Gestational Diabetes Mellitus: A Cross-Sectional Survey of Its Knowledge and Associated Factors among United Arab Emirates University Students
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Setting
2.2. Participants and Sampling
2.3. Sample Size
2.4. Data Collection and Procedure
2.5. Outcome Variables
2.6. Associated Factors
2.7. Statistical Analysis
3. Results
3.1. Students’ Sociodemographic Characteristics
3.2. Students’ GDM Knowledge Status
3.3. Students’ GDM Knowledge Levels
3.4. Regression Analysis for GDM Knowledge levels
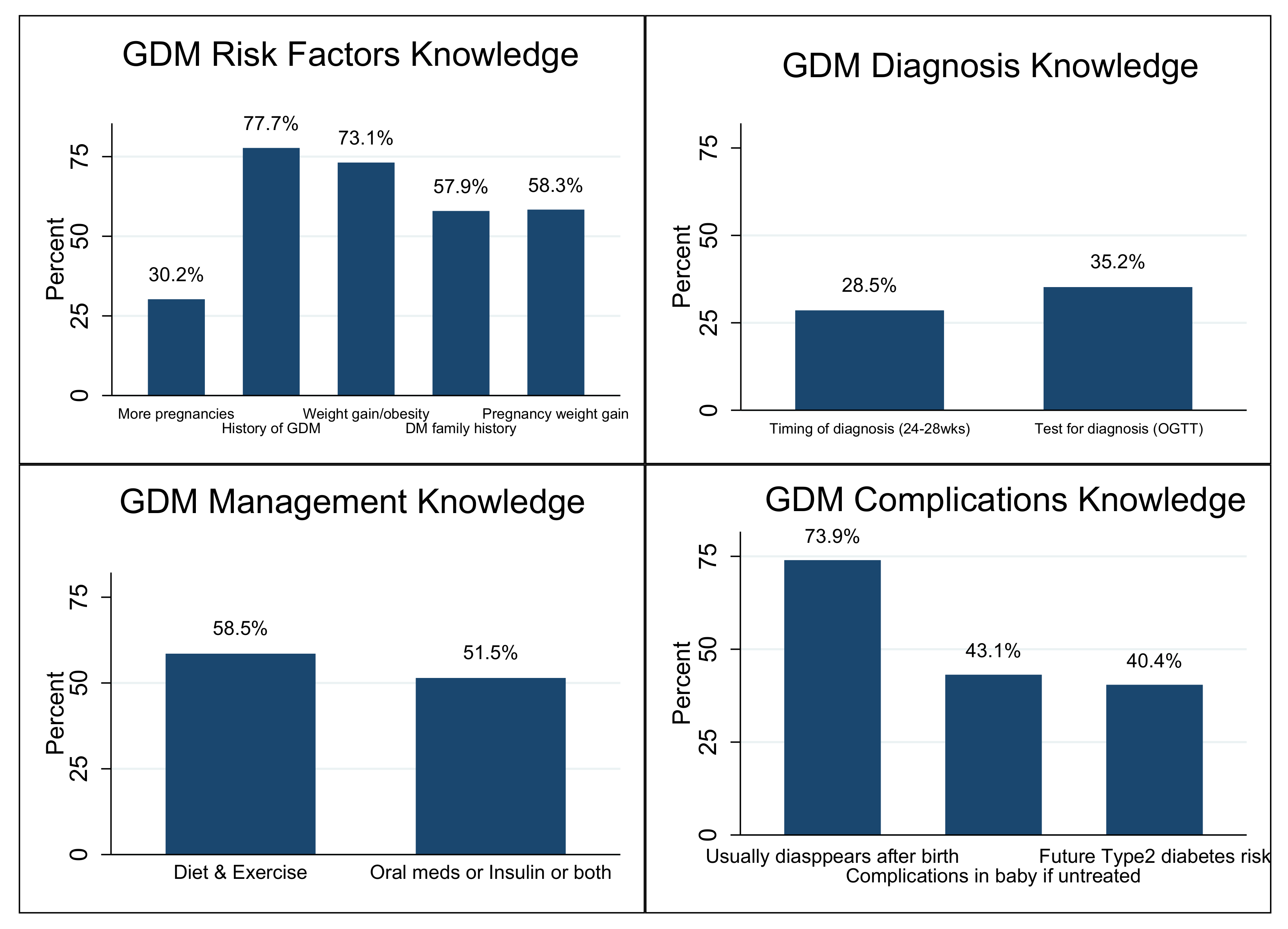
3.5. Knowledge Domains (GDM Risk Factors, Diagnosis, Management, and Complications)
3.6. Sources of GDM Knowledge among the Students
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| GDM | gestational diabetes mellitus |
| DM | diabetes mellitus |
| ANC | antenatal care |
| OGTT | oral glucose tolerance test |
| BMI | body mass index |
| UAE | United Arab Emirates |
References
- Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37 (Suppl. S1), S81–S90. [CrossRef] [PubMed] [Green Version]
- Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: A World Health Organization Guideline. Diabetes Res. Clin. Pract. 2014, 103, 341–363. [CrossRef] [PubMed]
- Stacey, T.; Tennant, P.; McCowan, L.; Mitchell, E.; Budd, J.; Li, M.; Thompson, J.; Martin, B.; Roberts, D.; Heazell, A. Gestational diabetes and the risk of late stillbirth: A case–control study from England, UK. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 973–982. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Lancet. Gestational diabetes in England: Cause for concern. Lancet 2019, 393, 1262. [Google Scholar] [CrossRef]
- Coustan, D.R.; Lowe, L.P.; Metzger, B.E.; Dyer, A.R.; International Association of Diabetes and Pregnancy Study Groups. The Hyperglycemia and Adverse Pregnancy Outcome (HAPO) study: Paving the way for new diagnostic criteria for gestational diabetes mellitus. Am. J. Obs. Gynecol. 2010, 202, 654.e1–654.e6. [Google Scholar] [CrossRef] [Green Version]
- Garrison, A. Screening, diagnosis, and management of gestational diabetes mellitus. Am. Fam. Physician 2015, 91, 460–467. [Google Scholar]
- Agarwal, M.M.; Dhatt, G.S.; Punnose, J.; Koster, G. Gestational diabetes: Dilemma caused by multiple international diagnostic criteria. Diabet. Med. 2005, 22, 1731–1736. [Google Scholar] [CrossRef]
- Kim, C.; Newton, K.M.; Knopp, R.H. Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care 2002, 25, 1862–1868. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, M.M. Gestational Diabetes in the Arab Gulf Countries: Sitting on a Land-Mine. Int. J. Environ. Res. Public Health 2020, 17, 9270. [Google Scholar] [CrossRef]
- Fetita, L.S.; Sobngwi, E.; Serradas, P.; Calvo, F.; Gautier, J.F. Consequences of fetal exposure to maternal diabetes in offspring. J. Clin. Endocrinol. Metab. 2006, 91, 3718–3724. [Google Scholar] [CrossRef]
- Saravanan, P.; Magee, L.A.; Banerjee, A.; Coleman, M.A.; Von Dadelszen, P.; Denison, F.; Farmer, A.; Finer, S.; Fox-Rushby, J.; Holt, R. Gestational diabetes: Opportunities for improving maternal and child health. Lancet Diabetes Endocrinol. 2020, 8, 793–800. [Google Scholar] [CrossRef]
- Lu, J.; Zhang, S.; Li, W.; Leng, J.; Wang, L.; Liu, H.; Li, W.; Zhang, C.; Qi, L.; Tuomilehto, J.; et al. Maternal Gestational Diabetes Is Associated With Offspring’s Hypertension. Am. J. Hypertens. 2019, 32, 335–342. [Google Scholar] [CrossRef] [Green Version]
- Seeland, U.; Nemcsik, J.; Lønnebakken, M.T.; Kublickiene, K.; Schluchter, H.; Park, C.; Pucci, G.; Mozos, I.; Bruno, R.M. Sex and Gender Aspects in Vascular Ageing—Focus on Epidemiology, Pathophysiology, and Outcomes. Heart Lung Circ. 2021, 30, 1637–1646. [Google Scholar] [CrossRef]
- Dall, T.M.; Yang, W.; Gillespie, K.; Mocarski, M.; Byrne, E.; Cintina, I.; Beronja, K.; Semilla, A.P.; Iacobucci, W.; Hogan, P.F. The Economic Burden of Elevated Blood Glucose Levels in 2017: Diagnosed and Undiagnosed Diabetes, Gestational Diabetes Mellitus, and Prediabetes. Diabetes Care 2019, 42, 1661–1668. [Google Scholar] [CrossRef] [Green Version]
- Alawadi, F.; Abusnana, S.; Afandi, B.; Aldahmani, K.M.; Alhajeri, O.; Aljaberi, K.; Alkaabi, J.; Almadani, A.; Bashier, A.; Beshyah, S.A.; et al. Emirates Diabetes Society Consensus Guidelines for the Management of Type 2 Diabetes Mellitus—2020. Dubai Diabetes Endocrinol. J. 2020, 26, 1–20. [Google Scholar] [CrossRef]
- Zhu, Y.; Zhang, C. Prevalence of Gestational Diabetes and Risk of Progression to Type 2 Diabetes: A Global Perspective. Curr. Diab. Rep. 2016, 16, 7. [Google Scholar] [CrossRef]
- Al-Rifai, R.H.; Abdo, N.M.; Paulo, M.S.; Saha, S.; Ahmed, L.A. Prevalence of Gestational Diabetes Mellitus in the Middle East and North Africa, 2000-2019: A Systematic Review, Meta-Analysis, and Meta-Regression. Front. Endocrinol. 2021, 12, 668447. [Google Scholar] [CrossRef]
- Agarwal, M.M.; Dhatt, G.S.; Shah, S.M. Gestational diabetes mellitus: Simplifying the international association of diabetes and pregnancy diagnostic algorithm using fasting plasma glucose. Diabetes Care 2010, 33, 2018–2020. [Google Scholar] [CrossRef] [Green Version]
- Baker, D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [Green Version]
- Cavanaugh, K.L. Health literacy in diabetes care: Explanation, evidence and equipment. Diabetes Manag. 2011, 1, 191–199. [Google Scholar] [CrossRef] [Green Version]
- Bhowmik, B.; Afsana, F.; Ahmed, T.; Siddiquee, T.; Ahmed, T.; Pathan, F.; Mahtab, H.; Khan, A.K.A. Evaluation of knowledge regarding gestational diabetes mellitus: A Bangladeshi study. Public Health 2018, 161, 67–74. [Google Scholar] [CrossRef]
- Draffin, C.R.; Alderdice, F.A.; McCance, D.R.; Maresh, M.; Harper Md Consultant Physician, R.; McSorley, O.; Holmes, V.A. Exploring the needs, concerns and knowledge of women diagnosed with gestational diabetes: A qualitative study. Midwifery 2016, 40, 141–147. [Google Scholar] [CrossRef] [Green Version]
- Thomas, S.; Pienyu, R.; Rajan, S.K. Awareness and Knowledge About Gestational Diabetes Mellitus Among Antenatal Women. Psychol. Community Health 2020, 8, 12. [Google Scholar] [CrossRef]
- Gastrich, M.; Peck, S.; Janevic, T.; Bachmann, G.; Lotwala, N.; Siyam, A. Gestational diabetes mellitus: An educational opportunity Article points. J. Diabetes Nurs. 2013, 17, 220–224. [Google Scholar]
- Lis-Kuberka, J.; Orczyk-Pawiłowicz, M. Polish Women Have Moderate Knowledge of Gestational Diabetes Mellitus and Breastfeeding Benefits. Int. J. Environ. Res Public Health 2021, 18, 409. [Google Scholar] [CrossRef]
- Alharthi, A.S.; Althobaiti, K.A.; Alswat, K.A. Gestational Diabetes Mellitus Knowledge Assessment among Saudi Women. Open Access Maced. J. Med. Sci. 2018, 6, 1522–1526. [Google Scholar] [CrossRef] [Green Version]
- Elmekresh, A. Gestational diabetes awareness in women of childbearing age in Sharjah. Glob. J. Obes. Diabetes Metab. Syndr. 2017, 4, 51–53. [Google Scholar] [CrossRef] [Green Version]
- Byakwaga, E.; Sekikubo, M.; Nakimuli, A. Level of and factors associated with awareness of gestational diabetes mellitus among pregnant women attending antenatal care at Kawempe National Referral Hospital: A cross sectional study. BMC Pregnancy Childbirth 2021, 21, 467. [Google Scholar] [CrossRef]
- Carolan, M.; Steele, C.; Margetts, H. Knowledge of gestational diabetes among a multi-ethnic cohort in Australia. Midwifery 2010, 26, 579–588. [Google Scholar] [CrossRef] [Green Version]
- Borgen, I.; Garnweidner-Holme, L.M.; Jacobsen, A.F.; Fayyad, S.; Cvancarova Småstuen, M.; Lukasse, M. Knowledge of gestational diabetes mellitus at first consultation in a multi-ethnic pregnant population in the Oslo region, Norway—A cross-sectional study. Ethn. Health 2019, 27, 209–222. [Google Scholar] [CrossRef]
- Salhi, A.A.; Intern, M.; Alshahrani, M.S.; Alyamin, M.M.; Hamdi, W.A.; Alyami, S.R.; Almagbool, A.S.; Almoqati, N.H.; Almoqati, S.H.; Al-Saaed, E.A.A.N.; et al. Assessment of the knowledge of pregnant women regarding the effects of GDM on mothers and neonates at a Maternal and Children hospital in Najran, Saudi Arabia. IJMDC 2019, 3, 370–375. [Google Scholar] [CrossRef]
- Ogu, R.N.; Maduka, O.; Agala, V.; Alamina, F.; Adebiyi, O.; Edewor, U.; Porbeni, I.; Abam, C. Gestational Diabetes Mellitus Knowledge Among Women of Reproductive Age in Southern Nigeria: Implications for Diabetes Education. Int. Q. Community Health Educ. 2020, 40, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Shriraam, V.; Rani, M.A.; Sathiyasekaran, B.W.; Mahadevan, S. Awareness of gestational diabetes mellitus among antenatal women in a primary health center in South India. Indian J. Endocrinol. Metab. 2013, 17, 146–148. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.T.; McNamara, M.J.; Milot, A.S.; Halle, T.; Hair, E.C. The effects of father involvement during pregnancy on receipt of prenatal care and maternal smoking. Matern. Child Health J. 2007, 11, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Bhavadharini, B.; Deepa, M.; Nallaperumal, S.; Anjana, R.; Mohan, V. Knowledge about gestational diabetes mellitus amongst pregnant women in South Tamil Nadu. J. Diabetol. 2017, 8, 22–26. [Google Scholar] [CrossRef] [Green Version]
- Price, L.A.; Lock, L.J.; Archer, L.E.; Ahmed, Z. Awareness of Gestational Diabetes and its Risk Factors among Pregnant Women in Samoa. Hawaii J. Med. Public Health 2017, 76, 48–54. [Google Scholar]
- Hussain, Z.; Yusoff, Z.M.; Sulaiman, S.A. Evaluation of knowledge regarding gestational diabetes mellitus and its association with glycaemic level: A Malaysian study. Prim. Care Diabetes 2015, 9, 184–190. [Google Scholar] [CrossRef]
- Abdulrahman, M.; Tabatabaei, Z.; Maqbool, S.; Hafidh, K.; Husain, Z.S.; Al Raeesi, F.H.; Abo Sada, N.M.; Akbar, M.; Hubaishi, N.M.; Tahlak, M.A.R.; et al. A review of gestational diabetes mellitus management, risk factors, maternal and neonatal outcomes in two major maternity hospitals in the United Arab Emirates: A report from Dubai. J. Neonatal. Perinat. Med. 2020, 13, 555–562. [Google Scholar] [CrossRef]
- Alkaabi, J.; Almazrouei, R.; Zoubeidi, T.; Alkaabi, F.M.; Alkendi, F.R.; Almiri, A.E.; Sharma, C.; Souid, A.-K.; Ali, N.; Ahmed, L.A. Burden, associated risk factors and adverse outcomes of gestational diabetes mellitus in twin pregnancies in Al Ain, UAE. BMC Pregnancy Childbirth 2020, 20, 612. [Google Scholar] [CrossRef]
- Hashim, M.; Radwan, H.; Hasan, H.; Obaid, R.S.; Al Ghazal, H.; Al Hilali, M.; Rayess, R.; Chehayber, N.; Mohamed, H.J.J.; Naja, F. Gestational weight gain and gestational diabetes among Emirati and Arab women in the United Arab Emirates: Results from the MISC cohort. BMC Pregnancy Childbirth 2019, 19, 463. [Google Scholar] [CrossRef]
- Roessner, V. Large sample size in child and adolescent psychiatric research: The way of salvation? Eur. Child Adolesc. Psychiatry 2014, 23, 1003–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Sociodemographic Characteristics | Total Population N * | n (%)/Median (IQR) | Knowledge Status | p-Value a | |
|---|---|---|---|---|---|
| Ever-Heard of GDM n = 462 (79.7%) | Never-Heard of GDM n = 118 (20.3%) | ||||
| Age (years) | 580 | 20.0 (4.0) | 20.0 (4.0) | 20.0 (4.0) | 0.483 |
| Weight (kg) | 554 | 58.0 (17.0) | 58.0 (18.0) | 58.5 (16.0) | 0.553 |
| Height (m) | 558 | 1.6 (0.1) | 1.6 (0.1) | 1.6 (0.1) | 0.592 |
| BMI (kg/m2) | 551 | 22.9 (6.1) | 22.9 (6.4) | 22.5 (5.3) | 0.409 |
| Program | 580 | ||||
| Undergraduate | 496 (85.5) | 396 (79.8) | 100 (20.2) | ||
| Postgraduate | 84 (14.5) | 66 (78.6) | 18 (21.4) | 0.071 | |
| Marital status | 580 | ||||
| Single | 506 (87.2) | 397 (78.5) | 109 (21.5) | ||
| Married | 74 (12.8) | 65 (87.8) | 9 (12.2) | 0.061 | |
| Working status | 580 | ||||
| Yes | 50 (8.6) | 39 (78.0) | 11 (22.0) | ||
| No | 530 (91.4) | 423 (79.8) | 107 (20.2) | 0.093 | |
| Anyone in your home working in the Health Sector | 580 | ||||
| Yes | 111 (19.1) | 85 (76.6) | 26 (23.4) | ||
| No | 469 (80.9) | 377 (80.4) | 92 (19.6) | 0.370 | |
| Family history of diabetes | 580 | ||||
| Yes | 303 (52.2) | 246 (81.2) | 57 (18.8) | ||
| No | 277 (47.8) | 216 (78.0) | 61 (22.0) | 0.337 | |
| Sociodemographic Characteristics | Total Population N * | n (%)/Median (IQR) | Knowledge Status | p-Value a | |
|---|---|---|---|---|---|
| Ever Heard of GDM n = 73 (47.1%) | Never Heard of GDM n = 82 (52.9%) | ||||
| Age (years) | 155 | 21.0 (7.0) | 22.0 (8.0) | 21.0 (4.0) | 0.019 |
| Weight (kg) Mean (SD) | 144 | 77.2 (16.2) | 78.3 (16.4) | 76.3 (16.0) | 0.464 b |
| Height (m) | 126 | 1.7 (0.1) | 1.7 (0.1) | 1.7 (0.1) | 0.136 |
| BMI (kg/m2) | 126 | 25.4 (6.5) | 25.5 (7.0) | 25.2 (5.8) | 0.254 |
| Program | 155 | ||||
| Undergraduate | 109 (70.3) | 45 (41.3) | 64 (58.7) | ||
| Postgraduate | 46 (26.7) | 28 (60.9) | 18 (39.1) | 0.026 | |
| Marital status | 155 | ||||
| Single | 123 (79.4) | 53 (43.1) | 70 (56.9) | ||
| Married | 32 (20.6) | 20 (62.5) | 12 (37.5) | 0.050 | |
| Working status | 155 | ||||
| Yes | 39 (25.2) | 22 (56.4) | 17 (43.6) | ||
| No | 116 (74.8) | 51 (44.0) | 65 (56.0) | 0.178 | |
| Anyone in your home working in the Health Sector | 155 | ||||
| Yes | 29 (18.7) | 15 (51.7) | 14 (48.3) | ||
| No | 126 (81.3) | 58 (46.0) | 68 (54.0) | 0.580 | |
| Family history of diabetes | 155 | ||||
| Yes | 66 (42.6) | 37 (56.1) | 29 (43.9) | ||
| No | 89 (57.4) | 36 (40.5) | 53 (59.5) | 0.054 | |
| Knowledge Levels | ||||||
|---|---|---|---|---|---|---|
| Students’ Characteristics | Total Population N * | %/Median (IQR) | Poor GDM Knowledge b 115 (24.0%) % | Fair GDM Knowledge b 281 (58.5%) % | Good GDM Knowledge b 161 (17.5%) % | p-Value a |
| Age (years) | 480 | 21.0 (3.0) | 21.0 (3.0) | 21.0 (4.0) | 21.0 (5.0) | 0.170 |
| Weight (kg) | 457 | 60.0 (21.0) | 60.0 (20.0) | 59.0 (21.0) | 65.0 (20.0) | 0.185 |
| Height (m) | 452 | 1.6 (0.1) | 1.6 (0.1) | 1.6 (0.1) | 1.6 (0.1) | 0.440 |
| BMI (kg/m2) | 449 | 23.3 (6.9) | 23.1 (7.1) | 23.1 (7.0) | 24.4 (6.4) | 0.384 |
| Gender | 480 | |||||
| Male | 13.8 | 31.8 | 56.1 | 12.1 | ||
| Female | 86.2 | 22.7 | 58.9 | 18.4 | 0.190 | |
| Program | 480 | |||||
| Undergraduate | 81.7 | 24.2 | 59.7 | 16.1 | ||
| Postgraduate | 18.3 | 22.7 | 53.4 | 23.9 | 0.218 | |
| Marital status | 480 | |||||
| Single | 84.6 | 24.4 | 60.8 | 14.8 | ||
| Married | 15.4 | 21.6 | 46.0 | 32.4 | 0.001 | |
| Working status | 480 | |||||
| Yes | 11.7 | 23.2 | 55.4 | 21.4 | ||
| No | 88.3 | 24.1 | 58.9 | 17.0 | 0.710 | |
| Anyone in your home working in the Health Sector | 480 | |||||
| Yes | 19.0 | 18.7 | 57.1 | 24.2 | ||
| No | 81.0 | 25.2 | 58.9 | 15.9 | 0.122 | |
| Family history of diabetes | 480 | |||||
| Yes | 53.8 | 20.9 | 62.0 | 17.1 | ||
| No | 46.2 | 27.5 | 54.5 | 18.0 | 0.187 | |
| Know someone who had GDM | 480 | |||||
| Yes | 65.6 | 20.3 | 59.1 | 20.6 | ||
| No | 34.4 | 30.9 | 57.6 | 11.5 | 0.006 | |
| Total GDM knowledge points (out of 12) | 480 | 6.0 (3.0) | 4.0 (2.0) | 7.0 (1.0) | 10.0 (1.0) | <0.001 |
| Students’ Characteristics | Adjusted OR (95% CI) * | |
|---|---|---|
| Marital status | Single | ref |
| Married | 1.82 (1.10–3.03) a | |
| Know someone who had GDM | No | ref |
| Yes | 1.78 (1.23–2.60) a | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bashir, M.M.; Ahmed, L.A.; Alshamsi, M.R.; Almahrooqi, S.; Alyammahi, T.; Alshehhi, S.A.; Alhammadi, W.I.; Alhosani, H.A.; Alhammadi, F.H.; Al-Rifai, R.H.; et al. Gestational Diabetes Mellitus: A Cross-Sectional Survey of Its Knowledge and Associated Factors among United Arab Emirates University Students. Int. J. Environ. Res. Public Health 2022, 19, 8381. https://doi.org/10.3390/ijerph19148381
Bashir MM, Ahmed LA, Alshamsi MR, Almahrooqi S, Alyammahi T, Alshehhi SA, Alhammadi WI, Alhosani HA, Alhammadi FH, Al-Rifai RH, et al. Gestational Diabetes Mellitus: A Cross-Sectional Survey of Its Knowledge and Associated Factors among United Arab Emirates University Students. International Journal of Environmental Research and Public Health. 2022; 19(14):8381. https://doi.org/10.3390/ijerph19148381
Chicago/Turabian StyleBashir, Maryam M., Luai A. Ahmed, Meera R. Alshamsi, Sara Almahrooqi, Taif Alyammahi, Shooq A. Alshehhi, Waad I. Alhammadi, Hind A. Alhosani, Fatima H. Alhammadi, Rami H. Al-Rifai, and et al. 2022. "Gestational Diabetes Mellitus: A Cross-Sectional Survey of Its Knowledge and Associated Factors among United Arab Emirates University Students" International Journal of Environmental Research and Public Health 19, no. 14: 8381. https://doi.org/10.3390/ijerph19148381
APA StyleBashir, M. M., Ahmed, L. A., Alshamsi, M. R., Almahrooqi, S., Alyammahi, T., Alshehhi, S. A., Alhammadi, W. I., Alhosani, H. A., Alhammadi, F. H., Al-Rifai, R. H., & Al-Maskari, F. (2022). Gestational Diabetes Mellitus: A Cross-Sectional Survey of Its Knowledge and Associated Factors among United Arab Emirates University Students. International Journal of Environmental Research and Public Health, 19(14), 8381. https://doi.org/10.3390/ijerph19148381






