Uptake, Engagement and Acceptance, Barriers and Facilitators of a Text Messaging Intervention for Postnatal Care of Mother and Child in India—A Mixed Methods Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Text Messaging Service
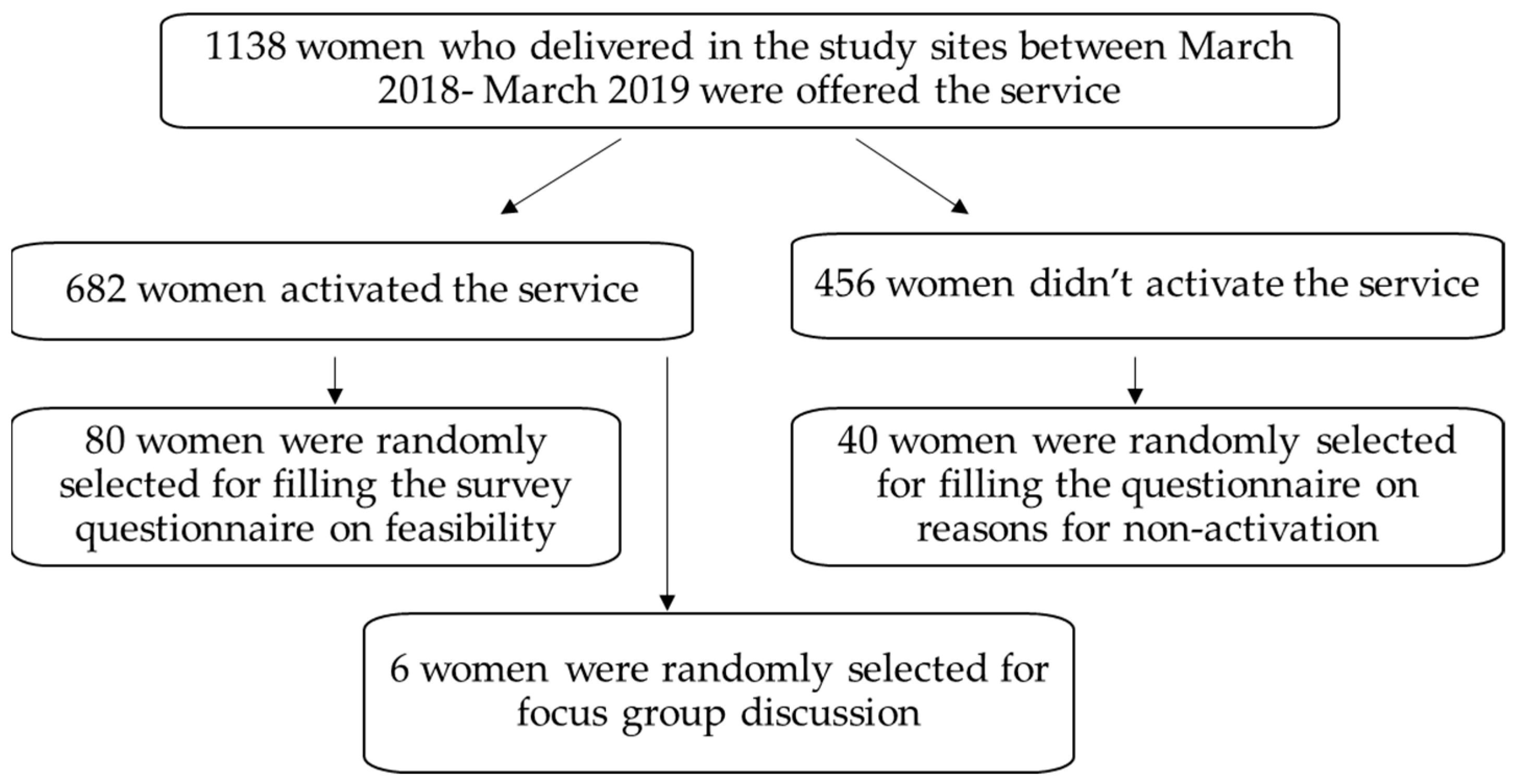
2.3. Participants
2.4. Data Collection
2.4.1. Telephonic Survey
2.4.2. Focus Group Discussions
2.5. Statistical Analysis
3. Results
3.1. Telephonic Survey
3.2. Reasons for Engaging in the Service
3.3. Themes Identified from the Focus Group Discussion
- Reliable, current, up-to-date information: Respondents believed the messages were crafted by the providers at the hospital and their knowledge and expertise lent credibility to the service.
- Topical issues and themes that are well aligned with new mothers’ needs and priorities: The messages covered a wide range of topics from breastfeeding to sleeping to even self-care for the new mother. The alignment of the topics to the development stage of the newborn was particularly valued by new mothers. Coverage of socially taboo topics, such as when sexual intercourse could begin or contraception, were seen particularly valuable as these topics could not be discussed with anyone other than your provider.
- Expanded the repertoire of information sources available to the new mother: New mothers have access to a wide range of information sources including the internet, social media, a variety of apps, books and magazines. Although this was valued, it was often challenging to ascertain the credibility of the information and to separate fact from fiction. The text messages by contrast had the seal of approval from ‘their’ provider and were tailored to meet their unique needs.
- High quality information in an accessible format: The messages were clear, and easy to read and understand. They were written in simple, plain English and were of an appropriate length. Receiving the information in a text format was particularly appreciated as mothers could read it repeatedly and save it for future use.
3.4. Value and Benefits of the Service
- Increased new mothers’ awareness and understanding about postnatal healthcare practices: The messages provide an explanation for the issues experienced by new mothers; thus, they can be used to normalize the issues and provide clear actions to address the issues being faced. This helps to grow the mothers’ confidence in caring for her newborn which in turn improves the physical and emotional well-being of both the mother and the child.
- New mothers’ felt increased connectedness and emotional support as a direct result of the service: Many of the women interviewed talked about the helplessness, anxiety and an emotional low they experienced immediately following the birth of the child. Being home on their own with their newborn was a stressful time for many and there was a lack of connectedness with their usual social groups. The text messages helped overcome some of this loneliness and anxiety—it was a crutch and a link to the hospital, and this provided tremendous reassurance.
“Post-delivery it is quite common to feel a bit low. When I went home and I received the first message, I felt happy. My heart lifted and I felt like I was being looked after even after leaving the hospital. I cannot express how I felt at the time.”(Mother, aged 28)
“The vaccination reminders are so useful. I feel like someone cares about me and my child. I am not alone in this.”(Mother, aged 30)
- Prevented continuation of harmful and dated practices: All those interviewed talked about the ongoing stream of advice from well-wishers relating to the dos and don’ts associated with being a new mother. These included advice on appropriate diet (e.g., mangoes, ice cream, tender coconut water, spices, meat, egg); physical movement (e.g., no running or exercise); and outdated parenting tips (e.g., treating colic, feeding schedules, dealing with crying, sleeping). New mothers realized that these tips and practices were outdated and not supported by their providers. The text messages helped new mothers counter the pressure they felt from elder family members and break the cycle of continuing dated practices.
“There are so many people who are quick to give advice. They may have had their child 50 years ago, but they still try to influence you, particularly when it comes to food. My mother-in-law for example tells me not to eat meat or eggs or even lentils. But in the hospital, the day after delivery they served me sambhar (lentil stew) and rice.”(Mother, aged 32)
“I follow the advice given by the provider and the text message, which is also from the provider. They know best, they have seen us through the entire pregnancy, and they have seen so many pregnancies. Their knowledge is current. I trust them. I won’t follow the advice given by my mother or mother-in-law as it is not current. There is no scientific basis for what they say or ask you to do. They just scare you.”(Mother, aged 28)
- Improved quality of relationship between health practitioners and service users: The text messaging service made the users more alert to the current issues (common postnatal issues related to breastfeeding, sleep newborn care and common postpartum complaints related to bleeding and breast engorgement, etc.) faced by new mothers and built their confidence to deal with them. As a result, the mothers felt they did not need to ring the pediatrician for every little problem or concern, and they could wait and raise questions during the periodic visits. The proactive identification of issues and heightened vigilance led to improved self-efficacy.
- Positioning the healthcare facility as one that cares: Those interviewed were aware that the hospital was the only one providing this kind of text messaging service. Although this was not the reason for choosing this healthcare facility for their delivery, it certainly reinforced their view that this was the hospital which cared for its patients. The text messaging service extended their contact with the hospital and reassured them that the hospital cared for them even after they were no longer in the care of the hospital.
“After you go home, you really feel alone. You are trained and equipped for delivery but after that you are left in the dark. But the texts are a gentle reminder that you are not alone. The hospital still cares for you, and I really feel good about that.”(Mother, aged 30)
3.5. Reflections on Process Measures
- Timing: Information and invitation to sign up to the service was often provided at the time of discharge. This was a stressful period and new mothers reported feeling overwhelmed and distracted. They have limited ability to take in new information. There may be an opportunity to introduce the concept of the text messaging service when they come for their appointments leading up to the delivery, so that the pregnant woman is less pressured and is more likely to engage in such discussions.
“At the hospital there are so many papers I had to sign. I don’t remember what I signed. I may have signed over all my assets away for all I know! This is not the right time for giving information about this useful service as I am not likely to remember anything.”(Mother, aged 27)
- 2.
- Repetitive: Some new mothers noticed that they frequently received the same message twice. This caused some frustration and needs to be addressed.
- 3.
- Clarity: For a few instances, the messages were contradictory to the information provided at the hospital. The demand feed versus scheduled feed was identified as one such example, where the hospital at the time of discharge advised that mothers should feed on a schedule; however, the text message suggested demand feed. This was confusing.
- 4.
- Alignment: Aligning the message to where the new mother is at in her first 100 days needs to be considered. The messages began from the date the service was activated. The service considered the day of activation as day 1. However, the activation may occur one week after the delivery which means the messages were not synchronizing with the development cycle of the newborn. There has to be a way of ensuring the messages are aligned to the delivery date and to make sure that the messages are synchronized with the baby’s evolution.
- 5.
- Miscellaneous: In some instances, when signing up for the service, the husband provided his phone number to activate the service. As a result, the messages went to him, and the mother missed out on direct access to the message.
3.6. Barriers for Non-Engagement
4. Discussion
4.1. Implications for Future Research
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. WHO Recommendations on Maternal and Newborn Care for a Positive Postnatal Experience. Available online: https://www.who.int/publications/i/item/9789240045989 (accessed on 29 March 2022).
- Bick, D.; Ram, U.; Saravanan, P.; Temmerman, M. New global WHO postnatal guidance is welcome but misses the long-term perspective. Lancet 2022, 399, 1578–1580. [Google Scholar] [CrossRef]
- ACOG. ACOG Committee Opinion No. 736: Optimizing Postpartum Care. Obstet Gynecol. 2018, 131, e140–e150. [Google Scholar] [CrossRef] [PubMed]
- Sacks, E.; Langlois, E.V. Postnatal care: Increasing coverage, equity, and quality. Lancet Glob. Health. 2016, 4, e442–e443. [Google Scholar] [CrossRef]
- Victora, C.G.; Requejo, J.H.; Barros, A.J.; Berman, P.; Bhutta, Z.; Boerma, T.; Chopra, M.; de Francisco, A.; Daelmans, B.; Hazel, E.; et al. Countdown to 2015: A decade of tracking progress for maternal, newborn, and child survival. Lancet 2016, 387, 2049–2059. [Google Scholar] [CrossRef]
- Langlois, É.V.; Miszkurka, M.; Zunzunegui, M.V.; Ghaffar, A.; Ziegler, D.; Karp, I. Inequities in postnatal care in low- and middle-income countries: A systematic review and meta-analysis. Bull. World Health Organ. 2015, 93, 259–270G. [Google Scholar] [CrossRef]
- Lee, H.-Y.; Leslie, H.H.; Oh, J.; Kim, R.; Kumar, A.; Subramanian, S.V.; Kruk, M.E. The association between institutional delivery and neonatal mortality based on the quality of maternal and newborn health system in India. Sci. Rep. 2022, 12, 6220. [Google Scholar] [CrossRef]
- Fadel, S.A.; Ram, U.; Morris, S.K.; Begum, R.; Shet, A.; Jotkar, R.; Jha, P. Facility Delivery, Postnatal Care and Neonatal Deaths in India: Nationally-Representative Case-Control Studies. PLoS ONE. 2015, 10, e0140448. [Google Scholar] [CrossRef]
- Kishun, J. Association of postnatal care with neonatal mortality in India: Evidences from DLHS-4 data. Int. J. Community Med. Public Health 2019, 6, 7. [Google Scholar] [CrossRef]
- Upadhyay, R.P.; Chowdhury, R.; Aslyeh, S.; Sarkar, K.; Singh, S.K.; Sinha, B.; Pawar, A.; Rajalakshmi, A.K.; Kumar, A. Postpartum depression in India: A systematic review and meta-analysis. Bull. World Health Organ. 2017, 95, 706–717C. [Google Scholar] [CrossRef]
- Moola, S.; Tyagi, J.; Shah, P.; Nambiar, D.; Bhaumik, S. Harmful Postpartum Beliefs and Practices of Mothers in India: Rapid Evidence Synthesis; The George Institute for Global Health: Vishakhapatnam, India, 2020. [Google Scholar]
- Choudhary, R.; Gothwal, S.; Nayan, S.; Meena, B.S. Common ritualistic myths during pregnancy in Northern India. Int. J. Contemp. Pediatr. 2017, 4, 4. [Google Scholar] [CrossRef][Green Version]
- Schmied, V.; Cooke, M.; Gutwein, R.; Steinlein, E.; Homer, C. An evaluation of strategies to improve the quality and content of hospital-based postnatal care in a metropolitan Australian hospital. J. Clin. Nurs. 2009, 18, 1850–1861. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, I.H.; Simonsen, M.; Trillingsgaard, T.; Pontoppidan, M.; Kronborg, H. First-time mothers’ confidence mood and stress in the first months postpartum. A cohort study. Sex. Reprod. Healthc. 2018, 17, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Cole-Lewis, H.; Kershaw, T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol. Rev. 2010, 32, 56–69. [Google Scholar] [CrossRef]
- Ødegård, E.S.; Langbråten, L.S.; Lundh, A.; Linde, D.S. Two-way text message interventions and healthcare outcomes in Africa: Systematic review of randomized trials with meta-analyses on appointment attendance and medicine adherence. PLoS ONE 2022, 17, e0266717. [Google Scholar] [CrossRef]
- Basu, S.; Rajeev, A.; Garg, S.; Singh, M.M. Effect of a Text-Messaging Intervention on Oral Self-Care Practices in Antenatal Women in Delhi, India: A Pilot Randomized Control Trial. Indian J. Community Med. 2022, 47, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Singleton, A.C.; Raeside, R.; Partridge, S.R.; Hyun, K.K.; Tat-Ko, J.; Sum, S.C.M.; Hayes, M.; Chow, C.K.; Thiagalingam, A.; Maka, K.; et al. Supporting women’s health outcomes after breast cancer treatment comparing a text message intervention to usual care: The EMPOWER-SMS randomised clinical trial. J. Cancer Surviv. 2022. [Google Scholar] [CrossRef] [PubMed]
- Vodopivec-Jamsek, V.; de Jongh, T.; Gurol-Urganci, I.; Atun, R.; Car, J. Mobile phone messaging for preventive health care. Cochrane Database Syst. Rev. 2012, 12, CD007457. [Google Scholar] [CrossRef]
- Yadav, P.; Kant, R.; Kishore, S.; Barnwal, S.; Khapre, M. The Impact of Mobile Health Interventions on Antenatal and Postnatal Care Utilization in Low- and Middle-Income Countries: A Meta-Analysis. Cureus 2022, 14, e21256. [Google Scholar] [CrossRef]
- Remick, A.P.; Kendrick, J.S. Breaking new ground: The text4baby program. Am. J. Health Promot. 2013, 27 (Suppl. 3), S4–S6. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122. [Google Scholar] [CrossRef]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef] [PubMed]
- Christakis, N.A. Social networks and collateral health effects. BMJ 2004, 329, 184–185. [Google Scholar] [CrossRef] [PubMed]
- Cobb, S. Presidential Address-1976. Social support as a moderator of life stress. Psychosom. Med. 1976, 38, 300–314. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310. [Google Scholar] [CrossRef] [PubMed]
- Chioma Ebuenyi, M.; Schnoor, K.; Versluis, A.; Meijer, E.; Chavannes, N.H. Short message services interventions for chronic disease management: A systematic review. Clin. eHealth 2021, 4, 24–29. [Google Scholar] [CrossRef]
- Dennis, C.L.; Hodnett, E.; Kenton, L.; Weston, J.; Zupancic, J.; Stewart, D.E.; Kiss, A. Effect of peer support on prevention of postnatal depression among high risk women: Multisite randomised controlled trial. BMJ 2009, 338, a3064. [Google Scholar] [CrossRef]
- Cooke, M.; Stacey, T. Differences in the evaluation of postnatal midwifery support by multiparous and primiparous women in the first two weeks after birth. Aust. Midwifery 2003, 16, 18–24. [Google Scholar] [CrossRef]
- Mushamiri, I.; Luo, C.; Iiams-Hauser, C.; Ben Amor, Y. Evaluation of the impact of a mobile health system on adherence to antenatal and postnatal care and prevention of mother-to-child transmission of HIV programs in Kenya. BMC Public Health 2015, 15, 102. [Google Scholar] [CrossRef]
- Lavender, T.; Richens, Y.; Milan, S.J.; Smyth, R.M.; Dowswell, T. Telephone support for women during pregnancy and the first six weeks postpartum. Cochrane Database Syst. Rev. 2013, 2013, CD009338. [Google Scholar] [CrossRef]
- Watson, A.R.; Wah, R.; Thamman, R. The Value of Remote Monitoring for the COVID-19 Pandemic. Telemed. e-Health 2020, 26, 1110–1112. [Google Scholar] [CrossRef]
- Dol, J.A.-O.; Aston, M.; Grant, A.; McMillan, D.; Tomblin Murphy, G.; Campbell-Yeo, M. Effectiveness of the “Essential Coaching for Every Mother” postpartum text message program on maternal psychosocial outcomes: A randomized controlled trial. Digit. Health 2022, 8, 20552076221107886. [Google Scholar] [CrossRef] [PubMed]
- El Ayadi, A.A.-O.; Duggal, M.A.-O.; Bagga, R.A.-O.; Singh, P.A.-O.; Kumar, V.A.-O.; Ahuja, A.A.-O.; Kankaria, A.A.-O.; Hosapatna Basavarajappa, D.A.-O.; Kaur, J.A.-O.; Sharma, P.A.-O.; et al. A Mobile Education and Social Support Group Intervention for Improving Postpartum Health in Northern India: Development and Usability Study. MIR Form. Res. 2021, 6, e34087. [Google Scholar] [CrossRef] [PubMed]
- Kant, R.; Yadav, P.; Kishore, S.; Barnwal, S.; Kumar, R.; Khapre, M. Impact of mHealth interventions on antenatal and postnatal care utilization in low and middle-income countries: A Systematic Review and Meta-Analysis. medRxiv 2020. [Google Scholar] [CrossRef]
- Datta, L.-E. The wheelbarrow, the mosaic and the double helix:Challenges and strategies for successfully carrying out mixed methods evaluation. Eval. J. Australas. 2001, 1, 33–40. [Google Scholar] [CrossRef]
- Slomian, J.; Emonts, P.; Vigneron, L.; Acconcia, A.; Glowacz, F.; Reginster, J.Y.; Oumourgh, M.; Bruyère, O. Identifying maternal needs following childbirth: A qualitative study among mothers, fathers and professionals. BMC Pregnancy Childbirth 2017, 17, 213. [Google Scholar] [CrossRef]
- Slomian, J.; Reginster, J.-Y.; Emonts, P.; Bruyère, O. Identifying maternal needs following childbirth: Comparison between pregnant women and recent mothers. BMC Pregnancy Childbirth 2021, 21, 405. [Google Scholar] [CrossRef]
- The Economist. The Second Half of Humanity Is Joining the Internet. 2019. Available online: https://www.economist.com/leaders/2019/06/08/the-second-half-of-humanity-is-joining-the-internet (accessed on 29 March 2022).
- Perry, C.; Chhatralia, K.; Damesick, D.; Hobden, S.; Volpe, L. Behavioural Insights in Health Care; The Health Foundation: London, UK, 2015. [Google Scholar]
- Loewenstein, G.; Hagmann, D.; Schwartz, J.; Ericson, K.; Kessler, J.B.; Bhargava, S.; Blumenthal-Barby, J.; D’Aunno, T.; Handel, B.; Kolstad, J.; et al. A behavioral blueprint for improving health care policy. Behav. Sci. Policy 2017, 3, 52–66. [Google Scholar] [CrossRef]
- Zinsser, L.A.; Stoll, K.; Wieber, F.; Pehlke-Milde, J.; Gross, M.M. Changing behaviour in pregnant women: A scoping review. Midwifery 2020, 85, 102680. [Google Scholar] [CrossRef]
| Total (n = 1138) | Users (n= 682) | Non-Users (n= 456) | |
|---|---|---|---|
| Age n (%) | |||
| 24 and less | 159 (14.0) | 87(12.8) | 72 (15.8) |
| 25 to 35 | 924 (81.2) | 565(82.8) | 359 (78.7) |
| 36 and above | 55(4.8) | 30(4.4) | 25 (5.5) |
| Parity n (%) | |||
| 1 | 635 (55.8) | 389(57.0) | 246(53.9) |
| 2 | 395 (34.7) | 236(34.6) | 159(34.9) |
| 3 | 79 (6.9) | 40(5.9) | 39(8.5) |
| 4 | 21 (1.9) | 13(1.9) | 8(1.8) |
| 5–7 | 8 (0.7) | 4(0.6) | 4(0.9) |
| Complication n (%) | |||
| GDM | 279 (24.5) | 175(25.7) | 104(22.8) |
| Hypothyroid | 136 (11.95) | 88(12.9) | 48(10.5) |
| Others (Multiple) | 108 (9.5) | 56(8.2) | 52(11.4) |
| None | 615 (54.05) | 363(53.2) | 252(55.3) |
| Delivery type n (%) | |||
| LSCS | 469 (41.2) | 261(38.3) | 208(45.6) |
| Normal Delivery * | 669 (58.8) | 421(61.7) | 248(54.4) |
| Why Did You Activate and Take Up This Service? | ||
|---|---|---|
| It was a service offered by the hospital. | 53.16% | 42 |
| It would help me understand what is going on with me and my child. | 73.75% | 59 |
| I expected the information to be reliable. | 29.49% | 23 |
| Such a service would help clarify any doubts I had after I went home. | 42.31% | 33 |
| Having such information would help build my confidence in caring for my newborn. | 35.00% | 28 |
| The information comes to me directly from the hospital. | 25.00% | 20 |
| I would know first-hand what to do and take appropriate action. | 21.05% | 16 |
| Any other please specify. | 15.79% | 3 |
| Which of the Following Statements Best Describe Your Experience of the Service? | ||
|---|---|---|
| The texts helped me to understand my situation and what I was going through. | 94.94% | 75 |
| It helped me to seek the right type of help at the right time. | 82.28% | 65 |
| I was able to handle many issues myself. | 68.35% | 54 |
| I felt the hospital continued to care for me even after I was discharged. | 89.87% | 71 |
| It helped me to clarify conflicting information on topics like diet/activity/breastfeeding. | 88.61% | 70 |
| It was information I could store and go back and read. | 68.35% | 54 |
| It reminded me about vaccination and review visits. | 78.21% | 61 |
| It addressed issues such as activity and contraception that I could then discuss with my provider. | 50.00% | 37 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sampathkumar, S.; Sankar, M.; Ramasamy, S.; Sriram, N.; Saravanan, P.; Ram, U. Uptake, Engagement and Acceptance, Barriers and Facilitators of a Text Messaging Intervention for Postnatal Care of Mother and Child in India—A Mixed Methods Feasibility Study. Int. J. Environ. Res. Public Health 2022, 19, 8914. https://doi.org/10.3390/ijerph19158914
Sampathkumar S, Sankar M, Ramasamy S, Sriram N, Saravanan P, Ram U. Uptake, Engagement and Acceptance, Barriers and Facilitators of a Text Messaging Intervention for Postnatal Care of Mother and Child in India—A Mixed Methods Feasibility Study. International Journal of Environmental Research and Public Health. 2022; 19(15):8914. https://doi.org/10.3390/ijerph19158914
Chicago/Turabian StyleSampathkumar, Swetha, Meenakshi Sankar, Sankar Ramasamy, Nivedita Sriram, Ponnusamy Saravanan, and Uma Ram. 2022. "Uptake, Engagement and Acceptance, Barriers and Facilitators of a Text Messaging Intervention for Postnatal Care of Mother and Child in India—A Mixed Methods Feasibility Study" International Journal of Environmental Research and Public Health 19, no. 15: 8914. https://doi.org/10.3390/ijerph19158914
APA StyleSampathkumar, S., Sankar, M., Ramasamy, S., Sriram, N., Saravanan, P., & Ram, U. (2022). Uptake, Engagement and Acceptance, Barriers and Facilitators of a Text Messaging Intervention for Postnatal Care of Mother and Child in India—A Mixed Methods Feasibility Study. International Journal of Environmental Research and Public Health, 19(15), 8914. https://doi.org/10.3390/ijerph19158914







