Assessing Patient Experience and Attitude: BSC-PATIENT Development, Translation, and Psychometric Evaluation—A Cross-Sectional Study
Abstract
1. Introduction
1.1. Health Care System in Palestine
1.2. History of Balanced Scorecard (BSC)
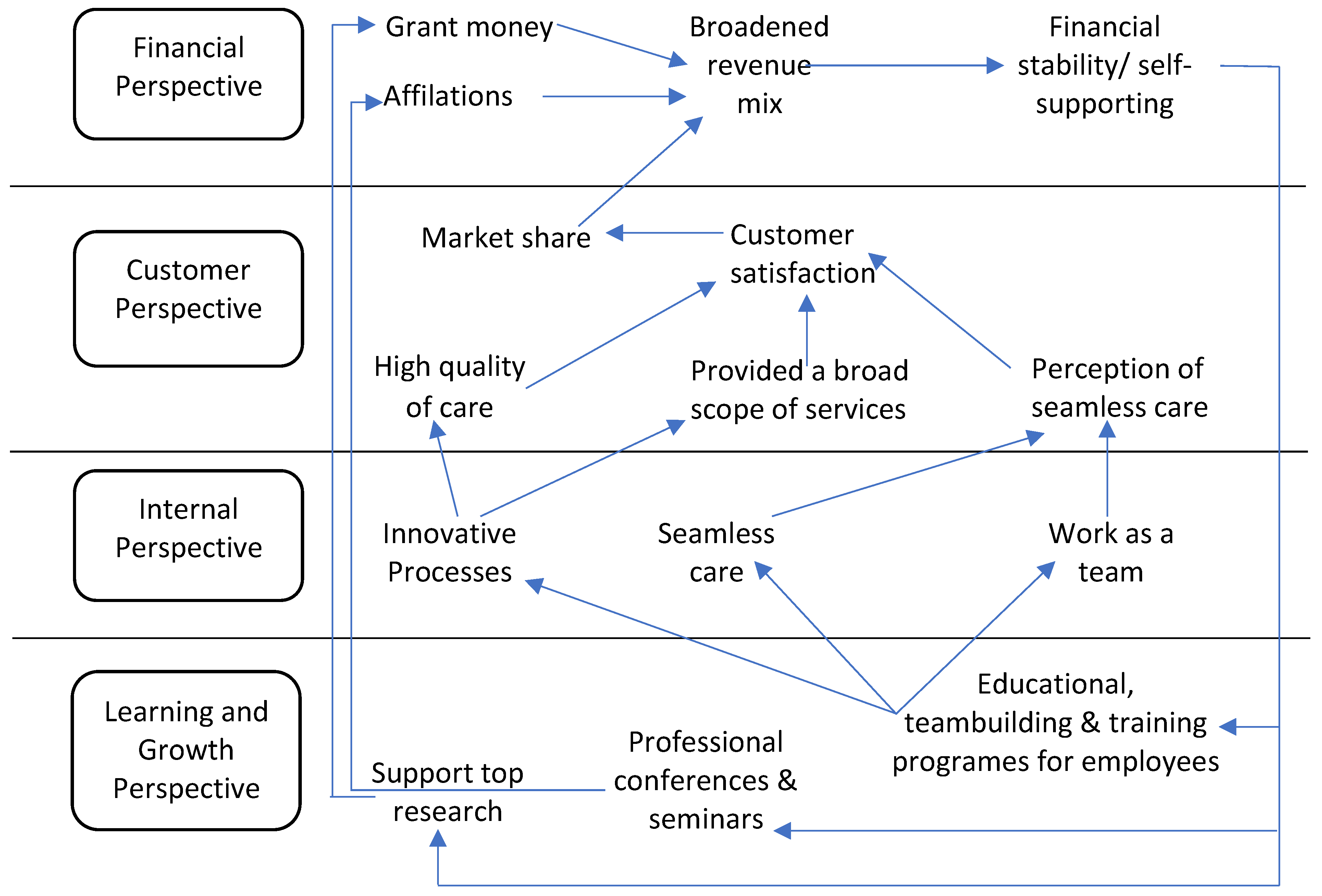
1.3. The Impact of BSC
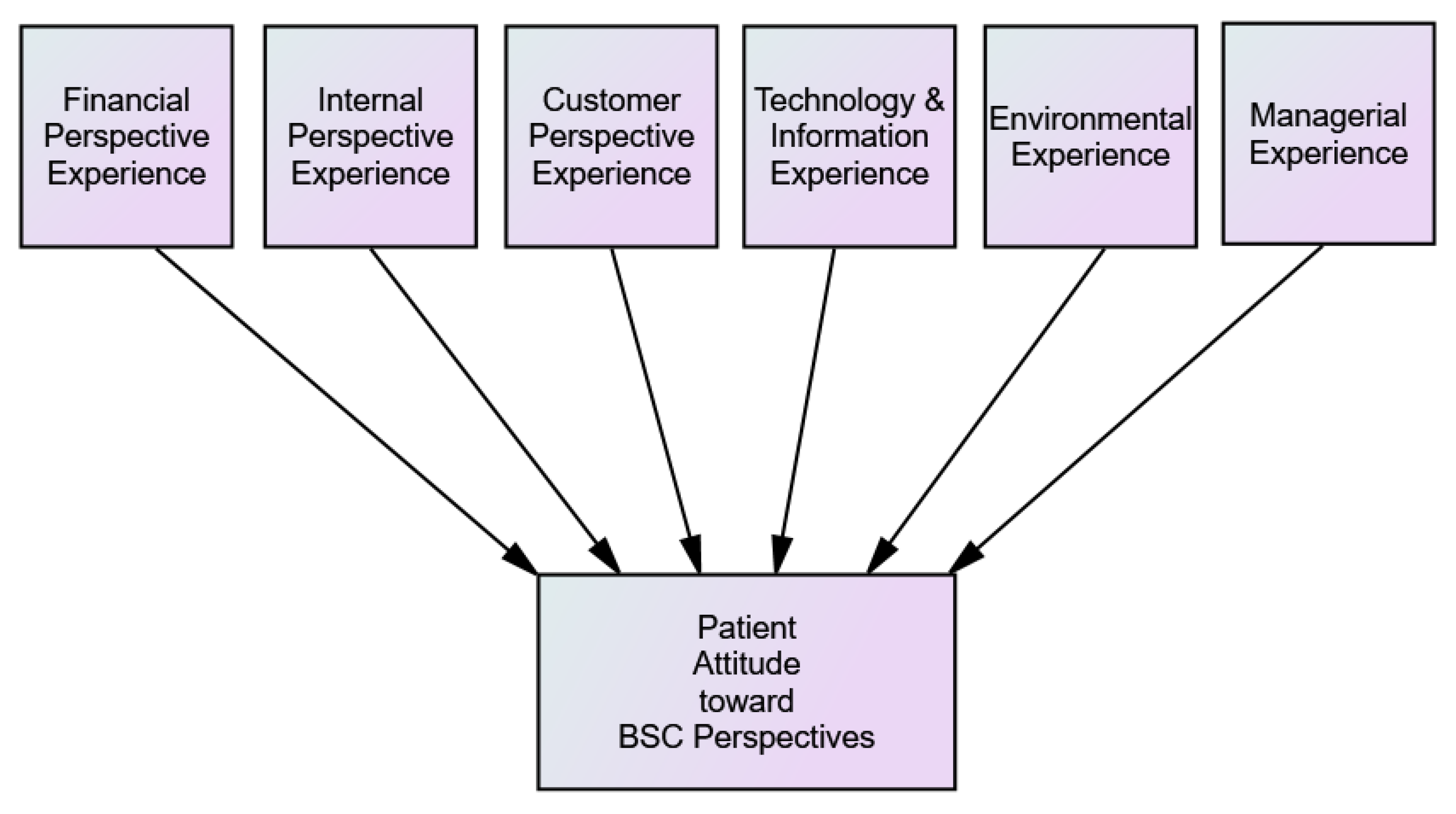
2. The Conceptual Framework
2.1. The Experience
2.2. Attitudes
2.2.1. Patient Satisfaction Attitude
2.2.2. Brand Preference Attitude
2.2.3. Perceived Quality (PQ) Attitude
2.2.4. Perceived Image (PI) Attitude
2.2.5. Loyalty Attitude
Repurchase Intention Attitude
Willingness to Recommend an Attitude
3. Methods
3.1. Research Design
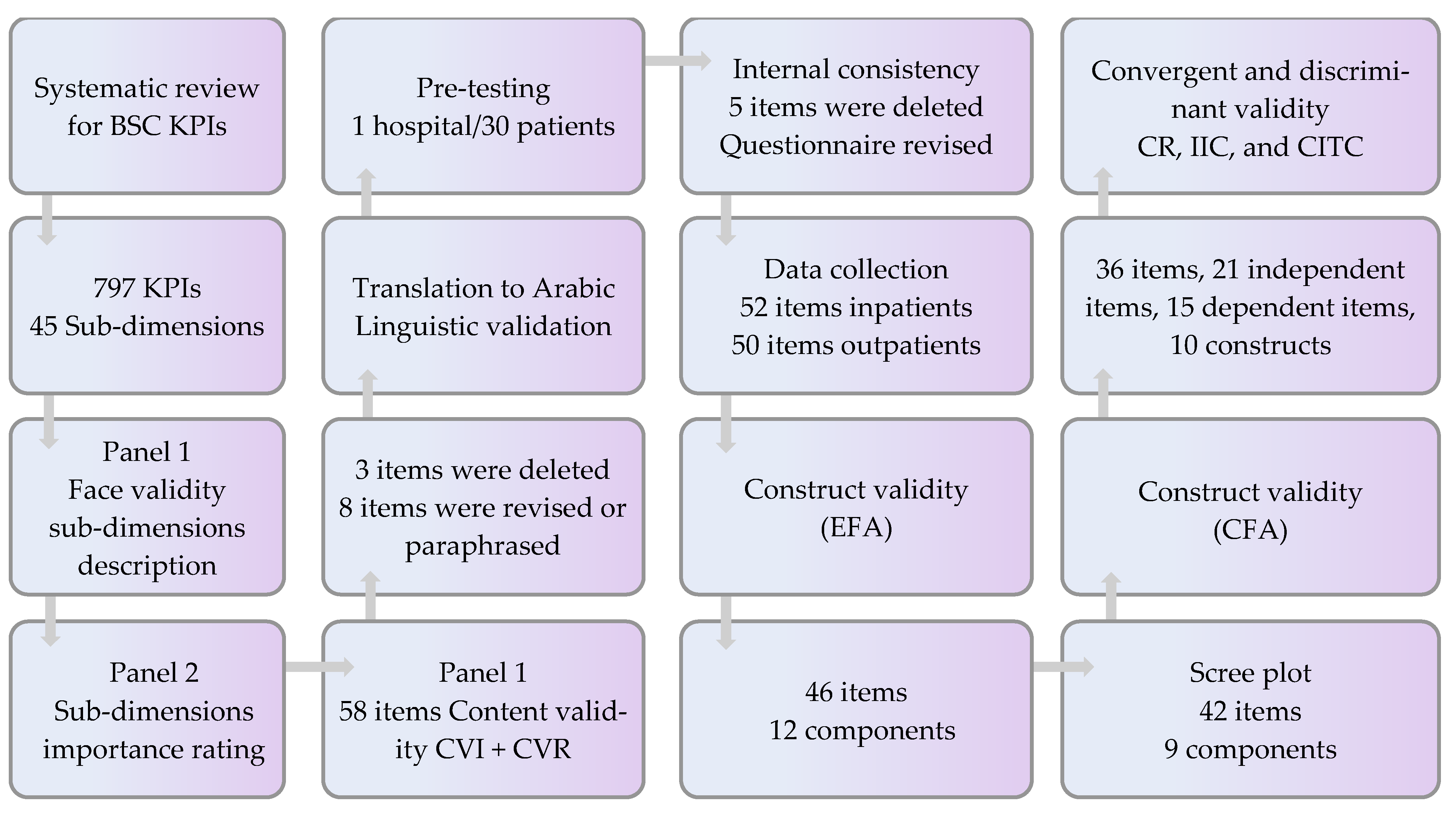
3.2. Item Generation
3.3. Linguistic Validation and Translation
3.4. Pretest and Internal Consistency
3.5. Sampling Procedure and Power Calculation
3.6. Data Collection and Participants
3.7. Statistical Analysis
4. Results
4.1. Item Generation and Scoring
4.2. The Instrument’s Structure and Items
4.2.1. The Financial Perspective
4.2.2. The Internal Perspective
4.2.3. The Knowledge and growth Perspective
4.2.4. The Customer Perspective
4.2.5. The Environmental Perspective
4.2.6. The Managerial Perspective
4.3. The Pretest and the Internal Consistency
4.4. Linguistic Validation and Translation
4.5. Sample Size and Characteristics
4.6. Statistical Analysis
4.6.1. Construct Validity in EFA
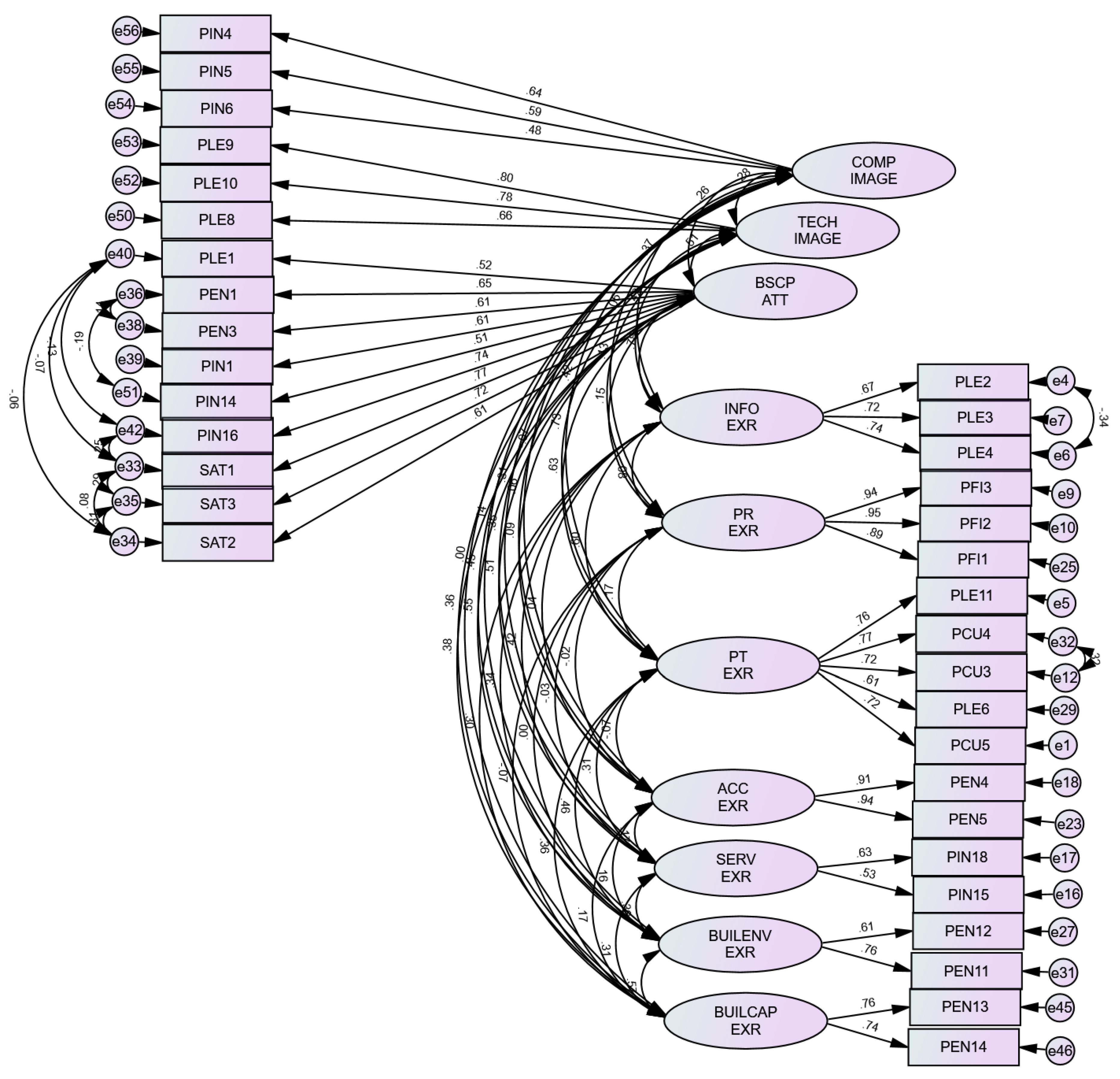
4.6.2. Construct Validity in CFA
4.6.3. Composite Reliability and Interitem Correlations
4.6.4. Convergent and Discriminant Validity
5. Discussion
5.1. Discussion of the Main Results
5.2. Comparison with BSC Implementations
5.3. Comparison with Other Validated Instruments
5.3.1. Service Quality Scale (SERVQUAL)
5.3.2. Press Ganey
5.3.3. Hospital Consumer Assessment of Health Care Providers and Systems (HCAHPS)
5.4. Strengths and Limitations
5.5. Practical Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Code | Question |
|---|---|
| PIN16 | The services provided to me at this hospital have high quality.>> |
| PCU1 | The medical staff at this hospital speaks a simple language with me. |
| PEN10 | The staff at this hospital protects and respect my privacy. |
| PIN19 | The food offered to you at this hospital has high quality. |
| PCU2 | The staff at this hospital are kind, deal with courtesy and respect, and have a good relationship with me and my family. |
| PIN17 | The hospital staff can respond to my inquiries rapidly. |
| PLE8 | I believe this hospital uses the newest technology and devices for diagnosing and treating patients. << |
| PLE5 | Patient counseling services are available at this hospital. |
| PIN14 | I believe the medications prescribed to me at this hospital have good quality and efficacy. >> |
| PIN8 | The doctors and nurses at this hospital spend sufficient time with me. |
| PIN7 | The hospital staff applies safety standards (gloves, masks, hygiene, etc.). |
| PEN15 | My room is calm and peaceful. |
| PIN13 | The medications prescribed to me are available at the hospital’s pharmacy. |
| PLE3 | Oral and written information provided to me or my family during my hospital experience is sufficient. # |
| PLE2 | Information and guidance provided at admission or the first visit are sufficient. # |
| Construct | Code | No. | Question |
|---|---|---|---|
| BSCP ATT | SAT3 | Q1 | I will recommend this hospital to my family and friends. |
| PIN1 | Q2 | I believe I receive an accurate medical examination at this hospital. | |
| PEN2 | Q3 | I will choose this hospital again when I need a medical consultation. | |
| PEN3 | Q4 | I believe this hospital offers me better treatment than the other Palestinian hospitals. | |
| SAT1 | Q5 | My overall satisfaction with this hospital’s performance is high. | |
| PEN1 | Q6 | I believe this hospital has a high cure rate. | |
| SAT2 | Q7 | I will choose this hospital again when I need a medical consultation. | |
| PLE1 | Q8 | I believe the staff at this hospital are competent, knowledgeable, updated, and skilled. | |
| PIN16 | Q9 | The services provided to me at this hospital have high quality. | |
| PIN14 | Q10 | I believe the medications prescribed to me at this hospital have good quality and efficacy. | |
| PT EXR | PCU4 | Q11 | This hospital distributes surveys to assess my satisfaction before discharge. |
| PCU3 | Q12 | This hospital distributes surveys to assess my needs upon arrival to the hospital, admission, or during the stay. | |
| PEN9 | Q13 | Separate male/female waiting area are available at this hospital. | |
| PLE11 | Q14 | This hospital follows up with me after the discharge. | |
| PCU5 | Q15 | My complaints are taken seriously into consideration and solved immediately at this hospital. | |
| PLE7 | Q16 | I can book an online or a phone appointment at this hospital easily. | |
| PLE6 | Q17 | Staff trained me on infection precaution measures such as hand hygiene, cough etiquette, isolation rational, personal protective equipment, etc. | |
| SERV EXR | PEN8 | Q18 | Female doctors are available at this hospital. |
| PIN12 | Q19 | There are a variety of departments at this hospital. | |
| PIN18 | Q20 | Services at night, vacations, and weekends are available at this hospital. | |
| PIN15 | Q21 | There are a variety of specialties at this hospital. | |
| PR EXR | PFI2 | Q22 | I pay a reasonable price for the other medical services (laboratory, radiology, etc.) at this hospital. |
| PFI3 | Q23 | I pay a reasonable price for the medications at this hospital. | |
| PFI1 | Q24 | I pay a reasonable price for the medical consultation at this hospital. | |
| BUIL EXR | PEN13 | Q25 | There is a sufficient number of chairs in the waiting area. |
| PEN12 | Q26 | The hospital has clean departments, corridors, rooms, bathrooms. | |
| PEN14 | Q27 | The capacity of departments at this hospital including (ER, ICU, waiting room, etc.) is sufficient enough. | |
| PEN11 | Q28 | This hospital has new building infrastructure (walls, ceiling, bathrooms, etc.). | |
| ACC EXR | PEN4 | Q29 | The accessibility to this hospital is easy by either public transportation or my car. |
| PEN5 | Q30 | The accessibility to this hospital in an emergency is easy. | |
| COMP IMAGE | PIN6 | Q31 | There is a probability for postoperative bacterial infection at this hospital |
| PIN5 | Q32 | There is a probability for case referral to another hospital | |
| PIN4 | Q33 | There is a probability for case readmission at the same hospital | |
| TECH IMAGE | PLE9 | Q34 | This hospital use technology to link my prescriptions and tests with pharmacy and labs. |
| PLE10 | Q35 | This hospital use technology for saving my records. | |
| PLE8 | Q36 | I believe this hospital uses the newest technology and devices for diagnosing and treating patients. | |
| INFO EXR | PLE4 | Q37 | Information provided to me to be used after discharge is sufficient (medication and side effects, health condition, etc.). |
| PLE3 | Q38 | Oral and written information provided to me or my family during my hospital experience is sufficient. | |
| PLE2 | Q39 | Information and guidance provided at admission or the first visit are sufficient. | |
| HSRP IMAGE | PEN7 | Q40 | I believe this hospital offers social and volunteering activities to the community. |
| PEN6 | Q41 | I believe this hospital offers exemptions for poor patients. | |
| WT EXR | PIN9 | Q42 | I wait for a long time before receiving the medical service at this hospital. |
| Construct | Code | No. | Question |
|---|---|---|---|
| PT EXR | PCU4 | Q1 | This hospital distributes surveys to assess my satisfaction before discharge. |
| PCU3 | Q2 | This hospital distributes surveys to assess my needs upon arrival to the hospital, admission, or during the stay. | |
| PLE11 | Q3 | This hospital follows up with me after the discharge. | |
| PCU5 | Q4 | My complaints are taken seriously into consideration and solved immediately at this hospital. | |
| PLE6 | Q5 | Staff trained me on infection precaution measures such as hand hygiene, cough etiquette, isolation rational, personal protective equipment, etc. | |
| PR EXR | PFI2 | Q6 | I pay a reasonable price for the other medical services (laboratory, radiology, etc.) at this hospital. |
| PFI3 | Q7 | I pay a reasonable price for the medications at this hospital. | |
| PFI1 | Q8 | I pay a reasonable price for the medical consultation at this hospital. | |
| BUILENV EXR | PEN13 | Q9 | There is a sufficient number of chairs in the waiting area. |
| PEN12 | Q10 | The hospital has clean departments, corridors, rooms, bathrooms. | |
| BUILCAP EXR | PEN14 | Q11 | The capacity of departments at this hospital including (ER, ICU, waiting room, etc.) is sufficient enough. |
| PEN11 | Q12 | This hospital has new building infrastructure (walls, ceiling, bathrooms, etc.). | |
| ACC EXR | PEN4 | Q13 | The accessibility to this hospital is easy by either public transportation or my car. |
| PEN5 | Q14 | The accessibility to this hospital in an emergency is easy. | |
| INFO EXR | PLE4 | Q15 | Information provided to me to be used after discharge is sufficient (medication and side effects, health condition, etc.). |
| PLE3 | Q16 | Oral and written information provided to me or my family during my hospital experience is sufficient. | |
| PLE2 | Q17 | Information and guidance provided at admission or the first visit are sufficient. | |
| SERV | PEN8 | Q18 | Female doctors are available at this hospital. |
| PIN12 | Q19 | There are a variety of departments at this hospital. | |
| PIN18 | Q20 | Services at night, vacations, and weekends are available at this hospital. | |
| PIN15 | Q21 | There are a variety of specialties at this hospital. | |
| BSCP ATT | SAT3 | Q22 | I will recommend this hospital to my family and friends. |
| PIN1 | Q23 | I believe I receive an accurate medical examination at this hospital. | |
| PEN3 | Q24 | I believe this hospital offers me better treatment than the other Palestinian hospitals. | |
| SAT1 | Q25 | My overall satisfaction with this hospital’s performance is high. | |
| PEN1 | Q26 | I believe this hospital has a high cure rate. | |
| SAT2 | Q27 | I will choose this hospital again when I need a medical consultation. | |
| PLE1 | Q28 | I believe the staff at this hospital are competent, knowledgeable, updated, and skilled. | |
| PIN16 | Q29 | The services provided to me at this hospital have high quality. | |
| PIN14 | Q30 | I believe the medications prescribed to me at this hospital have good quality and efficacy. | |
| COMP IMAGE | PIN6 | Q31 | There is a probability for postoperative bacterial infection at this hospital |
| PIN5 | Q32 | There is a probability for case referral to another hospital | |
| PIN4 | Q33 | There is a probability for case readmission at the same hospital | |
| TECH IMAGE | PLE9 | Q34 | This hospital use technology to link my prescriptions and tests with pharmacy and labs. |
| PLE10 | Q35 | This hospital use technology for saving my records. | |
| PLE8 | Q36 | I believe this hospital uses the newest technology and devices for diagnosing and treating patients. |
References
- Meena, K.; Thakkar, J. Development of Balanced Scorecard for Healthcare Using Interpretive Structural Modeling and Analytic Network Process. J. Adv. Manag. Res. 2014, 11, 232–256. [Google Scholar] [CrossRef]
- Giacaman, R.; Abdul-Rahim, H.F.; Wick, L. Health Sector Reform in the Occupied Palestinian Territories (OPT): Targeting the Forest or the Trees? Health Policy Plan. 2003, 18, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Barghouthi, M.; Lennock, J. Health in Palestine: Potential and Challenges; Palestine Economic Policy Research Institute (MAS): Jerusalem, Israel, 1997. [Google Scholar]
- PMOH. Health Annual Report, Palestine 2020. May 2021. Available online: https://Moh.Ps (accessed on 10 April 2022).
- Sabella, A.R.; Kashou, R.; Omran, O. Assessing Quality of Management Practices in Palestinian Hospitals. Int. J. Organ. Anal. 2015, 23, 213–232. [Google Scholar] [CrossRef]
- Palestinian News and Info Agency (WAFA) Hospitals in Palestine. Available online: https://info.wafa.ps/ar_page.aspx?id=14977 (accessed on 10 July 2021).
- Regional Health Systems Observatory (EMRO). Health Systems Profile: Palestine; Regional Health Systems Observatory (EMRO): Cairo, Egypt, 2006. [Google Scholar]
- World Health Organisation (WHO). Vulnerability and the International Health Response in the West Bank and Gaza Strip; An Analysis of Health and the Health Sector; World Health Organisation (WHO): Geneva, Switzerland, 2001.
- World Health Organisation (WHO). Health Conditions in the Occupied Palestinian Territory, Including East Jerusalem, and in the Occupied Syrian Golan Report; World Health Organisation (WHO): Geneva, Switzerland, 2020.
- Hammoudeh, W.; Kienzler, H.; Meagher, K.; Giacaman, R. Social and Political Determinants of Health in the Occupied Palestine Territory (OPT) during the COVID-19 Pandemic: Who Is Responsible? BMJ Glob. Health 2020, 5, e003683. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, R.; Norton, D. The Balanced Scorecard-Measures That Drive Performance. Harv. Bus. Rev. 1992, 70, 71–79. [Google Scholar] [PubMed]
- Amer, F.; Hammoud, S.; Khatatbeh, H.; Lohner, S.; Boncz, I.; Endrei, D. A Systematic Review: The Dimensions to Evaluate Health Care Performance and an Implication during the Pandemic. BMC Health Serv. Res. 2022, 22, 621. [Google Scholar] [CrossRef]
- Speckbacher, G.; Bischof, J.; Pfeiffer, T. A Descriptive Analysis on the Implementation of Balanced Scorecards in German-Speaking Countries. Manag. Account. Res. 2003, 14, 361–388. [Google Scholar] [CrossRef]
- Kalender, Z.T.; Vayvay, Ö. The Fifth Pillar of the Balanced Scorecard: Sustainability. Procedia Soc. Behav. Sci. 2016, 235, 76–83. [Google Scholar] [CrossRef]
- Duke-Children’s-Hospital Duke Childrens’ Hospital Case Abstract. Available online: https://thepalladiumgroup.com/download?file=AED_1551102784_116attachment_dubai_boot_camp_-_march_2019_opt.pdf%23Dubai_Boot_Camp_-_March_2019_opt.pdf (accessed on 15 May 2021).
- Rabbani, F.; Jafri, S.M.W.; Abbas, F.; Pappas, G.; Brommels, M.; Tomson, G. Reviewing the Application of the Balanced Scorecard with Implications for Low-Income Health Settings. J. Healthc. Qual. 2007, 29, 21–34. [Google Scholar] [CrossRef]
- Mcdonald, B. A Review of the Use of the Balanced Scorecard in Healthcare. BMcD Consult. 2012, 2012, 1–32. [Google Scholar]
- Kaplan, R.S. Conceptual Foundations of the Balanced Scorecard. Handbooks Manag. Account. Res. 2009, 3, 1253–1269. [Google Scholar] [CrossRef]
- Amer, F.; Hammoud, S.; Khatatbeh, H.; Lohner, S.; Boncz, I.; Endrei, D. The Deployment of Balanced Scorecard in Health Care Organizations: Is It Beneficial? A Systematic Review. BMC Health Serv. Res. 2022, 22, 65. [Google Scholar] [CrossRef]
- Edward, A.; Osei-bonsu, K.; Branchini, C.; Yarghal, T.; Arwal, S.H.; Naeem, A.J. Enhancing Governance and Health System Accountability for People Centered Healthcare: An Exploratory Study of Community Scorecards in Afghanistan. BMC Health Serv. Res. 2015, 15, 299. [Google Scholar] [CrossRef] [PubMed]
- Bohm, V.; Lacaille, D.; Spencer, N.; Barber, C.E. Scoping Review of Balanced Scorecards for Use in Healthcare Settings: Development and Implementation. BMJ Open Qual. 2021, 10, e001293. [Google Scholar] [CrossRef] [PubMed]
- Fields, S.A.; Cohen, D. Performance Enhancement Using a Balanced Scorecard in a Patient-Centered Medical Home. Fam. Med. 2011, 43, 735–739. [Google Scholar] [PubMed]
- Smith, H.; Kim, I. Balanced Scorecard at Summa Health System. J. Corp. Account. Financ. 2005, 16, 65–72. [Google Scholar] [CrossRef]
- Gagliardi, A.R.; Lemieux-Charles, L.; Brown, A.D.; Sullivan, T.; Goel, V. Barriers to Patient Involvement in Health Service Planning and Evaluation: An Exploratory Study. Patient Educ. Couns. 2008, 70, 234–241. [Google Scholar] [CrossRef]
- Anderson, N.N.; Baker, G.R.; Moody, L.; Scane, K.; Urquhart, R.; Wodchis, W.P.; Gagliardi, A.R. Approaches to Optimize Patient and Family Engagement in Hospital Planning and Improvement: Qualitative Interviews. Health Expect. 2021, 24, 967–977. [Google Scholar] [CrossRef]
- Bellows, M.; Kovacs Burns, K.; Jackson, K.; Surgeoner, B.; Gallivan, J. Meaningful and Effective Patient Engagement: What Matters Most to Stakeholders. Patient Exp. J. 2015, 2, 18–28. [Google Scholar] [CrossRef]
- Domecq, J.P.; Prutsky, G.; Elraiyah, T.; Wang, Z.; Nabhan, M.; Shippee, N.; Brito, J.P.; Boehmer, K.; Hasan, R.; Firwana, B.; et al. Patient Engagement in Research: A Systematic Review. BMC Health Serv. Res. 2014, 14, 89. [Google Scholar] [CrossRef]
- David Susman Attitudes and Behavior in Psychology. Available online: https://www.verywellmind.com/ (accessed on 19 February 2022).
- American Psychological Association APA Dictionary of Psychology. Available online: https://dictionary.apa.org/ (accessed on 19 February 2022).
- Keiningham, T.L.; Cooil, B.; Aksoy, L.; Andreassen, T.W.; Weiner, J. The Value of Different Customer Satisfaction and Loyalty Metrics in Predicting Customer Retention, Recommendation, and Share-of-Wallet. Manag. Serv. Qual. Int. J. 2007, 17, 361–384. [Google Scholar] [CrossRef]
- Genoveva, G. Analyzing of Customer Satisfaction and Customer Loyalty Based on Brand Image and Perceived Service Quality. J. US-China Public Adm. 2015, 12, 497–508. [Google Scholar] [CrossRef]
- Zhou, W.-J.; Wan, Q.-Q.; Liu, C.-Y.; Feng, X.-L.; Shang, S.-M. Determinants of Patient Loyalty to Healthcare Providers: An Integrative Review. Int. J. Qual. Health Care 2017, 29, 442–449. [Google Scholar] [CrossRef] [PubMed]
- Taneja, U. Brand Image to Loyalty through Perceived Service Quality and Patient Satisfaction: A Conceptual Framework. Health Serv. Manag. Res. 2021, 34, 250–257. [Google Scholar] [CrossRef] [PubMed]
- Kotler, P.; Clarke, R.N. Marketing for Healthcare Organizations, 1st ed.; Prentice Hall: Englewood Cliffs, NJ, USA, 1987. [Google Scholar]
- Kotler, P.; Keller, K. Marketing Management, 15th ed.; Prentice Hall: Saddle River, NJ, USA, 2014. [Google Scholar]
- Peppers, D. Don Peppers Customer Loyalty: Is It an Attitude? Or a Behavior? Retrieved Febr. 2009, 13, 2012. [Google Scholar]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quiñonez, H.R.; Young, S.L. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef]
- Dalkey, N.; Helmer, O. An Experimental Apllication of Deplhi Method to Use of Experts. Manage. Sci. 1963, 9, 458–467. [Google Scholar] [CrossRef]
- Simbar, M.; Rahmanian, F.; Nazarpour, S.; Ramezankhani, A.; Eskandari, N.; Zayeri, F. Design and Psychometric Properties of a Questionnaire to Assess Gender Sensitivity of Perinatal Care Services: A Sequential Exploratory Study. BMC Public Health 2020, 20, 1063. [Google Scholar] [CrossRef]
- Zamanzadeh, V.; Ghahramanian, A.; Rassouli, M.; Abbaszadeh, A.; Alavi-Majd, H.; Nikanfar, A.-R. Design and Implementation Content Validity Study: Development of an Instrument for Measuring Patient-Centered Communication. J. Caring Sci. 2015, 4, 165–178. [Google Scholar] [CrossRef]
- Lawshe, C.H. A Quantitative Approach to Content Validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- Tyser, A.R.; Abtahi, A.M.; McFadden, M.; Presson, A.P. Evidence of Non-Response Bias in the Press-Ganey Patient Satisfaction Survey. BMC Health Serv. Res. 2016, 16, 350. [Google Scholar] [CrossRef]
- Patel, A.B.; LaCouture, T.; Hunter, K.; Tartaglia, A.; Kubicek, G.J. Pitfalls and Predictors of Poor Press Ganey Patient Satisfaction Scores. Int. J. Radiat. Oncol. 2014, 90, S719–S720. [Google Scholar] [CrossRef]
- Mann, R.K.; Siddiqui, Z.; Kurbanova, N.; Qayyum, R. Effect of HCAHPS Reporting on Patient Satisfaction with Physician Communication. J. Hosp. Med. 2016, 11, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, Z.K.; Wu, A.W.; Kurbanova, N.; Qayyum, R. Comparison of Hospital Consumer Assessment of Healthcare Providers and Systems Patient Satisfaction Scores for Specialty Hospitals and General Medical Hospitals: Confounding Effect of Survey Response Rate. J. Hosp. Med. 2014, 9, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Sousa, V.D.; Rojjanasrirat, W. Translation, Adaptation and Validation of Instruments or Scales for Use in Cross-Cultural Health Care Research: A Clear and User-Friendly Guideline. J. Eval. Clin. Pract. 2011, 17, 268–274. [Google Scholar] [CrossRef]
- Cho, E.; Kim, S. Cronbach’s Coefficient Alpha: Well Known but Poorly Understood. Organ. Res. Methods 2015, 18, 207–230. [Google Scholar] [CrossRef]
- Thompson, S.K. Sampling, 3rd ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012. [Google Scholar]
- Comrey, A.L.; Lee, H.B. A First Course in Factor Analysis; Psychology Press: London, UK, 2013; ISBN 9781315827506. [Google Scholar]
- Williams, B.; Onsman, A.; Brown, T. Exploratory Factor Analysis: A Five-Step Guide for Novices. Australas. J. Paramed. 2010, 8. [Google Scholar] [CrossRef]
- Bentler, P.M.; Chou, C.-P. Practical Issues in Structural Modeling. Sociol. Methods Res. 1987, 16, 78–117. [Google Scholar] [CrossRef]
- Knafl, G.J.; Grey, M. Factor Analysis Model Evaluation through Likelihood Cross-Validation. Stat. Methods Med. Res. 2007, 16, 77–102. [Google Scholar] [CrossRef]
- Sedgwick, P. Non-Response Bias versus Response Bias. BMJ 2014, 348, g2573. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191. [Google Scholar] [CrossRef] [PubMed]
- Mintzberg, H. Mintzberg on Management. Inside Our Strange World of Organizations 1989, New York and London: Free Press/Collier Macmillan. 418 pages. Organ. Stud. 1990, 11, 599. [Google Scholar] [CrossRef]
- Kaiser, H.F.; Rice, J. Little Jiffy, Mark Iv. Educ. Psychol. Meas. 1974, 34, 111–117. [Google Scholar] [CrossRef]
- Larsen, R.; Warne, R.T. Estimating Confidence Intervals for Eigenvalues in Exploratory Factor Analysis. Behav. Res. Methods 2010, 42, 871–876. [Google Scholar] [CrossRef] [PubMed]
- Cattell, R.B. The Scree Test for the Number of Factors. Multivar. Behav. Res. 1966, 1, 245–276. [Google Scholar] [CrossRef]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural Equation Modelling: Guidelines for Determining Model Fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Shi, D.; Lee, T.; Maydeu-Olivares, A. Understanding the Model Size Effect on SEM Fit Indices. Educ. Psychol. Meas. 2019, 79, 310–334. [Google Scholar] [CrossRef]
- Cohen, J. Set Correlation and Contingency Tables. Appl. Psychol. Meas. 1988, 12, 425–434. [Google Scholar] [CrossRef]
- Tavakol, M.; Dennick, R. Making Sense of Cronbach’s Alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef]
- Peterson, R.A.; Kim, Y. On the Relationship between Coefficient Alpha and Composite Reliability. J. Appl. Psychol. 2013, 98, 194–198. [Google Scholar] [CrossRef]
- Ab Hamid, M.R.; Sami, W.; Mohmad Sidek, M.H. Discriminant Validity Assessment: Use of Fornell & Larcker Criterion versus HTMT Criterion. J. Phys. Conf. Ser. 2017, 890, 012163. [Google Scholar] [CrossRef]
- Hair, J.; Hult, G.T.M.; Ringle, C.S.M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); SAGE Publications, Incorporated: Los Angeles, CA, USA, 2014; ISBN 78-1-4522-1744-4. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating Structural Equation Models with Unobservable Variables and Measurement Error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Hair, J.; Wolfinbarger, M.; Money, A.H.; Samouel, P.; Page, M.J. Essentials of Business Research Methods; Routledge: England, UK, 2015; ISBN 9781317471233. [Google Scholar]
- Bookter, A.I. Convergent and Divergent Validity of the Learning Transfer Questionnaire; Louisiana State University: Baton Rouge, LA, USA, 1999. [Google Scholar]
- Willits, F.K.; Theodori, G.L.; Luloff, A.E. Another Look at Likert Scales. J. Rural Soc. Sci. 2016, 31, 126. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff Criteria for Fit Indexes in Covariance Structure Analysis: Conventional Criteria versus New Alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Palestinian Central Bureau of Statistics (PCBS) Percentage Distribution of Current Expenditure on Health in Palestine by Financing Schemes, 2017–2018. Available online: https://www.pcbs.gov.ps/ (accessed on 27 November 2021).
- Rowe, J.S.; Natiq, K.; Alonge, O.; Gupta, S.; Agarwal, A.; Peters, D.H. Evaluating the Use of Locally-Based Health Facility Assessments in Afghanistan: A Pilot Study of a Novel Research Method. Confl. Health 2014, 8, 24. [Google Scholar] [CrossRef][Green Version]
- Khan, M.M.; Hotchkiss, R.D.; Dmytraczenko, T.; Zunaid Ahsan, K. Use of a Balanced Scorecard in Strengthening Health Systems in Developing Countries: An Analysis Based on Nationally Representative Bangladesh Health Facility Survey. Int. J. Health Plan. Manag. 2013, 28, 202–215. [Google Scholar] [CrossRef]
- Peters, D.H.; Noor, A.A.; Singh, L.P.; Kakar, F.K.; Hansen, P.M.; Burnhama, G. A Balanced Scorecard for Health Services in Afghanistan. Bull. World Health Organ. 2007, 85, 146–151. [Google Scholar] [CrossRef]
- Hansen, P.M.; Peters, D.H.; Niayesh, H.; Singh, L.P.; Dwivedi, V.; Burnham, G. Measuring and Managing Progress in the Establishment of Basic Health Services: The Afghanistan Health Sector Balanced Scorecard. Int. J. Health Plan. Manag. 2008, 23, 107–117. [Google Scholar] [CrossRef]
- Josey, C.; Kim, I. Implementation of the Balanced Scorecard at Barberton Citizens Hospital. J. Corp. Account. Financ. 2008, 19, 57–63. [Google Scholar] [CrossRef]
- Edward, A.; Kumar, B.; Kakar, F.; Salehi, A.S.; Burnham, G.; Peters, D.H. Configuring Balanced Scorecards for Measuring Health System Performance: Evidence from 5 Years’ Evaluation in Afghanistan. PLoS Med. 2011, 8, e1001066. [Google Scholar] [CrossRef]
- Mutale, W.; Stringer, J.; Chintu, N.; Chilengi, R.; Mwanamwenge, M.T.; Kasese, N.; Balabanova, D.; Spicer, N.; Lewis, J.; Ayles, H. Application of Balanced Scorecard in the Evaluation of a Complex Health System Intervention: 12 Months Post Intervention Findings from the BHOMA Intervention: A Cluster Randomised Trial in Zambia. PLoS ONE 2014, 9, e93977. [Google Scholar] [CrossRef] [PubMed]
- Rabbani, F.; Pradhan, N.A.; Zaidi, S.; Azam, S.I.; Yousuf, F. Service Quality in Contracted Facilities. Int. J. Health Care Qual. Assur. 2015, 28, 520–531. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Chen, H.; Feng, J.; Qin, X.; Wang, X.; Liang, S.; Zhao, J.; Feng, Q. Balanced Scorecard-Based Performance Evaluation of Chinese County Hospitals in Underdeveloped Areas. J. Int. Med. Res. 2018, 46, 1947–1962. [Google Scholar] [CrossRef] [PubMed]
- Parasuraman, A.; Zeithaml, V.A.; Berry, L.L. A Conceptual Model of Service Quality and Its Implications for Future Research. J. Mark. 1985, 49, 41. [Google Scholar] [CrossRef]
- Ladhari, R. A Review of Twenty Years of SERVQUAL Research. Int. J. Qual. Serv. Sci. 2009, 1, 172–198. [Google Scholar] [CrossRef]
- Buttle, F. SERVQUAL: Review, Critique, Research Agenda. Eur. J. Mark. 1996, 30, 8–32. [Google Scholar] [CrossRef]
- Press Ganey Corporation Press Ganey Associates, Inc. Available online: https://www.pressganey.com/products/patient-experience (accessed on 20 November 2021).
- Centers for Medicare & Medicaid Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). Available online: https://www.ahrq.gov/cahps/surveys-guidance/hospital/about/adult_hp_survey.html (accessed on 27 November 2021).
- Bin Traiki, T.A.; AlShammari, S.A.; AlAli, M.N.; Aljomah, N.A.; Alhassan, N.S.; Alkhayal, K.A.; Al-Obeed, O.A.; Zubaidi, A.M. Impact of COVID-19 Pandemic on Patient Satisfaction and Surgical Outcomes: A Retrospective and Cross Sectional Study. Ann. Med. Surg. 2020, 58, 14–19. [Google Scholar] [CrossRef]

| Sociodemographic Characteristic | Panelists N | % | Sociodemographic Characteristic | Panelists N | % | ||
|---|---|---|---|---|---|---|---|
| Age | Position | ||||||
| 30–39 years | 4 | 30.7 | CMO | 3 | 23.1 | ||
| 40–49 years | 7 | 53.8 | CFO | 3 | 23.1 | ||
| 60–69 years | 2 | 15.4 | CEO | 3 | 23.1 | ||
| Gender | Managing director | 3 | 23.1 | ||||
| Male | 7 | 53.8 | Operation manager | 1 | 7.7 | ||
| Female | 6 | 46.2 | Highest degree | ||||
| Academic background | Bachelor degree | 8 | 61.5 | ||||
| Medicine | 4 | 30.8 | Master’s degree | 5 | 38.5 | ||
| Management | 4 | 30.8 | Administrative type | ||||
| Accounting | 3 | 23.1 | Private | 4 | 30.8 | ||
| Accounting and management | 2 | 15.4 | NGO | 4 | 30.8 | ||
| Years of experience | Public | 5 | 38.5 | ||||
| 5–10 years | 1 | 7.6 | |||||
| More than 10 years | 12 | 92.3 | |||||
| Number of Patients (N = 740) | % | Number of Patients (N = 740) | % | ||||
|---|---|---|---|---|---|---|---|
| Age (years) | Less than 20 | 63 | 8.5 | Income (NIS) | Less than 1000 | 195 | 26.4 |
| 20–29 | 209 | 28.2 | 1000–2000 | 98 | 13.2 | ||
| 30–39 | 208 | 28.1 | 2001–3000 | 152 | 20.5 | ||
| 40–49 | 159 | 21.5 | 3001–4000 | 140 | 18.9 | ||
| 50–59 | 71 | 9.6 | More than 4000 | 155 | 20.9 | ||
| 60–69 | 24 | 3.2 | Insurance type # | Public | 492 | 66.5 | |
| More than 70 | 6 | 0.8 | |||||
| Gender | Females | 325 | 43.9 | Private | 143 | 19.3 | |
| UNRWA | 63 | 8.5 | |||||
| Males | 415 | 56.1 | No insurance | 109 | 14.7 | ||
| Highest degree | Elementary | 85 | 11.5 | Number of the current visit | First | 227 | 30.7 |
| Secondary | 217 | 29.3 | Second | 187 | 25.3 | ||
| Bachelor | 366 | 49.5 | Third | 91 | 12.3 | ||
| Masters | 63 | 8.5 | Fourth | 54 | 7.3 | ||
| PhD | 9 | 1.2 | Fifth | 181 | 24.5 | ||
| Working sector | Public | 175 | 23.6 | Admission status | Inpatients | 350 | 47.3 |
| Private | 183 | 24.7 | Outpatients | 390 | 52.7 | ||
| Free lancer | 156 | 21.1 | Respondent opinion is based on # | Personal experience | 570 | 77 | |
| Retired | 17 | 2.3 | |||||
| Unemployed | 209 | 28.2 | Family experience | 306 | 41.4 | ||
| Friends experience | 96 | 13 |
| Number of Patients (N = 740) | % | Number of Hospitals (N = 14) | % | ||
|---|---|---|---|---|---|
| Administrative Type | Public | 252 | 34.1 | 5 | 36 |
| NGO | 277 | 37.4 | 5 | 36 | |
| private | 159 | 21.5 | 3 | 21 | |
| UNRWA | 52 | 7 | 1 | 7 | |
| City | Hebron | 150 | 20.3 | 3 | 21 |
| Jerusalem | 86 | 11.6 | 1 | 7 | |
| Nablus | 249 | 33.6 | 5 | 36 | |
| Qalqilya | 52 | 7 | 1 | 7 | |
| Ramallah | 151 | 20.4 | 3 | 21 | |
| Tulkarm | 52 | 7 | 1 | 7 | |
| Area | North | 353 | 47.7 | 7 | 50 |
| Middle | 237 | 32 | 4 | 29 | |
| South | 150 | 20.3 | 3 | 21 | |
| Accredited hospital | Yes | 185 | 25 | 3 | 21 |
| No | 555 | 75 | 11 | 79 | |
| Size | Small (No. of beds <80) | 241 | 32.6 | 5 | 36 |
| Medium (No. of beds 80–160) | 261 | 35.3 | 5 | 36 | |
| Large (No. of beds >160) | 238 | 32.2 | 4 | 29 |
| Component | Item | Item Code | Component/Item Loadings | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |||
| BSCP ATT | I will recommend this hospital to my family and friends. | SAT3 | 0.894 | |||||||||||
| I believe I receive an accurate medical examination at this hospital. | PIN1 | 0.783 | ||||||||||||
| I will choose this hospital again when I need a medical consultation. | PEN2 | 0.754 | ||||||||||||
| I believe this hospital offers me better treatment than the other Palestinian hospitals. | PEN3 | 0.686 | ||||||||||||
| My overall satisfaction with this hospital’s performance is high. | SAT1 | 0.683 | ||||||||||||
| I believe this hospital has a high cure rate. | PEN1 | 0.651 | ||||||||||||
| I will choose this hospital again when I need a medical consultation. | SAT2 | 0.579 | 0.556 | |||||||||||
| I believe the staff at this hospital are competent, knowledgeable, updated, and skilled. | PLE1 | 0.537 | ||||||||||||
| PT EXR | This hospital distributes surveys to assess my satisfaction before discharge. | PCU4 | 0.968 | |||||||||||
| This hospital distributes surveys to assess my needs upon arrival to the hospital, admission, or during the stay. | PCU3 | 0.755 | ||||||||||||
| Separate male/female waiting area are available at this hospital. | PEN9 | 0.655 | ||||||||||||
| This hospital follows up with me after the discharge. | PLE11 | 0.645 | ||||||||||||
| My complaints are taken seriously into consideration and solved immediately at this hospital. | PCU5 | 0.601 | ||||||||||||
| I can book an online or a phone appointment at this hospital easily. | PLE7 | 0.586 | ||||||||||||
| Staff trained me on infection precaution measures such as hand hygiene, cough etiquette, isolation rational, personal protective equipment, etc. | PLE6 | 0.560 | ||||||||||||
| SERV EXR | Female doctors are available at this hospital. | PEN8 | 0.625 | |||||||||||
| There are a variety of departments at this hospital. | PIN12 | 0.616 | ||||||||||||
| Services at night, vacations, and weekends are available at this hospital. | PIN18 | 0.556 | ||||||||||||
| There are a variety of specialties at this hospital. | PIN15 | 0.540 | ||||||||||||
| PR EXR | I pay a reasonable price for the other medical services (laboratory, radiology, etc.) at this hospital. | PFI2 | 0.959 | |||||||||||
| I pay a reasonable price for the medications at this hospital. | PFI3 | 0.888 | ||||||||||||
| I pay a reasonable price for the medical consultation at this hospital. | PFI1 | 0.848 | ||||||||||||
| BUIL EXR | There is a sufficient number of chairs in the waiting area. | PEN13 | 0.639 | |||||||||||
| The hospital has clean departments, corridors, rooms, bathrooms. | PEN12 | 0.585 | ||||||||||||
| The capacity of departments at this hospital including (ER, ICU, waiting room, etc.) is sufficient enough. | PEN14 | 0.562 | ||||||||||||
| This hospital has new building infrastructure (walls, ceiling, bathrooms, etc.). | PEN11 | 0.519 | ||||||||||||
| ACC EXR | The accessibility to this hospital is easy by either public transportation or my car. | PEN4 | 0.910 | |||||||||||
| The accessibility to this hospital in an emergency is easy. | PEN5 | 0.907 | ||||||||||||
| COMP IMAGE | There is a probability for postoperative bacterial infection at this hospital | PIN6 | 0.765 | |||||||||||
| There is a probability for case referral to another hospital | PIN5 | 0.752 | ||||||||||||
| There is a probability for case readmission at the same hospital | PIN4 | 0.602 | ||||||||||||
| TECH IMAGE | This hospital use technology to link my prescriptions and tests with pharmacy and labs. | PLE9 | 0.842 | |||||||||||
| This hospital use technology for saving my records. | PLE10 | 0.564 | ||||||||||||
| INFO EXR | Information provided to me to be used after discharge is sufficient (medication and side effects, health condition, etc.). | PLE4 | 0.708 | |||||||||||
| HSRP IMAGE | I believe this hospital offers social and volunteering activities to the community. | PEN7 | 0.601 | |||||||||||
| I believe this hospital offers exemptions for poor patients. | PEN6 | 0.566 | ||||||||||||
| WT EXR | I wait for a long time before receiving the medical service at this hospital. | PIN9 | 0.556 | |||||||||||
| Percentage of Variance (%) Total variance = 63.29% | 27.46 | 5.81 | 5.02 | 3.71 | 3.40 | 3.24 | 2.79 | 2.70 | 2.48 | 2.37 | 2.22 | 2.09 | ||
| Eigenvalues | 14.28 | 3.02 | 2.61 | 1.93 | 1.78 | 1.69 | 1.45 | 1.40 | 1.29 | 1.23 | 1.16 | 1.10 | ||
| EFA [50,57] | CFA [70] | ||
|---|---|---|---|
| Criteria for Good Fit [56,64] | Measurements | Criteria for Good Fit | Measurements |
| -KMO: 0.6: low adequacy 0.7: medium adequacy 0.8: high adequacy 0.9: very high adequacy -Bartlett’s test p value < 0.05 -Inclusion/exclusion criteria for the components:
| -KMO = 0.901 (Chi square = 9052.693, degrees of freedom = 1326) -Bartlett’s test p value < 0.001 -12 components which have Eigenvalues above 1 -Cumulative variance = 63.29% |
| χ2/df = 1.58 p value < 0.001 GFI = 0.901 CFI = 0.953 TLI = 0.944 RMSEA = 0.039 SRMR = 0.0439 |
| Construct | IIC (Min.–Max.) | CTIC (Min.–Max.) | CR | N of Items (Total = 34) |
|---|---|---|---|---|
| COMP IMAGE | 0.395–0.411 | 0.474–0.486 | 0.664 | 3 |
| TECH IMAGE | 0.390–0.594 | 0.486–0.642 | 0.794 | 3 |
| BSCP ATT | 0.328–0.641 | 0.505–0.735 | 0.861 | 9 |
| INFO EXR | 0.389–0.531 | 0.501–0.609 | 0.750 | 3 |
| PR EXR | 0.509–0.725 >> | 0.596–0.760 >> | 0.948 | 3 |
| PT EXR | 0.413–0.678 | 0.552–0.736 | 0.841 | 5 |
| ACC EXR | 0.853 | 0.853 | 0.906 | 2 |
| SERV EXR | 0.360 | 0.360 | 0.502 | 2 |
| BUILENV EXR | 0.412 | 0.412 | 0.643 | 2 |
| BUILCAP EXR | 0.527 | 0.527 | 0.721 | 2 |
| Construct | AVE | INFO EXR | PR EXR | PT EXR | ACC EXR | SERV EXR | BUILENV EXR | BUILCAP EXR |
|---|---|---|---|---|---|---|---|---|
| INFO EXR | 0.501 | 0.708 | ||||||
| PR EXR | 0.858 | 0.084 * | 0.926 | |||||
| PT EXR | 0.515 | 0.507 ** | 0.095 * | 0.718 | ||||
| ACC EXR | 0.828 | 0.121 ** | -0.005 | 0.053 | 0.910 | |||
| SERV EXR | 0.337 | 0.341 ** | 0.002 | 0.242 ** | 0.164 ** | 0.581 | ||
| BUILENV EXR | 0.477 | 0.302 ** | -0.006 | 0.336 ** | 0.110 ** | 0.209 ** | 0.691 | |
| BUILCAP EXR | 0.564 | 0.288 ** | 0.016 | 0.366 ** | 0.164 ** | 0.238 ** | 0.394 ** | 0.751 |
| Construct | AVE | BSCP ATT | TECH IMAGE | COMP IMAGE |
|---|---|---|---|---|
| BSCP ATT | 0.413 | 0.643 | ||
| TECH IMAGE | 0.564 | 0.397 ** | 0.751 | |
| COMP IMAGE | 0.400 | 0.216 ** | 0.156 ** | 0.633 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amer, F.; Hammoud, S.; Onchonga, D.; Alkaiyat, A.; Nour, A.; Endrei, D.; Boncz, I. Assessing Patient Experience and Attitude: BSC-PATIENT Development, Translation, and Psychometric Evaluation—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 7149. https://doi.org/10.3390/ijerph19127149
Amer F, Hammoud S, Onchonga D, Alkaiyat A, Nour A, Endrei D, Boncz I. Assessing Patient Experience and Attitude: BSC-PATIENT Development, Translation, and Psychometric Evaluation—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(12):7149. https://doi.org/10.3390/ijerph19127149
Chicago/Turabian StyleAmer, Faten, Sahar Hammoud, David Onchonga, Abdulsalam Alkaiyat, Abdulnaser Nour, Dóra Endrei, and Imre Boncz. 2022. "Assessing Patient Experience and Attitude: BSC-PATIENT Development, Translation, and Psychometric Evaluation—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 12: 7149. https://doi.org/10.3390/ijerph19127149
APA StyleAmer, F., Hammoud, S., Onchonga, D., Alkaiyat, A., Nour, A., Endrei, D., & Boncz, I. (2022). Assessing Patient Experience and Attitude: BSC-PATIENT Development, Translation, and Psychometric Evaluation—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(12), 7149. https://doi.org/10.3390/ijerph19127149








