High Challenge Exercise and Learning Safe Landing Strategies among Community-Dwelling Older Adults: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
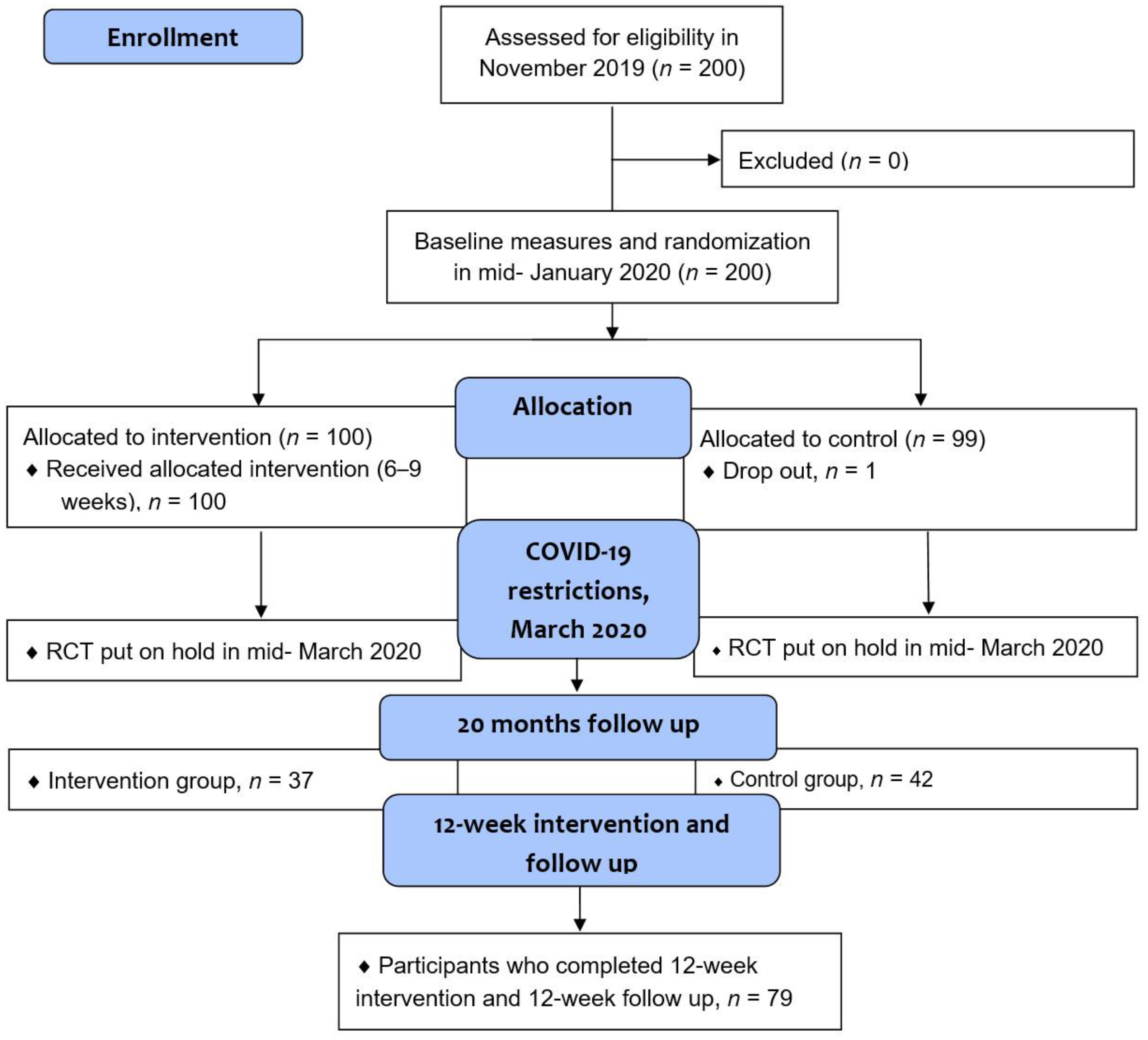
2.1. Study Design and Population
2.2. Intervention
- (1)
- Practicing fall techniques and strength exercises, body awareness, mobility training, building up load of resistance in muscles, tendons, joints, and skeleton, as well as highly challenging exercises to train balance by performing movements that are not usually carried out in everyday life activities, e.g., getting up and down from the floor;
- (2)
- Continuing fall techniques and strength exercises, increasing load in strength exercises, challenging balance and coordination ability, greater range of movements in exercises, possibly power in exercises, continuing to build up load resistance in muscles, tendons, joints, and skeleton;
- (3)
- Training in ability to develop power (fast power), power in strength exercises, and possibly in training in fall techniques, challenging one’s balance with increased difficulty.
2.3. Measurements
2.4. Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Step Safely: Strategies for Preventing and Managing Falls across the Life-Course; World Health Organization: Geneva, Switzerland, 2021.
- Deandrea, S.; Lucenteforte, E.; Bravi, F.; Foschi, R.; La Vecchia, C.; Negri, E. Risk Factors for Falls in Community-Dwelling Older People: A Systematic Review and Meta-Analysis. Epidemiology 2010, 21, 658–668. [Google Scholar] [CrossRef]
- Kyrdalen, I.L.; Thingstad, P.; Sandvik, L.; Ormstad, H. Associations between Gait Speed and Well-Known Fall Risk Factors among Community-Dwelling Older Adults. Physiother. Res. Int. 2019, 24, e1743. [Google Scholar] [CrossRef] [Green Version]
- Gardner, M.M.; Buchner, D.M.; Robertson, M.C.; Campbell, A.J. Practical Implementation of an Exercise-Based Falls Prevention Programme. Age Ageing 2001, 30, 77–83. [Google Scholar] [CrossRef] [Green Version]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for Preventing Falls in Older People Living in the Community. Cochrane Database Syst. Rev. 2012, 9, CD007146. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for Preventing Falls in Older People Living in the Community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Skelton, D.; Dinan, S.; Campbell, M.; Rutherford, O. Tailored Group Exercise (Falls Management Exercise—FaME) Reduces Falls in Community-Dwelling Older Frequent Fallers (an RCT). Age Ageing 2005, 34, 636–639. [Google Scholar] [CrossRef] [Green Version]
- Tiedemann, A.; Sherrington, C.; Close, J.C.T.; Lord, S.R.; Exercise and Sports Science Australia. Exercise and Sports Science Australia Position Statement on Exercise and Falls Prevention in Older People. J. Sci. Med. Sport 2011, 14, 489–495. [Google Scholar] [CrossRef]
- Touchette, A.J.; Oates, A.R.; Menec, V.H.; Sibley, K.M. Design characteristics and inclusion of evidence-based exercise recommendation in fall prevention community exercise programs for older adults in Canada: A national descriptive self-report study. BMC Geriatr. 2021, 21, 33. [Google Scholar] [CrossRef]
- Binns, E.; Kerse, N.; Peri, K.; Cheung, G.; Taylor, D. Program Fidelity Challenges Discovered during a Feasibility Randomized Controlled Trial of Group Falls Prevention Exercises; SAGE Publications Ltd.: London, UK, 2020. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Cederbom, S.; Tonkonogi, M.; Umb Carlsson, Õ. Older Adults’ Experiences with mHealth for Fall Prevention Exercise: Usability and Promotion of Behavior Change Strategies. Physiother. Theor. Pract. 2021, 37, 1346–1352. [Google Scholar] [CrossRef]
- Yardley, L.; Donovan-Hall, M.; Francis, K.; Todd, C. Older People’s Views of Advice about Falls Prevention: A Qualitative Study. Health Educ. Res. 2006, 21, 508–517. [Google Scholar] [CrossRef]
- Lacroix, A.; Hortobágyi, T.; Beurskens, R.; Granacher, U. Effects of Supervised vs. Unsupervised Training Programs on Balance and Muscle Strength in Older Adults: A Systematic Review and Meta-Analysis. Sports Med. 2017, 47, 2341–2361. [Google Scholar] [CrossRef] [PubMed]
- Leonhardt, R.; Becker, C.; Groß, M.; Mikolaizak, A.S. Impact of the Backward Chaining Method on Physical and Psychological Outcome Measures in Older Adults at Risk of Falling: A Systematic Review. Aging Clin. Exp. Res. 2020, 32, 985–997. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Vakula, M.N.; Bolton, D.A.E.; Dakin, C.J.; Thompson, B.J.; Slocum, T.A.; Teramoto, M.; Bressel, E. Which Exercise Interventions Can Most Effectively Improve Reactive Balance in Older Adults? A Systematic Review and Network Meta-Analysis. Front. Aging Neurosci. 2021, 13, 764826. [Google Scholar] [CrossRef]
- Okubo, Y.; Schoene, D.; Lord, S.R. Step Training Improves Reaction Time, Gait and Balance and Reduces Falls in Older People: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2017, 51, 586–593. [Google Scholar] [CrossRef]
- Schmidt, R.A.; Lee, T.D.; Winstein, C.J.; Wulf, G.; Zelaznik, H.N. Motor Control and Learning: A Behavioral Emphasis, 6th ed.; Human Kinetics Publishers: Champaign, IL, USA, 2019. [Google Scholar]
- Arkkukangas, M.; Bååthe, K.S.; Hamilton, J.; Ekholm, A.; Tonkonogi, M. Feasibility of a Novel Judo4Balance—Fall Preventive Exercise Programme Targeting Community-Dwelling Older Adults. J. Frailty Sarcopenia Falls. 2020, 5, 47–52. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 1994, 49, 85–94. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Strömqvist Bååthe, K.; Ekholm, A.; Tonkonogi, M. Health Promotion and Prevention: The Impact of Specifically Adapted Judo-Inspired Training Program on Risk Factors for Falls among Adults. Prev. Med. Rep. 2020, 19, 101126. [Google Scholar] [CrossRef]
- Franchignoni, F.; Horak, F.; Godi, M.; Nardone, A.; Giordano, A. Using Psychometric Techniques to Improve the Balance Evaluation Systems Test: The Mini-BESTest. J. Rehabil. Med. 2010, 42, 323–331. [Google Scholar] [CrossRef] [Green Version]
- Hellström, K.; Lindmark, B.; Wahlberg, B.; Fugl-Meyer, A.R. Self-Efficacy in Relation to Impairments and Activities of Daily Living Disability in Elderly Patients with Stroke: A Prospective Investigation. J. Rehabil. Med. 2003, 35, 202–207. [Google Scholar] [CrossRef] [Green Version]
- Frändin, K.; Grimby, G. Assessment of Physical Activity, Fitness and Performance in 76-Year-Olds. Scand. J. Med. Sci. Sports 2007, 4, 41–46. [Google Scholar] [CrossRef]
- Szende, A.; Janssen, B.; Cabases, J. (Eds.) Self-Reported Population Health: An International Perspective Based on EQ-5D; Springer: Dordrecht, The Netherlands, 2014. [Google Scholar] [CrossRef] [Green Version]
- Newell, K.M. Motor Skill Acquisition. Annu. Rev. Psychol. 1991, 42, 213–237. [Google Scholar] [CrossRef] [PubMed]
- Moon, Y.; Sosnoff, J.J. Safe Landing Strategies during a Fall: Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2017, 98, 783–794. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Mackey, D.C.; Liu-Ambrose, T.; Feldman, F.; Robinovitch, S.N. Risk Factors for Hip Impact during Real-Life Falls Captured on Video in Long-Term Care. Osteoporos. Int. 2016, 27, 537–547. [Google Scholar] [CrossRef]
- Moon, Y.; Bishnoi, A.; Sun, R.; Shin, J.C.; Sosnoff, J.J. Preliminary Investigation of Teaching Older Adults the Tuck-and-Roll Strategy: Can Older Adults Learn to Fall with Reduced Impact Severity. J. Biomech. 2019, 83, 291–297. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.; Kwok, W.; Wallbank, G.; Tiedemann, A.; Michaleff, Z.A.; Ng, C.A.C.M.; Bauman, A. Evidence on Physical Activity and Falls Prevention for People Aged 65+ Years: Systematic Review to Inform the WHO Guidelines on Physical Activity and Sedentary Behaviour. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 144. [Google Scholar] [CrossRef]
- Arkkukangas, M.; Cederbom, S. Movement toward an Evidence-Based, Digital Fall Prevention Future—Perceptions from a Physiotherapy Perspective. Physiother. Theory Pract. 2021, 1–9. [Google Scholar] [CrossRef]
- Di Lorito, C.; Long, A.; Byrne, A.; Harwood, R.H.; Gladman, J.R.F.; Schneider, S.; Logan, P.; Bosco, A.; van der Wardt, V. Exercise Interventions for Older Adults: A Systematic Review of Meta-Analyses. J. Sport Health Sci. 2021, 10, 29–47. [Google Scholar] [CrossRef]
- Osho, O.; Owoeye, O.; Armijo-Olivo, S. Adherence and Attrition in Fall Prevention Exercise Programs for Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. J. Aging Phys. Act. 2018, 26, 304–326. [Google Scholar] [CrossRef] [Green Version]
- Baldwin, C.E.; Phillips, A.C.; Edney, S.M.; Lewis, L.K. Recommendations for Older Adults’ Physical Activity and Sedentary Behaviour during Hospitalisation for an Acute Medical Illness: An International Delphi Study. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 69. [Google Scholar] [CrossRef]
- Kehler, D.S. The Impact of Sedentary and Physical Activity Behaviour on Frailty in Middle-Aged and Older Adults. Appl. Physiol. Nutr. Metab. 2018, 43, 638. [Google Scholar] [CrossRef] [Green Version]
- Krendl, A.C.; Perry, B.L. The Impact of Sheltering in Place during the COVID-19 Pandemic on Older Adults’ Social and Mental Well-Being. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, 76, e53–e58. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, H.; Yagasaki, K.; Saito, Y.; Oguma, Y. Regular Group Exercise Contributes to Balanced Health in Older Adults in Japan: A Qualitative Study. BMC Geriatr. 2017, 17, 190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gawler, S.; Skelton, D.A.; Dinan-Young, S.; Masud, T.; Morris, R.W.; Griffin, M.; Kendrick, D.; Iliffe, S.; ProAct65+ team. Reducing Falls among Older People in General Practice: The ProAct65+ Exercise Intervention Trial. Arch. Gerontol. Geriatr. 2016, 67, 46–54. [Google Scholar] [CrossRef] [PubMed]
- King, L.A.; Priest, K.C.; Salarian, A.; Pierce, D.; Horak, F.B. Comparing the Mini-BESTest with the Berg Balance Scale to Evaluate Balance Disorders in Parkinson’s Disease. Parkinsons Dis. 2012, 2012, 375419. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar] [CrossRef] [Green Version]
- Wanner, P.; Cheng, F.H.; Steib, S. Effects of acute cardiovascular exercise on motor memory encoding and consolidation: A systematic review with meta-analysis. Neurosci. Biobehav. Rev. 2020, 116, 365–381. [Google Scholar] [CrossRef]
- Parra-Rizo, M.A.; Sanchis-Soler, G. Satisfaction with Life, Subjective Well-Being and Functional Skills in Active Older Adults Based on Their Level of Physical Activity Practice. Int. J. Environ. Res. Public Health 2020, 17, 1299. [Google Scholar] [CrossRef] [Green Version]
- Papp, M.E.; Grahn-Kronhed, A.; Rauch Lundin, H.; Salminen, H. Changes in physical activity levels and relationship to balance performance, gait speed, and self-rated health in older Swedish women: A longitudinal study. Aging Clin. Exp. Res. 2022, 34, 775–783. [Google Scholar] [CrossRef]
| Baseline Characteristic | Total | Exercise Group, Median (Min–Max) | Control Group, Median (Min–Max) |
|---|---|---|---|
| Sex (female/male) | 79%/21% (n = 199) | 76%/24% | 82%/18% |
| Age (mean, SD) | 72 (4, 9) (n = 199) | 72 (4.5) | 73 (5.2) |
| BMI >25 kg/m2 | 52% (n = 196) | 54% | 50% |
| EQ-5D-3L score, mobility (1–3) | 3 (2–3) (n = 197) | 3 (2–3) | 3 (2–3) |
| EQ-5D-3L score, self-care (1–3) | 3 (1–3) (n = 197) | 3 (1–3) | 3 (1–3) |
| EQ-5D-3L score, activity (1–3) | 3 (2–3) (n = 197) | 3 (2–3) | 3 (2–3) |
| EQ-5D-3L score, pain (1–3) | 2 (1–3) (n = 197) | 2 (1–3 | 2 (1–3) |
| EQ-5D-3L score, anxiety (1–3) | 3 (1–3) (n = 196) | 3 (1–3) | 3 (2–3) |
| Rated health status (0–100) | 80 (25–100) (n = 195) | 80 (25–100) | 80 (36–100) |
| Activity level, summer (1–6) | 4 (1–6) (n = 197) | 4 (2–6) | 4 (1–6) |
| Activity level, winter (1–6) | 4 (1–6) (n = 198) | 4 (1–6) | 4 (1–6) |
| FES-S score (0–130) | 127 (52–130) (n = 196) | 126.5 (52–130) | 127 (65–130) |
| SPPB score (0–12) | 11 (2–12) (n = 198) | 11 (2–12) | 11 (5–12) |
| Mini-BESTest score (0–28) | 22 (4–27) (n = 198) | 22 (11–27) | 21 (4–27) |
| Fall competence backward score (0–4) | 1 (0–4) (n = 198) | 1 (0–3) | 1 (0–4) |
| Fall competence forward score (0–4) | 1 (0–4) (n = 197) | 1 (0–3) | 1 (0–4) |
| Fall competence sideways score (0–4) | 1 (0–4) (n = 196) | 1 (0–4) | 1 (0–4) |
| Outcome | Exercise Group | n | p-Value | Control Group | n | p-Value |
|---|---|---|---|---|---|---|
| EQ-5D-3L score, mobility (1–3) | 3 (2–3) | 37 | 0.414 | 3 (2–3) | 41 | 0.564 |
| EQ-5D-3L score, self-care (1–3) | 3 (3–3) | 37 | 0.317 | 3 (3–3) | 41 | 0.180 |
| EQ-5D-3L score, activities (1–3) | 3 (2–3) | 37 | 0.564 | 3 (3–3) | 41 | 1.0 |
| EQ-5D-3L score, pain (1–3) | 2 (1–3) | 37 | 0.366 | 3 (1–3) | 41 | 0.197 |
| EQ-5D-3L score, anxiety (1–3) | 3 (2–3) | 37 | 1.0 | 3 (1–3) | 41 | 0.593 |
| Rated health status (0–100) | 75 (50–99) | 37 | 0.852 | 80 (40–100) | 41 | 0.058 |
| Activity level, summer (1–6) | 4 (2–6) | 37 | 0.140 | 4 (1–6) | 41 | 0.002 |
| Activity level, winter (1–6) | 4 (2–6) | 37 | 0.870 | 4 (1–6) | 42 | 0.003 |
| FES-S score (0–130) | 125 (66–130) | 37 | 0.284 | 124 (66–130) | 41 | 0.563 |
| SPPB score (0–12) | 12 (5–12) | 37 | 0.463 | 11 (6–13) | 42 | 0.248 |
| Mini-BESTest score (0–28) | 22 (6–27) | 37 | 0.696 | 21 (7–27) | 42 | 0.830 |
| Fall competence backward score (0–4) | 1 (0–4) | 37 | 0.011 | 1 (0–4) | 42 | 0.026 |
| Fall competence forward score (0–4) | 1 (0–4) | 37 | 0.029 | 1 (0–3) | 42 | 0.527 |
| Fall competence sideways score (0–4) | 1 (0–4) | 37 | 0.010 | 1 (1–4) | 42 | 0.167 |
| Measurement | Exercise Group | n | p-Value | Control Group | n | p-Value |
|---|---|---|---|---|---|---|
| EQ-5D-3L score, mobility (1–3) | 3 (2–3) | 30 | 0.157 | 3 (2–3) | 28 | 0.564 |
| EQ-5D-3L score, self-care (1–3) | 3 (3–3) | 30 | 1.0 | 3 (3–3) | 28 | 1.0 |
| EQ-5D-3L score, activity (1–3) | 3 (2–3) | 30 | 0.564 | 3 (3–3) | 28 | 1.0 |
| EQ-5D-3L score, pain (1–3) | 2 (1–3) | 30 | 0.180 | 2 (1–3) | 27 | 0.005 |
| EQ-5D-3L score, anxiety (1–3) | 3 (2–3) | 30 | 0.705 | 3 (2–3) | 28 | 0.414 |
| Rated health status (0–100) | 80 (50–98) | 30 | 0.089 | 80 (50–100) | 28 | 0.037 |
| Activity level, summer (1–6) | 4 (3–6) | 31 | 0.022 | 4 (2–6) | 31 | 0.253 |
| Activity level, winter (1–6) | 4 (3–6) | 31 | 0.380 | 4 (2–6) | 31 | 0.490 |
| FES-S score (0–130) | 128 (86–130) | 21 | 0.049 | 127.5 (8–130) | 24 | 0.368 |
| SPPB score (0–12) | 12 (10–12) | 31 | 0.009 | 12 (8–12) | 31 | <0.001 |
| Mini-BESTest score (0–28) | 25 (18–28) | 31 | <0.001 | 24 (18–28) | 31 | <0.001 |
| Fall competence backward score (0–4) | 4 (1–4) | 31 | <0.001 | 4 (1–4) | 31 | <0.001 |
| Fall competence forward score (0–4) | 3 (1–4) | 31 | <0.001 | 3 (1–4) | 31 | <0.001 |
| Fall competence sideways score (0–4) | 3 (1–4) | 28 | <0.001 | 3 (1–4) | 25 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arkkukangas, M.; Strömqvist Bååthe, K.; Ekholm, A.; Tonkonogi, M. High Challenge Exercise and Learning Safe Landing Strategies among Community-Dwelling Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 7370. https://doi.org/10.3390/ijerph19127370
Arkkukangas M, Strömqvist Bååthe K, Ekholm A, Tonkonogi M. High Challenge Exercise and Learning Safe Landing Strategies among Community-Dwelling Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(12):7370. https://doi.org/10.3390/ijerph19127370
Chicago/Turabian StyleArkkukangas, Marina, Karin Strömqvist Bååthe, Anna Ekholm, and Michail Tonkonogi. 2022. "High Challenge Exercise and Learning Safe Landing Strategies among Community-Dwelling Older Adults: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 12: 7370. https://doi.org/10.3390/ijerph19127370
APA StyleArkkukangas, M., Strömqvist Bååthe, K., Ekholm, A., & Tonkonogi, M. (2022). High Challenge Exercise and Learning Safe Landing Strategies among Community-Dwelling Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(12), 7370. https://doi.org/10.3390/ijerph19127370








