Idiosyncratic Profile of Perceived Emotional Intelligence and Post-Traumatic Growth in Breast Cancer Survivors: Findings of a Multiple Mediation Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Procedure
2.3. Measures and Instruments
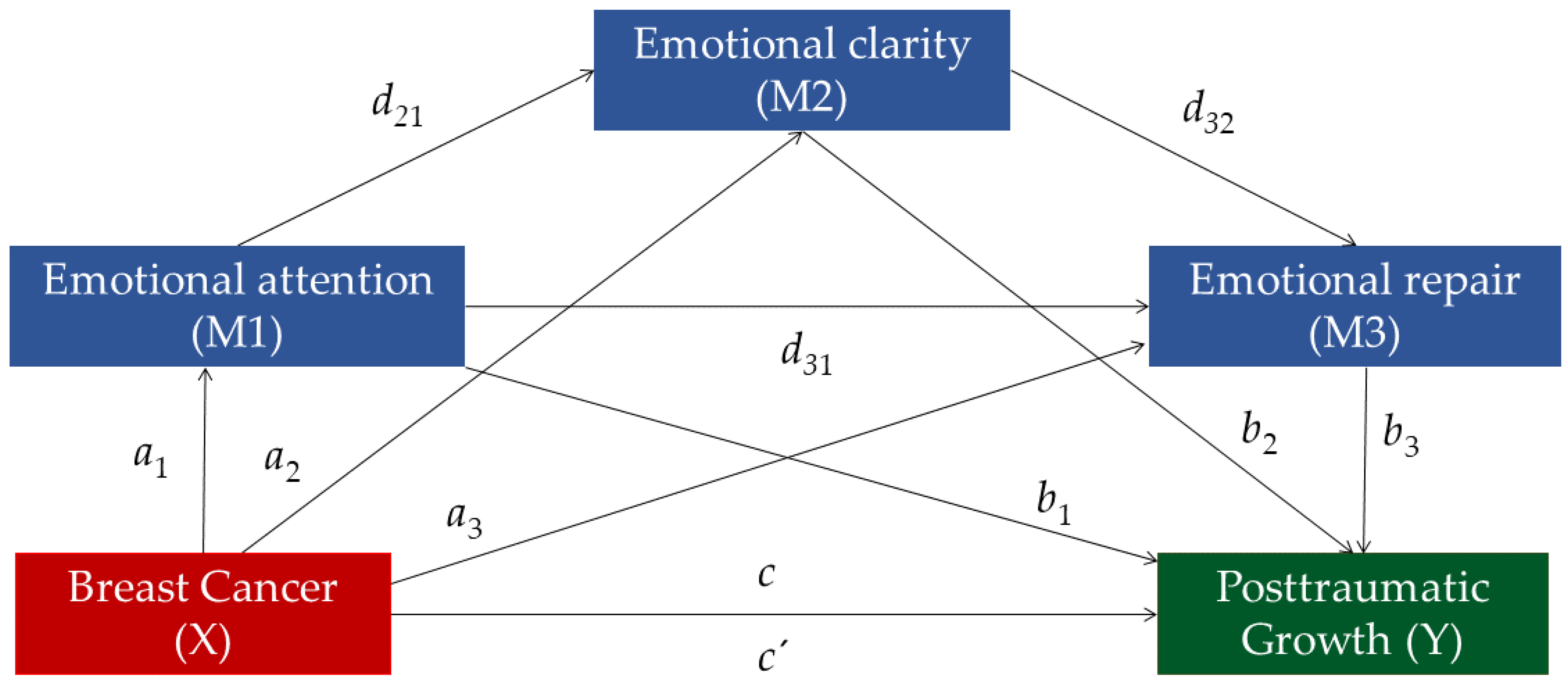
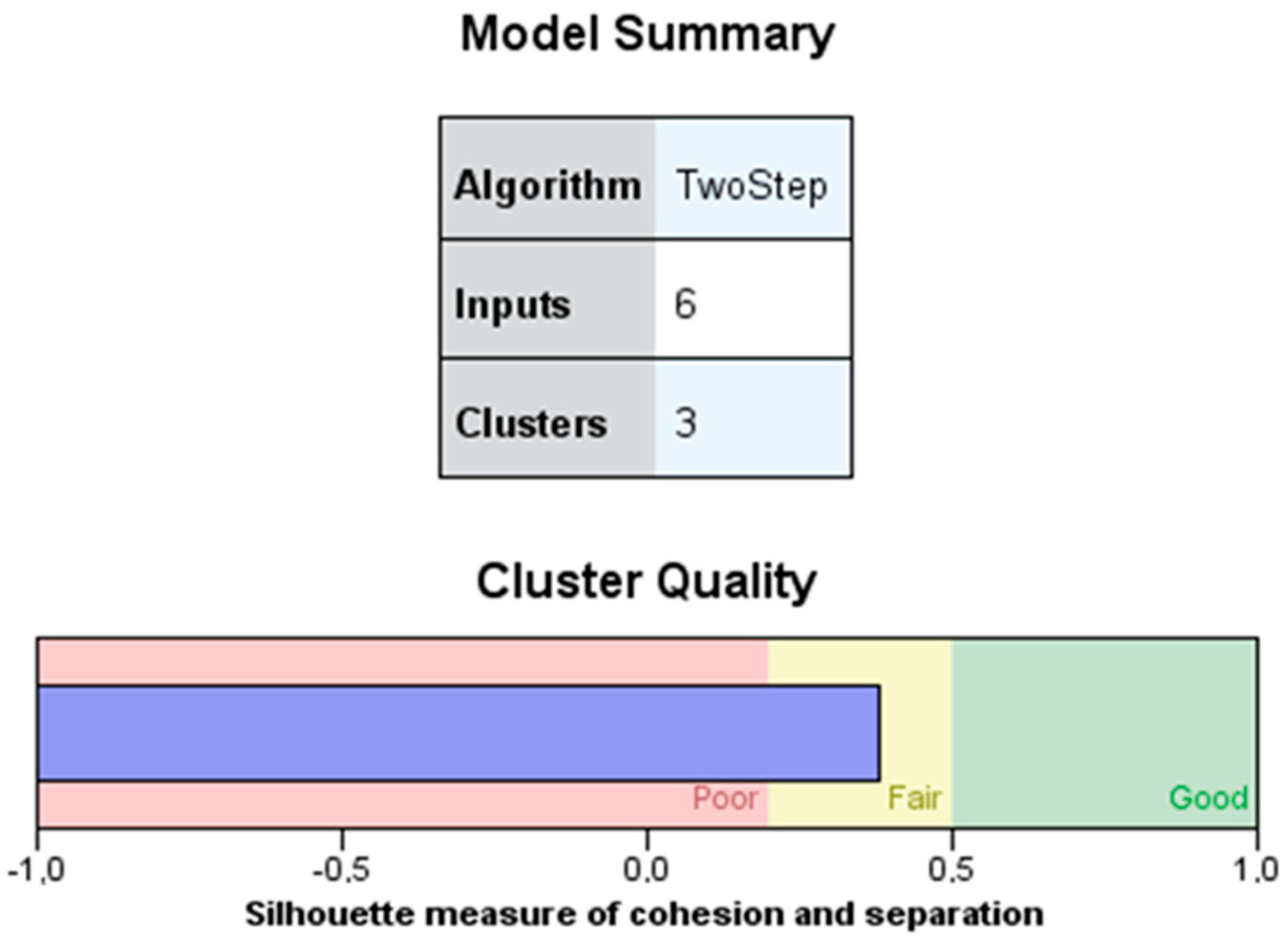
2.4. Statistical Analysis
3. Results
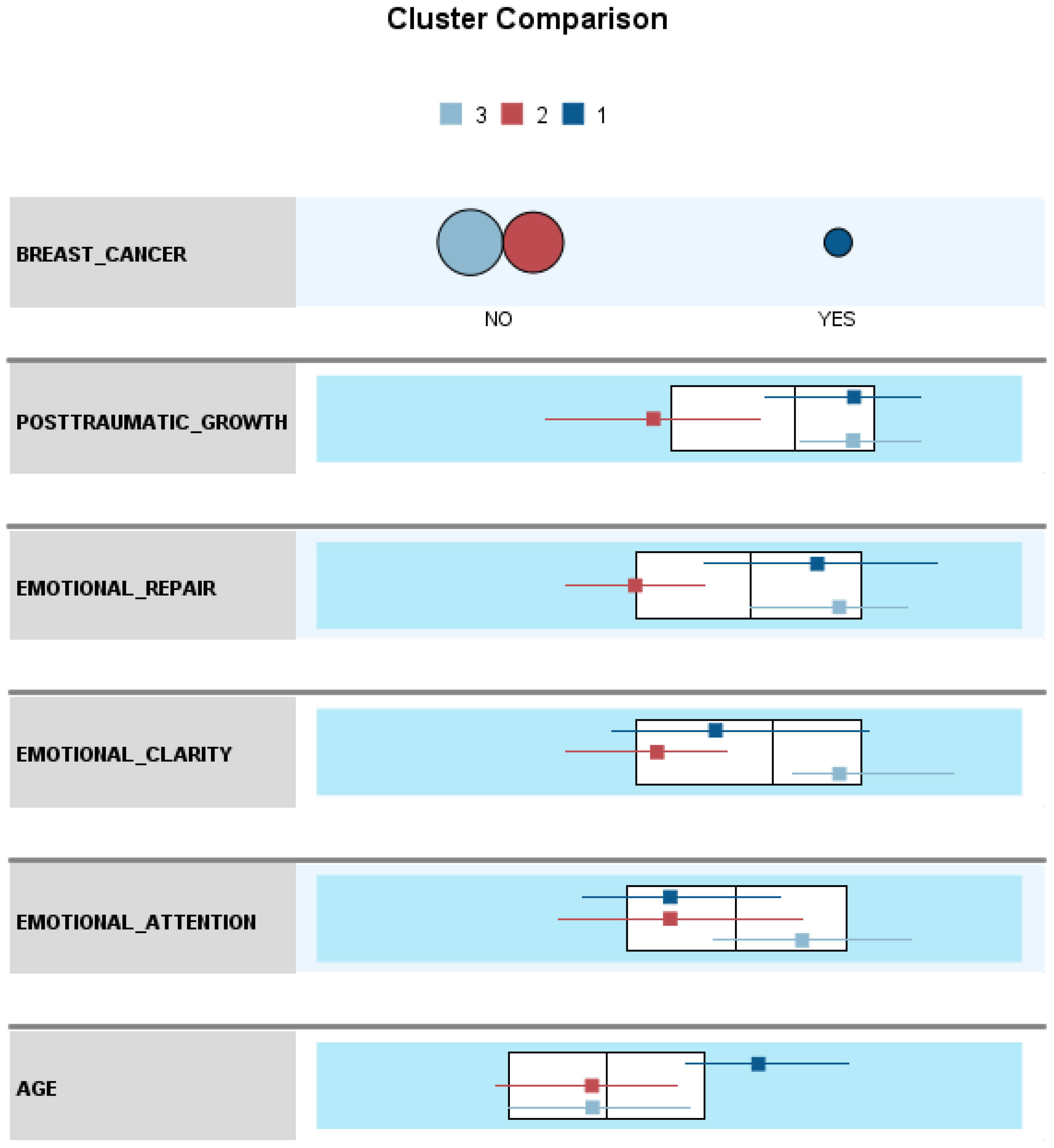
- (1)
- Breast cancer survivors (cluster 1) differed significantly in age (p = 0.000) and showed higher levels of PTG (p = 0.000), emotional clarity (p = 0.001), and emotional repair (p = 0.000) compared to healthy women with low PTG (cluster 2). Cohen’s d results showed a strong effect for age (d = 1.25; [8.26–15.22] 95% CI), PTG (d = 1.44; [21.68–33.96] 95% CI), and emotional repair (d = 1.13; [5.26–9.02] 95% CI), and a medium effect for emotional clarity (d = 0.47; [1.13–5.05] 95% CI). In emotional attention, no significant differences were found between groups (p > 0.05).
- (2)
- The mean scores of breast cancer survivors (cluster 1) differed significantly from healthy women with high PTG (cluster 3) in being older (p = 0.000) and showing lower levels of emotional attention (p = 0.000) and emotional clarity (p = 0.000). Cohen’s d results demonstrated a strong effect for age (d = 1.19; [7.62–14.49] 95% CI) and emotional clarity (d = 0.91; [3.57–7.43] 95% CI), and medium effect for emotional attention (d = 0.76; [2.65–7.51] 95% CI). No differences were found in PTG levels and emotional repair (p > 0.05).
- (3)
- Healthy women with low levels of PTG (cluster 2) differed significantly from women with high PTG levels (cluster 3) in lower scores on PTG (p = 0.000) and emotional attention (p = 0.000), clarity (p = 0.000), and emotional repair (p = 0.000). Cohen’s d results showed a strong effect for PTG (d = 1.78; [27.36,34.33] 95% CI), emotional clarity (d = 1.62; [7.49–9.70] 95% CI), and emotional repair (d = 1.70; [7.47–9.60] 95% CI), and medium effect for emotional attention (d = 0.71; [3.52–6.30] 95% CI).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arnaboldi, P.; Riva, S.; Crico, C.; Pravettoni, G. A systematic literature review exploring the prevalence of post-traumatic stress disorder and the role played by stress and traumatic stress in breast cancer diagnosis and trajectory. Breast Cancer Targets Ther. 2017, 9, 473–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, H.; Brand, J.S.; Fang, F.; Chiesa, F.; Johansson, A.L.; Hall, P.; Czene, K. Time-dependent risk of depression, anxiety, and stress-related disorders in patients with invasive and in situ breast cancer. Int. J. Cancer 2017, 140, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Nardin, S.; Mora, E.; Varughese, F.M.; D’Avanzo, F.; Vachanaram, A.R.; Rossi, V.; Gennari, A. Breast cancer survivorship, quality of life, and late toxicities. Front. Oncol. 2020, 10, 864. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.E.; Wiskemann, J.; Steindorf, K. Quality of life, problems, and needs of disease-free breast cancer survivors 5 years after diagnosis. Qual. Life Res. 2018, 27, 2077–2086. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.J.; Sidhu, N.; Singh, B. Psychiatric co-morbidity (anxiety and depression) in patients of advanced breast cancer on palliative treatment. Eur. J. Surg. Oncol. 2021, 47, e41–e42. [Google Scholar] [CrossRef]
- Zabora, J.; BrintzenhofeSzoc, K.; Curbow, B.; Hooker, C.; Piantadosi, S. The prevalence of psychological distress by cancer site. Psycho-Oncology 2001, 10, 19–28. [Google Scholar] [CrossRef]
- Brandão, T.; Schulz, M.S.; Matos, P.M. Psychological adjustment after breast cancer: A systematic review of longitudinal studies. Psycho-Oncology 2017, 26, 917–926. [Google Scholar] [CrossRef]
- Tu, P.C.; Yeh, D.C.; Hsieh, H.C. Positive psychological changes after breast cancer diagnosis and treatment: The role of trait resilience and coping styles. J. Psychosoc. Oncol. 2020, 38, 156–170. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. A clinical approach to posttraumatic growth. In Positive Psychology in Practice; Linley, A., Joseph, S., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2004; pp. 405–419. [Google Scholar]
- Wu, X.; Kaminga, A.C.; Dai, W.; Deng, J.; Wang, Z.; Pan, X.; Liu, A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect. Disord. 2019, 243, 408–415. [Google Scholar] [CrossRef]
- Zoellner, T.; Maercker, A. Posttraumatic growth in clinical psychology—A critical review and introduction of a two component model. Clin. Psychol. Rev. 2006, 26, 626–653. [Google Scholar] [CrossRef]
- Cormio, C.; Muzzatti, B.; Romito, F.; Mattioli, V.; Annunziata, M.A. Posttraumatic growth and cancer: A study 5 years after treatment end. Support. Care Cancer 2017, 25, 1087–1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamama-Raz, Y.; Pat-Horenczyk, R.; Roziner, I.; Perry, S.; Stemmer, S.M. Can posttraumatic growth after breast cancer promote positive coping?-A cross-lagged study. Psycho-Oncology 2019, 28, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Zhai, J.; Newton, J.; Copnell, B. Posttraumatic growth experiences and its contextual factors in women with breast cancer: An integrative review. Health Care Women Int. 2019, 40, 554–580. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.E.; Wang, H.Y.; Wang, M.L.; Su, Y.L.; Wang, P.L. Posttraumatic growth and psychological distress in Chinese early-stage breast cancer survivors: A longitudinal study. Psycho-Oncology 2014, 23, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Thong, M.S.; Doege, D.; Koch-Gallenkamp, L.; Bertram, H.; Eberle, A.; Arndt, V. Prevalence of benefit finding and posttraumatic growth in long-term cancer survivors: Results from a multi-regional population-based survey in Germany. Br. J. Cancer 2021, 125, 877–883. [Google Scholar] [CrossRef]
- Wang, M.L.; Liu, J.E.; Wang, H.Y.; Chen, J.; Li, Y.Y. Posttraumatic growth and associated socio-demographic and clinical factors in Chinese breast cancer survivors. Eur. J. Oncol. Nurs. 2014, 18, 478–483. [Google Scholar] [CrossRef]
- Weiss, T. Posttraumatic growth in women with breast cancer and their husbands: An intersubjective validation study. J. Psychosoc. Oncol. 2002, 20, 65–80. [Google Scholar] [CrossRef]
- Sharma, A.; Zhang, J. Predictors of post traumatic growth among breast cancer patients in Nepal. Asian Pac. J. Health Sci. 2017, 4, 9–17. [Google Scholar] [CrossRef]
- Zsigmond, O.; Vargay, A.; Józsa, E.; Bányai, É. Factors contributing to post-traumatic growth following breast cancer: Results from a randomized longitudinal clinical trial containing psychological interventions. Dev. Health Sci. 2019, 2, 29–35. [Google Scholar] [CrossRef]
- Groarke, A.; Curtis, R.; Groarke, J.M.; Hogan, M.J.; Gibbons, A.; Kerin, M. Post-traumatic growth in breast cancer: How and when do distress and stress contribute? Psycho-Oncology 2017, 26, 967–974. [Google Scholar] [CrossRef] [Green Version]
- Paredes, A.C.; Pereira, M.G. Spirituality, distress and posttraumatic growth in breast cancer patients. J. Relig. Health 2018, 57, 1606–1617. [Google Scholar] [CrossRef] [PubMed]
- Romeo, A.; Di Tella, M.; Ghiggia, A.; Tesio, V.; Torta, R.; Castelli, L. Posttraumatic growth in breast cancer survivors: Are depressive symptoms really negative predictors? Psychol. Trauma 2020, 12, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Larsen, S.E.; Berenbaum, H. Are specific emotion regulation strategies differentially associated with posttraumatic growth versus stress? J. Aggress. Maltreat. Trauma 2015, 24, 794–808. [Google Scholar] [CrossRef]
- Orejuela-Dávila, A.I.; Levens, S.M.; Sagui-Henson, S.J.; Tedeschi, R.G.; Sheppes, G. The relation between emotion regulation choice and posttraumatic growth. Cogn. Emot. 2019, 33, 1709–1717. [Google Scholar] [CrossRef]
- Pazderka, H.; Brown, M.R.; McDonald-Harker, C.B.; Greenshaw, A.J.; Agyapong, V.I.; Noble, S.; Silverstone, P.H. Model of Post-traumatic Growth in Newly Traumatized vs. Retraumatized Adolescents. Front. Psychiatry 2021, 12, 682055. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. Trauma and Transformation; Sage Publications: Thousand Oak, CA, USA; London, UK, 1995. [Google Scholar]
- Lotfi-Kashani, F.; Vaziri, S.; Akbari, M.E.; Kazemi-Zanjani, N.; Shamkoeyan, L. Predicting post traumatic growth based upon self-efficacy and perceived social support in cancer patients. Iran. J. Cancer Prev. 2014, 7, 115–123. [Google Scholar] [PubMed]
- Zeng, W.; Zeng, Y.; Xu, Y.; Huang, D.; Shao, J.; Wu, J.; Wu, X. The influence of post-traumatic growth on college students’ creativity during the COVID-19 pandemic: The mediating role of general self-efficacy and the moderating role of deliberate rumination. Front. Psychol. 2021, 12, 665973. [Google Scholar] [CrossRef]
- Hartman, S.D.; Wasieleski, D.T.; Whatley, M.A. Just breathe: The effects of emotional dysregulation and test anxiety on GPA. Coll. Stud. J. 2017, 51, 142–151. [Google Scholar]
- Lu, Q.; Yeung, N.; Man, J.; Gallagher, M.W.; Chu, Q.; Deen, S.H. Ambivalence over emotional expression, intrusive thoughts, and posttraumatic stress symptoms among Chinese American breast cancer survivors. Support. Care Cancer 2017, 25, 3281–3287. [Google Scholar] [CrossRef]
- Mestre, J.M.; Núñez-Lozano, J.M.; Gómez-Molinero, R.; Zayas, A.; Guil, R. Emotion Regulation Ability and Resilience in a Sample of Adolescents from a Suburban Area. Front. Psychol. 2017, 8, 1980. [Google Scholar] [CrossRef] [Green Version]
- Wills, T.A.; Simons, J.S.; Sussman, S.; Knight, R. Emotional self-control and dysregulation: A dual-process analysis of pathways to externalizing/internalizing symptomatology and positive well-being in younger adolescents. Drug Alcohol Depend. 2016, 163, 37–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez, S.; Conchado, A.; Andreu, Y.; Galdón, M.J.; Cardeña, E.; Ibáñez, E.; Durá, E. Acute stress trajectories 1 year after a breast cancer diagnosis. Support. Care Cancer 2016, 24, 1671–1678. [Google Scholar] [CrossRef] [PubMed]
- Cohee, A.A.; Adams, R.N.; Johns, S.A.; Von Ah, D.; Zoppi, K.; Fife, B.; Monahan, P.O.; Stump, T.; Cella, D.; Champion, V.L. Long-term fear of recurrence in young breast cancer survivors and partners. Psycho-Oncology 2017, 26, 22–28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conley, C.C.; Bishop, B.T.; Andersen, B.L. Emotions and emotion regulation in breast cancer survivorship. Healthcare 2016, 4, 56. [Google Scholar] [CrossRef] [Green Version]
- Di Fabio, A.; Kenny, M.E. Promoting well-being: The contribution of emotional intelligence. Front. Psychol. 2016, 7, 1182. [Google Scholar] [CrossRef] [Green Version]
- Dooley, L.N.; Slavich, G.M.; Moreno, P.I.; Bower, J.E. Strength through adversity: Moderate lifetime stress exposure is associated with psychological resilience in breast cancer survivors. Stress Health 2017, 33, 549–557. [Google Scholar] [CrossRef]
- Friedman, H.S.; Kern, M.L. Personality, well-Being, and Health. Annu. Rev. Psychol. 2014, 65, 719–742. [Google Scholar] [CrossRef] [Green Version]
- Wischerth, G.A.; Mulvaney, M.K.; Brackett, M.A.; Perkins, D. The Adverse Influence of Permissive Parenting on Personal Growth and the Mediating Role of Emotional Intelligence. J. Genet. Psychol. 2016, 177, 185–189. [Google Scholar] [CrossRef]
- Mayer, J.D.; Salovey, P. What is emotional intelligence? In Emotional Development and Emotional Intelligence: Educational Implications; Salovey, P., Sluyter, D.J., Eds.; Basic Books: New York, NY, USA, 1997; pp. 3–31. [Google Scholar]
- Petrides, K.V. Trait emotional intelligence theory. Indust. Organ. Psychol. 2010, 3, 136–139. [Google Scholar] [CrossRef]
- Salovey, P.; Mayer, J.D.; Goldman, S.L.; Turvey, C.; Palfai, T.P. Emotional attention, clarity, and repair: Exploring emotional intelligence using the Trait Meta-Mood Scale. In Emotion, Disclosure, and Health; Pennebaker, J.W., Ed.; American Psychological Association: Washington, DC, USA, 1995; pp. 125–154. [Google Scholar]
- Extremera, N.; Fernández-Berrocal, P. Relation of perceived emotional intelligence and health-related quality of life of middle-aged women. Psychol. Rep. 2002, 91, 47–59. [Google Scholar] [CrossRef]
- Fernández-González, L.; Calvete, E.; Orue, I.; Echezarraga, A. The role of emotional intelligence in the maintenance of adolescent dating violence perpetration. Pers. Individ. Differ. 2018, 127, 68–73. [Google Scholar] [CrossRef]
- Merchán-Clavellino, A.; Salguero-Alcañiz, M.P.; Guil, R.; Alameda-Bailén, J.R. Impulsivity, emotional intelligence, and alcohol consumption in young people: A mediation analysis. Foods 2020, 9, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, A.; Ramalho, N.; Morin, E. A comprehensive meta-analysis of the relationship between emotional intelligence and health. Pers. Individ. Differ. 2010, 49, 554–564. [Google Scholar] [CrossRef]
- Amirifard, N.; Payandeh, M.; Aeinfar, M.; Sadeghi, M.; Sadeghi, E.; Ghafarpor, S. A survey on the relationship between emotional intelligence and level of depression and anxiety among women with breast cancer. Int. J. Hemato. Oncol. Stem Cell Res. 2017, 11, 54–57. [Google Scholar]
- Baudry, A.S.; Anota, A.; Mariette, C.; Bonnetain, F.; Renaud, F.; Piessen, G. The role of trait emotional intelligence in quality of life, anxiety and depression symptoms after surgery for esophageal or gastric cancer: A French national database FREGAT. Psycho-Oncology 2019, 28, 799–806. [Google Scholar] [CrossRef]
- Li, Y.; Cao, F.; Cao, D.; Liu, J. Nursing students’ post-traumatic growth, emotional intelligence and psychological resilience. J. Psychiatr. Ment. Health Nurs. 2015, 22, 326–332. [Google Scholar] [CrossRef]
- Sadeghpour, F.; Heidarzadeh, M.; Naseri, P.; Nadr-Mohammadi Moghadam, M. Emotional intelligence as a predictor of posttraumatic growth in patients undergoing hemodialysis. Illn. Cris. Loss 2018, 29, 131–142. [Google Scholar] [CrossRef]
- Tuck, D.; Patlamazoglou, L. The relationship between traumatic stress, emotional intelligence, and posttraumatic growth. J. Loss Trauma 2019, 24, 721–735. [Google Scholar] [CrossRef]
- Danhauer, S.C.; Case, L.D.; Tedeschi, R.; Russell, G.; Vishnevsky, T.; Triplett, K.; Ip, E.H.; Avis, N.E. Predictors of posttraumatic growth in women with breast cancer. Psycho-Oncology 2013, 22, 2676–2683. [Google Scholar] [CrossRef] [Green Version]
- Manne, S.; Ostroff, J.; Winkel, G.; Goldstein, L.; Fox, K.; Grana, G. Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosom. Med. 2004, 66, 442–454. [Google Scholar]
- Zhou, X.; Wu, X.; Zhen, R. Understanding the relationship between social support and posttraumatic stress disorder/posttraumatic growth among adolescents after Ya’an earthquake: The role of emotion regulation. Psychol. Trauma 2017, 9, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, A.; Pradhan, R.K.; Jena, L.K. Curiosity and meaning of life leading towards personal growth: The role of emotional intelligence. J. Indian Acad. Appl. Psychol. 2015, 41, 226–235. [Google Scholar]
- Kira, I.A.; Arıcı Özcan, N.; Shuwiekh, H.; Kucharska, J.; Al-Huwailah, A.H.; Kanaan, A. The compelling dynamics of “will to exist, live, and survive” on effecting posttraumatic growth upon exposure to adversities: Is it mediated, in part, by emotional regulation, resilience, and spirituality? Traumatology 2020, 26, 405–419. [Google Scholar] [CrossRef]
- Rider Mundey, K.; Nicholas, D.; Kruczek, T.; Tschopp, M.; Bolin, J. Posttraumatic growth following cancer: The influence of emotional intelligence, management of intrusive rumination, and goal disengagement as mediated by deliberate rumination. J. Psychosoc. Oncol. 2018, 37, 456–477. [Google Scholar] [CrossRef] [PubMed]
- Pat-Horenczyk, R.; Perry, S.; Hamama-Raz, Y.; Ziv, Y.; Schramm-Yavin, S.; Stemmer, S.M. Posttraumatic growth in breast cancer survivors: Constructive and illusory aspects. J. Trauma. Stress 2015, 28, 214–222. [Google Scholar] [CrossRef]
- Guil, R.; Ruiz-González, P.; Merchán-Clavellino, A.; Morales-Sánchez, L.; Zayas, A.; Gómez-Molinero, R. Breast Cancer and Resilience: The Controversial Role of Perceived Emotional Intelligence. Front. Psychol. 2020, 11, 595713. [Google Scholar] [CrossRef]
- Hamidian, P.; Rezaee, N.; Shakiba, M.; Navidian, A. The effect of cognitive-emotional training on post-traumatic growth in women with breast cancer in Middle East. J. Clin. Psychol. Med. 2019, 26, 25–32. [Google Scholar] [CrossRef]
- Davis, S.K.; Nichols, R. Does emotional intelligence have a “dark” side? A review of the literature. Front. Psychol. 2016, 7, 1316. [Google Scholar] [CrossRef] [Green Version]
- Guil, R.; Gómez-Molinero, R.; Merchan-Clavellino, A.; Gil-Olarte, P.; Zayas García, A. Facing anxiety, growing up. Trait emotional intelligence as a mediator of the relationship between self-esteem and pre-university anxiety. Front. Psychol. 2019, 10, 567. [Google Scholar] [CrossRef] [Green Version]
- Fernández-Berrocal, P.; Extremera, N.; Ramos, N. Validity and reliability of the Spanish modified version of the Trait Meta-Mood Scale. Psychol. Rep. 2004, 94, 751–755. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–472. [Google Scholar] [CrossRef] [PubMed]
- Weiss, T.; Berger, R. Reliability and Validity of a Spanish Version of the Posttraumatic Growth Inventory. Res. Soc. Work Pract. 2006, 16, 191–199. [Google Scholar] [CrossRef]
| Variables | Total Sample | BC Survivors | Control Group | ||||
|---|---|---|---|---|---|---|---|
| α | M | SD | M | SD | M | SD | |
| Age | - | 41.40 | 10.12 | 51.77 | 8.91 | 40.40 | 9.71 |
| PTG | 0.95 | 66.89 | 22.69 | 77.08 | 17.70 | 65.91 | 22.89 |
| EA | 0.92 | 27.07 | 7.24 | 24.50 | 7.04 | 27.32 | 7.21 |
| EC | 0.94 | 28.55 | 6.80 | 27.14 | 7.18 | 28.68 | 6.76 |
| ER | 0.91 | 28.01 | 6.64 | 30.32 | 7.16 | 27.78 | 6.55 |
| Regression Analyses | Predictor Variables | R2 | F | β | p |
|---|---|---|---|---|---|
| Total sample | Breast cancer | 0.27 | 45.41 *** | 9.49 | 0.001 |
| EA | 0.36 | 0.003 | |||
| EC | 0.32 | 0.026 | |||
| ER | 1.39 | 0.000 | |||
| Healthy controls | EA | 0.27 | 53.09 *** | 0.29 | 0.021 |
| ER | 1.56 | 0.000 | |||
| Breast cancer survivors | EA | 0.23 | 3.83 ** | 0.84 | 0.036 |
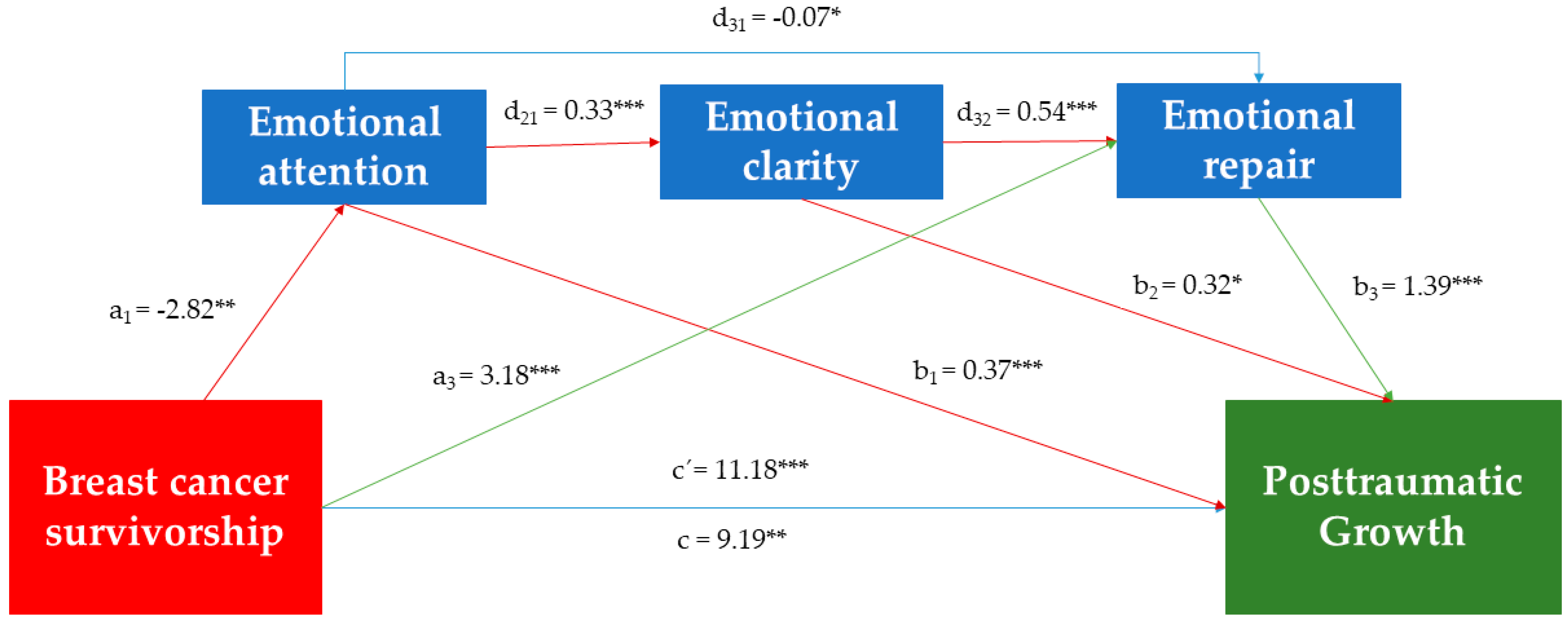
| Model Summary | R2 | MSE | F | df1 | df2 | p (sig) | |
| 0.265 | 381.13 | 56.81 | 4.00 | 631.00 | 0.000 | ||
| Total effect model BCS on PTG | 0.019 | 505.87 | 12.62 | 1.00 | 634.00 | 0.004 | |
| 95% CI | |||||||
| Total effect | Path | Coeff. | SE | T | p | BootLL | BootUL |
| BCS on PTG without accounting for mediators | c | 9.19 | 2.78 | 3.30 | 0.001 | 3.72 | 14.66 |
| Direct Effects | |||||||
| BCS on PTG when accounting for mediators | c’ | 11.18 | 3.15 | 3.55 | 0.000 | 5.00 | 17.36 |
| BCS on EA | a1 | −2.82 | 1.01 | −2.80 | 0.005 | −4.80 | −0.84 |
| BCS on ER | a3 | 3.18 | 0.79 | 4.02 | 0.000 | 1.63 | 4.73 |
| EA on PTG | b1 | 0.37 | 0.12 | 3.18 | 0.001 | 0.14 | 0.59 |
| EC on PTG | b2 | 0.32 | 0.14 | 2.21 | 0.03 | 0.04 | 0.60 |
| ER on PTG | b3 | 1.39 | 0.14 | 10.03 | 0.000 | 1.12 | 1.66 |
| EA on EC | d21 | 0.33 | 0.04 | 9.51 | 0.000 | 0.26 | 0.40 |
| EA on ER | d31 | −0.07 | 0.03 | −1.99 | 0.046 | −0.13 | −0.00 |
| EC on ER | d32 | 0.54 | 0.04 | 15.35 | 0.000 | 0.47 | 0.61 |
| Indirect effects | |||||||
| Ind1. BCS on PTG via EA | a1b1 | −1.03 | 0.50 | −2.13 | −0.20 | ||
| Ind3. BCS on PTG via ER | a3b3 | 4.41 | 1.31 | 1.96 | 7.14 | ||
| Ind4. BCS on PTG via EA and EC in serial | a1d21b2 | −0.30 | 0.19 | −0.73 | −0.01 | ||
| Ind7. BCS on PTG via EA, EC, and ER in serial | a1d21d32b3 | −0.70 | 0.28 | −1.31 | −0.21 | ||
| Specific indirect effect contrast definitions | |||||||
| (C2) Ind1 minus Ind3 | −5.44 | 1.48 | −8.46 | −2.67 | |||
| (C4) Ind1 minus Ind5 | −1.29 | 0.60 | −2.61 | −0.28 | |||
| (C7) Ind2 minus Ind3 | −4.60 | 1.32 | −7.32 | −2.12 | |||
| (C12) Ind3 minus Ind4 | 4.71 | 1.33 | 2.21 | 7.45 | |||
| (C13) Ind3 minus Ind5 | 4.15 | 1.32 | 1.69 | 6.91 | |||
| (C14) Ind3 minus Ind6 | 4.86 | 1.46 | 2.20 | 7.87 | |||
| (C15) Ind3 minus Ind7 | 5.11 | 1.42 | 2.48 | 8.06 | |||
| (C16) Ind4 minus Ind5 | −0.56 | 0.30 | −1.26 | −0.08 | |||
| (C18) Ind4 minus Ind7 | 0.41 | 0.26 | 0.02 | 1.01 | |||
| (C20) Ind5 minus Ind7 | 0.96 | 0.43 | 0.26 | 1.92 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guil, R.; Ruiz-González, P.; Morales-Sánchez, L.; Gómez-Molinero, R.; Gil-Olarte, P. Idiosyncratic Profile of Perceived Emotional Intelligence and Post-Traumatic Growth in Breast Cancer Survivors: Findings of a Multiple Mediation Model. Int. J. Environ. Res. Public Health 2022, 19, 8592. https://doi.org/10.3390/ijerph19148592
Guil R, Ruiz-González P, Morales-Sánchez L, Gómez-Molinero R, Gil-Olarte P. Idiosyncratic Profile of Perceived Emotional Intelligence and Post-Traumatic Growth in Breast Cancer Survivors: Findings of a Multiple Mediation Model. International Journal of Environmental Research and Public Health. 2022; 19(14):8592. https://doi.org/10.3390/ijerph19148592
Chicago/Turabian StyleGuil, Rocío, Paula Ruiz-González, Lucía Morales-Sánchez, Rocío Gómez-Molinero, and Paloma Gil-Olarte. 2022. "Idiosyncratic Profile of Perceived Emotional Intelligence and Post-Traumatic Growth in Breast Cancer Survivors: Findings of a Multiple Mediation Model" International Journal of Environmental Research and Public Health 19, no. 14: 8592. https://doi.org/10.3390/ijerph19148592
APA StyleGuil, R., Ruiz-González, P., Morales-Sánchez, L., Gómez-Molinero, R., & Gil-Olarte, P. (2022). Idiosyncratic Profile of Perceived Emotional Intelligence and Post-Traumatic Growth in Breast Cancer Survivors: Findings of a Multiple Mediation Model. International Journal of Environmental Research and Public Health, 19(14), 8592. https://doi.org/10.3390/ijerph19148592










