Health Promotion Behaviors of Pregnant Couples in the COVID-19 Pandemic: Actor-Partner Interdependence Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measures
2.2.1. Fear of COVID-19
2.2.2. Depression
2.2.3. Post Traumatic Growth
2.2.4. Marital Adjustment
2.2.5. Health Promotion Behavior
2.3. Data Collection
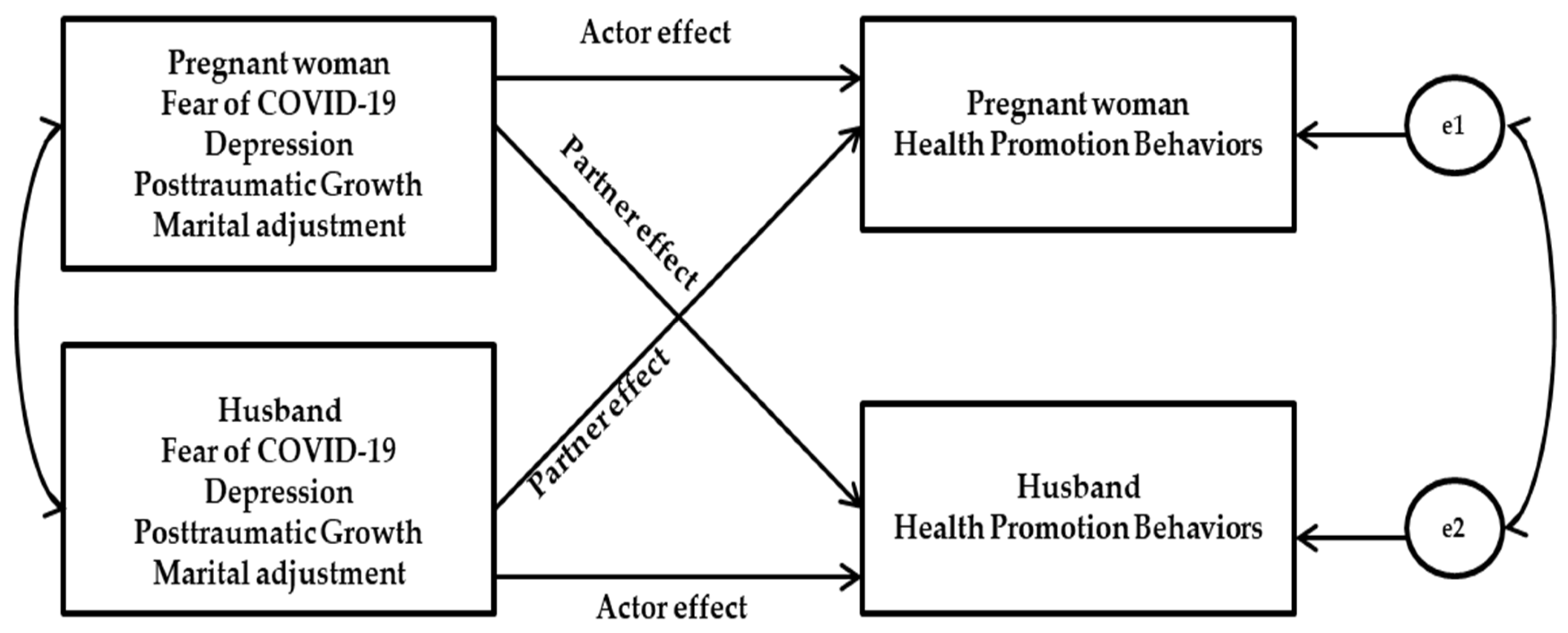
2.4. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Correlations among Study Variables
3.3. Actor-Partner Interdependence Model (APIM) Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jin, Y.; Yang, H.; Ji, W.; Wu, W.; Chen, S.; Zhang, W.; Duan, G. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses 2020, 12, 372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 12 January 2022).
- Abouzid, M.; El-Sherif, D.M.; Eltewacy, N.K.; Dahman, N.; Okasha, S.A.; Ghozy, S.; Islam, S.; EARG Collaborators. Influence of COVID-19 on lifestyle behaviors in the Middle East and North Africa region: A survey of 5896 individuals. J. Transl. Med. 2021, 19, 129. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Rawat, D.; Dixit, V.; Gulati, S.; Gulati, S.; Gulati, A. Impact of COVID-19 outbreak on lifestyle behaviour: A review of studies published in India. Diabetes Metab. Syndr. 2021, 15, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Phoswa, W.N.; Khaliq, O.P. Is pregnancy a risk factor of COVID-19? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 252, 605–609. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guo, J.; Wang, C.; Luo, F.; Yu, X.; Zhang, W.; Li, J.; Zhao, D.; Xu, D.; Gong, Q.; et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020, 395, 809–815. [Google Scholar] [CrossRef] [Green Version]
- Huntley, B.J.; Huntley, E.S.; Di Mascio, D.; Chen, T.; Berghella, V.; Chauhan, S.P. Rates of maternal and perinatal mortality and vertical transmission in pregnancies complicated by severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2) infection: A systematic review. Obstet. Gynecol. 2020, 136, 303–312. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, H.; Tang, K.; Guo, Y. Withdrawn: Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J. Infect. 2020, 82, 282–327. [Google Scholar] [CrossRef] [Green Version]
- Smith, V.; Seo, D.; Warty, R.; Payne, O.; Salih, M.; Chin, K.L.; Ofori-Asenso, R.; Krishnan, S.; da Silva Costa, F.; Vollenhoven, B.; et al. Maternal and neonatal outcomes associated with COVID-19 infection: A systematic review. PLoS ONE 2020, 15, e0234187. [Google Scholar] [CrossRef]
- Zaigham, M.; Andersson, O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef] [Green Version]
- Zhu, H.; Wang, L.; Fang, C.; Peng, S.; Zhang, L.; Chang, G.; Xia, S.; Zhou, W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020, 9, 51–60. [Google Scholar] [CrossRef]
- Dashraath, P.; Wong, J.; Lim, M.; Lim, L.M.; Li, S.; Biswas, A.; Choolani, M.; Mattar, C.; Su, L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020, 222, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Aydin, R.; Aktaş, S. An investigation of women’s pregnancy experiences during the COVID-19 pandemic: A qualitative study. Int. J. Clin. Pract. 2021, 75, e14418. [Google Scholar] [CrossRef] [PubMed]
- Javaid, S.; Barringer, S.; Compton, S.D.; Kaselitz, E.; Muzik, M.; Moyer, C.A. The impact of COVID-19 on prenatal care in the United States: Qualitative analysis from a survey of 2519 pregnant women. Midwifery 2021, 98, 102991. [Google Scholar] [CrossRef]
- Rabbani, U.; Saigul, A.A.; Sulaiman, A.; Ibrahim, T.H. Impact of COVID-19 on antenatal care utilization among pregnant women in Qassim, Saudi Arabia. Cureus 2021, 13, e19554. [Google Scholar] [CrossRef]
- Bakır, N.; Irmak Vural, P.; Demir, C. Relationship of depression, anxiety and stress levels with religious coping strategies among Turkish pregnant women during the COVID-19 pandemic. J. Relig. Health 2021, 60, 3379–3393. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Imani, V.; Lin, C.Y.; Timpka, T.; Broström, A.; Updegraff, J.A.; Årestedt, K.; Griffiths, M.D.; Pakpour, A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: An Actor-Partner Interdependence Modelling. Int. J. Ment. Health Addict. 2020, 20, 68–82. [Google Scholar] [CrossRef] [PubMed]
- Durmuş, M.; Öztürk, Z.; Şener, N.; Eren, S.Y. The relationship between the fear of Covid-19, depression, and spiritual well-being in pregnant women. J. Relig. Health 2021, 61, 798–810. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [Green Version]
- Ayaz, R.; Hocaoğlu, M.; Günay, T.; Yardımcı, O.D.; Turgut, A.; Karateke, A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J. Perinat. Med. 2020, 48, 965–970. [Google Scholar] [CrossRef]
- Kotlar, B.; Gerson, E.; Petrillo, S.; Langer, A.; Tiemeier, H. The impact of the COVID-19 pandemic on maternal and perinatal health: A scoping review. Reprod. Health 2021, 18, 10. [Google Scholar] [CrossRef]
- Moyer, C.A.; Compton, S.D.; Kaselitz, E.; Muzik, M. Pregnancy-related anxiety during COVID-19: A nation wide survey of 2740 pregnant women. Arch. Womens Ment. Health 2020, 23, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Zhu, J.; Tao, H.; Ma, Y.; Jin, W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J. Psychosom. Obstet. Gynaecol. 2021, 42, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, K.M.; Hung, P.; Alberg, A.J.; Hair, N.L.; Liu, J. Variations in health behaviors among pregnant women during the COVID-19 pandemic. Midwifery 2021, 95, 102929. [Google Scholar] [CrossRef] [PubMed]
- Rashan, N.; Sharifi, N.; Fathnezhad-Kazemi, A.; Golnazari, K.; Taheri, S. The association between social support and psychological factors with health-promoting behaviours in pregnant women: A cross-sectional study. J. Educ. Health Promot. 2021, 10, 9. [Google Scholar] [CrossRef]
- Zhang, H.L.; Li, C.Y.; Kim, H.L. Status and influencing factors of health behavior in pregnant women in Yanbian area. JKAIS 2015, 16, 7863–7869. [Google Scholar] [CrossRef] [Green Version]
- Tedeschi, R.G.; Calhoun, L.G. Posttraumatic growth: Conceptual foundations and empirical evidence. Psychol. Inq. 2004, 15, 1–18. [Google Scholar] [CrossRef]
- Aldwin, C.M.; Levenson, M.R. Posttraumatic growth: A developmental perspective. Psychol. Inq. 2004, 15, 19–22. Available online: http://www.jstor.org/stable/20447195 (accessed on 1 December 2019).
- Ayers, S. Birth trauma and post-traumatic stress disorder: The importance of risk and resilience. J. Reprod. Infant Psychol. 2017, 35, 427–430. [Google Scholar] [CrossRef] [Green Version]
- Beck, C.T.; Watson, S.; Gable, R.K. Traumatic childbirth and its aftermath: Is there anything positive? J. Perinat. Educ. 2018, 27, 175–184. [Google Scholar] [CrossRef]
- Sawyer, A.; Ayers, S.; Young, D.; Bradley, R.; Smith, H. Posttraumatic growth after childbirth: A prospective study. Psychol. Health 2012, 27, 362–377. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, A.; Nakić Radoš, S.; Ayers, S.; Burn, E. Personal growth in UK and Croatian women following childbirth: A preliminary study. J. Reprod. Infant Psychol. 2015, 33, 294–307. [Google Scholar] [CrossRef]
- Büchi, S.; Mörgeli, H.; Schnyder, U.; Jenewein, J.; Glaser, A.; Fauchère, J.C.; Ulrich Bucher, H.; Sensky, T. Shared or discordant grief in couples 2–6 years after the death of their premature baby: Effects on suffering and posttraumatic growth. Psychosomatics 2009, 50, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.T.; Watson, S. Posttraumatic growth after birth trauma: “I was broken, now I am unbreakable”. MCN Am. J. Matern. Child. Nurs. 2016, 41, 264–271. [Google Scholar] [CrossRef]
- Rozen, G.; Taubman–Ben-Ari, O.; Strauss, T.; Morag, I. Personal growth of mothers of preterms: Objective severity of the event, subjective stress, personal resources, and maternal emotional support. J. Happiness Stud. 2018, 19, 2167–2186. [Google Scholar] [CrossRef]
- Wang, Z.; Hania, A.; Muzaffar, A.; Zia, S. Post traumatic growth for gestational diabetic patients during COVID-19: Role of partner supportive communication and family environment. Int. J. Womens Health 2021, 13, 1017–1023. [Google Scholar] [CrossRef] [PubMed]
- Yun, J.H. Influencing Factors of Posttraumatic Growth in Postpartum Women. Master’s Thesis, Dong-A University, Busan, Korea, 2021. [Google Scholar]
- Kim, J.H.; Song, Y.A. Health promoting behavior in pregnant couples: Actor-partner interdependence model analysis. JKAN 2017, 47, 467–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torres-Cruz, D.; Aznar-Martínez, B.; Pérez-Testor, C. Impact of the COVID-19 confinement on couple satisfaction and sexuality. J. Sex. Marital Ther. 2021, 48, 363–375. [Google Scholar] [CrossRef]
- Kenny, D.A. Models of non-independence in dyadic research. J. Soc. Pers. Relat. 1996, 13, 279–294. [Google Scholar] [CrossRef]
- Seong, M.; Kim, I.; Kang, M.; Lee, M. Validity and reliability evaluation of the Korean version of the Fear of COVID-19 Scale. KSW 2020, 15, 391–399. [Google Scholar] [CrossRef]
- Chon, K.K.; Rhee, M.K. Preliminary Development of Korean Version of CES-D. Kor. J. Clin. Psychol. 1992, 11, 65–76. Available online: https://kiss.kstudy.com/thesis/thesis-view.asp?key=154256 (accessed on 1 December 2019).
- Radloff, L.S. The CES-D Scale: A self-report depression scale or research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Song, S.-H.; Lee, H.-S.; Park, J.-H.; Kim, K.-H. Validity and reliability of the Korean version of the posttraumatic growth inventory. Korean J. Health Psychol. 2009, 14, 193–214. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Calhoun, L.G. The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. J. Trauma. Stress 1996, 9, 455–471. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.I. A study of the reliability and the validity of revised dyadic adjustment scale. Go Hwang Non-Jib Kyung Hee Grad. Sch. 2004, 35, 97–113. Available online: https://www.koreascience.or.kr/article/JAKO201109649109600.pdf (accessed on 1 December 2019).
- Spanier, G.B. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J. Marriage Fam. 1976, 38, 15–28. [Google Scholar] [CrossRef]
- Busby, D.M.; Christensen, C.; Crane, D.R.; Larson, J.H. A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. J. Marital Fam. Ther. 1995, 21, 289–308. [Google Scholar] [CrossRef]
- Walker, S.N.; Sechrist, K.R.; Pender, N.J. The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nurs. Res. 1987, 36, 76–81. [Google Scholar] [CrossRef]
- Lee, T.W. Determinants of Health Promotion Behavior: Centered on Well Adults Living in Seoul. Master’s Thesis, Yonsei University, Seoul, Korea, 1990. [Google Scholar]
- Choi, S.R. The Factors That Affect Health-Promotion Lifestyle of Nurses. Master’s Thesis, Kyunghee University, Seoul, Korea, 2006. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structl. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Stolow, J.A.; Moses, L.M.; Lederer, A.M.; Carter, R. How fear appeal approaches in COVID-19 health communication may be harming the global community. Health Educ. Behav. 2020, 47, 531–535. [Google Scholar] [CrossRef]
- Kumari, A.; Ranjan, P.; Sharma, K.A.; Sahu, A.; Bharti, J.; Zangmo, R.; Bhatla, N. Impact of COVID-19 on psychosocial functioning of peripartum women: A qualitative study comprising focus group discussions and in-depth interviews. Int. J. Gynaecol. Obstet. 2021, 152, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Tzur Bitan, D.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef] [PubMed]
- Naghizadeh, S.; Mirghafourvand, M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch. Psychiatr Nurs. 2021, 35, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Lebel, C.; MacKinnon, A.; Bagshawe, M.; Tomfohr-Madsen, L.; Giesbrecht, G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020, 277, 5–13. [Google Scholar] [CrossRef]
- Molgora, S.; Acquati, C.; Fenaroli, V.; Saita, E. Dyadic coping and marital adjustment during pregnancy: A cross-sectional study of Italian couples expecting their first child. Int. J. Psychol. 2019, 54, 277–285. [Google Scholar] [CrossRef]
- Unruh, L.; Allin, S.; Marchildon, G.; Burke, S.; Barry, S.; Siersbaek, R.; Thomas, S.; Rajan, S.; Koval, A.; Alexander, M.; et al. A comparison of 2020 health policy responses to the COVID-19 pandemic in Canada, Ireland, the United Kingdom and the United States of America. Health Policy, 2021; in press. [Google Scholar] [CrossRef]
- Kim, W.; Jung, T.Y.; Roth, S.; Um, W.; Kim, C. Management of the COVID-19 Pandemic in the Republic of Korea from the Perspective of Governance and Public-Private Partnership. Yonsei Med. J. 2021, 62, 777–791. [Google Scholar] [CrossRef]
- Lee, H.; Lee, J.R.; Jung, H.; Lee, J.Y. Power of universal health coverage in the era of COVID-19: A nationwide observational study. Lancet Reg. Health West. Pac. 2021, 7, 100088. [Google Scholar] [CrossRef]

| Variable | Pregnant Women r (p) | Husbands r (p) | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 HPB | 2 Fear | 3 Depression | 4 PTG | 5 MA | 6 HPB | 7 Fear | 8 Depression | 9 MA | M ± SD | |
| Pregnant woman | ||||||||||
| 1. HPB | 1 | 70.46 ± 10.40 | ||||||||
| 2. Fear | 0.33 *** | 1 | 24.43 ± 5.18 | |||||||
| 3. Depression | −0.21 * | 0.18 * | 1 | 17.60 ± 10.20 | ||||||
| 4. PTG | 0.47 *** | 0.07 | −0.22 * | 1 | 69.12 ± 3.34 | |||||
| 5. MA | 0.23 * | 0.03 | −0.43 *** | 0.27 ** | 1 | 65.10 ± 8.54 | ||||
| Husband | ||||||||||
| 6. HPB | 0.32 *** | 0.19 * | −0.03 | 0.07 | 0.08 | 1 | 73.84 ± 14.30 | |||
| 7. Fear | 0.06 | 0.20 * | 0.16 | −0.08 | 0.07 | 0.22 * | 1 | 18.69 ± 5.81 | ||
| 8. Depression | −0.15 | 0.05 | 0.10 | −0.04 | −0.14 | −0.39 *** | 0.24 ** | 1 | 8.40 ± 6.00 | |
| 9. PTG | −0.02 | −0.08 | −0.08 | 0.05 | −0.08 | 0.38 *** | −0.11 | −0.26 ** | 1 | 66.24 ± 12.64 |
| 10. MA | 0.22 * | 0.08 | −0.00 | 0.05 | −0.01 | 0.48 *** | −0.17 | −0.40 *** | 0.23 * | 66.50 ± 9.50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.H.; Kang, H.S. Health Promotion Behaviors of Pregnant Couples in the COVID-19 Pandemic: Actor-Partner Interdependence Model. Int. J. Environ. Res. Public Health 2022, 19, 7501. https://doi.org/10.3390/ijerph19127501
Kim SH, Kang HS. Health Promotion Behaviors of Pregnant Couples in the COVID-19 Pandemic: Actor-Partner Interdependence Model. International Journal of Environmental Research and Public Health. 2022; 19(12):7501. https://doi.org/10.3390/ijerph19127501
Chicago/Turabian StyleKim, Sun Hee, and Hee Sun Kang. 2022. "Health Promotion Behaviors of Pregnant Couples in the COVID-19 Pandemic: Actor-Partner Interdependence Model" International Journal of Environmental Research and Public Health 19, no. 12: 7501. https://doi.org/10.3390/ijerph19127501
APA StyleKim, S. H., & Kang, H. S. (2022). Health Promotion Behaviors of Pregnant Couples in the COVID-19 Pandemic: Actor-Partner Interdependence Model. International Journal of Environmental Research and Public Health, 19(12), 7501. https://doi.org/10.3390/ijerph19127501





