The Mediating Role of Compassion between Social Job Resources, and Healthy Healthcare Professionals: A Cross-Sectional Study with Gender Perspective
Abstract
:1. Introduction
2. Theoretical Framework
2.1. Compassion towards Others as a Personal Resource
2.2. The Mediating Role of Compassion towards Others between Social Job Resources and Healthy Employees
2.3. The Mediating Role of Compassion towards Others between Social Job Resources, Healthy Organisational Outcomes and Productive Workers
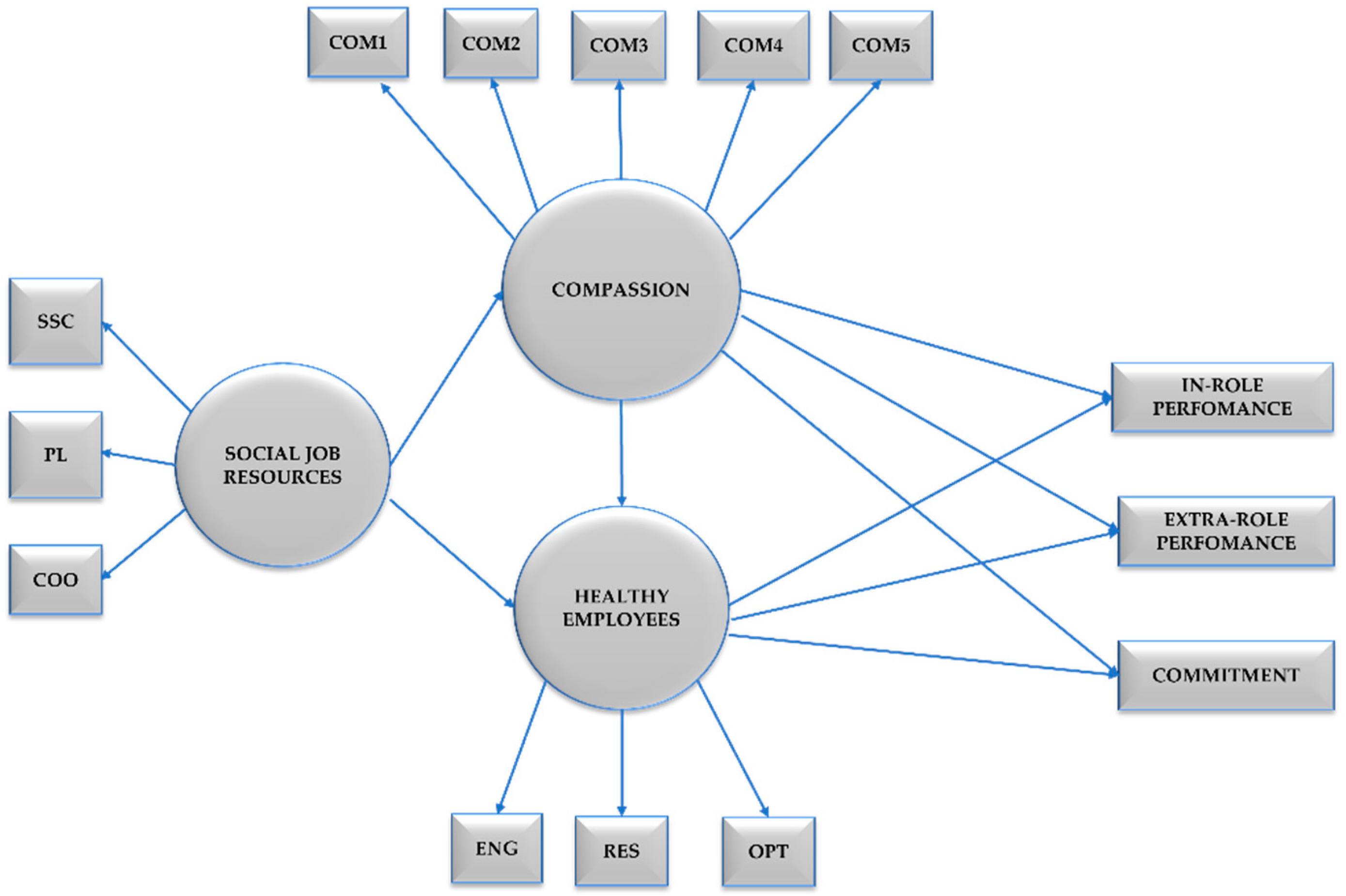
2.4. The Current Study
3. Materials and Methods
3.1. Participants
3.2. Instruments
- Compassion towards others was measured using a brief adaptation of the Compassion Scale [68,69]. Five items were chosen from the original scale (since, after conducting the analyses, they were the ones with the best factor scores), distributed between self-kindness, common humanity, mindfulness, and non-judgement/forgiveness. The items are scored on a seven-point frequency rating scale ranging from 0 (never) to 6 (always). Sample items include “If I see that someone is having difficulties, I try to help” (kindness), “I try not to judge others when they make mistakes or are wrong” (non-judgement/forgiveness), “I think everyone feels sad sometimes, it is part of being human” (common humanity), “I usually listen patiently when people tell me about their problems” (mindfulness). Cronbach’s Alpha (α = 0.65), and McDonald’s Omega (ω = 0.65): the Cronbach’s Alpha is moderate, so it is above the acceptable limit [70], which is why the decision was made not to remove the item that scored less, as it would remain with two of the three constructs that make up Compassion.
- Social Job Resources were measured using the HERO questionnaire subscale by the same name including social support climate, positive leadership, and coordination. Each of these items was represented by a single item, where each of these single items is the mean of the HERO subscale [15,16]. Participants answered using a seven-point frequency type scale with scores from 0 (never) to 6 (always). Sample items include “Degree to which your supervisor considers the needs of your service/care unit, recognising the effort and achievement of goals of the service/care unit” (positive leadership), “Degree to which you feel supported by your colleagues and supervisor personally and professionally” (social support climate) and “Degree to which you are coordinated with your work team, in order to respond to work situations” (coordination). (Cronbach’s Alpha (α = 0.80), and McDonald’s Omega (ω = 0.81))
- Healthy Employees were measured using the HERO questionnaire subscale by the same name including engagement, resilience, self-efficacy, and optimism. Each of these items was represented by a single item, where each of these single items is the mean of the HERO subscale [15,16]. Participants answered using a seven-point frequency with scores from 0 (never) to 6 (always). Sample items include “Degree to which you feel immersed, full of energy and dedicated to your work, creating a positive climate of fulfilment and hope” (engagement), “Degree to which you feel capable of emerging stronger after facing adversity and failures at work” (resilience), and “Degree to which you generally expect the best in difficult times, you are optimistic about the future and in general, you expect more good things to happen than bad” (optimism). (Cronbach’s alpha (α = 0.81), and McDonald’s omega (ω = 0.81))
- Healthy Organisational Outcomes were measured using items from the HERO questionnaire subscale by the same name including a single item each for commitment, extra-role, and in-role performance [15,16]. Each one of these elements was represented by a single item, this was due to factor loadings where they fitted best as observed variables. Participants answered using a seven-point frequency type scale with scores from 0 (never) to 6 (always). Sample items include “Degree to which your work tasks are carried out and fulfilled” (in-role performance), “Degree to which tasks that exceed what is prescribed by your work are performed” (extra-role performance), “Degree to which you feel committed to the health centre and its outcomes, how proud you feel to belong there” (commitment).
3.3. Data Analyses
4. Results
4.1. Multiple Analyses of Variance (MANOVA)
4.2. Descriptive Analyses
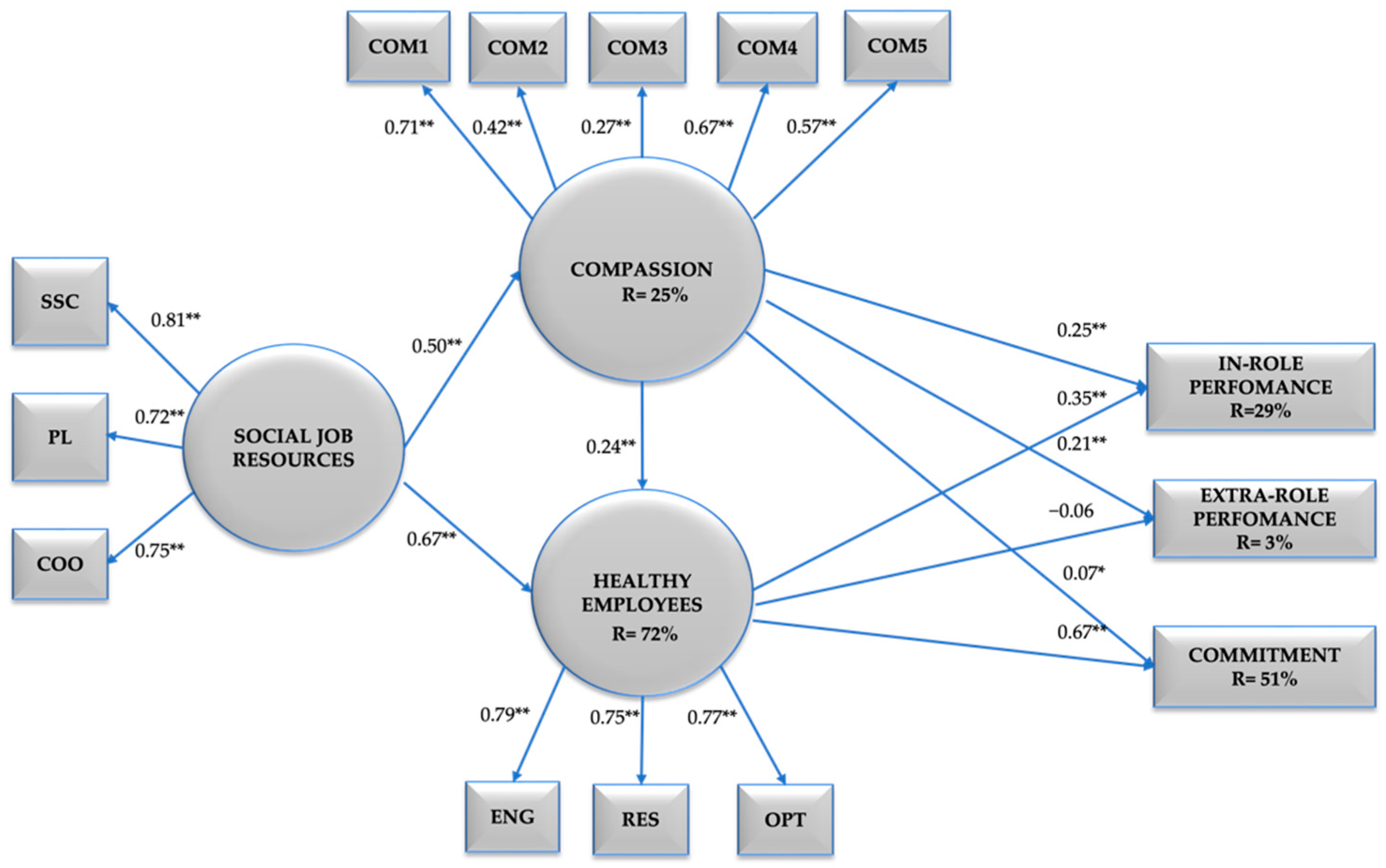
4.3. Structural Equation Modelling Analyses
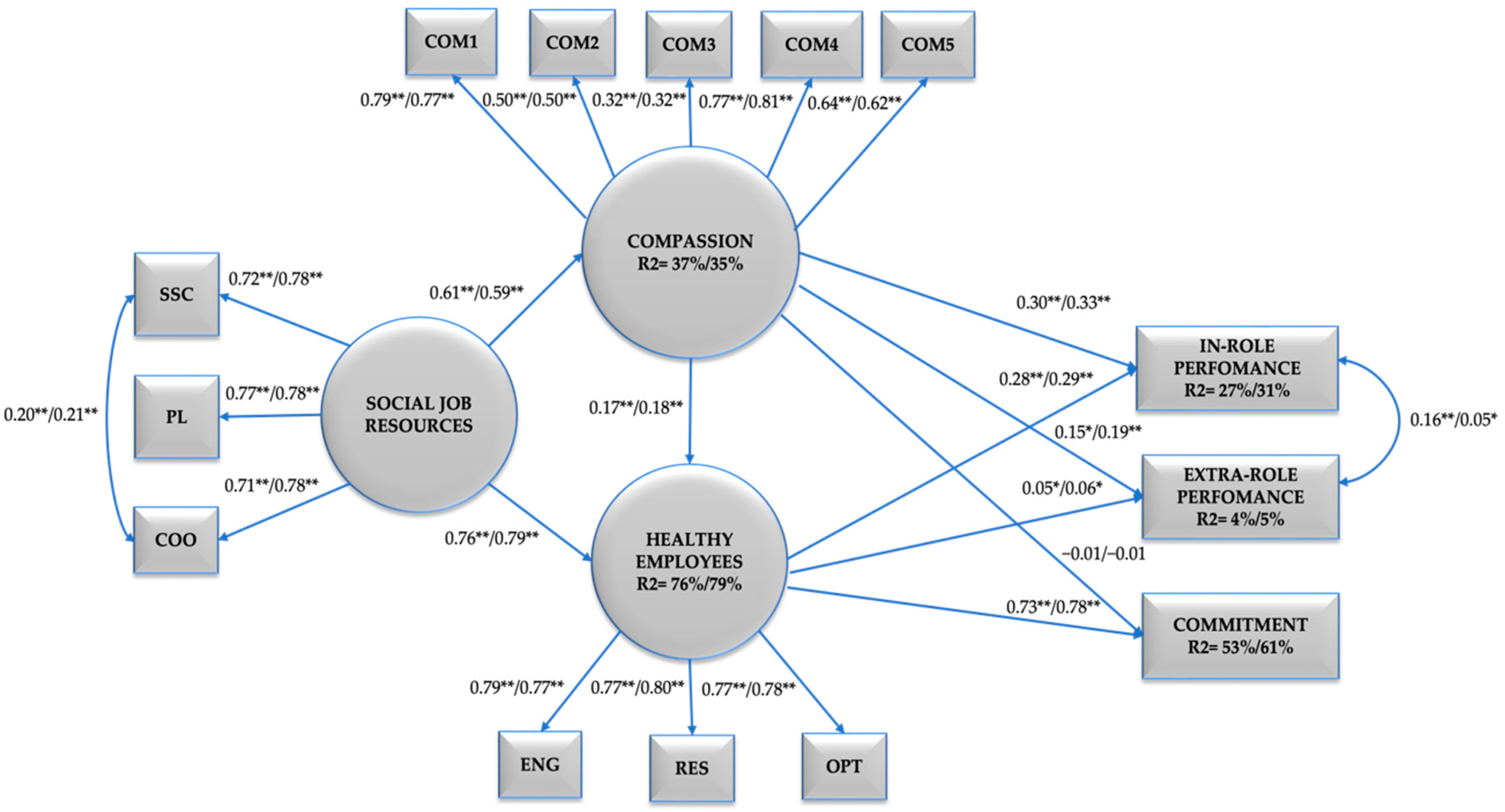
4.4. Multiple-Group Configural Factor Analyses
5. Discussion
6. Conclusions
6.1. Theoretical Contributions
6.2. Practical Implications
6.3. Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Halifax, J. The Precious Necessity of Compassion. J. Pain Symptom Manag. 2011, 41, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Adriaenssens, J.; de Gucht, V.; Maes, S. Determinants and Prevalence of Burnout in Emergency Nurses: A Systematic Review of 25 Years of Research. Int. J. Nurs. Stud. 2015, 649–661. [Google Scholar] [CrossRef] [PubMed]
- Cameron, C.D.; Payne, B.K. Escaping Affect: How Motivated Emotion Regulation Creates Insensitivity to Mass Suffering. J. Personal. Soc. Psychol. 2011, 100, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rydon-Grange, M. Psychological Perspective on Compassion in Modern Healthcare Settings. J. Med. Ethics 2018, 44, 729–733. [Google Scholar] [CrossRef]
- Sinclair, S.; McClement, S.; Raffin-Bouchal, S.; Hack, T.F.; Hagen, N.A.; McConnell, S.; Chochinov, H.M. Compassion in Health Care: An Empirical Model. J. Pain Symptom Manag. 2016, 51, 193–203. [Google Scholar] [CrossRef] [Green Version]
- Schaufeli, W.B.; Taris, T.W. A Critical Review of the Job Demands-Resources Model: Implications for Improving Work and Health. In Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach; Springer: Dordrecht, The Netherlands, 2014; Volume 9789400756403, pp. 43–68. [Google Scholar] [CrossRef]
- Bakker, A.B.; Demerouti, E. Job Demands-Resources Theory: Taking Stock and Looking Forward. J. Occup. Health Psychol. 2017, 22, 273–285. [Google Scholar] [CrossRef]
- Xanthopoulou, D.; Bakker, A.B.; Demerouti, E.; Schaufeli, W.B. The Role of Personal Resources in the Job Demands-Resources Model. Int. J. Stress Manag. 2007, 14, 121–141. [Google Scholar] [CrossRef] [Green Version]
- Vink, J.; Ouweneel, E.; le Blanc, P. Psychological Resources for Engaged Employees: Psychological Capital in the Job Demands-Resources Model. Gedrag En Organ. 2011, 24, 101–120. [Google Scholar]
- van den Broeck, A.; Vansteenkiste, M.; de Witte, H.; Lens, W. Explaining the Relationships between Job Characteristics, Burnout, and Engagement: The Role of Basic Psychological Need Satisfaction. Work. Stress 2008, 22, 277–294. [Google Scholar] [CrossRef] [Green Version]
- Bramley, L.; Matiti, M. How Does It Really Feel to Be in My Shoes? Patients’ Experiences of Compassion within Nursing Care and Their Perceptions of Developing Compassionate Nurses. J. Clin. Nurs. 2014, 23, 2790–2799. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, P.; Choden, K. Mindful Compassion: Using the Power of Mindfulness and Compassion to Transform Our Lives; Hachette: London, UK, 2013. [Google Scholar]
- Mauno, S.; Ruokolainen, M.; Kinnunen, U.; de Bloom, J. Emotional Labour and Work Engagement among Nurses: Examining Perceived Compassion, Leadership and Work Ethic as Stress Buffers. J. Adv. Nurs. 2016, 72, 1169–1181. [Google Scholar] [CrossRef] [PubMed]
- Orellana-Rios, C.L.; Radbruch, L.; Kern, M.; Regel, Y.U.; Anton, A.; Sinclair, S.; Schmidt, S. Mindfulness and Compassion-Oriented Practices at Work Reduce Distress and Enhance Self-Care of Palliative Care Teams: A Mixed-Method Evaluation of an “on the Job” Program. BMC Palliat. Care 2017, 17, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salanova, M.; Llorens, S.; Cifre, E.; Martínez, I.M. We Need a Hero! Toward a Validation of the Healthy and Resilient Organization (HERO) Model. Group Organ. Manag. 2012, 37, 785–822. [Google Scholar] [CrossRef]
- Salanova, M.; Llorens, S.; Martínez, I.M. Organizaciones Saludables: Una Mirada Desde La Psicología Positiva, 1st ed.; Aranzadi: Toronto, ON, Canada, 2019. [Google Scholar]
- Keane, K. Gendering of Compassion in Organizations. Bachelor’s Thesis, University of Michigan, Ann Arbor, MI, USA, 2014. [Google Scholar]
- Grant, A.M.; Parker, S.K. 7 Redesigning Work Design Theories: The Rise of Relational and Proactive Perspectives. Acad. Manag. Ann. 2009, 3, 317–375. [Google Scholar] [CrossRef]
- Strauss, C.; Lever Taylor, B.; Gu, J.; Kuyken, W.; Baer, R.; Jones, F.; Cavanagh, K. What Is Compassion and How Can We Measure It? A Review of Definitions and Measures. Clin. Psychol. Rev. 2016, 15–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinclair, S.; Norris, J.M.; McConnell, S.J.; Chochinov, H.M.; Hack, T.F.; Hagen, N.A.; McClement, S.; Bouchal, S.R. Compassion: A Scoping Review of the Healthcare Literature Knowledge, Education and Training. BMC Palliat. Care 2016, 15, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baguley, S.I.; Dev, V.; Fernando, A.T.; Consedine, N.S. How Do Health Professionals Maintain Compassion Over Time? Insights From a Study of Compassion in Health. Front. Psychol. 2020, 11, 564554. [Google Scholar] [CrossRef]
- Leget, C.; Olthuis, G. Compassion as a Basis for Ethics in Medical Education. J. Med. Ethics 2007, 33, 617–620. [Google Scholar] [CrossRef] [Green Version]
- Frampton, S.B.; Guastello, S.; Lepore, M. Compassion as the Foundation of Patient-Centered Care: The Importance of Compassion in Action. J. Comp. Eff. Res. 2013, 443–455. [Google Scholar] [CrossRef]
- Chochinov, H.M. Dignity and the Essence of Medicine: The A, B, C, and D of Dignity Conserving Care. BMJ 2007, 335, 184–187. [Google Scholar] [CrossRef] [Green Version]
- Fogarty, L.A.; Curbow, B.A.; Wingard, J.R.; Mcdonnell, K.; Somerfield, M.R. Can 40 Seconds of Compassion Reduce Patient Anxiety? J. Clin. Oncol. 1999, 17, 371–379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eide, H.; Eide, T.; Rustøen, T.; Finset, A. Patient Validation of Cues and Concerns Identified According to Verona Coding Definitions of Emotional Sequences (VR-CoDES): A Video- and Interview-Based Approach. Patient Educ. Couns. 2011, 82, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Hanson, L.C.; Winzelberg, G. Research Priorities for Geriatric Palliative Care: Goals, Values, and Preferences. J. Palliat. Med. 2013, 16, 1175–1179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patel, S.; Pelletier-Bui, A.; Smith, S.; Roberts, M.B.; Kilgannon, H.J.; Trzeciak, S.; Roberts, B.W. Curricula and Methods for Physician Compassion Training: Protocol for a Systematic Review. BMJ Open. 2018, 8, e024320. [Google Scholar] [CrossRef] [Green Version]
- Sansó, N.; Galiana, L.; González, B.; Sarmentero, J.; Reynes, M.; Oliver, A.; Garcia-Toro, M. Differential Effects of Two Contemplative Practice-Based Programs for Health Care Professionals. Psychosoc. Interview 2019, 28, 131–138. [Google Scholar] [CrossRef] [Green Version]
- Scarlet, J.; Altmeyer, N.; Knier, S.; Harpin, R.E. The Effects of Compassion Cultivation Training (CCT) on Health-Care Workers. Clin. Psychol. 2017, 21, 116–124. [Google Scholar] [CrossRef] [Green Version]
- Kemper, K.J.; Lynn, J.; Mahan, J.D. What Is the Impact of Online Training in Mind–Body Skills? J. Evid. Based Complement. Altern. Med. 2015, 20, 275–282. [Google Scholar] [CrossRef] [Green Version]
- Zenasni, F.; Boujut, E.; du Vaure, B.; Catu-Pinault, A.; Tavani, J.; Rigal, L.; Jaury, P.; Magnier, M.A.; Falcoff, H.; Sultan, S.; et al. Development of a French-Language Version of the Jefferson Scale of Physician Empathy and Association with Practice Characteristics and Burnout in a Sample of General Practitioners. Int. J. Pers. Cent. Med. 2012, 2, 759–766. [Google Scholar]
- Oruç, Ö.; Hörmet İğde, M.; Kocatepe, V.; Yildirim, D. Examining the Compassion Status of Healthcare Professionals Working in the Palliative Care Units. Turk Onkol. Derg. 2020, 35, 250–256. [Google Scholar] [CrossRef]
- Pavlova, A.; Wang, C.X.Y.; Boggiss, A.L.; O’Callaghan, A.; Consedine, N.S. Predictors of Physician Compassion, Empathy, and Related Constructs: A Systematic Review. J. Gen. Intern. Med. 2022, 37, 900–911. [Google Scholar] [CrossRef]
- Neff, K.D.; Pommier, E. The Relationship between Self-Compassion and Other-Focused Concern among College Undergraduates, Community Adults, and Practicing Meditators. Self Identity 2013, 12, 160–176. [Google Scholar] [CrossRef]
- Çingöl, N.; Çelebi, E.; Zengin, S.; Karakaþ, M. Bir Saðlýk Yüksekokulu Hemþirelik Bölümü Öðrencilerinin Merhamet Düzeylerinin Ýncelenmesi. Klin. Psikiyatr. Derg. 2018, 21, 61–67. [Google Scholar] [CrossRef]
- Arkan, B.; Yılmaz, D.; Düzgün, F. Determination of Compassion Levels of Nurses Working at a University Hospital. J. Relig. Health 2020, 59, 29–39. [Google Scholar] [CrossRef] [PubMed]
- Boniol, M.; Mcisaac, M.; Xu, L.; Wuliji, T.; Diallo, K.; Campbell, J. Gender Equity in the Health Workforce: Analysis of 104 Countries; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Dutton, J.; Lilius, J.; Kanov, J. The Transformative Potential of Compassion at Work. In New Designs for Transformative Cooperation; Cooperrider, D., Fry, R., Piderit, S., Eds.; Stanford University Press: Stanford, CA, USA, 2007; pp. 107–124. [Google Scholar]
- Goetz, J.L.; Keltner, D.; Simon-Thomas, E. Compassion: An Evolutionary Analysis and Empirical Review. Psychol. Bull. 2010, 136, 351–374. [Google Scholar] [CrossRef] [Green Version]
- Batson, C.D.; Lishner, D.A.; Stocks, E.L. The Empathy–Altruism Hypothesis. In The Oxford Handbook of Prosocial Behavior; Shroeder, D.A., Graziano, W.G., Eds.; Oxford University Press: New York, NY, USA, 2015; pp. 259–281. [Google Scholar] [CrossRef]
- Condon, P.; Desbordes, G.; Miller, W.B.; DeSteno, D. Meditation Increases Compassionate Responses to Suffering. Psychol. Sci. 2013, 24, 2125–2127. [Google Scholar] [CrossRef]
- Demerouti, E.; Nachreiner, F.; Bakker, A.B.; Schaufeli, W.B. The Job Demands-Resources Model of Burnout. J. Appl. Psychol. 2001, 86, 499–512. [Google Scholar] [CrossRef]
- Lown, B.A.; Manning, C.F. The Schwartz Center Rounds: Evaluation of an Interdisciplinary Approach to Enhancing Patient-Centered Communication, Teamwork, and Provider Support. Acad. Med. 2010, 85, 1073–1081. [Google Scholar] [CrossRef]
- West, M.A.; Lyubovnikova, J.; Eckert, R.; Denis, J.L. Collective Leadership for Cultures of High Quality Health Care. J. Organ. Eff. 2014, 1, 240–260. [Google Scholar] [CrossRef]
- Valentine, M.A.; Edmondson, A.C. Team Scaffolds: How Meso-Level Structures Support Role-Based Coordination in Temporary Groups. Organ. Sci. 2014, 26, 311–631. [Google Scholar]
- Vogus, T.J.; McClelland, L.E.; Lee, Y.S.H.; McFadden, K.L.; Hu, X. Creating a Compassion System to Achieve Efficiency and Quality in Health Care Delivery. J. Serv. Manag. 2020, 32, 560–580. [Google Scholar] [CrossRef]
- Schaufeli, W.B. Engaging Leadership in the Job Demands-Resources Model. Career Dev. Int. 2015, 20, 446–463. [Google Scholar] [CrossRef] [Green Version]
- García-Sierra, R.; Fernández-Castro, J.; Martínez-Zaragoza, F. Work Engagement in Nursing: An Integrative Review of the Literature. J. Nurs. Manag. 2016, 24, E101–E111. [Google Scholar] [CrossRef] [PubMed]
- Deao, C. The E Factor: How Engaged Patients, Clinicians, Leaders, and Employees Will Transform Healthcare; Fire Starter Publishing: Pensacola, FL, USA, 2017. [Google Scholar]
- Sutcliffe, K.M.; Vogus, T.J. Organizing For Resilience. In Positive Organizational Scholarship; Cameron, K., Dutton, J.E., Quinn, R.E., Eds.; Berrett-Koehler: San Francisco, CA, USA, 2003; pp. 94–110. [Google Scholar]
- Lamothe, M.; Boujut, E.; Zenasni, F.; Sultan, S. To Be or Not to Be Empathic: The Combined Role of Empathic Concern and Perspective Taking in Understanding Burnout in General Practice. BMC Fam. Pract. 2014, 15, 15. [Google Scholar] [CrossRef] [PubMed]
- Cosley, B.J.; McCoy, S.K.; Saslow, L.R.; Epel, E.S. Is Compassion for Others Stress Buffering? Consequences of Compassion and Social Support for Physiological Reactivity to Stress. J. Exp. Soc. Psychol. 2010, 46, 816–823. [Google Scholar] [CrossRef]
- Carver, C.S.; Scheier, M.F.; Segerstrom, S.C. Optimism. Clin. Psychol. Rev. 2010, 879–889. [Google Scholar] [CrossRef] [Green Version]
- Wright, T.A.; Cropanzano, R. The Happy/Productive Worker Thesis Revisited. In Research in Personnel and Human Resources Management; Emerald Publishing: Bingley, UK, 2007; pp. 269–307. [Google Scholar] [CrossRef]
- Lyubomirsky, S.; King, L.; Diener, E. The Benefits of Frequent Positive Affect: Does Happiness Lead to Success? Psychol. Bull. 2005, 131, 803–855. [Google Scholar] [CrossRef] [Green Version]
- Dutton, J.E.; Worline, M.C.; Frost, P.J.; Lilius, J. Explaining Compassion Organizing. Adm. Sci. Q. 2006, 51, 59–96. [Google Scholar] [CrossRef] [Green Version]
- Lutgen-Sandvik, P.; Tracy, S.J. Answering Five Key Questions about Workplace Bullying: How Communication Scholarship Provides Thought Leadership for Transforming Abuse at Work. Manag. Commun. Q. 2012, 26, 3–47. [Google Scholar] [CrossRef] [Green Version]
- Moon, T.W.; Hur, W.M.; Ko, S.H.; Kim, J.W.; Yoo, D.K. Positive Work-Related Identity as a Mediator of the Relationship between Compassion at Work and Employee Outcomes. Hum. Factors Ergon. Manuf. 2016, 26, 84–94. [Google Scholar] [CrossRef]
- Lilius, J.M.; Kanov, J.; Dutton, J.E.; Worline, M.C.; Maitlis, S. Compassion Revealed: What We Know About Compassion at Work (and Where We Need to Know More). In The Oxford Handbook of Positive Organizational Scholarship; Oxford University Press: New York, NY, USA, 2012. [Google Scholar] [CrossRef]
- Chu, L.C. Impact of Providing Compassion on Job Performance and Mental Health: The Moderating Effect of Interpersonal Relationship Quality. J. Nurs. Scholarsh. 2017, 49, 456–465. [Google Scholar] [CrossRef]
- Chang, C.S. Moderating Effects of Nurses’ Organizational Support on the Relationship Between Job Satisfaction and Organizational Commitment. West. J. Nurs. Res. 2015, 37, 724–745. [Google Scholar] [CrossRef] [PubMed]
- Han, K.S.; Chung, K.H. Positive Psychological Capital, Organizational Commitment and Job Stress of Nurses in Small and Medium-Sized Hospitals. Adv. Sci. Technol. Lett. 2015, 88, 208–211. [Google Scholar]
- Karami, A.; Farokhzadian, J.; Foroughameri, G. Nurses’ Professional Competency and Organizational Commitment: Is It Important for Human Resource Management? PLoS ONE 2017, 12, e0187863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, R.; Kashif, M. The Role of Resonant Leadership, Workplace Friendship and Serving Culture in Predicting Organizational Commitment: The Mediating Role of Compassion at Work. Rev. Bras. De Gest. De Neg. 2020, 22, 799–819. [Google Scholar] [CrossRef]
- Acosta, H.; Torrente, P.; Llorens, S.; Salanova, M. La Confianza Es Pasión: La Relación Entre Confianza Organizacional y El Engagement de Los Equipos. Rev. Latinoam. Psicol. Posit. 2016, 1, 8–22. [Google Scholar]
- Farris, K.B. Are You Happy? How Employee Satisfaction Affects Employee Productivity in Private Hospitals; University of South Alabama: Mobile, AL, USA, 2021. [Google Scholar]
- Amutio, A.; Pizarro, J.J.; Basabe, N.; Telletxea, S.; Harizmendi, M. Propiedades Psicométricas de La Escala de Compasión Hacia Los Demás (Psychometric Properties for the Scale of Compassion for Others). Rev. Latinoam. Psicol. Posit. 2018, 4, 24–37. [Google Scholar]
- Pommier, E.; Neff, K.D.; Tóth-Király, I. The Development and Validation of the Compassion Scale. Assessment 2020, 27, 21–39. [Google Scholar] [CrossRef]
- Brown, J.D. The Cronbach Alpha Reliability Estimate The Cronbach Alpha Reliability Estimate How Should We Interpret Cronbach Alpha? Shiken JALT Test. Eval. SIG Newsl. 2002, 6, 17–19. [Google Scholar]
- Yoon, M.; Lai, M.H.C. Testing Factorial Invariance with Unbalanced Samples. Struct. Equ. Model. 2018, 25, 201–213. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Peters, G. The Alpha and the Omega of Scale Reliability and Validity: Why and How to Abandon Cronbach’s Alpha and the Route towards More Comprehensive Assessment of Scale Quality. Eur. Health Psychol. 2014, 16, 56–69. [Google Scholar] [CrossRef] [Green Version]
- Schreiber, J.B. Update to Core Reporting Practices in Structural Equation Modeling. Res. Soc. Adm. Pharm. 2017, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Tingley, D.; Yamamoto, T.; Hirose, K.; Keele, L.; Imai, K. Mediation: R Package for Causal Mediation Analysis; UCLA Statistics/American Statistical Association: Los Angeles, CA, USA, 2014. [Google Scholar]
- Chen, F.F. What Happens If We Compare Chopsticks with Forks? The Impact of Making Inappropriate Comparisons in Cross-Cultural Research. J. Pers. Soc. Psychol. 2008, 95, 1005. [Google Scholar] [CrossRef] [PubMed]
- Kanov, J.M.; Maitlis, S.; Worline, M.C.; Dutton, J.E.; Frost, P.J.; Lilius, J.M. Compassion in Organizational Life. Am. Behav. Sci. 2004, 808–827. [Google Scholar] [CrossRef]
- Condon, P. Meditation in Context: Factors That Facilitate Prosocial Behavior. Curr. Opin. Psychol. 2019, 15–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dutton, J.E.; Roberts, L.M.; Bednar, J. Pathways for Positive Identity Construction at Work: Four Types of Positive Identity and the Building of Social Resources. Acad. Manag. Rev. 2010, 35, 265–293. [Google Scholar] [CrossRef]
- Bakker, A.B. An Evidence-Based Model of Work Engagement. Curr. Dir. Psychol. Sci. 2011, 265–269. [Google Scholar] [CrossRef]
- Lilius, J.M.; Worline, M.C.; Maitlis, S.; Kanov, J.; Dutton, J.E.; Frost, P. The Contours and Consequences of Compassion at Work. J. Organ. Behav. 2008, 29, 193–218. [Google Scholar] [CrossRef] [Green Version]
- Hashim, M.J. Patient-Centered Communication: Basic Techniques. Am. Fam. Physician. 2017, 95, 29–34. [Google Scholar]
- Ekman, P.; Ekman, E. Is Global Compassion Achievable? In The Oxford Handbook of Compassion Science; Seppälä, E.M., Simon-Thomas, E., Brown, S.L., Worline, M.C., Cameron, C.D., Doty, J.R., Eds.; Oxford University Press: New York, NY, USA, 2017; Volume 1, pp. 41–49. [Google Scholar] [CrossRef]
- Loewenthal, K.M. An Introduction to Psychological Tests and Scales; UCL Press Limited: London, UK, 1996. [Google Scholar]
- Nunnally, J.; Bernstein, I. Psychometric Theory; McGraw Hill: New York, NY, USA, 1994. [Google Scholar]
- Kaplan, R.M.; Saccuzzo, D.P. Psychological Testing: Principles, Applications, and Issues; Cengage Learning: Boston, MA, USA, 2017. [Google Scholar]
- Barello, S.; Graffigna, G. Caring for Health Professionals in the COVID-19 Pandemic Emergency: Toward an “Epidemic of Empathy” in Healthcare. Front. Psychol. 2020, 11, 1431. [Google Scholar] [CrossRef]
| Variables | Demographic Information |
|---|---|
| Age ranges | 14.71% (209) aged 20–29 28.66% (407) aged 30–39 32.18% (457) aged 40–49 17.60% (250) aged 50–59 6.26% (89) aged 60–75 |
| Job Position | 39.64% (563) nurses 18.45% (262) nursing assistants 9.92% (141) physicians 9.71% (138) coordinators/supervisors 5.28% (75) dieticians and kitchen 3.87% (55) administrative 3.16% (45) technicians 9.92% (141) others (e.g., orderlies, psychologists, midwives, support staff) |
| Tenure | 33.59% (477) one to five years 18.09% (257) six to 10 years 16.97% (241) 11 to 15 years 11.33% (161) 16 to 20 years 13.52% (192) 21 to 30 years 6.05% (86) 31 to 45 years |
| Type of contract | 65.63% (932) permanent contract 22.6% (321) temporary contract 11.76% (167) another type of contract |
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Compassion | 4.91 | 0.70 | - | ||||||||||
| 2. Social Job Resources | 4.89 | 0.83 | −0.11 ** | - | |||||||||
| 3. Social Support | 4.89 | 1.11 | −0.12 ** | −0.01 | - | ||||||||
| 4. Coordination | 4.99 | 0.98 | −0.62 ** | −0.05 | 0.32 ** | - | |||||||
| 5. Positive Leadership | 4.82 | 1.24 | −0.07 * | −0.02 | 0.28 ** | 0.83 ** | - | ||||||
| 6. In-Role Performance | 5.45 | 0.82 | −0.09 ** | −0.01 | 0.36 ** | 0.45 ** | 0.31 ** | - | |||||
| 7. Extra Role Performance | 3.85 | 1.40 | 0.02 | 0.04 | 0.12 ** | 0.01 | −0.00 | 0.05 | - | ||||
| 8.Organisational Commitment | 4.96 | 1.14 | −0.13 ** | 0.02 | 0.37 ** | 0.51 ** | 0.37 ** | 0.42 ** | 0.42 ** | - | |||
| 9. Healthy Employees | 4.66 | 0.94 | −0.13 ** | −0.01 | 0.43 ** | 0.72 ** | 0.58 ** | 0.60 ** | 0.56 ** | 0.43 ** | - | ||
| 10. Work Engagement | 4.81 | 1.01 | −0.14 ** | 0.02 | 0.39 ** | 0.62 ** | 0.47 ** | 0.54 ** | 0.45 ** | 0.42 ** | 0.07 * | - | |
| 11. Resilience | 4.58 | 1.11 | −0.11 ** | −0.00 | 0.35 ** | 0.61 ** | 0.50 ** | 0.51 ** | 0.47 ** | 0.36 ** | 0.03 | 0.54 ** | - |
| 12. Optimism | 4.58 | 1.21 | −0.09 ** | 0.00 | 0.36 ** | 0.60 ** | 0.51 ** | 0.48 ** | 0.50 ** | 0.34 ** | 0.05 | 0.57 ** | 0.86 ** |
| Model | χ² | df | χ²/df | p | TLI | CFI | RMSEA | Lower | Upper |
|---|---|---|---|---|---|---|---|---|---|
| M1 Partial Mediation | 153.688 | 41 | 3.75 | 0.000 | 0.964 | 0.973 | 0.050 | 0.041 | 0.058 |
| M2 Full Mediation | 503.951 | 42 | 11.99 | 0.000 | 0.858 | 0.891 | 0.099 | 0.092 | 0.107 |
| M3 Partial Mediation | 190.792 | 40 | 4.769 | 0.000 | 0.933 | 0.951 | 0.058 | 0.050 | 0.067 |
| M4 Full Mediation | 328.533 | 43 | 7.640 | 0.000 | 0.882 | 0.907 | 0.077 | 0.069 | 0.085 |
| M5 Partial Mediation | 268.676 | 71 | 3.784 | 0.000 | 0.952 | 0.963 | 0.050 | 0.044 | 0.056 |
| M6 Full Mediation | 233.759 | 68 | 3.437 | 0.000 | 0.958 | 0.969 | 0.047 | 0.040 | 0.053 |
| χ2 | df | χ2/df | RMSEA | 90% CI | CFI | TLI | SRMR | CMs | ∆χ2 (∆ df) | ∆CFI | ∆SRMR | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Single Group SEM | ||||||||||||
| M5 | 157.890 ** | 69 | 2.288 | 0.046 | [0.037, 0.056] | 0.973 | 0.964 | 0.032 | - | - | - | - |
| Multiple Group (Gender) | ||||||||||||
| M5.1 configural invariance | 337.390 ** | 186 | 1.814 | 0.037 | [0.030, 0.043] | 0.954 | 0.955 | 0.046 | - | - | - | - |
| M5.2 metric invariance | 380.419 ** | 187 | 2.034 | 0.041 | [0.035, 0.047] | 0.941 | 0.943 | 0.052 | M5.1–M5.2 | 43.029 (1) ** | 0.013 | 0.006 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
San Román-Niaves, M.; Coo, C.; Llorens, S.; Salanova, M. The Mediating Role of Compassion between Social Job Resources, and Healthy Healthcare Professionals: A Cross-Sectional Study with Gender Perspective. Int. J. Environ. Res. Public Health 2022, 19, 7500. https://doi.org/10.3390/ijerph19127500
San Román-Niaves M, Coo C, Llorens S, Salanova M. The Mediating Role of Compassion between Social Job Resources, and Healthy Healthcare Professionals: A Cross-Sectional Study with Gender Perspective. International Journal of Environmental Research and Public Health. 2022; 19(12):7500. https://doi.org/10.3390/ijerph19127500
Chicago/Turabian StyleSan Román-Niaves, Mabel, Cristián Coo, Susana Llorens, and Marisa Salanova. 2022. "The Mediating Role of Compassion between Social Job Resources, and Healthy Healthcare Professionals: A Cross-Sectional Study with Gender Perspective" International Journal of Environmental Research and Public Health 19, no. 12: 7500. https://doi.org/10.3390/ijerph19127500
APA StyleSan Román-Niaves, M., Coo, C., Llorens, S., & Salanova, M. (2022). The Mediating Role of Compassion between Social Job Resources, and Healthy Healthcare Professionals: A Cross-Sectional Study with Gender Perspective. International Journal of Environmental Research and Public Health, 19(12), 7500. https://doi.org/10.3390/ijerph19127500









