The Association between Cardiorespiratory Fitness and Reported Physical Activity with Sleep Quality in Apparently Healthy Adults: A Cross-Sectional Study
Abstract
1. Introduction
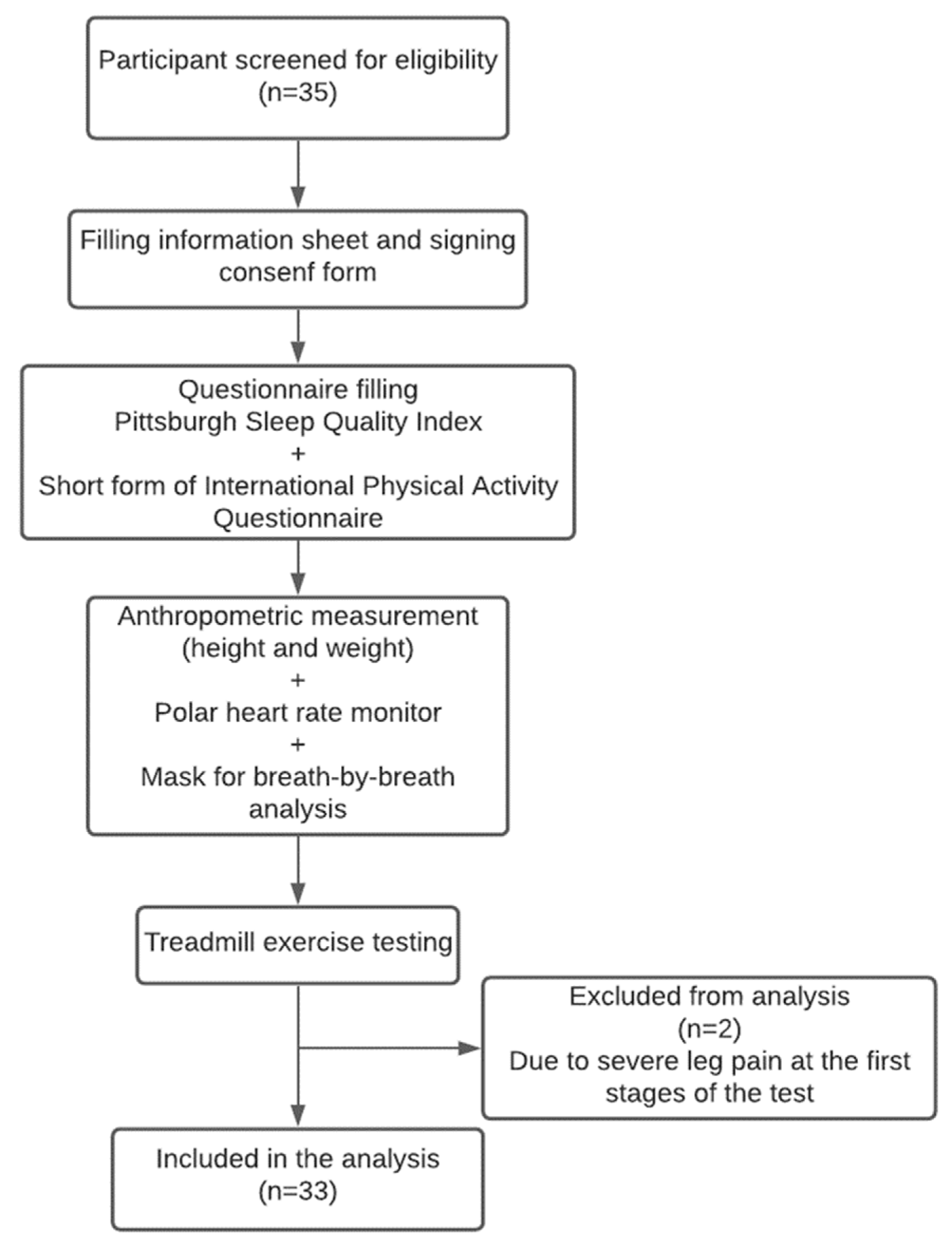
2. Materials and Methods
2.1. Participants
2.2. Protocol
2.3. Graded Exercise Test (GXT) Protocol
2.4. Outcome Measures
2.4.1. Sleep Quality
2.4.2. Physical Activity
2.4.3. Cardiorespiratory Fitness (VO2PEAK)
2.5. Statistical Analysis
3. Results
3.1. Correlation between VO2PEAK and PSQI and Its Components
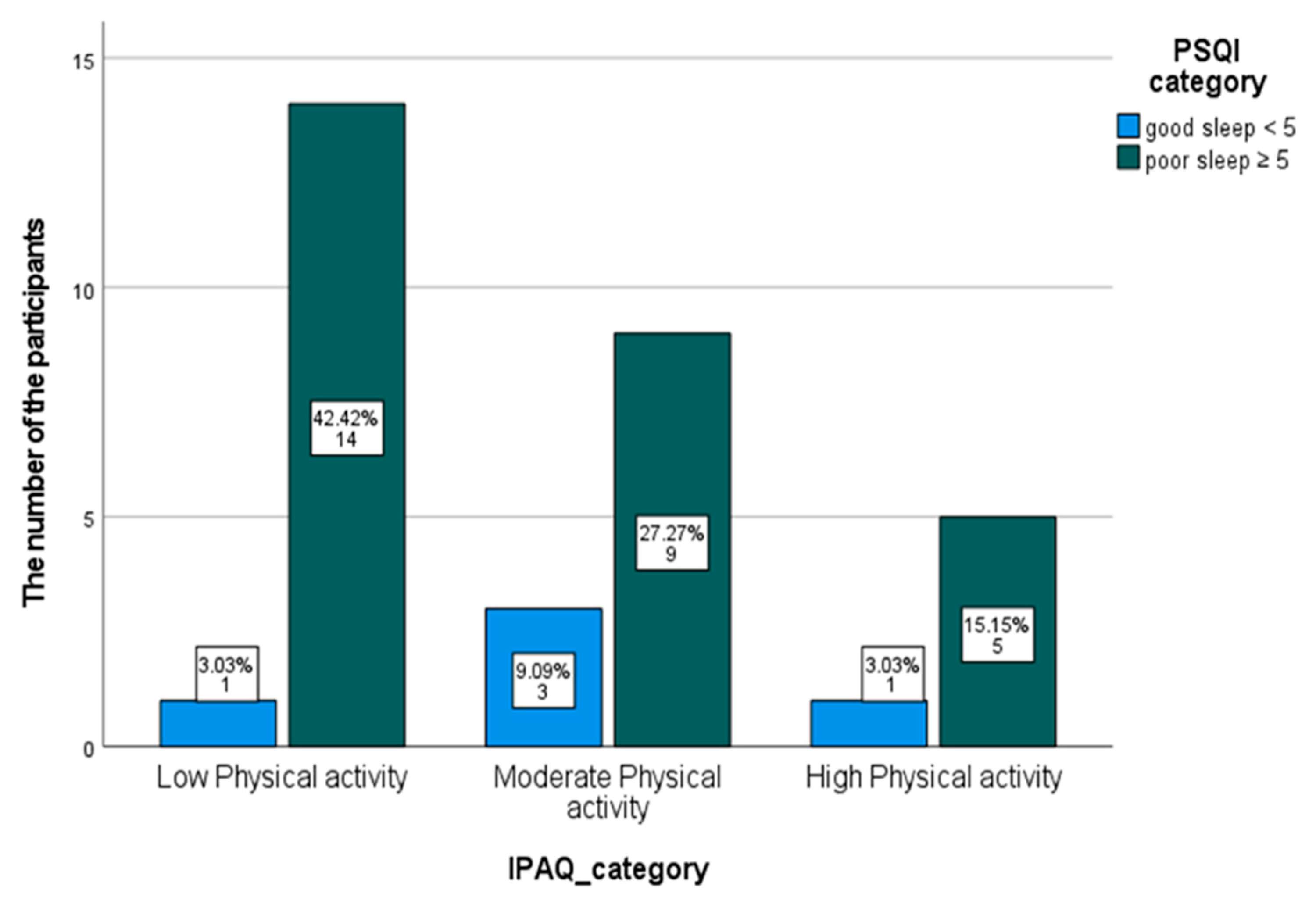
3.2. Cross-Tabulation of the Categorical Data between IPAQ and PSQI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Altevogt, B.M.; Colten, H.R. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Bliwise, D.L. Historical Change in the Report of Daytime Fatigue. Sleep 1996, 19, 462–464. [Google Scholar] [CrossRef]
- Gottlieb, D.J.; Redline, S.; Nieto, F.J.; Baldwin, C.M.; Newman, A.B.; Resnick, H.E.; Punjabi, N.M. Association of Usual Sleep Duration with Hypertension: The Sleep Heart Health Study. Sleep 2006, 29, 1009–1014. [Google Scholar] [CrossRef]
- Knutson, K.L.; Ryden, A.M.; Mander, B.A.; Van Cauter, E. Role of Sleep Duration and Quality in the Risk and Severity of Type 2 Diabetes Mellitus. Arch. Intern. Med. 2006, 166, 1768–1774. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, C.; Gong, W.; Peng, H.; Tang, Y.; Li, C.C.; Zhao, W.; Ye, Z.; Lou, T. Association between Sleep Quality and Cardiovascular Damage in Pre-Dialysis Patients with Chronic Kidney Disease. BMC Nephrol. 2014, 15, 131. [Google Scholar] [CrossRef]
- Lim, S.-T.; Lee, E. Association of Sleep Quality with Cardiorespiratory Fitness in Male High School Students. Indian J. Pediatr. 2020, 87, 954. [Google Scholar] [CrossRef] [PubMed]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep Duration and All-Cause Mortality: A Systematic Review and Meta-Analysis of Prospective Studies. Sleep 2010, 33, 585–592. [Google Scholar] [CrossRef]
- Strand, L.B.; Laugsand, L.E.; Wisløff, U.; Nes, B.M.; Vatten, L.; Janszky, I. Insomnia Symptoms and Cardiorespiratory Fitness in Healthy Individuals: The Nord-Trøndelag Health Study (HUNT). Sleep 2013, 36, 99–108. [Google Scholar] [CrossRef]
- Mota, J.; Vale, S. Associations between Sleep Quality with Cardiorespiratory Fitness and BMI among Adolescent Girls. Am. J. Hum. Biol. Off. J. Hum. Biol. Assoc. 2010, 22, 473–475. [Google Scholar] [CrossRef] [PubMed]
- Al-Mallah, M.H.; Sakr, S.; Al-Qunaibet, A. Cardiorespiratory Fitness and Cardiovascular Disease Prevention: An Update. Curr. Atheroscler. Rep. 2018, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between Sleep and Exercise: A Systematic Review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar]
- Lindegård, A.; Wastensson, G.; Hadzibajramovic, E.; Grimby-Ekman, A. Longitudinal Associations between Cardiorespiratory Fitness and Stress-Related Exhaustion, Depression, Anxiety and Sleep Disturbances. BMC Public Health 2019, 19, 1–13. [Google Scholar] [CrossRef]
- Dishman, R.K.; Sui, X.; Church, T.S.; Kline, C.E.; Youngstedt, S.D.; Blair, S.N. Decline in Cardiorespiratory Fitness and Odds of Incident Sleep Complaints. Med. Sci. Sports Exerc. 2015, 47, 960. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stavrou, V.T.; Astara, K.; Daniil, Z.; Gourgoulianis, K.I.; Kalabakas, K.; Karagiannis, D.; Basdekis, G. The Reciprocal Association between Fitness Indicators and Sleep Quality in the Context of Recent Sport Injury. Int. J. Environ. Res. Public Health 2020, 17, 4810. [Google Scholar] [CrossRef] [PubMed]
- Franklin, B.A.; Whaley, M.H.; Howley, E.T.; Balady, G.J. American College of Sports Medicine: ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins Philadelphia: Philadelphia, PA, USA, 2000. [Google Scholar]
- Bonett, D.G.; Wright, T.A. Sample Size Requirements for Estimating Pearson, Kendall and Spearman Correlations. Psychometrika 2000, 65, 23–28. [Google Scholar] [CrossRef]
- Looney, S.W. Sample Size Determination for Correlation Coefficient Inference: Practical Problems and Practical Solutions. In American Statistical Association 1996 Proceedings of the Section on Statistical Education; American Statistical Association: Alexandria, VA, USA, 1996; pp. 240–245. [Google Scholar]
- Fletcher, G.F.; Balady, G.J.; Amsterdam, E.A.; Chaitman, B.; Eckel, R.; Fleg, J.; Froelicher, V.F.; Leon, A.S.; Piña, I.L.; Rodney, R. Exercise Standards for Testing and Training: A Statement for Healthcare Professionals from the American Heart Association. Circulation 2001, 104, 1694–1740. [Google Scholar] [CrossRef]
- Myers, J.; Bellin, D. Ramp Exercise Protocols for Clinical and Cardiopulmonary Exercise Testing. Sport. Med. 2000, 30, 23–29. [Google Scholar] [CrossRef]
- Backhaus, J.; Junghanns, K.; Broocks, A.; Riemann, D.; Hohagen, F. Test–Retest Reliability and Validity of the Pittsburgh Sleep Quality Index in Primary Insomnia. J. Psychosom. Res. 2002, 53, 737–740. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.-P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef]
- Mondal, H.; Mishra, S.P. Effect of BMI, Body Fat Percentage and Fat Free Mass on Maximal Oxygen Consumption in Healthy Young Adults. J. Clin. Diagn. Res. JCDR 2017, 11, CC17. [Google Scholar] [CrossRef] [PubMed]
- Antunes, B.M.; Campos, E.Z.; Parmezzani, S.S.; Santos, R.V.; Franchini, E.; Lira, F.S. Sleep Quality and Duration Are Associated with Performance in Maximal Incremental Test. Physiol. Behav. 2017, 177, 252–256. [Google Scholar] [CrossRef] [PubMed]
- Mochón-Benguigui, S.; Carneiro-Barrera, A.; Castillo, M.J.; Amaro-Gahete, F.J. Role of Physical Activity and Fitness on Sleep in Sedentary Middle-Aged Adults: The FIT-AGEING Study. Sci. Rep. 2021, 11, 539. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, T. Investigating the Association between Cardiorespiratory Fitness, Sleep, and Cognition in Aging. Doctoral Thesis, McMaster University, Hamilton, ON, Canada, 2020. MacSphere Institutional Repositories. Available online: http://hdl.handle.net/11375/25785 (accessed on 10 January 2021).
- Pina, I.L.; Balady, G.J.; Hanson, P.; Labovitz, A.J.; Madonna, D.W.; Myers, J. Guidelines for Clinical Exercise Testing Laboratories: A Statement for Healthcare Professionals from the Committee on Exercise and Cardiac Rehabilitation, American Heart Association. Circulation 1995, 91, 912–921. [Google Scholar] [CrossRef]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and Exercise: A Reciprocal Issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Mitchell, J.A.; Godbole, S.; Moran, K.; Murray, K.; James, P.; Laden, F.; Hipp, J.A.; Kerr, J.; Glanz, K. No Evidence of Reciprocal Associations between Daily Sleep and Physical Activity. Med. Sci. Sports Exerc. 2016, 48, 1950. [Google Scholar] [CrossRef]
- Sloan, R.A.; Kim, Y.; Sawada, S.S.; Asakawa, A.; Blair, S.N.; Finkelstein, E.A. Is Less Sedentary Behavior, More Physical Activity, or Higher Fitness Associated with Sleep Quality? A Cross-Sectional Study in Singapore. Int. J. Environ. Res. Public Health 2020, 17, 1337. [Google Scholar] [CrossRef]
- Štefan, L.; Sporiš, G.; Krističević, T.; Knjaz, D. Associations between Sleep Quality and Its Domains and Insufficient Physical Activity in a Large Sample of Croatian Young Adults: A Cross-Sectional Study. BMJ Open 2018, 8, e021902. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M. Physical Inactivity in Saudi Arabia Revisited: A Systematic Review of Inactivity Prevalence and Perceived Barriers to Active Living. Int. J. Health Sci. 2018, 12, 50. [Google Scholar]
- Al-Hazzaa, H.M. The Public Health Burden of Physical Inactivity in Saudi Arabia. J. Fam. Community Med. 2004, 11, 45. [Google Scholar]
- Almutairi, K.M.; Alonazi, W.B.; Vinluan, J.M.; Almigbal, T.H.; Batais, M.A.; Alodhayani, A.A.; Alsadhan, N.; Tumala, R.B.; Moussa, M.; Aboshaiqah, A.E. Health Promoting Lifestyle of University Students in Saudi Arabia: A Cross-Sectional Assessment. BMC Public Health 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mahfouz, M.S.; Ageely, H.; Al-Saruri, S.M.; Aref, L.A.; Hejje, N.H.; Al-Attas, S.A.; Bani, I.A. Sleep Quality among Students of the Faculty of Medicine in Jazan University, Saudi Arabia. Middle-East J. Sci. Res. 2013, 16, 508–513. [Google Scholar]
- Spira, A.P.; Beaudreau, S.A.; Stone, K.L.; Kezirian, E.J.; Lui, L.-Y.; Redline, S.; Ancoli-Israel, S.; Ensrud, K.; Stewart, A. Reliability and Validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in Older Men. Journals Gerontol. Ser. A Biomed. Sci. Med. Sci. 2012, 67, 433–439. [Google Scholar]
| Characteristic | Value |
|---|---|
| Age (years) | 23 (22–24) |
| Weight (kg) | 81.9 ± 17.9 |
| Height (m) | 1.72 ± 0.07 |
| BMI (kg/m2) | 27.8 ± 8.7 |
| - Underweight (n, %) | 1, 3% |
| - Normal weight (n, %) | 10, 30.3% |
| - Overweight (n, %) | 12, 36.4% |
| - Obesity class I (n, %) | 7, 21.2% |
| - Obesity class II (n, %) | 1, 3% |
| - Obesity class III (n, %) | 2, 6.1% |
| Smoker (n, %) | 10, 30.3% |
| Sleep and physical activity variables | |
| PSQI total score | 7.3 ± 3.2 |
| IPAQ (MET-min/week) | 1173 (241–2203.5) |
| Hemodynamic variables | |
| Resting HR (bpm) | 77 (70–80) |
| Resting SBP (mmHg) | 127 ± 9.9 |
| Resting DBP (mmHg) | 83 (63–83) |
| HR maximum (bpm) | 169 ± 13.6 |
| HRR1 | 34.2 ± 12.8 |
| Post-exercise test SBP | 153 ± 14.5 |
| Post-exercise test DBP | 88 ± 8.01 |
| RF (b/min) | 39.4 ± 7.14 |
| PETCO2-Resting (mmHg) | 33.3 ± 3.43 |
| PETCO2-Peak (mmHg) | 44.5 ± 3.38 |
| RER | 1.15 ± 0.10 |
| Vt peak (litre) | 2.09 ± 0.45 |
| VE peak (L/min) | 74.04 ± 18.12 |
| VO2 (L/min) | 2.28 ± 0.48 |
| VO2PEAK (ml/kg/min) | 28.4 ± 5.8 |
| Reasons for test termination | |
| Maximum exhaustion (n, %) | 11, 33.3% |
| Lower limb fatigue (n, %) | 13, 39.4% |
| Request to stop (n, %) | 2, 6.1% |
| SOB and HR higher than 90% HRr (n, %) | 2, 6.1% |
| HR higher than 90% of HRr (n, %) | 2, 6.1% |
| Severe SOB | 3, 9.1% |
| Variable | Smokers n = 10 | Non-Smokers n = 23 | p |
|---|---|---|---|
| PSQI | 8 ± 2.4 | 7 ± 3.5 | 0.42 |
| IPAQ (MET-min/week) | 1251.6 ± 1768.4 | 2503 ± 4999.3 | 0.45 |
| VO2PEAK (ml/kg/min) | 26.3 ± 5.9 | 29.2 ± 5.7 | 0.19 |
| Variable | VO2PEAK | |
|---|---|---|
| r | p | |
| Sleep quality | −0.21 | 0.91 |
| Sleep latency | 0.50 | 0.78 |
| Sleep duration | 0.60 | 0.73 |
| Sleep efficiency | −0.15 | 0.40 |
| Sleep disturbances | −0.29 | 0.09 |
| Sleep medication | 0.54 | 0.77 |
| Sleep dysfunction | 0.56 | 0.76 |
| PSQI total score | −0.07 | 0.71 |
| Variable | IPAQ | |
|---|---|---|
| r | p | |
| Sleep quality | −0.18 | 0.31 |
| Sleep latency | 0.03 | 0.89 |
| Sleep duration | −0.28 | 0.12 |
| Sleep efficiency | −0.14 | 0.43 |
| Sleep disturbances | −0.33 | 0.06 |
| Sleep medication | −0.40 | 0.02 |
| Sleep dysfunction | −0.18 | 0.33 |
| PSQI total score | −0.36 | 0.04 |
| IPAQ Category | PSQI Category | Total | |
|---|---|---|---|
| Good Sleep Quality | Poor Sleep Quality | ||
| Low PA n (%) | 1 (6.7%) a | 14 (93.3%) b | 15 (45.5%) c |
| Moderate PA n (%) | 3 (25%) a | 9 (75%) b | 12 (33.3%) c |
| High PA n (%) | 1 (16.7%) a | 5 (83.3%) b | 6 (18.2%) c |
| Total | 5 (15.2%) a | 28 (84.8%) b | 33 |
| Authors and Year | Participants’ Age (Mean or Median) | Body Mass Index Inclusion Criteria | Physical Activity Inclusion Criteria | Graded Exercise Testing | Assessment of Sleep Quality | Assessment of Physical Activity | Cardiorespiratory Fitness Variable | VO2MAX Criteria | Results |
|---|---|---|---|---|---|---|---|---|---|
| Antunes et al. [25] (2017) | 29 years | BMI ≤ 25 kg/m2 | No restrictions | Using cycle ergometer | PSQI | Using IPAQ | VO2MAX | Not fulfilled or mentioned | No association between VO2MAX and sleep quality |
| Mochón-Benguigui et al. [26] (2021) | 53.7 years | BMI between 18.5 and 35 kg/m2 | Sedentary | Using treadmill | Accelerometer + PSQI | Accelerometer | VO2MAX | Fulfilled | Inverse association between VO2MAX and sleep quality |
| Current study | 23 years | No restrictions | No restrictions | Using treadmill | PSQI | Using IPAQ | VO2PEAK | NA | No association between VO2PEAK and sleep quality |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Osailan, A.M.; Elnaggar, R.K.; Alsubaie, S.F.; Alqahtani, B.A.; Abdelbasset, W.K. The Association between Cardiorespiratory Fitness and Reported Physical Activity with Sleep Quality in Apparently Healthy Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 4263. https://doi.org/10.3390/ijerph18084263
Osailan AM, Elnaggar RK, Alsubaie SF, Alqahtani BA, Abdelbasset WK. The Association between Cardiorespiratory Fitness and Reported Physical Activity with Sleep Quality in Apparently Healthy Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(8):4263. https://doi.org/10.3390/ijerph18084263
Chicago/Turabian StyleOsailan, Ahmad M., Ragab K. Elnaggar, Saud F. Alsubaie, Bader A. Alqahtani, and Walid Kamal Abdelbasset. 2021. "The Association between Cardiorespiratory Fitness and Reported Physical Activity with Sleep Quality in Apparently Healthy Adults: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 8: 4263. https://doi.org/10.3390/ijerph18084263
APA StyleOsailan, A. M., Elnaggar, R. K., Alsubaie, S. F., Alqahtani, B. A., & Abdelbasset, W. K. (2021). The Association between Cardiorespiratory Fitness and Reported Physical Activity with Sleep Quality in Apparently Healthy Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 18(8), 4263. https://doi.org/10.3390/ijerph18084263






