Validation of Content for an App for Caregivers of Stroke Patients through the Delphi Method
Abstract
1. Introduction
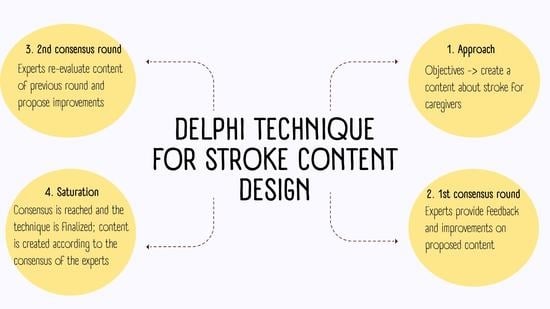
2. Materials and Methods
2.1. Sample/Participants
2.2. Data Collection
2.3. Data Analysis
2.4. Validity and Reliability/Rigour
2.5. Ethical Considerations
3. Results
3.1. Group of Experts
3.2. Development of the Delphi Technique
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- SEN.es. Spanish Society of Neurology. Recovery 18 October 2021. Available online: https://www.sen.es/ (accessed on 18 November 2021).
- Tejada Meza, H.; Campello Morer, I.; Bestué Cardiel, M.; Fernández Sanz, A.; Tejero Juste, C.; Muñoz Farjas, E.; Hernando Quintana, N.; Jarauta Lahoz, L.; Clavo Pérez, L.M.; Cruz Velásquez, G.; et al. Epidemiology and characteristics of ischaemic stroke in young adults in Aragon. Neurology 2019. [Google Scholar] [CrossRef] [PubMed]
- Bierhals, C.C.B.K.; Low, G.; Paskulin, L.M.G. Quality of life perceptions of family caregivers of older adults stroke survivors: A longitudinal study. Appl. Nurs. Res. ANR 2019, 47, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Caqueo-Urízar, A.; Urzúa, M. Quality of Life: A Theoretical Review of the Concept. EndNote Click, Recovery 18 October 2021. Available online: https://click.endnote.com/viewer?doi=10.4067%2Fs0718-48082012000100006&token=WzM1MTQ1MjYsIjEwLjQwNjcvczA3MTgtNDgwODIwMTIwMDAxMDAwMDYiXQ.BEAxe33dFRVUCTTz9aA9EHNjvZk (accessed on 18 September 2021).
- Andrades-González, I.; Romero-Franco, N.; Molina-Mula, J. e-Health as a tool to improve the quality of life of informal caregivers dealing with stroke patients: Systematic review with meta-analysis. J. Nurs. Scholarsh. 2021, 53, 790–802. [Google Scholar] [CrossRef] [PubMed]
- Woodford, J.; Farrand, P.; Watkins, E.R.; LLewellyn, D.J. Full article: “I Don’t Believe in Leading a Life of My Own, I Lead His Life”: A Qualitative Investigation of Difficulties Experienced by Informal Caregivers of Stroke Survivors Experiencing Depressive and Anxious Symptoms. 2017. Recovery 18 October 2021. Available online: https://www.tandfonline.com/doi/full/10.1080/07317115.2017.1363104 (accessed on 18 November 2021).
- Hernández-García, F.; Robaina Castillo, J. Guide for the Use of Delphi Methodology in the Testing Stages of Educational Software Finished Products; Spanish Society of Geriatrics and Gerontology: Madrid, Spain, 2017; pp. 26–31. [Google Scholar]
- Boonen, A.; van Berkel, M.; Kirchberger, I.; Cieza, A.; Stucki, G.; van der Heijde, D. Aspects relevant for functioning in patients with ankylosing spondylitis according to the health professionals: A Delphi study with the ICF as reference. Rheumatology 2009, 48, 997–1002. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nikolaus, S.; Bode, C.; Taal, E.; van der Laar, M.A.F.J. Expert evaluations of fatigue questionnaires used in rheumatoid arthritis: A Delphi study among patients, nurses and rheumatologists in the Netherlands. Clin. Exp. Rheumatol. 2012, 30, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Palomino-Camargo, C.; González-Muñoz, Y.; Pérez-Sira, E.; Aguilar, V.H. Delphi methodology in food safety management and prevention of foodborne diseases. Peruv. J. Exp. Med. Public Health 2018, 35, 483–490. [Google Scholar] [CrossRef]
- Martínez-Ezquerro, J.D.; Ruiz-Cejudo, S.M.; Bustamante-Fuentes, A.; Díaz-Badillo, Á.; García-Oropesa, E.M.; López-Sosa, E.B.; Martínez-López, Y.E.; Moctezuma-Chávez, Ó.O.; Nava-González, E.J.; Perales-Torres, A.L.; et al. Expert consensus in times of COVID-19: Applications of the Delphi method in health. Surg. Surg. 2021, 89, 120–129. [Google Scholar] [CrossRef]
- Altuna Azkargota, M.; Arenaza Basterrechea, N.; Barrientos Herrero, R.; Beistegui Alejandre, I.; Belarrinaga Oyanguren, B.; Carbajal de la Red, M.; Delgado González, J.; Domaica Aguinaco, I.; Gómez de Balugera Fernández de Trocóniz, A.; Isidro Diego, B.S.; et al. Care Guide for Stroke Patients and Carers. 2018. Available online: http://www.osiaraba.eus/infopacientes/documentos/servicios/neurologia/hojasinfo/cas/Gu%C3%ADa%20de%20cuidados%20para%20pacientes%20con%20ICTUS%20y%20personas%20cuidadoras.pdf (accessed on 18 September 2021).
- Ferré i Grau, C.; Rodero Sánchez, V.; Cid Buera, D.; Vives Relats, C.; Aparicio Casals, M.R. Nursing Care Guide: Caring for the Caregiver in Primary Care; Spanish Society of Geriatrics and Gerontology: Madrid, Spain, 2011. [Google Scholar]
- García Antón, M.; Ángeles; Campos Dompedro, J.R. Skills Manual for Family Carers of Dependent Elderly People; Spanish Society of Geriatrics and Gerontology: Madrid, Spain, 2013. [Google Scholar]
- Sierra Díaz, A.; Bravo Piqueras, F. Caregiver’s Manual. 2021. Available online: https://portal.guiasalud.es/wpcontent/uploads/2018/12/GPC_466_Ictus_AP_Lain_Entr_compl.pdf (accessed on 18 November 2021).
- García, L.; Fernández, S.J. Procedure for the application of creative work in a group of experts. Energy Eng. 2008, XXIX, 46–50. [Google Scholar]
- Almenara, C.J.; Osuna, B.J. The use of expert judgement for ict evaluation: The expert competence quotient. J. Pedagog. 2013, 65, 25–38. [Google Scholar]
- Guimaraes Marcelino, C.A.; da Cruz, D.M.; Rueda, L.J. The efficacy of telephone use to assist and improve the wellbeing of family caregivers of persons with chronic diseases: A systematic review protocol. JBI Evid. Synth. 2013, 11, 330–342. [Google Scholar] [CrossRef]
- Corry, M.; Neenan, K.; Brabyn, S.; Sheaf, G.; Smith, V. Telephone interventions, delivered by healthcare professionals, for providing education and psychosocial support for informal caregivers of adults with diagnosed illnesses. Cochrane Database Syst. Rev. 2019, 5, CD012533. [Google Scholar] [CrossRef] [PubMed]
- Romero Guevara, S.L.; Villamizar Carvajal, B.; Rueda Díaz, L.J. Telephone support: An intervention strategy for family caregivers of people with chronic illness. J. Univ. Ind. Santander Health 2011, 43, 191–201. [Google Scholar]
- Beaver, K.; Wilson, C.; Procter, D.; Sheridan, J.; Towers, G.; Heath, J.; Susnerwala, S.; Luker, K. Colorectal cancer follow-up: Patient satisfaction and amenability to telephone after care. Eur. J. Oncol. Nurs. Off. J. Eur. Oncol. Nurs. Soc. 2011, 15, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Chi, N.-C.; Demiris, G. A systematic review of telehealth tools and interventions to support family caregivers. J. Telemed. Telecare 2015, 21, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Martínez Moreno, J.; Martínez Moreno, O.A.; Mud Castelló, S.; Mud Castelló, F.; Moreno Rodriguez, L.; Martínez Garví, O. Analysis of the quality and security of information from mobile applications in tertiary prevention. Community Pharm. 2015, 7, 23–26. [Google Scholar] [CrossRef]
- WHO. WHO Guideline: Recommendations on Digital Interventions for Health System Strengthening; WHO—World Health Organization: Geneva, Switzerland, Recovery 18 October 2021; Available online: https://www.who.int/reproductivehealth/publications/digital-interventions-health-system-strengthening/en/ (accessed on 18 November 2021).
- Boudreaux, E.D.; Waring, M.E.; Hayes, R.B.; Sadasivam, R.S.; Mullen, S.; Pagoto, S. Evaluating and selecting mobile health apps: Strategies for healthcare providers and healthcare organizations. Transl. Behav. Med. 2014, 4, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Crow, R.; Gage, H.; Hampson, S.; Hart, J.; Kimber, A.; Storey, L.; Thomas, H. The measurement of satisfaction with healthcare: Implications for practice from a systematic review of the literature. Health Technol. Assess. 2002, 6, 1–244. [Google Scholar] [CrossRef] [PubMed]
| Categories | Content |
|---|---|
| Disease (stroke) | In this first category, they are given detailed information about stroke, how to recognize it, prevention and risk factors, aftereffects, rehabilitation, and the activities that the nurse will be limited from doing after it. |
| Caregivers | The caregivers’ category discusses the concept of informal caregiving as well as the changes and consequences of taking on such a role. |
| Tips | There is a decalogue of tips for caregivers and an explanation that reinforces these tips in this class: asking for help, taking care of themselves, and learning new communication skills. |
| Resources | The term “Resources” refers to the different types of social resources available to informal caregivers and the patients they care for. These aids are intended to improve the population’s quality of life. Dependency law, Tele-assistance, and residences are a few examples. |
| Associations | The associations’ section includes a list of national and local associations of informal caregivers. They are also asked to contribute new partnerships that are not on the list. |
| Incorporating videos | They are given a link to watch videos on mobilization techniques and physical exercise. We are also looking for fresh ideas. |
| Participant No. | Sex | Education | Occupation | Years of Experience |
|---|---|---|---|---|
| 1 | Female | Degree in Nursing | Inpatient neurology nurse | 15 |
| 2 | Male | Degree in Nursing | Inpatient neurology nurse | >5 |
| 3 | Female | Degree in Nursing | Inpatient neurology nurse | 8 |
| 4 | Female | Degree in Nursing | Inpatient neurology nurse | >5 |
| 5 | Female | Degree in Nursing | Inpatient neurology nurse | 10 |
| 6 | Male | Degree in Nursing and Graduate in Psychology | Primary Care Nurse | 16 |
| 7 | Female | Degree in Nursing | Inpatient neurology nurse | 12 |
| 8 | Female | Degree in Nursing | Nurse Case Manager | 19 |
| 9 | Female | Degree in Nursing | Nurse in critical care unit | 10 |
| 10 | Male | Degree in Social Education | Director General for Dependency Care | 16 |
| 11 | Female | Degree in Nursing | Sub-Directorate for Chronic Care and Socio-Sanitary Coordination | 30 |
| 12 | Female | Degree in Nursing and Graduate in Economics | Sub-Directorate for Chronic Care and Socio-Sanitary Coordination | 21 |
| 13 | Female | Degree in Medicine | Inpatient neurologist | 15 |
| Experts | Kc * | Ka ** | K *** | Level of Competence |
|---|---|---|---|---|
| 1 | 0.8 | 0.5 | 0.65 | Medium |
| 2 | 0.7 | 0.5 | 0.6 | Medium |
| 3 | 0.6 | 0.5 | 0.55 | Medium |
| 4 | 0.7 | 0.8 | 0.75 | Medium |
| 5 | 0.5 | 0.5 | 0.5 | Medium |
| 6 | 0.5 | 0.5 | 0.5 | Medium |
| 7 | 0.7 | 0.8 | 0.75 | Medium |
| 8 | 0.6 | 0.8 | 0.7 | Medium |
| 9 | 0.7 | 0.8 | 0.75 | Medium |
| 10 | 0.9 | 0.8 | 0.8 | High |
| 11 | 0.8 | 0.7 | 0.75 | Medium |
| 12 | 0.7 | 0.8 | 0.75 | Medium |
| 13 | 0.9 | 0.8 | 0.85 | High |
| Aspects | Very Adequate | Quite Adequate | Adequate | Not Adequate | Sum | Average | N-P |
|---|---|---|---|---|---|---|---|
| Stroke | 1.02 | 1.02 | 3.09 | 3.09 | 8.22 | 2.055 | −0.3 |
| Caregivers | 0.73 | 1.02 | 3.09 | 3.09 | 7.93 | 1.9825 | −0.23 |
| Tips | 0.923 | 1.42 | 3.09 | 3.09 | 8.523 | 2.1307 | −0.38 |
| Resources | 1.42 | 1.02 | 1.42 | 3.09 | 6.95 | 1.7375 | 0.01 |
| Associations | 0.923 | 3.09 | 3.09 | 3.09 | 10.193 | 2.5482 | −0.798 |
| Videos | 1.42 | 3.09 | 3.09 | 3.09 | 10.69 | 2.6725 | −0.92 |
| Sum | 6.436 | 10.66 | 16.87 | 18.54 | 52.506 | ||
| Cut-off points | 1.07 | 1.77 | 2.81 | 3.09 | N = 1.7502 |
| Aspects | Mean | Standard Deviation | Coefficient of Variation |
|---|---|---|---|
| Stroke | 4.69 | 0.75 | 0.16 |
| Caregivers | 4.61 | 0.77 | 0.16 |
| Tips | 4.85 | 0.55 | 0.11 |
| Resources | 4.61 | 0.96 | 0.2 |
| Associations | 4.92 | 0.27 | 0.05 |
| Videos | 4.84 | 0.37 | 0.07 |
| Categories | Suggestions from Participants | Improvements Made after the First Round |
|---|---|---|
| Stroke |
|
|
| Caregivers |
|
|
| Tips |
|
|
| Resources |
|
|
| Associations |
|
|
| Videos |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andrades-González, I.; Molina-Mula, J. Validation of Content for an App for Caregivers of Stroke Patients through the Delphi Method. Int. J. Environ. Res. Public Health 2022, 19, 7523. https://doi.org/10.3390/ijerph19127523
Andrades-González I, Molina-Mula J. Validation of Content for an App for Caregivers of Stroke Patients through the Delphi Method. International Journal of Environmental Research and Public Health. 2022; 19(12):7523. https://doi.org/10.3390/ijerph19127523
Chicago/Turabian StyleAndrades-González, Ismael, and Jesús Molina-Mula. 2022. "Validation of Content for an App for Caregivers of Stroke Patients through the Delphi Method" International Journal of Environmental Research and Public Health 19, no. 12: 7523. https://doi.org/10.3390/ijerph19127523
APA StyleAndrades-González, I., & Molina-Mula, J. (2022). Validation of Content for an App for Caregivers of Stroke Patients through the Delphi Method. International Journal of Environmental Research and Public Health, 19(12), 7523. https://doi.org/10.3390/ijerph19127523