, L.R. Zika Virus and Birth Defects—Reviewing the Evidence for Causality. N. Engl. J. Med. 2016, 374, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Spirhanzlova, P.; Sébillot, A.; Vancamp, P.; Gothié, J.D.; LeMével, M.L.; Wejaphikul, K.; Meima, M.; Mughal, B.B.; Butruille, L.; Roques, P.; et al. ZIKA virus effects on neuroprogenitors are exacerbated by the main pyriproxyfen metabolite via thyroid hormone signaling disruption. bioRxiv 2020. [Google Scholar] [CrossRef]
- Bancroft, D.; Power, G.M.; Jones, R.T.; Massad, E.; Iriat, J.B.; Preet, R.; Kinsman, J.; Logan, J.G. Vector control strategies in Brazil: A qualitative investigation into community knowledge, attitudes and perceptions following the 2015-2016 Zika virus epidemic. BMJ Open 2022, 12, e050991. [Google Scholar] [CrossRef] [PubMed]
- Dusfour, I.; Vontas, J.; David, J.P.; Weetman, D.; Fonseca, D.M.; Corbel, V.; Raghavendra, K.; Coulibaly, M.B.; Martins, A.J.; Kasai, S.; et al. Management of insecticide resistance in the major Aedes vectors of arboviruses: Advances and challenges. PLoS Negl. Trop. Dis. 2019, 13, e0007615. [Google Scholar] [CrossRef] [PubMed]
- Wen, J.; Shresta, S. Antigenic cross-reactivity between Zika and dengue viruses: Is it time to develop a universal vaccine? Curr. Opin. Immunol. 2019, 59, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Borchering, R.K.; Huang, A.T.; Mier-Y-Teran-Romero, L.; Rojas, D.P.; Rodriguez-Barraquer, I.; Katzelnick, L.C.; Martinez, S.D.; King, G.D.; Cinkovich, S.C.; Lessler, J.; et al. Impacts of Zika emergence in Latin America on endemic dengue transmission. Nat Commun. 2019, 10, 5730. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Scale | Determinant | Summary of Variables in Each Determinant | |
|---|---|---|---|
| Context determinants | 1. Governance (0.434) | Governance was approached as the formalized convergence of diverse social actors of decision making, such as municipal planning agencies, mechanisms for empowering citizens and involvement in high level policy agendas [12]. | |
| 2. Macroeconomic policy (0.361) | Variables describe the balance through economic impositions and fostering, and the resulting economic inequalities in population by Gini and Theil indices [2,12,13,14]. | ||
| 3. Social policy (0.149) | Variables about social support in municipalities through proxies of ZEIS (Zonas Especiais de Interesse Social) for low income housing and interinstitutional social support and development [2,12,13,14]. | ||
| 4. Public policy (0.786) | Variables describe diverse instruments such as plans and legislations that stabilize general public policies on environment, land use, urban settlement, development and housing, economy and transportation. | ||
| 5. Culture and social values (0.872) | Variables about institutional concerns of cultural and educational affairs in municipalities [12]. | ||
| 6. Demographic Epidemiologic conditions (0.598) | Population age pyramid according to the last 2010 census and 2015 population estimate for municipalities. Institutional concern of health and sanitation in municipalities [12,15]. | ||
| Structural determinants | 7. Income (0.755) | Population percent and income distribution between rich, vulnerable, poor and poorest populations, and for workers and unemployed. We also included the mean income by race, and the GDP, per capita GDP and the human development index (HDI) and its income dimension in municipalities [14,16]. | |
| 8. Education (0.878) | Attainment and enrollment in basic school (primary and middle), literacy by race, sex and according to age thresholds, and the expected years of study. We included the dimension of ‘education’ of HDI [14]. | ||
| 9. Occupation (0.876) | Participation in the work force and unemployment, differentiated by race, educational attainment and work sector, and commuting [12,14,16]. | ||
| 10. Social Class (0.976) | Social class was negatively approached by individuals and households located in agglomerates qualified as subnormal, and variables labeling social vulnerability [13]. | ||
| 11. Race-Ethnicity (0.926) | Distribution by Brazil’s racial groups [2,12,13]. | ||
| Intermediary determinants | 12. Social Networks/Socio-env. Psych. Circumstances (0.896) | Civil status, people and children in households supported by people without education of who are vulnerable, and dependency ratio [12,14,16]. | |
| 13. Biological Factors (0.993) | Population distributed by sex, and women population in fertile age groups, fertility rate, infant female and male populations, life expectancy, longevity and ageing rate. Longevity dimension of the HDI [16]. | ||
| 14. Childhood Development (0.948) | Negative approach by Low Birth Weight (LBW) and less than 1-year undernourished children [12,16]. | ||
| 15. Material Circumstances (0.885) | Dwelling material, availability and access to aqueduct/in-house pipe water, sewage system, and waste disposal. Access to electricity. Vegetation distribution and land use. Potential exposure to agro-toxic by agricultural use or residue disposal. Rapid assessment of indices for Aedes aegypti (Levantamiento Rápido de Indices para Aedes aegypti LIRAa) [13,17]. | ||
| 16. Health System (0.974) | Variables of investment (national and local) and performance of Brazil Health System in municipalities, prenatal care and normal delivery, primary and higher levels of care coverage and public health actions. We included as one of the main public health action a very detailed documentation of vaccination about the number of doses (as a proxy of the strength of this intervention) and coverage (width of intervention over beneficiary population) for 2015 and 2016 [15,16]. | ||
| Health outcomes | 17. Vector Borne Diseases (0.677) | Severe dengue, Malaria and Chagas disease cases [15,16]. | |
| 18. Other Health Results (0.965) | Infant and childhood mortality, and incidence rate of congenital syphilis. Different poisoning incidence according to municipality of exposure, notification and residence [18]. Place of exposure hints direct contact with toxic substances, while place of residence and notification correspond to the administrative process. | ||
| 19. Microcephaly Surveillance | Surveillance of microcephaly incidence, including incoming and investigated microcephaly cases, and confirmed/discarded ZVI cases during the first semester of 2016 [19]. | ||
| 20. Stillbirths Surveillance | Surveillance of stillbirth incidence, including incoming and investigated stillbirth cases, and confirmed/discarded ZVI cases [19]. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cifuentes, M.P.; Suarez, C.M.; Cifuentes, R.; Malod-Dognin, N.; Windels, S.; Valderrama, J.F.; Juarez, P.D.; Valdez, R.B.; Colen, C.; Phillips, C.; et al. Big Data to Knowledge Analytics Reveals the Zika Virus Epidemic as Only One of Multiple Factors Contributing to a Year-Over-Year 28-Fold Increase in Microcephaly Incidence. Int. J. Environ. Res. Public Health 2022, 19, 9051. https://doi.org/10.3390/ijerph19159051
Cifuentes MP, Suarez CM, Cifuentes R, Malod-Dognin N, Windels S, Valderrama JF, Juarez PD, Valdez RB, Colen C, Phillips C, et al. Big Data to Knowledge Analytics Reveals the Zika Virus Epidemic as Only One of Multiple Factors Contributing to a Year-Over-Year 28-Fold Increase in Microcephaly Incidence. International Journal of Environmental Research and Public Health. 2022; 19(15):9051. https://doi.org/10.3390/ijerph19159051
Chicago/Turabian StyleCifuentes, Myriam Patricia, Clara Mercedes Suarez, Ricardo Cifuentes, Noel Malod-Dognin, Sam Windels, Jose Fernando Valderrama, Paul D. Juarez, R. Burciaga Valdez, Cynthia Colen, Charles Phillips, and et al. 2022. "Big Data to Knowledge Analytics Reveals the Zika Virus Epidemic as Only One of Multiple Factors Contributing to a Year-Over-Year 28-Fold Increase in Microcephaly Incidence" International Journal of Environmental Research and Public Health 19, no. 15: 9051. https://doi.org/10.3390/ijerph19159051
APA StyleCifuentes, M. P., Suarez, C. M., Cifuentes, R., Malod-Dognin, N., Windels, S., Valderrama, J. F., Juarez, P. D., Valdez, R. B., Colen, C., Phillips, C., Ramesh, A., Im, W., Lichtveld, M., Mouton, C., Pržulj, N., & Hood, D. B. (2022). Big Data to Knowledge Analytics Reveals the Zika Virus Epidemic as Only One of Multiple Factors Contributing to a Year-Over-Year 28-Fold Increase in Microcephaly Incidence. International Journal of Environmental Research and Public Health, 19(15), 9051. https://doi.org/10.3390/ijerph19159051








