Health-Related Quality of Life of Moroccan COVID-19 Survivors: A Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
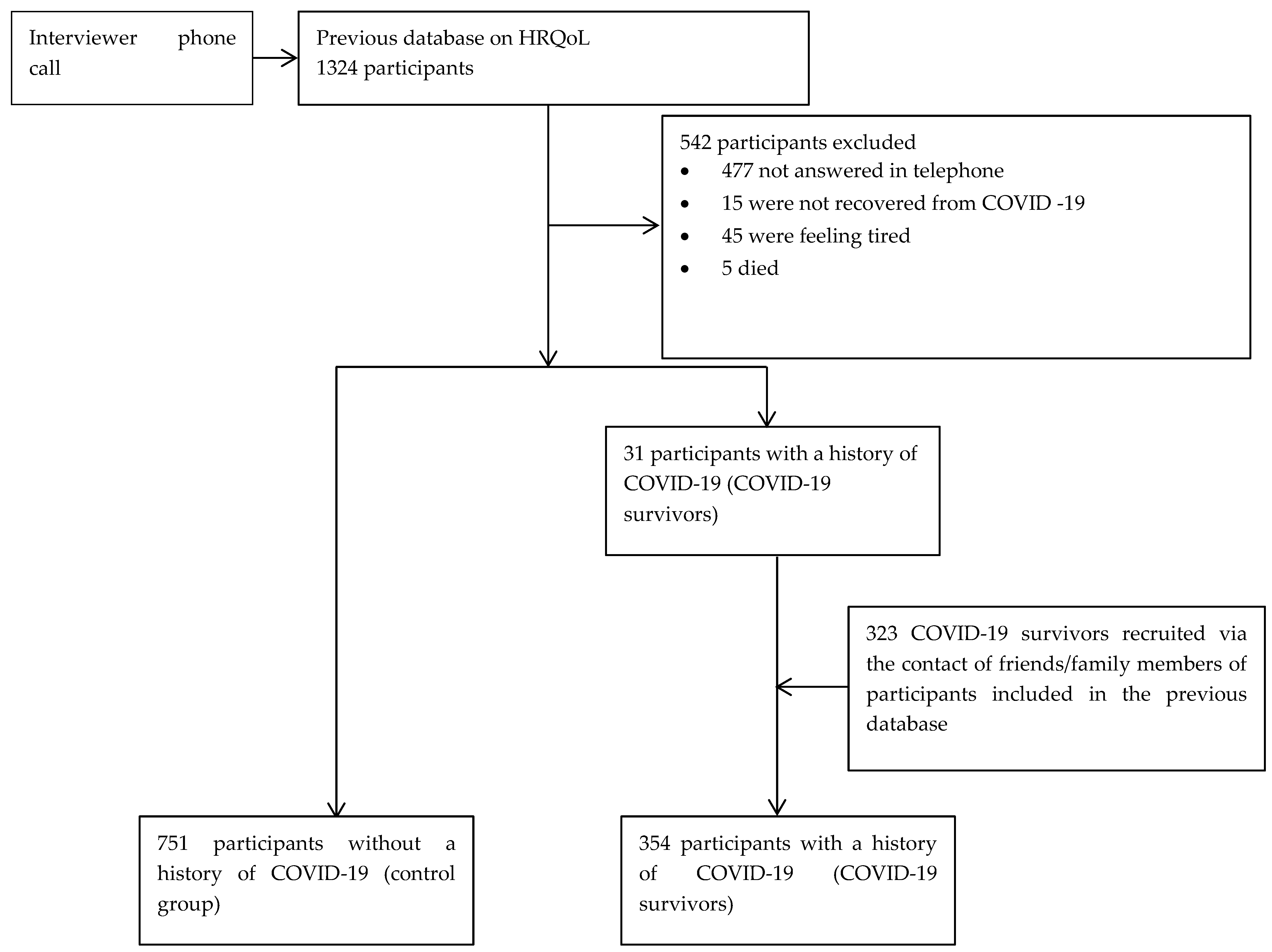
2.1. Study Design and Data Collection
2.2. Measurements
2.3. Sampling
2.4. Statistical Analysis
3. Results
3.1. Association between COVID-19 and Socio-Demographic and Clinical Characteristics
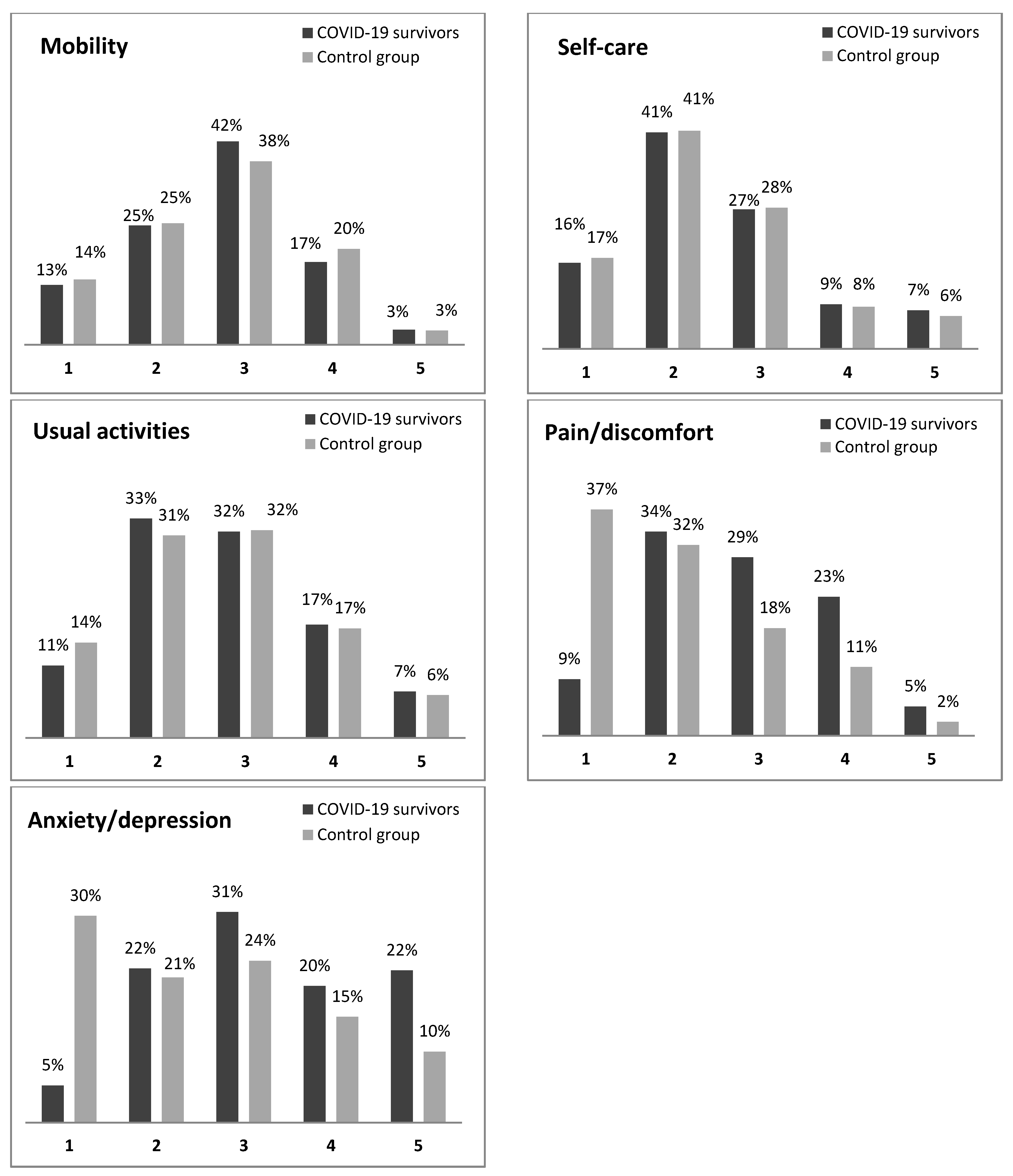
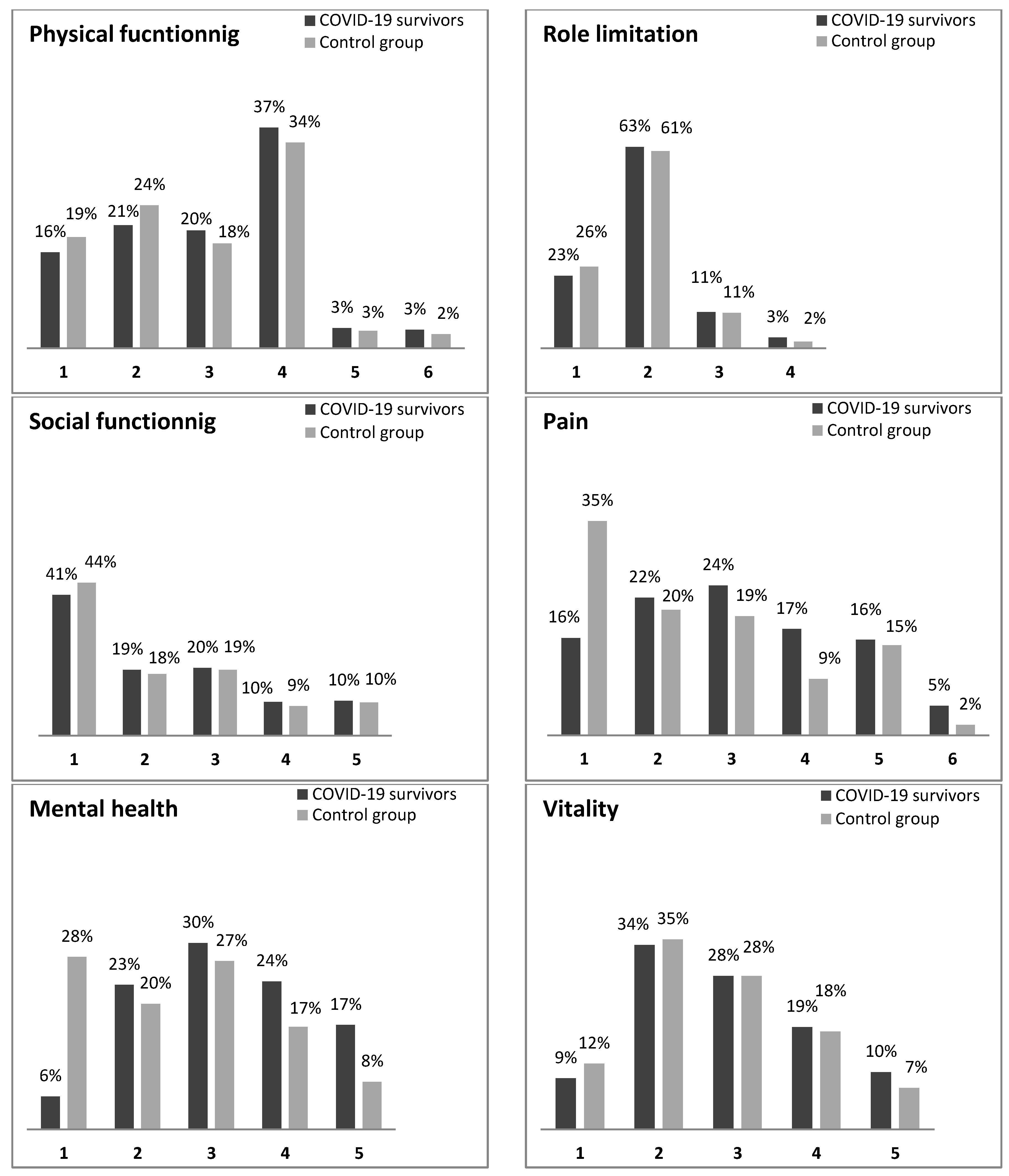
3.2. Health-Related Quality of Life of the COVID-19 Survivors versus Control Group
3.3. Comparison of EQ-5D-5L and SF-6D Dimensions between COVID-19 Survivors and the Control Group Stratified on Socio-Demographic and Clinical Variables
3.4. The COVID-19 Survivors’ HRQoL
3.5. Correlation between the SF-6D Domains and the EQ-5D-5L Dimensions of the COVID-19 Survivors and Non-COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lai, C.-C.; Shih, T.-P.; Ko, W.-C.; Tang, H.-J.; Hsueh, P.-R. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease-2019 (COVID-19): The Epidemic and the Challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19) Situation Reports. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 13 December 2021).
- Chang, T.-H.; Wu, J.-L.; Chang, L.-Y. Clinical Characteristics and Diagnostic Challenges of Pediatric COVID-19: A Systematic Review and Meta-Analysis. J. Formos. Med. Assoc. 2020, 119, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Jiang, F.; Deng, L.; Zhang, L.; Cai, Y.; Cheung, C.W.; Xia, Z. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19). J. Gen. Intern. Med. 2020, 35, 1545–1549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Yasuhara, J.; Kuno, T.; Takagi, H.; Sumitomo, N. Clinical Characteristics of COVID-19 in Children: A Systematic Review. Pediatric Pulmonol. 2020, 55, 2565–2575. [Google Scholar] [CrossRef]
- Meo, S.A.; Klonoff, D.C.; Akram, J. Efficacy of Chloroquine and Hydroxychloroquine in the Treatment of COVID-19. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4539–4547. [Google Scholar] [CrossRef]
- Becker, R.C. COVID-19 Treatment Update: Follow the Scientific Evidence. J. Thromb. Thrombolysis 2020, 50, 43–53. [Google Scholar] [CrossRef] [Green Version]
- Young, B.; Tan, T.T.; Leo, Y.S. The Place for Remdesivir in COVID-19 Treatment. Lancet Infect. Dis. 2021, 21, 20–21. [Google Scholar] [CrossRef]
- Tsang, H.F.; Chan, L.W.C.; Cho, W.C.S.; Yu, A.C.S.; Yim, A.K.Y.; Chan, A.K.C.; Ng, L.P.W.; Wong, Y.K.E.; Pei, X.M.; Li, M.J.W.; et al. An Update on COVID-19 Pandemic: The Epidemiology, Pathogenesis, Prevention and Treatment Strategies. Expert Rev. Anti Infect. Ther. 2021, 19, 877–888. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The Socio-Economic Implications of the Coronavirus Pandemic (COVID-19): A Review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Hawkins, R.B.; Charles, E.J.; Mehaffey, J.H. Socio-Economic Status and COVID-19-Related Cases and Fatalities. Public Health 2020, 189, 129–134. [Google Scholar] [CrossRef]
- Martin, A.; Markhvida, M.; Hallegatte, S.; Walsh, B. Socio-Economic Impacts of COVID-19 on Household Consumption and Poverty. Econ. Disasters Clim. Chang. 2020, 4, 453–479. [Google Scholar] [CrossRef]
- Azizi, A.; Achak, D.; Aboudi, K.; Saad, E.; Nejjari, C.; Nouira, Y.; Hilali, A.; Youlyouz-Marfak, I.; Marfak, A. Health-Related Quality of Life and Behavior-Related Lifestyle Changes Due to the COVID-19 Home Confinement: Dataset from a Moroccan Sample. Data Brief 2020, 32, 106239. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The Outbreak of COVID-19 Coronavirus and Its Impact on Global Mental Health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [Green Version]
- Nearchou, F.; Flinn, C.; Niland, R.; Subramaniam, S.S.; Hennessy, E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8479. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent Psychiatric Disorders during the COVID-19 Pandemic and Lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Cinelli, G.; Bigioni, G.; Soldati, L.; Attinà, A.; Bianco, F.F.; Caparello, G.; Camodeca, V.; Carrano, E.; et al. Psychological Aspects and Eating Habits during COVID-19 Home Confinement: Results of EHLC-COVID-19 Italian Online Survey. Nutrients 2020, 12, 2152. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-Month Consequences of COVID-19 in Patients Discharged from Hospital: A Cohort Study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Jacobs, L.G.; Gourna Paleoudis, E.; Lesky-Di Bari, D.; Nyirenda, T.; Friedman, T.; Gupta, A.; Rasouli, L.; Zetkulic, M.; Balani, B.; Ogedegbe, C.; et al. Persistence of Symptoms and Quality of Life at 35 Days after Hospitalization for COVID-19 Infection. PLoS ONE 2020, 15, e0243882. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F. Gemelli against COVID-19 Post-Acute Care Study Group Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Pietrobon, A.J.; Teixeira, F.M.E.; Sato, M.N. I Mmunosenescence and Inflammaging: Risk Factors of Severe COVID-19 in Older People. Front. Immunol. 2020, 11, 579220. [Google Scholar] [CrossRef] [PubMed]
- Bajgain, K.T.; Badal, S.; Bajgain, B.B.; Santana, M.J. Prevalence of Comorbidities among Individuals with COVID-19: A Rapid Review of Current Literature. Am. J. Infect. Control 2021, 49, 238–246. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- Brazier, J.E.; Mulhern, B.J.; Bjorner, J.B.; Gandek, B.; Rowen, D.; Alonso, J.; Vilagut, G.; Ware, J.E.; SF-6Dv2 International Project Group. Developing a New Version of the SF-6D Health State Classification System from the SF-36v2: SF-6Dv2. Med. Care 2020, 58, 557–565. [Google Scholar] [CrossRef]
- Dawoud, D.M.; El-Dahiyat, F.; Abojedi, A.; Dawoud, N.; Soliman, A.M.; Hussein, M.; Mohamed, O.; Hasan, S.S.; Babar, Z.U.; Kharroubi, S.A. Translation, cultural adaptation and psychometric validation of the SF-6D measure of health-related quality of life for use in Arabic-Speaking countries. Res. Soc. Adm. Pharm. 2020, 16, 1754–1759. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Qian, S.Z.; Hong, W.D.; Pan, J.Y. Clinical Characteristics and Outcomes of Severe and Critical Patients with 2019 Novel Coronavirus Disease (COVID-19) in Wenzhou: A Retrospective Study. Front. Med. 2020, 7, 552002. [Google Scholar] [CrossRef]
- Thai, P.Q.; Toan, D.T.T.; Son, D.T.; Van, H.T.H.; Minh, L.N.; Hung, L.X.; Toan, N.V.; Hoat, L.N.; Luong, D.H.; Khue, L.N.; et al. Factors Associated with the Duration of Hospitalisation among COVID-19 Patients in Vietnam: A Survival Analysis. Epidemiol. Infect. 2020, 148, e114. [Google Scholar] [CrossRef]
- Chadeau-Hyam, M.; Bodinier, B.; Elliott, J.; Whitaker, M.D.; Tzoulaki, I.; Vermeulen, R.; Kelly-Irving, M.; Delpierre, C.; Elliott, P. Risk Factors for Positive and Negative COVID-19 Tests: A Cautious and In-Depth Analysis of UK Biobank Data. Int. J. Epidemiol. 2020, 49, 1454–1467. [Google Scholar] [CrossRef]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and Comorbidities: Deleterious Impact on Infected Patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Booth, C.M.; Matukas, L.M.; Tomlinson, G.A.; Rachlis, A.R.; Rose, D.B.; Dwosh, H.A.; Walmsley, S.L.; Mazzulli, T.; Avendano, M.; Derkach, P.; et al. Clinical Features and Short-Term Outcomes of 144 Patients with SARS in the Greater Toronto Area. JAMA 2003, 289, 2801–2809. [Google Scholar] [CrossRef] [Green Version]
- Erener, S. Diabetes, infection risk and COVID-19. Mol. Metab. 2020, 39, 101044. [Google Scholar] [CrossRef]
- Luk, A.O.Y.; Ng, S.S.S.; Holt, R.I.G. Impact of Diabetes on COVID-19 and Other Infection: Report from the 22nd Hong Kong Diabetes and Cardiovascular Risk Factors-East Meets West Symposium. Diabet. Med. 2021, 38, e14547. [Google Scholar] [CrossRef]
- Fu, L.; Liu, X.; Su, Y.; Ma, J.; Hong, K. Prevalence and Impact of Cardiac Injury on COVID-19: A Systematic Review and Meta-Analysis. Clin. Cardiol. 2021, 44, 276–283. [Google Scholar] [CrossRef]
- Aggarwal, S.; Garcia-Telles, N.; Aggarwal, G.; Lavie, C.; Lippi, G.; Henry, B.M. Clinical Features, Laboratory Characteristics, and Outcomes of Patients Hospitalized with Coronavirus Disease 2019 (COVID-19): Early Report from the United States. Diagnosis 2020, 7, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Arab-Zozani, M.; Hashemi, F.; Safari, H.; Yousefi, M.; Ameri, H. Health-Related Quality of Life and Its Associated Factors in COVID-19 Patients. Osong Public Health Res. Perspect. 2020, 11, 296–302. [Google Scholar] [CrossRef]
- Kiekens, C.; Boldrini, P.; Andreoli, A.; Avesani, R.; Gamna, F.; Grandi, M.; Lombardi, F.; Lusuardi, M.; Molteni, F.; Perboni, A.; et al. Rehabilitation and Respiratory Management in the Acute and Early Post-Acute Phase. “Instant Paper from the Field” on Rehabilitation Answers to the COVID-19 Emergency. Eur. J. Phys. Rehabil. Med. 2020, 56, 323–326. [Google Scholar] [CrossRef]
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934–943. [Google Scholar] [CrossRef] [Green Version]
- Richards, F.; Kodjamanova, P.; Chen, X.; Li, N.; Atanasov, P.; Bennetts, L.; Patterson, B.J.; Yektashenas, B.; Mesa-Frias, M.; Tronczynski, K.; et al. Economic Burden of COVID-19: A Systematic Review. Clin. Outcomes Res. 2022, 14, 293–307. [Google Scholar] [CrossRef]
- Di Fusco, M.; Shea, K.M.; Lin, J.; Nguyen, J.L.; Angulo, F.J.; Benigno, M.; Malhotra, D.; Emir, B.; Sung, A.H.; Hammond, J.L.; et al. Health Outcomes and Economic Burden of Hospitalized COVID-19 Patients in the United States. J. Med. Econ. 2021, 24, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Kohli, M.; Maschio, M.; Becker, D.; Weinstein, M.C. The Potential Public Health and Economic Value of a Hypothetical COVID-19 Vaccine in the United States: Use of Cost-Effectiveness Modeling to Inform Vaccination Prioritization. Vaccine 2021, 39, 1157–1164. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.; Ali, F.M.; Nixon, S.J.; Ingram, J.R.; Salek, S.M.; Finlay, A.Y. Measuring the Impact of COVID-19 on the Quality of Life of the Survivors, Partners and Family Members: A Cross-Sectional International Online Survey. BMJ Open 2021, 11, e047680. [Google Scholar] [CrossRef]
- Mazza, M.G.; Palladini, M.; De Lorenzo, R.; Bravi, B.; Poletti, S.; Furlan, R.; Ciceri, F.; COVID-19 BioB Outpatient Clinic Study Group; Rovere-Querini, P.; Benedetti, F. One-Year Mental Health Outcomes in a Cohort of COVID-19 Survivors. J. Psychiatr. Res. 2021, 145, 118–124. [Google Scholar] [CrossRef]
- Dorri, M.; Mozafari Bazargany, M.H.; Khodaparast, Z.; Bahrami, S.; Seifi Alan, M.; Rahimi, F.; Kamipoor, Z.; Niksima, M.M.; Dehghan, H.; Rastad, H. Psychological Problems and Reduced Health-Related Quality of Life in the COVID-19 Survivors. J. Affect. Disord. Rep. 2021, 6, 100248. [Google Scholar] [CrossRef]
| Variables | COVID-19 Survivors (n = 354) | Control Group (n = 751) | Unadjusted OR [95% CI] | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age | ||||
| 18–40 41–60 +60 | 25 (7.1) 138 (39.0) 191 (53.9) | 134 (17.8) 311 (41.4) 306 (40.8) | 1 2.38 [1.48–3.81] 3.35 [2.10–5.32] | <0.0001 <0.0001 |
| Gender | ||||
| Female Male | 175 (49.4) 179 (50.6) | 395 (52.6) 356 (47.4) | 1 1.13 [0.88–1.46] | 0.327 |
| Marital status | ||||
| Single Married Widowed | 33 (9.3) 248 (70.1) 73 (20.6) | 137 (18.2) 515 (68.6) 99 (13.2) | 1 2 [1.33–3.01] 3.06 [1.88–4.97] | 0.001 <0.0001 |
| Presence of children | ||||
| No Yes | 42 (11.9) 312 (88.1) | 171 (22.8) 580 (77.2) | 1 2.19 [1.52–3.15] | <0.0001 |
| Educational level | ||||
| Illiterate Primaryschool Secondary school University | 153 (43.2) 50 (14.1) 82 (23.2) 69 (19.5) | 343 (45.7) 103 (13.7) 163 (21.7) 142 (18.9) | 1 1.09 [0.74–1.60] 1.13 [0.81–1.56] 1.09 [0.77–1.54] | 0.669 0.471 0.627 |
| Employment status | ||||
| Employed Unemployed/retired | 118 (33.3) 236 (66.7) | 256 (34.1) 495 (65.9) | 1 1.03 [0.79–1.35] | 0.805 |
| Place of residence | ||||
| Urban Rural | 309 (87.3) 45 (12.7) | 382 (50.9) 369 (49.1) | 1 0.15 [0.11–0.21] | <0.0001 |
| Socio-economic level | ||||
| Low Medium High | 132 (37.3) 189 (53.4) 33 (9.3) | 255 (33.9) 425 (56.6) 71(9.5) | 1 0.86 [0.65–1.13] 0.90 [0.56–1.43] | 0.272 0.649 |
| Tobacco use | ||||
| No Yes | 292 (82.5) 62 (17.5) | 672 (89.5) 79 (10.5) | 1 1.81 [1.26–2.59] | 0.001 |
| Presence of chronic diseases | ||||
| No Yes | 77 (21.8) 277 (78.2) | 457 (60.9) 294 (39.1) | 1 5.59 [4.18–7.49] | <0.0001 |
| Types of chronic diseases | ||||
| Type 1 diabetes | ||||
| No Yes | 204 (57.6) 150 (42.4) | 600 (79.9) 151 (20.1) | 1 2.92 [2.22–3.85] | <0.0001 |
| Type 2 diabetes | ||||
| No Yes | 303 (85.6) 51 (14.4) | 716 (95.3) 35 (4.7) | 1 3.44 [2.19–5.40] | <0.0001 |
| Hypertension | ||||
| No Yes | 242 (68.4) 112 (31.6) | 550 (73.2) 201 (26.8) | 1 1.27 [0.96–1.67] | 0.094 |
| Kidney diseases | ||||
| No Yes | 199 (56.2) 155 (43.8) | 564 (75.1) 187 (24.9) | 1 2.35 [1.80–3.07] | <0.0001 |
| Cardiovascular diseases | ||||
| No Yes | 292 (82.5) 62 (17.5) | 713 (94.9) 38 (5.1) | 1 3.98 [2.60–6.10] | <0.0001 |
| Variables | COVID-19 Survivors (n = 354) | Control Group (n = 751) | Adjusted OR [95% CI] | p-Value |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age | ||||
| 18–40 | 25 (7.1) | 134 (17.8) | 1 | |
| 41–60 | 138 (39.0) | 311 (41.4) | 1.95 [1.04–3.67] | 0.038 |
| +60 | 191 (53.9) | 306 (40.8) | 1.99 [1.01–3.92] | 0.047 |
| Marital status | ||||
| Single | 33 (9.3) | 137 (18.2) | 1 | |
| Married | 248 (70.1) | 515 (68.6) | 1.27 [0.45–3.59] | 0.656 |
| Widowed | 73 (20.6) | 99 (13.2) | 0.92 [0.30–2.81] | 0.890 |
| Presence of children | ||||
| No | 42 (11.9) | 171 (22.8) | 1 | |
| Yes | 312 (88.1) | 580 (77.2) | 1.56 [0.61–3.95] | 0.351 |
| Place of residence | ||||
| Urban | 309 (87.3) | 382 (50.9) | 1 | |
| Rural | 45 (12.7) | 369 (49.1) | 0.07 [0.05–0.11] | <0.0001 |
| Tobacco use | ||||
| No | 292 (82.5) | 672 (89.5) | 1 | |
| Yes | 62 (17.5) | 79 (10.5) | 2.28 [1.38–3.75] | 0.001 |
| Presence of chronic diseases | ||||
| No | 77 (21.8) | 475 (60.9) | 1 | |
| Yes | 277 (78.2) | 294 (39.1) | 4.28 [2.80–6.55] | <0.0001 |
| Types of chronic diseases | ||||
| Type 1 diabetes | ||||
| No | 204 (57.6) | 600 (79.9) | 1 | |
| Yes | 150 (42.4) | 151 (20.1) | 3.60 [2.39–5.41] | <0.0001 |
| Type 2 diabetes | ||||
| No | 303 (85.6) | 716 (95.3) | 1 | |
| Yes | 51 (14.4) | 35 (4.7) | 1.27 [0.65–2.49] | 0.479 |
| Kidney diseases | ||||
| No | 199 (56.2) | 564 (75.1) | 1 | |
| Yes | 155 (43.8) | 187 (24.9) | 1.67 [1.08–2.60] | 0.021 |
| Cardiovascular diseases | ||||
| No | 292 (82.5) | 713 (94.9) | 1 | |
| Yes | 62 (17.5) | 38 (5.1) | 4.93 [2.68–9.07] | <0.0001 |
| Variables | Mobility | Self Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | |
| Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | ||||||
| Age | |||||||||||||||
| 18–40 41–60 +60 | 83.98 216.05 242.87 | 79.26 228.97 252.83 | 0.623 0.310 0.425 | 90.20 215.22 247.94 | 78.10 229.34 249.66 | 0.189 0.261 0.892 | 103.62 214.94 240.82 | 75.59 229.46 254.11 | 0.003 0.254 0.296 | 125.24 266.97 292.59 | 71.56 206.37 221.79 | <0.0001 <0.0001 <0.0001 | 129.76 269.68 273.32 | 70.72 205.18 233.82 | <0.0001 <0.0001 0.002 |
| Gender | |||||||||||||||
| Female Male | 282.41 271.93 | 286.87 266.02 | 0.755 0.661 | 280.21 281.54 | 287.84 261.19 | 0.594 0.127 | 285.29 279.45 | 285.59 262.24 | 0.983 0.206 | 345.87 343.60 | 258.75 229.99 | <0.0001 <0.0001 | 334.68 340.34 | 263.71 231.63 | <0.0001 <0.0001 |
| Marital status | |||||||||||||||
| Single Married Widowed | 111.17 351.14 90.94 | 79.32 396.86 83.23 | 0.001 0.005 0.289 | 105.88 361.33 93.55 | 80.59 391.96 81.30 | 0.004 0.059 0.098 | 114.91 349.71 94.91 | 78.42 397.55 80.30 | <0.0001 0.003 0.049 | 140.55 443.47 106.06 | 72.24 352.40 72.08 | <0.0001 <0.0001 <0.0001 | 138.80 436.68 96.99 | 72.66 355.67 78.76 | <0.0001 <0.0001 0.014 |
| Presence of children | |||||||||||||||
| No Yes | 131.00 427.17 | 101.11 456.90 | 0.003 0.084 | 129.79 436.61 | 101.40 451.82 | 0.004 0.378 | 138.51 430.02 | 99.26 455.37 | <0.0001 0.145 | 168.23 526.55 | 91.96 403.44 | <0.0001 <0.0001 | 162.45 511.30 | 93.38 411.64 | <0.0001 <0.0001 |
| Educational level | |||||||||||||||
| Illiterate | 237.19 | 253.54 | 0.215 | 246.84 | 249.24 | 0.858 | 240.43 | 252.10 | 0.383 | 288.61 | 230.61 | <0.0001 | 267.02 | 240.24 | 0.049 |
| Primary school | 69.25 | 80.76 | 0.104 | 79.86 | 75.61 | 0.552 | 67.57 | 81.58 | 0.049 | 90.82 | 70.29 | 0.004 | 87.00 | 72.15 | 0.042 |
| Secondary school | 129.24 | 119.86 | 0.304 | 124.30 | 122.34 | 0.827 | 122.34 | 119.63 | 0.273 | 168.07 | 100.33 | <0.0001 | 165.05 | 101.84 | <0.0001 |
| University | 125.69 | 96.43 | 0.001 | 115.13 | 101.56 | 0.098 | 131.86 | 93.44 | <0.0001 | 150.40 | 84.43 | <0.0001 | 155.99 | 81.71 | <0.0001 |
| Employment status | |||||||||||||||
| Employed Unemployed/retired | 219.27 337.88 | 172.86 379.41 | <0.0001 0.008 | 206.96 355.18 | 178.53 371.16 | 0.010 0.319 | 220.86 343.92 | 172.12 376.53 | <0.0001 0.042 | 271.25 418.50 | 148.90 340.97 | <0.0001 <0.0001 | 274.79 400.08 | 147.27 349.75 | <0.0001 0.002 |
| Place of residence | |||||||||||||||
| Urban Rural | 369.95 182.92 | 326.62 210.50 | 0.003 0.118 | 363.39 206.53 | 331.93 207.62 | 0.028 0.952 | 382.36 201.87 | 316.59 208.19 | <0.0001 0.726 | 450.14 243.10 | 261.76 203.16 | <0.0001 0.028 | 433.72 244.44 | 275.04 202.99 | <0.0001 0.024 |
| Socio-economic level | |||||||||||||||
| Low Medium High | 174.36 330.26 47.39 | 204.17 297.38 54.87 | 0.008 0.027 0.210 | 180.52 332.17 47.71 | 200.98 296.53 54.73 | 0.073 0.016 0.244 | 179.81 334.03 49.24 | 201.35 295.70 54.73 | 0.062 0.010 0.428 | 217.29 411.95 58.32 | 181.95 261.05 49.80 | 0.002 <0.0001 0.162 | 201.25 407.69 64.76 | 190.25 262.95 46.80 | 0.345 <0.0001 0.004 |
| Tobacco use | |||||||||||||||
| No Yes | 471.65 78.93 | 487.21 64.78 | 0.404 0.032 | 475.90 84.32 | 485.37 60.54 | 0.610 <0.0001 | 472.62 89.23 | 486.79 56.70 | 0.452 <0.0001 | 588.30 99.45 | 436.53 48.67 | <0.0001 <0.0001 | 560.45 103.48 | 448.63 45.51 | <0.0001 <0.0001 |
| Presence of chronic diseases | |||||||||||||||
| Type 1 diabetes | |||||||||||||||
| Yes | 171.70 | 130.44 | <0.0001 | 168.21 | 133.91 | <0.0001 | 165.58 | 136.51 | 0.003 | 192.14 | 110.13 | <0.0001 | 194.78 | 107.51 | <0.0001 |
| Type 2 diabetes | |||||||||||||||
| Yes | 46.56 | 39.04 | 0.124 | 51.44 | 31.93 | <0.0001 | 45.87 | 40.04 | 0.261 | 51.15 | 32.36 | <0.0001 | 51.36 | 32.04 | <0.0001 |
| Hypertension | |||||||||||||||
| Yes | 161.32 | 154.59 | 0.497 | 165.26 | 152.40 | 0.212 | 162.08 | 154.17 | 0.434 | 196.52 | 134.98 | <0.0001 | 187.79 | 139.85 | <0.0001 |
| Kidney diseases | |||||||||||||||
| Yes | 168.17 | 174.26 | 0.547 | 183.53 | 161.53 | 0.033 | 179.00 | 165.28 | 0.183 | 212.52 | 137.50 | <0.0001 | 205.99 | 142.91 | <0.0001 |
| Cardiovascular diseases | |||||||||||||||
| Yes | 47.73 | 55.03 | 0.190 | 51.31 | 49.18 | 0.709 | 58.28 | 45.73 | 0.027 | 49.85 | 51.57 | 0.764 | 59.13 | 45.21 | 0.012 |
| Variables | Physical Functioning | Role Limitation | Social Functioning | Pain | Mental Health | Vitality | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | C+ | C− | p-Value * | |
| Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | Mean Rank | |||||||
| Age | ||||||||||||||||||
| 18–40 41–60 +60 | 99.12 235.62 239.23 | 76.43 235.62 255.10 | 0.017 0.224 0.215 | 105.76 218.13 242.04 | 75.19 228.05 253.35 | 0.001 0.371 0.295 | 65.80 195.52 278.32 | 82.65 238.08 230.70 | 0.051 <0.0001 <0.0001 | 117.80 251.15 265.92 | 72.95 213.40 238.44 | <0.0001 0.003 0.034 | 131.46 266.29 264.93 | 70.40 206.68 239.06 | <0.0001 <0.0001 0.044 | 108.74 230.66 235.54 | 74.64 222.49 257.40 | <0.0001 0.522 0.086 |
| Gender | ||||||||||||||||||
| Female Male | 289.21 286.66 | 283.85 258.62 | 0.712 0.039 | 282.42 285.01 | 286.86 259.45 | 0.734 0.034 | 288.03 259.45 | 284.38 262.80 | 0.797 0.249 | 313.03 322.68 | 273.31 240.51 | 0.007 <0.0001 | 329.12 336.66 | 266.17 233.48 | <0.0001 <0.0001 | 289.74 287.84 | 283.62 258.03 | 0.673 0.028 |
| Marital status | ||||||||||||||||||
| Single Married Widowed | 125.74 368.86 88.66 | 75.81 388.33 84.91 | <0.0001 0.235 0.613 | 114.48 383.85 73.58 | 78.52 381.11 96.03 | <0.0001 0.849 0.001 | 89.14 373.69 92.51 | 84.62 386.00 82.07 | 0.581 0.447 0.164 | 134.64 406.05 98.52 | 73.66 370.42 77.64 | <0.0001 0.032 0.006 | 137.79 430.17 96.76 | 72.91 358.80 78.93 | <0.0001 <0.0001 0.017 | 117.05 368.98 88.83 | 77.90 388.27 84.78 | <0.0001 0.238 0.584 |
| Presence of children | ||||||||||||||||||
| No Yes | 150.90 437.32 | 96.22 451.44 | <0.0001 0.418 | 132.39 439.68 | 100.76 450.17 | 0.001 0.490 | 112.20 449.62 | 105.72 444.82 | 0.494 0.782 | 160.33 483.46 | 93.90 426.62 | <0.0001 0.001 | 163.17 502.90 | 93.20 416.16 | <0.0001 <0.0001 | 141.62 436.88 | 98.50 451.67 | <0.0001 0.395 |
| Educational level | ||||||||||||||||||
| Illiterate | 232.62 | 255.58 | 0.086 | 230.78 | 256.40 | 0.024 | 239.63 | 252.46 | 0.344 | 260.83 | 243.00 | 0.192 | 264.60 | 241.32 | 0.087 | 232.43 | 255.67 | 0.083 |
| Primary school | 67.69 | 81.52 | 0.057 | 78.96 | 76.05 | 0.661 | 75.84 | 77.56 | 0.816 | 77.55 | 76.73 | 0.912 | 90.68 | 70.36 | 0.005 | 75.09 | 77.93 | 0.692 |
| Secondary school | 136.89 | 116.01 | 0.023 | 132.85 | 118.05 | 0.073 | 128.23 | 120.37 | 0.384 | 161.26 | 103.75 | <0.0001 | 162.31 | 103.22 | <0.0001 | 135.00 | 116.96 | 0.049 |
| University | 141.90 | 88.56 | <0.0001 | 126.60 | 95.99 | <0.0001 | 123.96 | 97.27 | <0.0001 | 143.98 | 87.55 | <0.0001 | 151.99 | 83.65 | <0.0001 | 137.42 | 90.73 | <0.0001 |
| Employment status | ||||||||||||||||||
| Employed | 243.67 | 161.61 | <0.0001 | 225.57 | 169.95 | <0.0001 | 234.53 | 165.82 | <0.0001 | 259.58 | 154.28 | <0.0001 | 269.88 | 149.53 | <0.0001 | 228.17 | 168.75 | <0.0001 |
| Unemployed/retired | 330.87 | 382.75 | 0.001 | 341.28 | 377.78 | 0.007 | 325.36 | 385.38 | <0.0001 | 376.56 | 360.97 | 0.340 | 396.50 | 351.46 | 0.005 | 351.46 | 374.96 | 0.083 |
| Place of residence | ||||||||||||||||||
| Urban Rural | 376.94 199.78 | 320.98 208.44 | <0.0001 0.632 | 372.03 207.38 | 324.95 207.51 | 0.001 0.992 | 380.88 176.99 | 317.79 211.22 | <0.0001 0.062 | 423.95 215.16 | 282.94 206.57 | <0.0001 0.642 | 425.86 249.37 | 281.40 202.39 | <0.0001 0.011 | 383.46 195.56 | 315.70 208.96 | <0.0001 0.457 |
| Socio-economic level | ||||||||||||||||||
| Low Medium High | 177.45 349.78 47.32 | 202.57 288.70 54.91 | 0.027 <0.0001 0.194 | 186.76 334.09 45.67 | 197.75 295.68 55.68 | 0.233 0.005 0.082 | 167.00 356.63 38.95 | 207.97 285.65 58.80 | <0.0001 <0.0001 0.001 | 197.26 383.72 51.71 | 192.31 273.60 52.87 | 0.673 <0.0001 0.853 | 198.86 398.49 67.20 | 191.48 267.04 45.67 | 0.526 <0.0001 <0.0001 | 176.45 343.46 54.48 | 203.08 291.51 51.58 | 0.021 0.001 0.624 |
| Tobacco use | ||||||||||||||||||
| No Yes | 480.17 90.83 | 483.51 55.44 | 0.859 <0.0001 | 475.72 88.02 | 485.45 57.64 | 0.559 <0.0001 | 476.12 88.64 | 485.27 57.16 | 0.625 <0.0001 | 536.94 97.34 | 458.85 50.33 | <0.0001 <0.0001 | 553.25 103.52 | 451.76 45.47 | <0.0001 <0.0001 | 481.29 87.25 | 483.02 58.25 | 0.927 <0.0001 |
| Presence of chronic diseases | ||||||||||||||||||
| Type 1 diabetes | ||||||||||||||||||
| Yes | 179.68 | 122.51 | <0.0001 | 154.43 | 147.60 | 0.356 | 161.45 | 140.62 | 0.030 | 190.46 | 111.80 | <0.0001 | 195.66 | 106.63 | <0.0001 | 166.92 | 135.19 | 0.001 |
| Type 2 diabetes | ||||||||||||||||||
| Yes | 46.05 | 39.79 | 0.177 | 49.49 | 34.77 | <0.0001 | 49.00 | 35.49 | 0.010 | 48.04 | 36.89 | 0.033 | 51.15 | 32.36 | <0.0001 | 46.62 | 38.96 | 0.130 |
| Hypertension | ||||||||||||||||||
| Yes | 168.33 | 150.69 | 0.049 | 168.72 | 150.47 | 0.015 | 155.34 | 157.93 | 0.804 | 177.45 | 145.60 | 0.002 | 185.13 | 141.32 | <0.0001 | 167.83 | 150.97 | 0.098 |
| Kidney diseases | ||||||||||||||||||
| Yes | 174.94 | 168.65 | 0.380 | 180.13 | 164.35 | 0.038 | 138.76 | 198.64 | <0.0001 | 194.93 | 152.08 | <0.0001 | 213.00 | 137.10 | <0.0001 | 190.19 | 156.01 | 0.001 |
| Cardiovascular diseases | ||||||||||||||||||
| Yes | 58.61 | 45.53 | 0.024 | 54.67 | 43.70 | 0.007 | 59.88 | 35.20 | <0.0001 | 60.18 | 44.56 | 0.007 | 61.00 | 44.06 | 0.002 | 58.32 | 45.71 | 0.026 |
| Variables | EQ-VAS | ||
|---|---|---|---|
| β [95% CI] | t | p-Value | |
| Age | −0.082 [−3.84; −0.66] | −2.779 | 0.006 |
| Marital status | −0.016 [−2.20; 1.19] | −0.587 | 0.558 |
| Tobacco use | −0.051 [−4.47; −0.15] | −2.106 | 0.036 |
| Presence of chronic diseases | −0.457 [−21.71; −16.37] | −14.012 | <0.0001 |
| Type 1 diabetes | −0.253 [−10.97; −6.60] | −7.922 | <0.0001 |
| Type 2 diabetes | −0.025 [−4.50; 2.02] | −0.748 | 0.455 |
| Hypertension | −0.015 [−3.13; 1.99] | −0.438 | 0.662 |
| Kidney diseases | −0.398 [−16.51; −11.06] | −9.960 | <0.0001 |
| Cardiovascular diseases | −0.253 [−13.93; −8.98] | −9.114 | <0.0001 |
| SF-6D | EQ-5D-5L | ||||
|---|---|---|---|---|---|
| Mobility | Self-Care | Usual Activities | Pain/Discomfort | Anxiety/Depression | |
| COVID-19 survivors (n = 354) | |||||
| Physical function | 0.85 *** | 0.71 ** | 0.70 ** | 0.71 ** | 0.75 *** |
| Role limitation | 0.57 * | 0.67 ** | 0.52 * | 0.57 * | 0.59 * |
| Social function | 0.59 * | 0.65 ** | 0.59 ** | 0.61 * | 0.51 * |
| Pain | 0.69 ** | 0.70 ** | 0.67 ** | 0.93 *** | 0.72 ** |
| Mental health | 0.61 * | 0.71 ** | 0.62 * | 0.75 *** | 0.95 *** |
| Vitality | 0.64 ** | 0.68 ** | 0.69 ** | 0.66 ** | 0.75 *** |
| Non-COVID-19 (n = 751) | |||||
| Physical function | 0.57 ** | 0.40 * | 0.49 * | 0.54 ** | 0.64 ** |
| Role limitation | 0.37 * | 0.27 * | 0.43 * | 0.34 * | 0.39 * |
| Social function | 0.42 * | 0.39 * | 0.45 * | 0.49 * | 0.56 ** |
| Pain | 0.51 * | 0.50 * | 0.58 ** | 0.91 *** | 0.65 ** |
| Mental health | 0.54 * | 0.42 * | 0.57 ** | 0.62 ** | 0.93 *** |
| Vitality | 0.52 * | 0.43 * | 0.65 ** | 0.61 ** | 0.59 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Azizi, A.; Achak, D.; Saad, E.; Hilali, A.; Nejjari, C.; Khalis, M.; Youlyouz-Marfak, I.; Marfak, A. Health-Related Quality of Life of Moroccan COVID-19 Survivors: A Case-Control Study. Int. J. Environ. Res. Public Health 2022, 19, 8804. https://doi.org/10.3390/ijerph19148804
Azizi A, Achak D, Saad E, Hilali A, Nejjari C, Khalis M, Youlyouz-Marfak I, Marfak A. Health-Related Quality of Life of Moroccan COVID-19 Survivors: A Case-Control Study. International Journal of Environmental Research and Public Health. 2022; 19(14):8804. https://doi.org/10.3390/ijerph19148804
Chicago/Turabian StyleAzizi, Asmaa, Doha Achak, Elmadani Saad, Abderraouf Hilali, Chakib Nejjari, Mohamed Khalis, Ibtissam Youlyouz-Marfak, and Abdelghafour Marfak. 2022. "Health-Related Quality of Life of Moroccan COVID-19 Survivors: A Case-Control Study" International Journal of Environmental Research and Public Health 19, no. 14: 8804. https://doi.org/10.3390/ijerph19148804
APA StyleAzizi, A., Achak, D., Saad, E., Hilali, A., Nejjari, C., Khalis, M., Youlyouz-Marfak, I., & Marfak, A. (2022). Health-Related Quality of Life of Moroccan COVID-19 Survivors: A Case-Control Study. International Journal of Environmental Research and Public Health, 19(14), 8804. https://doi.org/10.3390/ijerph19148804






