Transfusion Trends of Knee Arthroplasty in Korea: A Nationwide Study Using the Korean National Health Insurance Service Sample Data
Abstract
:1. Background
2. Methods
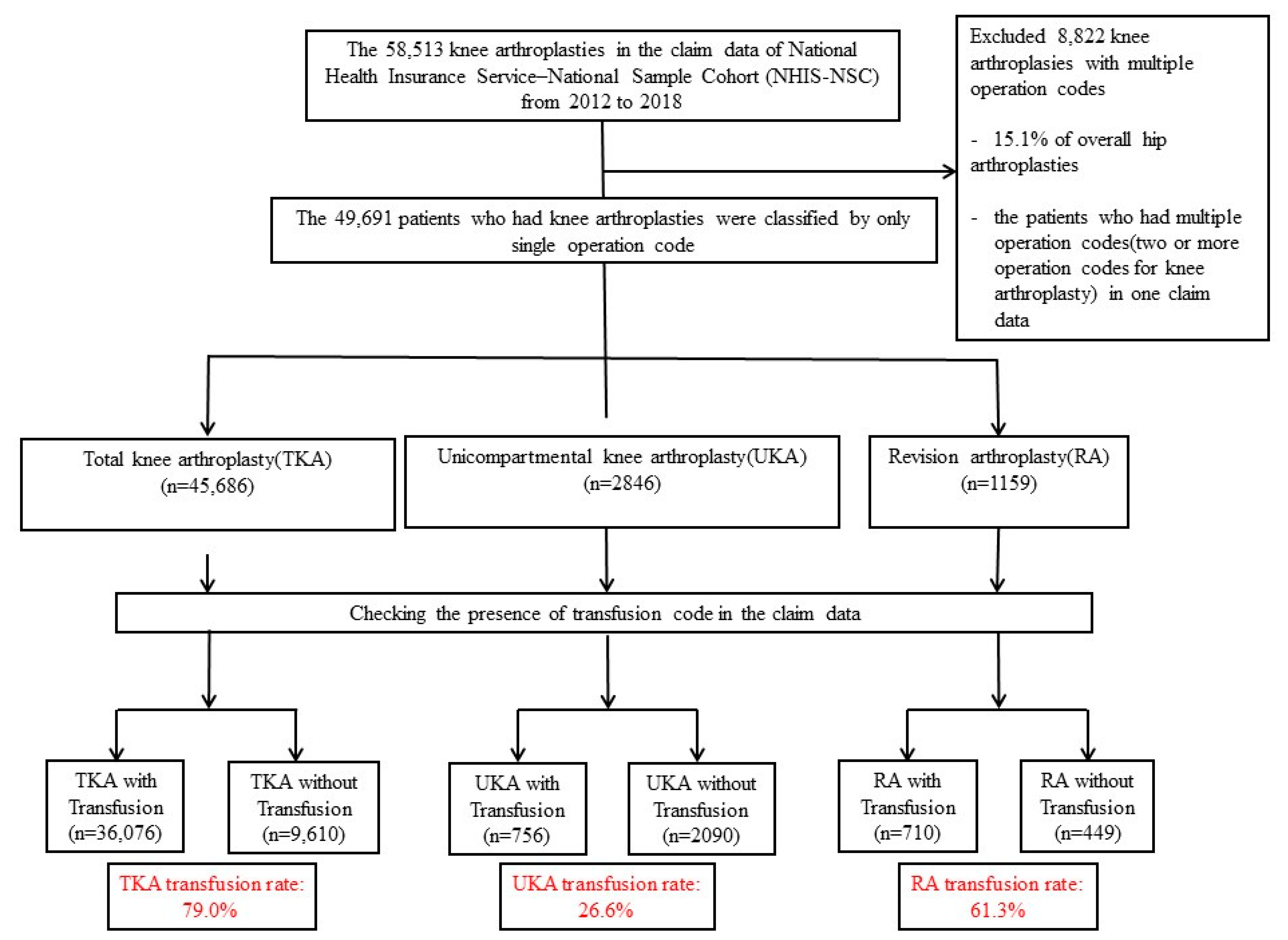
2.1. Subjects
2.2. Transfusion Rates, Amounts, Proportions, and Costs (Economic Burden)
2.3. Statistical Analysis
3. Results
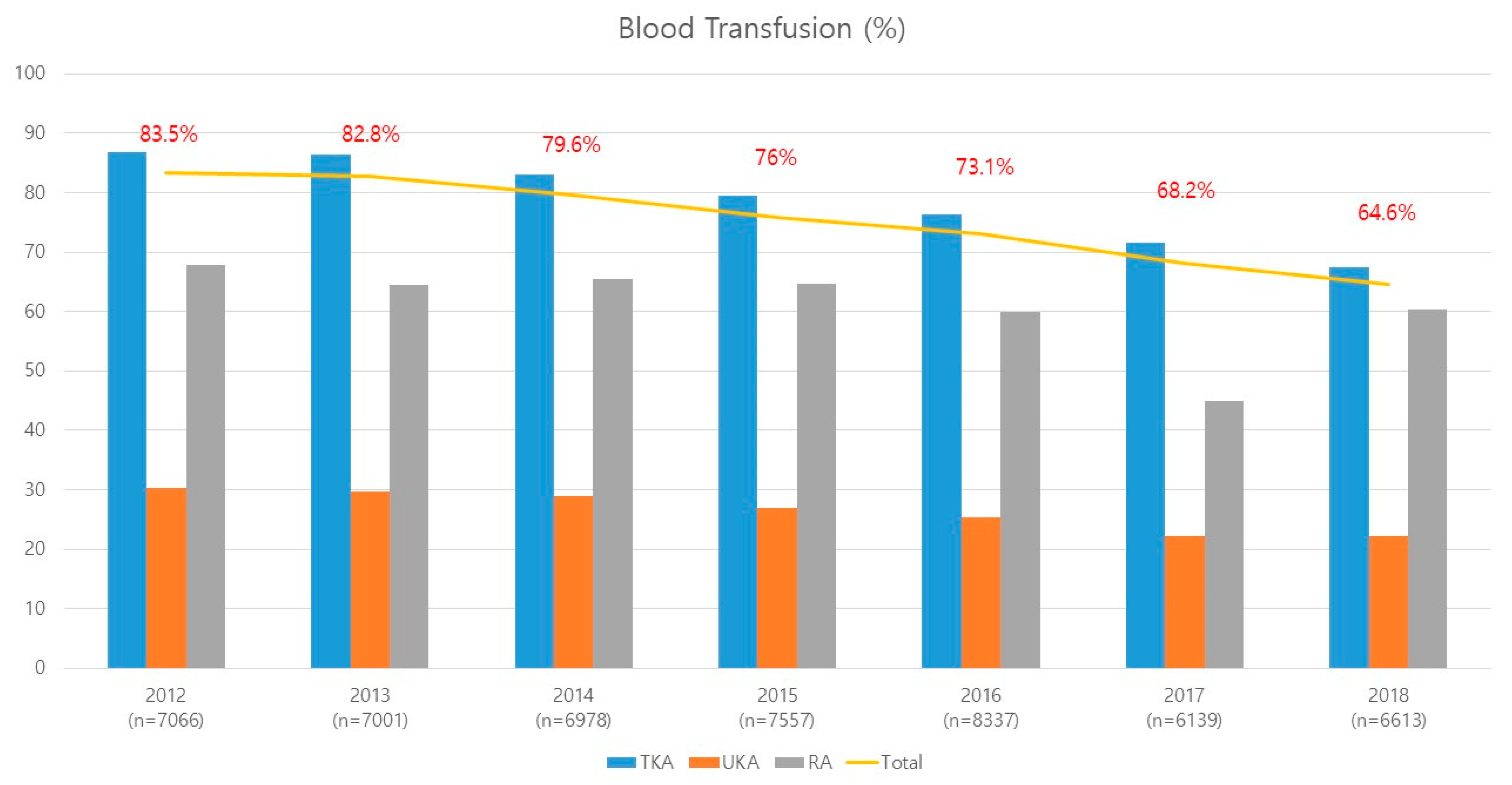
3.1. Transfusion Rates
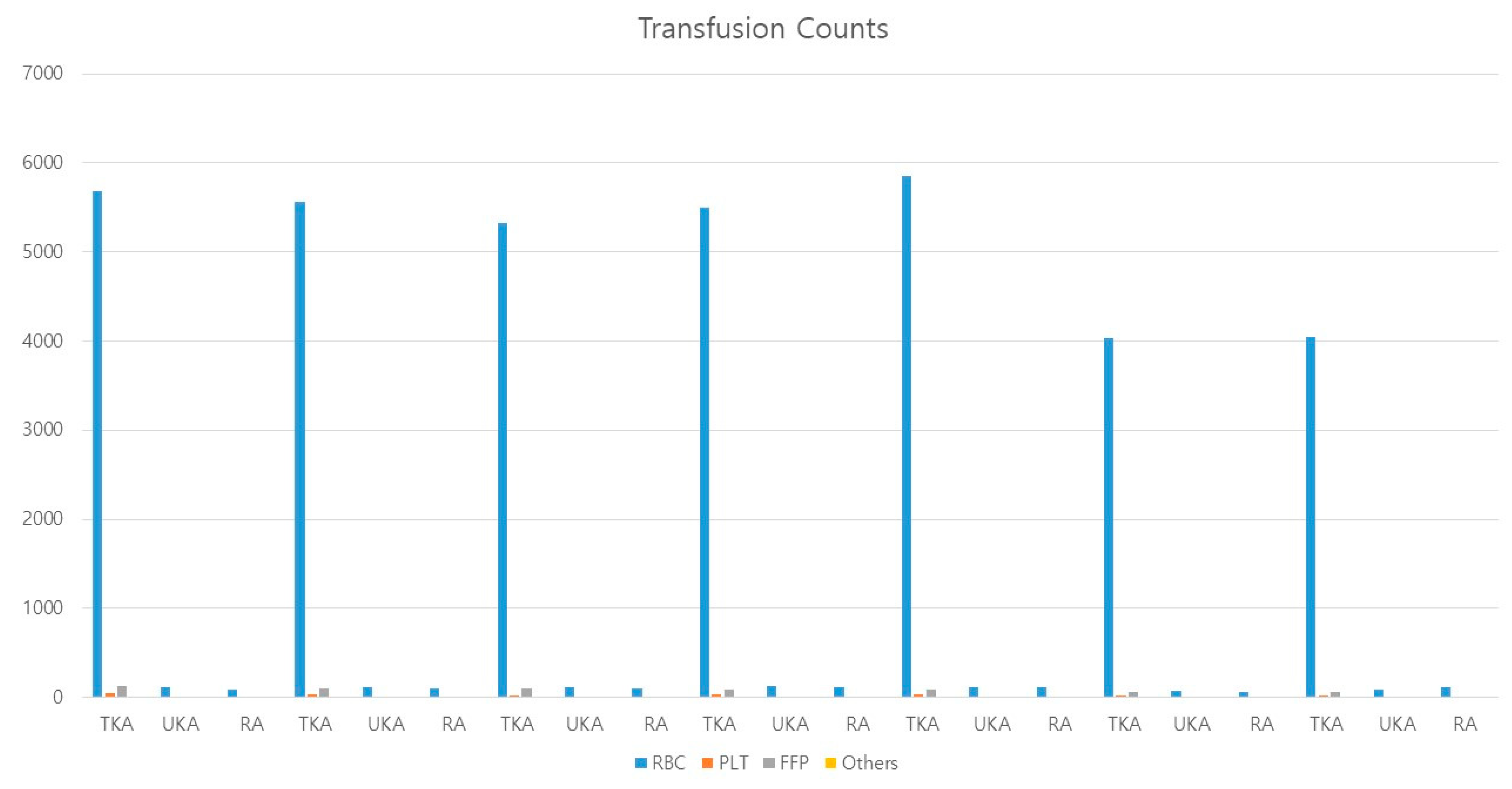
3.2. Transfusion Amounts and Transfusion Costs
| Transfusion | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Total | p-Value † | |
|---|---|---|---|---|---|---|---|---|---|---|
| TKA | Transfused | 5691 | 5576 | 5334 | 5507 | 5857 | 4045 | 4066 | 36,076 | 0.000 |
| Not transfused | 861 | 876 | 1081 | 1417 | 1817 | 1597 | 1961 | 9610 | ||
| UKA | Transfused | 115 | 117 | 115 | 125 | 118 | 80 | 86 | 756 | 0.000 |
| Not transfused | 265 | 277 | 283 | 338 | 345 | 279 | 303 | 2090 | ||
| RA | Transfused | 91 | 100 | 108 | 110 | 120 | 62 | 119 | 710 | 0.000 |
| Not transfused | 43 | 55 | 57 | 60 | 80 | 76 | 78 | 449 | ||
| Total | Transfused | 5897 | 5793 | 5557 | 5742 | 6095 | 4187 | 4271 | 37,542 | 0.000 |
| Not transfused | 1169 | 1208 | 1421 | 1815 | 2242 | 1952 | 2342 | 12,149 | ||
| Percentage (%) | 83.46 | 82.75 | 79.64 | 75.98 | 73.11 | 68.20 | 64.58 | 75.55 | ||
| Subtotal | 7066 | 7001 | 6978 | 7557 | 8337 | 6139 | 6613 | 49,691 | ||
| Multiple operation codes | 825 | 1108 | 1237 | 1441 | 1614 | 1250 | 1347 | 8822 | ||
| Total count | 7891 | 8109 | 8215 | 8998 | 9951 | 7389 | 7960 | 58,513 | ||
| Average cost | $123 | $124 | $123.3 | $110.6 | $100 | $92.9 | $90.1 | $109.1 | ||
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suh, Y.S.; Nho, J.H.; Choi, H.S.; Ha, Y.C.; Park, J.S.; Koo, K.H. A protocol avoiding allogeneic transfusion in joint arthroplasties. Arch. Orthop. Trauma Surg. 2016, 136, 1213–1226. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Rasouli, M.R.; Mortazavi, S.M.; Tokarski, A.T.; Maltenfort, M.G.; Parvizi, J. Predictors of perioperative blood loss in total joint arthroplasty. J. Bone Jt. Surg. 2013, 95, 1777–1783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suh, Y.S.; Nho, J.H.; Seo, J.; Jang, B.W.; Park, J.S. Hip Fracture Surgery without Transfusion in Patients with Hemoglobin Less Than 10 g/dL. Clin. Orthop. Surg. 2021, 13, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Newman, E.T.; Watters, T.S.; Lewis, J.S.; Jennings, J.M.; Wellman, S.S.; Attarian, D.E.; Grant, S.A.; Green, C.L.; Vail, T.P.; Bolognesi, M.P. Impact of perioperative allogeneic and autologous blood transfusion on acute wound infection following total knee and total hip arthroplasty. J. Bone Jt. Surg. 2014, 96, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Friedman, R.; Homering, M.; Holberg, G.; Berkowitz, S.D. Allogeneic blood transfusions and postoperative infections after total hip or knee arthroplasty. J. Bone Jt. Surg. 2014, 96, 272–278. [Google Scholar] [CrossRef] [PubMed]
- Song, J.H.; Park, J.W.; Lee, Y.K.; Kim, I.S.; Nho, J.H.; Lee, K.J.; Park, K.K.; Kim, Y.; Park, J.H.; Han, S.B. Management of Blood Loss in Hip Arthroplasty: Korean Hip Society Current Consensus. Hip Pelvis 2017, 29, 81–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suh, Y.S.; Lee, J.J.; Nho, J.H.; Lee, J.J.; Won, S.H.; Yang, H.J. Transfusion trends in hip arthroplasty in Korea: A nationwide study by the Korean National Health Insurance Service. Transfusion 2019, 59, 2324–2333. [Google Scholar] [CrossRef]
- Kim, Y.B.; Choi, H.S.; Kang, E.M.; Park, S.; Seo, G.W.; Chun, D.I.; Min, T.H. Trends of Total Knee Arthroplasty According to Age Structural Changes in Korea from 2011 to 2018. Int. J. Environ. Res. Public Health 2021, 18, 13397. [Google Scholar] [CrossRef]
- Alshryda, S.; Mason, J.; Vaghela, M.; Sarda, P.; Nargol, A.; Maheswaran, S.; Tulloch, C.; Anand, S.; Logishetty, R.; Stothart, B.; et al. Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: A randomized controlled trial (TRANX-K). J. Bone Jt. Surg. 2013, 95, 1961–1968. [Google Scholar] [CrossRef]
- Oh, J.Y.; Kim, S.M.; Lee, S.A. The Analysis of Hospital Characteristics affecting Blood Transfusion to the patients under Knee or Hip Total Replacement Arthroplasty. J. Korea Acad. Ind. Coop. Soc. 2015, 16, 4031–4039. [Google Scholar]
- Hart, A.; Khalil, J.A.; Carli, A.; Huk, O.; Zukor, D.; Antoniou, J. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Jt. Surg. 2014, 96, 1945–1951. [Google Scholar] [CrossRef] [PubMed]
- Mahringer-Kunz, A.; Efe, T.; Fuchs-Winkelmann, S.; Schuttler, K.F.; Paletta, J.R.; Heyse, T.J. Bleeding in TKA: Posterior stabilized vs. cruciate retaining. Arch. Orthop. Trauma Surg. 2015, 135, 867–870. [Google Scholar] [CrossRef] [PubMed]
- Aguilera, X.; Martinez-Zapata, M.J.; Hinarejos, P.; Jordan, M.; Leal, J.; Gonzalez, J.C.; Monllau, J.C.; Celaya, F.; Rodriguez-Arias, A.; Fernandez, J.A.; et al. Topical and intravenous tranexamic acid reduce blood loss compared to routine hemostasis in total knee arthroplasty: A multicenter, randomized, controlled trial. Arch. Orthop. Trauma Surg. 2015, 135, 1017–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shemshaki, H.; Nourian, S.M.; Nourian, N.; Dehghani, M.; Mokhtari, M.; Mazoochian, F. One step closer to sparing total blood loss and transfusion rate in total knee arthroplasty: A meta-analysis of different methods of tranexamic acid administration. Arch. Orthop. Trauma Surg. 2015, 135, 573–588. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Lee, J.S.; Park, S.H.; Shin, S.A.; Kim, K. Cohort Profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int. J. Epidemiol. 2017, 46, e15. [Google Scholar] [CrossRef]
- Kang, H.Y.; Yang, K.H.; Kim, Y.N.; Moon, S.H.; Choi, W.J.; Kang, D.R.; Park, S.E. Incidence and mortality of hip fracture among the elderly population in South Korea: A population-based study using the national health insurance claims data. BMC Public Health 2010, 10, 230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saleh, A.; Small, T.; Chandran Pillai, A.L.; Schiltz, N.K.; Klika, A.K.; Barsoum, W.K. Allogenic blood transfusion following total hip arthroplasty: Results from the nationwide inpatient sample, 2000 to 2009. J. Bone Jt. Surg. 2014, 96, e155. [Google Scholar] [CrossRef] [Green Version]
- Keating, E.M.; Ritter, M.A. Transfusion options in total joint arthroplasty. J Arthroplast. 2002, 17 (Suppl. 1), 125–128. [Google Scholar] [CrossRef]
- Nuttall, G.A.; Santrach, P.J.; Oliver, W.C., Jr.; Horlocker, T.T.; Shaughnessy, W.J.; Cabanela, M.E.; Bryant, S. The predictors of red cell transfusions in total hip arthroplasties. Transfusion 1996, 36, 144–149. [Google Scholar] [CrossRef]
- Kim, J.L.; Park, J.H.; Han, S.B.; Cho, I.Y.; Jang, K.M. Allogeneic Blood Transfusion Is a Significant Risk Factor for Surgical-Site Infection Following Total Hip and Knee Arthroplasty: A Meta-Analysis. J. Arthroplast. 2017, 32, 320–325. [Google Scholar] [CrossRef]
- Manrique, J.; Chen, A.F.; Gomez, M.M.; Maltenfort, M.G.; Hozack, W.J. Surgical site infection and transfusion rates are higher in underweight total knee arthroplasty patients. Arthroplast. Today 2017, 3, 57–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frisch, N.B.; Wessell, N.M.; Charters, M.A.; Yu, S.; Jeffries, J.J.; Silverton, C.D. Predictors and complications of blood transfusion in total hip and knee arthroplasty. J. Arthroplasty 2014, 29 (Suppl. 9), 189–192. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, N.; Heal, J.M. Immunomodulation by blood transfusion: An evolving scientific and clinical challenge. Am. J. Med. 1996, 101, 299–308. [Google Scholar] [CrossRef]
- Clark, D.A.; Gorczynski, R.M.; Blajchman, M.A. Transfusion-related immunomodulation due to peripheral blood dendritic cells expressing the CD200 tolerance signaling molecule and alloantigen. Transfusion 2008, 48, 814–821. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, R.L. Red blood cell storage and transfusion-related immunomodulation. Blood Transfus. 2010, 8 (Suppl. 3), s26–s30. [Google Scholar]
- Taylor, R.W.; Manganaro, L.; O’Brien, J.; Trottier, S.J.; Parkar, N.; Veremakis, C. Impact of allogenic packed red blood cell transfusion on nosocomial infection rates in the critically ill patient. Crit. Care Med. 2002, 30, 2249–2254. [Google Scholar] [CrossRef]
- Kuduvalli, M.; Oo, A.Y.; Newall, N.; Grayson, A.D.; Jackson, M.; Desmond, M.J.; Fabri, B.M.; Rashid, A. Effect of peri-operative red blood cell transfusion on 30-day and 1-year mortality following coronary artery bypass surgery. Eur. J. Cardio Thorac. Surg. 2005, 27, 592–598. [Google Scholar] [CrossRef]
- Engoren, M.; Mitchell, E.; Perring, P.; Sferra, J. The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J. Trauma 2008, 65, 1411–1415. [Google Scholar] [CrossRef]
- Glance, L.G.; Dick, A.W.; Mukamel, D.B.; Fleming, F.J.; Zollo, R.A.; Wissler, R.; Salloum, R.; Meredith, U.W.; Osler, T.M. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology 2011, 114, 283–292. [Google Scholar] [CrossRef] [Green Version]
- Guerin, S.; Collins, C.; Kapoor, H.; McClean, I.; Collins, D. Blood transfusion requirement prediction in patients undergoing primary total hip and knee arthroplasty. Transfus. Med. 2007, 17, 37–43. [Google Scholar] [CrossRef]
- Shander, A.; Hofmann, A.; Ozawa, S.; Theusinger, O.M.; Gombotz, H.; Spahn, D.R. Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 2010, 50, 753–765. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, A.B.; Mehnert, F.; Overgaard, S.; Johnsen, S.P. Allogeneic blood transfusion and prognosis following total hip replacement: A population-based follow up study. BMC Musculoskelet. Disord. 2009, 10, 167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.K.; Seo, W.Y.; Kim, H.J.; Yoo, J.J. Postoperative Intravenous Ferric Carboxymaltose Reduces Transfusion Amounts after Orthopedic Hip Surgery. Clin. Orthop. Surg. 2018, 10, 20–25. [Google Scholar] [CrossRef] [PubMed]
| Year | Number of Operations | Count of Transfusion Code | RBCs | PLTs | FFP | Others | Total |
|---|---|---|---|---|---|---|---|
| 2012 | 6552 | Total count | 5680 | 47 | 128 | 11 | 5866 |
| Total cost | $723,040 | $248 | $1004 | $4 | $724,296 | ||
| Average cost | $127 | $5 | $8 | $0.39 | $141 | ||
| 2013 | 6452 | Total count | 5569 | 32 | 99 | 7 | 5707 |
| Total cost | $715,433 | 102 | 544 | 2 | $716,081 | ||
| Average cost | $128 | $3 | $5 | $0.31 | $137 | ||
| 2014 | 6415 | Total count | 5325 | 25 | 99 | 12 | 5461 |
| Total cost | $675,466 | $71 | $564 | $6 | $676,107 | ||
| Average cost | $127 | $3 | $6 | $0.50 | $136 | ||
| 2015 | 6924 | Total count | 5498 | 31 | 93 | 13 | 5635 |
| Total cost | $622,231 | $96 | $478 | $6 | $622,811 | ||
| Average cost | $113 | $3 | $5 | $0.45 | $122 | ||
| 2016 | 7674 | Total count | 5857 | 38 | 90 | 7 | 5992 |
| Total cost | $585,740 | $108 | $306 | $1 | $586,155 | ||
| Average cost | $100 | $3 | $3 | $0.15 | $106 | ||
| 2017 | 5642 | Total count | 4038 | 23 | 58 | 7 | 4126 |
| Total cost | $372,154 | $52 | $180 | $2 | $372,388 | ||
| Average cost | $92 | $2 | $3 | $0.26 | $98 | ||
| 2018 | 6027 | Total count | 4051 | 22 | 57 | 5 | 4135 |
| Total cost | $358,552 | $59 | $148 | $1 | $358,760 | ||
| Average cost | $89 | $3 | $3 | $0.28 | $94 |
| Year | Number of Operations | Count of Transfusion Code | RBCs | PLTs | FFP | Others | Total |
|---|---|---|---|---|---|---|---|
| 2012 | 380 | Total count | 114 | 1 | 1 | 0 | 116 |
| Total cost | $2634 | $3 | $1 | $0 | $2638 | ||
| Average cost | $23 | $3 | $1 | $0 | $27 | ||
| 2013 | 394 | Total count | 117 | 0 | 1 | 0 | 118 |
| Total cost | $2412 | $0 | $0 | $0 | $2412 | ||
| Average cost | $21 | $0 | $0 | $0 | $21 | ||
| 2014 | 398 | Total count | 111 | 3 | 4 | 1 | 119 |
| Total cost | $2452 | $10 | $4 | $0 | $2467 | ||
| Average cost | $22 | $3 | $1 | $0.41 | $27 | ||
| 2015 | 463 | Total count | 124 | 2 | 2 | 0 | 128 |
| Total cost | $2865 | $6 | $8 | $0 | $2878 | ||
| Average cost | $23 | $3 | $4 | $0 | $30 | ||
| 2016 | 463 | Total count | 117 | 2 | 1 | 0 | 120 |
| Total cost | $2207 | $5 | $1 | $0 | $2213 | ||
| Average cost | $19 | $2 | $1 | $0 | $22 | ||
| 2017 | 359 | Total count | 79 | 1 | 4 | 0 | 84 |
| Total cost | $1269 | $2 | $8 | $0 | $1280 | ||
| Average cost | $16 | $2 | $2 | $0 | $20 | ||
| 2018 | 389 | Total count | 86 | 0 | 0 | 0 | 86 |
| Total cost | $1368 | $0 | $0 | $0 | $1368 | ||
| Average cost | $16 | $0 | $0 | $0 | $16 |
| Year | Number of Operations | Count of Transfusion Code | RBCs | PLTs | FFP | Others | Total |
|---|---|---|---|---|---|---|---|
| 2012 | 134 | Total count | 90 | 2 | 13 | 1 | 106 |
| Total cost | $12,096 | $85 | $938 | $2 | $13,120 | ||
| Average cost | $134 | $42 | $72 | $2 | $251 | ||
| 2013 | 155 | Total count | 100 | 4 | 7 | 1 | 112 |
| Total cost | $14,088 | $149 | $368 | $7 | $14,612 | ||
| Average cost | $141 | $37 | $53 | $7 | $238 | ||
| 2014 | 165 | Total count | 108 | 3 | 4 | 1 | 116 |
| Total cost | $11,298 | $38 | $65 | $1 | $11,402 | ||
| Average cost | $105 | $13 | $16 | $1 | $135 | ||
| 2015 | 170 | Total count | 109 | 2 | 7 | 1 | 119 |
| Total cost | $9618 | $11 | $69 | $2 | $9700 | ||
| Average cost | $88 | $6 | $10 | $2 | $106 | ||
| 2016 | 200 | Total count | 120 | 3 | 9 | 0 | 132 |
| Total cost | $9859 | $22 | $180 | $0 | $10,061 | ||
| Average cost | $82 | $7 | $20 | $0 | $110 | ||
| 2017 | 138 | Total count | 61 | 1 | 6 | 0 | 68 |
| Total cost | $3863 | $2 | $96 | $0 | $3961 | ||
| Average cost | $63 | $2 | $16 | $0 | $81 | ||
| 2018 | 197 | Total count | 119 | 3 | 10 | 0 | 132 |
| Total cost | $12,176 | $49 | $185 | $0 | $12,410 | ||
| Average cost | $102 | $16 | $19 | $0 | $137 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suh, Y.-S.; Choi, H.-S.; Lee, J.S.; Jang, B.-W.; Hwang, J.; Song, M.G.; Joo, J.; Chung, H.; Lee, J.J.; Nho, J.-H. Transfusion Trends of Knee Arthroplasty in Korea: A Nationwide Study Using the Korean National Health Insurance Service Sample Data. Int. J. Environ. Res. Public Health 2022, 19, 5982. https://doi.org/10.3390/ijerph19105982
Suh Y-S, Choi H-S, Lee JS, Jang B-W, Hwang J, Song MG, Joo J, Chung H, Lee JJ, Nho J-H. Transfusion Trends of Knee Arthroplasty in Korea: A Nationwide Study Using the Korean National Health Insurance Service Sample Data. International Journal of Environmental Research and Public Health. 2022; 19(10):5982. https://doi.org/10.3390/ijerph19105982
Chicago/Turabian StyleSuh, You-Sung, Hyung-Suk Choi, Jeong Seok Lee, Byung-Woong Jang, Jinyeong Hwang, Min Gon Song, Jaeeun Joo, Haran Chung, Jeong Jae Lee, and Jae-Hwi Nho. 2022. "Transfusion Trends of Knee Arthroplasty in Korea: A Nationwide Study Using the Korean National Health Insurance Service Sample Data" International Journal of Environmental Research and Public Health 19, no. 10: 5982. https://doi.org/10.3390/ijerph19105982
APA StyleSuh, Y.-S., Choi, H.-S., Lee, J. S., Jang, B.-W., Hwang, J., Song, M. G., Joo, J., Chung, H., Lee, J. J., & Nho, J.-H. (2022). Transfusion Trends of Knee Arthroplasty in Korea: A Nationwide Study Using the Korean National Health Insurance Service Sample Data. International Journal of Environmental Research and Public Health, 19(10), 5982. https://doi.org/10.3390/ijerph19105982






