Loud Music and Leisure Noise Is a Common Cause of Chronic Hearing Loss, Tinnitus and Hyperacusis
Abstract
1. Introduction
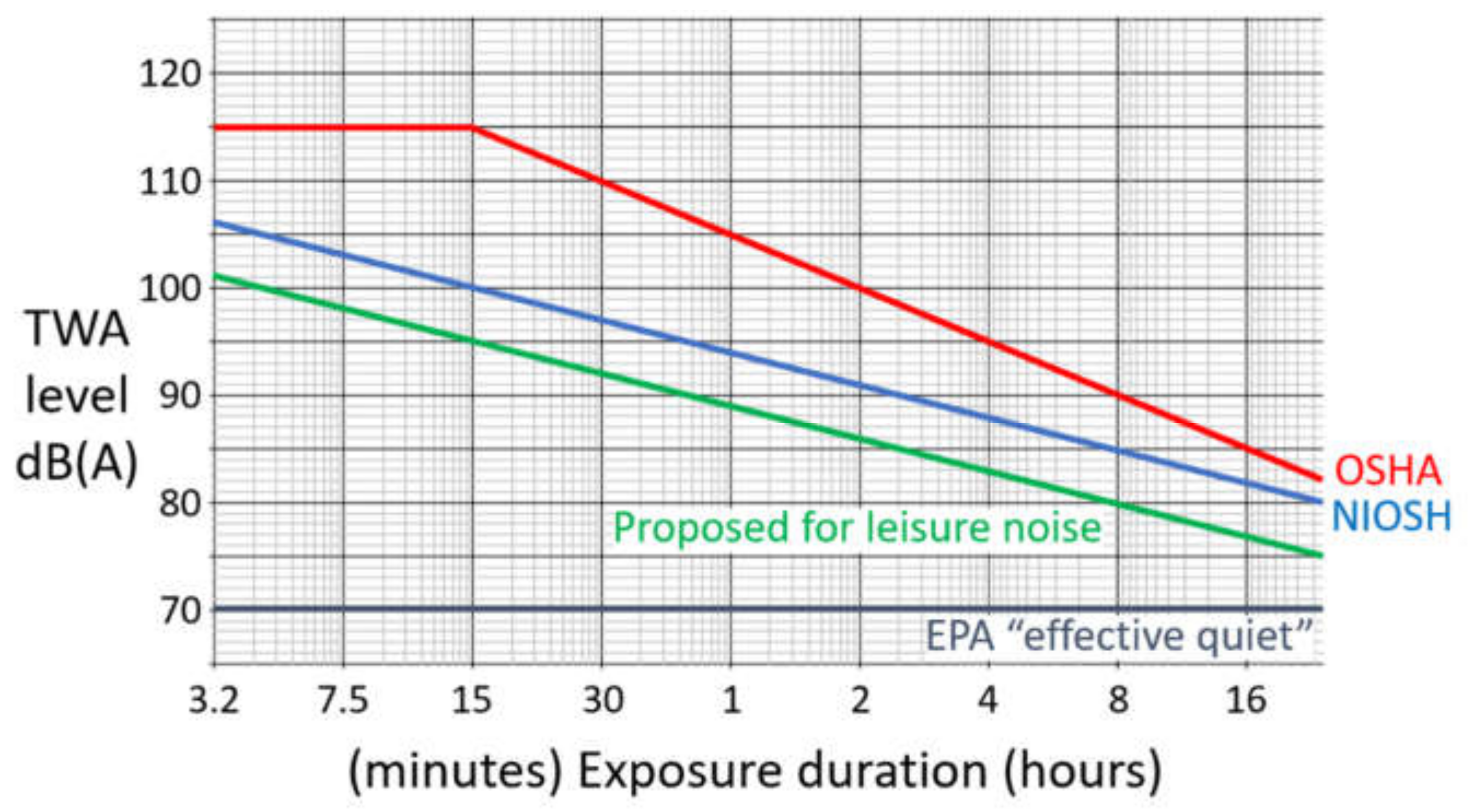
2. A Brief Summary of Occupational Noise Limits in the U.S.A.
3. Loud Music and Leisure Noise Is a Common Cause of Permanent Hearing Loss, Tinnitus, and Hyperacusis
3.1. Live Music Performances and Rehearsals
3.2. Discotheques and Nightclubs
3.3. Personal Listening Devices
3.4. Non-Motorized Sports
3.5. Motorized Sports and Hobbies
3.6. Rifle Shooting
4. Preventing Noise-Induced Hearing Loss
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilbert, D.J. Influence of industrial noises. J. Ind. Hyg. 1922, 3, 264–275. [Google Scholar]
- Bunch, C.C. The diagnosis of occupational or traumatic deafness; A historical and audiometric study. Laryngoscope 1937, 47, 615–691. [Google Scholar]
- Taylor, W.; Pearson, J.; Mair, A.; Burns, W. Study of noise and hearing in jute weaving. J. Acoust. Soc. Am. 1965, 38, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Zhao, F.; Manchaiah, V.K.; French, D.; Price, S.M. Music exposure and hearing disorders: An overview. Int. J. Audiol. 2010, 49, 54–64. [Google Scholar] [CrossRef]
- Le Prell, C.G.; Henderson, D.; Fay, R.R.; Popper, A.N. Noise Induced Hearing Loss: Scientific Advances. In Springer Handbook of Auditory Research; Springer: New York, NY, USA, 2012. [Google Scholar]
- Thurston, F.E. The worker’s ear: A history of noise-induced hearing loss. Am. J. Ind. Med. 2013, 56, 367–377. [Google Scholar] [CrossRef]
- Conroy, K.; Malik, V. Hearing loss in the trenches—a hidden morbidity of World War I. J. Laryngol. Otol. 2018, 132, 952–955. [Google Scholar] [CrossRef]
- Owen, D. Volume Control: Hearing in a Deafening World; Riverhead Books: New York, NY, USA, 2019. [Google Scholar]
- Ampel, F.J.; Uzzle, T. The history of audio and sound measurement. Pro Audio Encyclopedia. 2015. Available online: http://proaudioencyclopedia.com/the-history-of-audio-and-sound-measurement/ (accessed on 15 April 2021).
- Davis, H.; Morgan, C.T.; Hawkins, J.E.; Galambos, R.; Smith, F.W. Final report on temporary deafness following exposure to loud tones and noise. Acta Otolaryngologica 1950, 38, 1–88. [Google Scholar]
- Kryter, K.D.; Ward, W.D.; Miller, J.D.; Eldredge, D.H. Hazardous Exposures to Intermittent and Steady-State Noise. J. Acoust. Soc. Am. 1966, 39, 451–464. [Google Scholar] [CrossRef]
- Burns, W.; Robinson, D.W. Hearing and Noise in Industry; Her Majesty’s Stationery Office: London, UK, 1970. [Google Scholar]
- Passchier-Vermeer, W. Hearing loss due to continuous exposure to steady-state broad-band noise. J. Acoust. Soc. Am. 1974, 56, 1585–1593. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Occupational Safety and Health (NIOSH). Criteria for a Recommended Standard: Occupational Exposure to Noise; DHHS (NIOSH) Publication No. 73-11001; NIOSH: Washington, DC, USA, 1972. [Google Scholar]
- Energy Protection Agency (EPA). Information on Levels of Environmental Noise Requisite to Protect Public Health and Welfare with an Adequate Margin of Safety; Office of Noise Abatement and Control, Environmental Protection Agency: Washington, DC. USA, 1974. [Google Scholar]
- Occupational Safety and Health Administration (OSHA). Occupational noise exposure: Hearing conservation amendment, final rule. Fed. Regist. 1983, 48, 9738–9785. [Google Scholar]
- National Institute for Occupational Safety and Health (NIOSH). Revised Criteria for a Recommended Standard: Occupational Exposure to Noise; DHHS (NIOSH) Publication No. 98–126; NIOSH: Washington, DC, USA, 1998. [Google Scholar]
- Nelson, D.I.; Nelson, R.Y.; Concha-Barrientos, M.; Fingerhut, M. The global burden of occupational noise-induced hearing loss. Am. J. Ind. Med. 2005, 48, 446–458. [Google Scholar] [CrossRef]
- Daniell, W.E.; Swan, S.S.; McDaniel, M.M.; Camp, J.E.; Cohen, M.A.; Stebbins, J.G. Noise exposure and hearing loss prevention programmes after 20 years of regulations in the United States. Occup. Environ. Med. 2006, 63, 343–351. [Google Scholar] [CrossRef]
- Tak, S.; Davis, R.; Calvert, G. Exposure to hazardous workplace noise and use of hearing protection devices among US workers–NHANES, 1999–2004. Am. J. Ind. Med. 2009, 52, 358–371. [Google Scholar] [CrossRef]
- Fuente, A.; Hickson, L. Noise-induced hearing loss in Asia. Int. J. Audiol. 2011, 50, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Yankaskas, K. Prelude: Noise-induced tinnitus and hearing loss in the military. Hear. Res. 2013, 295, 3–8. [Google Scholar] [CrossRef]
- Masterson, E.A.; Tak, S.; Themann, C.L.; Wall, D.K.; Groenewold, M.R.; Deddens, J.A.; Calvert, G.M. Prevalence of hearing loss in the United States by industry. Am. J. Ind. Med. 2013, 56, 670–681. [Google Scholar] [CrossRef]
- Basner, M.; Babisch, W.; Davis, A.; Brink, M.; Clark, C.; Janssen, S.; Stansfeld, S. Auditory and non-auditory effects of noise on health. Lancet 2014, 383, 1325–1332. [Google Scholar] [CrossRef]
- Masterson, E.A.; Sweeney, M.H.; Deddens, J.A.; Themann, C.L.; Wall, D.K. Prevalence of workers with shifts in hearing by industry: A comparison of OSHA and NIOSH Hearing Shift Criteria. J. Occup. Environ. Med. 2014, 56, 446–455. [Google Scholar] [CrossRef]
- Masterson, E.A.; Deddens, J.A.; Themann, C.L.; Bertke, S.; Calvert, G.M. Trends in worker hearing loss by industry sector, 1981–2010. Am. J. Ind. Med. 2015, 58, 392–401. [Google Scholar] [CrossRef]
- Alamgir, H.; Tucker, D.L.; Kim, S.-Y.; Betancourt, J.; Turner, C.; Gorrell, N.S.; Wong, N.J.; Sagiraju, H.K.R.; Cooper, S.P.; Douphrate, D.I.; et al. Economic burden of hearing loss for the U. S. Military: A proposed framework for estimation. Mil. Med. 2016, 181, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Lie, A.; Skogstad, M.; Johannessen, H.A.; Tynes, T.; Mehlum, I.S.; Nordby, K.C.; Engdahl, B.; Tambs, K. Occupational noise exposure and hearing: A systematic review. Int. Arch. Occup. Environ. Health 2016, 89, 351–372. [Google Scholar] [CrossRef] [PubMed]
- Swan, A.A.; Nelson, J.T.; Swiger, B.; Jaramillo, C.A.; Eapen, B.C.; Packer, M.; Pugh, M.J. Prevalence of hearing loss and tinnitus in Iraq and Afghanistan Veterans: A Chronic Effects of Neurotrauma Consortium study. Hear. Res. 2017, 349, 4–12. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Costs of Unaddressed Hearing Loss and Cost-Effectiveness of Interventions; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Wilson, B.S.; Tucci, D.L.; Merson, M.H.; O’Donoghue, G.M. Global hearing health care: New findings and perspectives. Lancet 2017, 390, 2503–2515. [Google Scholar] [CrossRef]
- Kerns, E.; Masterson, E.A.; Themann, C.L.; Calvert, G.M. Cardiovascular conditions, hearing difficulty, and occupational noise exposure within US industries and occupations. Am. J. Ind. Med. 2018, 61, 477–491. [Google Scholar] [CrossRef] [PubMed]
- Graydon, K.; Waterworth, C.; Miller, H.; Gunasekera, H. Global burden of hearing impairment and ear disease. J. Laryngol. Otol. 2019, 133, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Themann, C.L.; Masterson, E.A. Occupational noise exposure: A review of its effects, epidemiology, and impact with recommendations for reducing its burden. J. Acoust. Soc. Am. 2019, 146, 3879–3905. [Google Scholar] [CrossRef]
- Barlow, C.; Castilla-Sanchez, F. Occupational noise exposure and regulatory adherence in music venues in the United Kingdom. Noise Health 2012, 14, 86–90. [Google Scholar] [CrossRef]
- Fosbroke, J. Practical observations on the pathology and treatment of deafness. Lancet 1830, 15, 645–648. [Google Scholar] [CrossRef]
- Chung, D.Y.; Gannon, R.P.; Mason, K. Factors affecting the prevalence of tinnitus. Audiology 1984, 23, 441–452. [Google Scholar] [CrossRef]
- Nondahl, D.M.; Cruickshanks, K.J.; Huang, G.-H.; Klein, B.E.; Klein, R.; Nieto, F.J.; Tweed, T.S. Tinnitus and its risk factors in the Beaver Dam Offspring Study. Int. J. Audiol. 2011, 50, 313–320. [Google Scholar] [CrossRef]
- Bhatt, J.M.; Lin, H.W.; Bhattacharyya, N. Prevalence, severity, exposures, and treatment patterns of tinnitus in the United States. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 959–965. [Google Scholar] [CrossRef]
- Barnea, G.; Attias, J.; Gold, S.; Shahar, A. Tinnitus with normal hearing sensitivity: Extended high-frequency audiometry and auditory-nerve brain-stem-evoked responses. Audiology 1990, 29, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.C.; Lovell, E.A.; Smith, P.A.; Ferguson, M.A. The contribution of social noise to tinnitus in young people—A preliminary report. Noise Health 1998, 1, 40–46. [Google Scholar]
- Griest, S.E.; Bishop, P.M. Tinnitus as an early indicator of permanent hearing loss. A 15 year longitudinal study of noise exposed workers. Workplace Health Safety J. 1998, 46, 325–329. [Google Scholar]
- Holgers, K.M.; Pettersson, B. Noise exposure and subjective hearing symptoms among school children in Sweden. Noise Health 2005, 7, 27–37. [Google Scholar] [CrossRef]
- Sanchez, T.G.; Medeiros, I.R.; Levy, C.P.; Ramalho Jda, R.; Bento, R.F. Tinnitus in normally hearing patients: Clinical aspects and repercussions. Braz. J. Otorhinolaryngol. 2005, 71, 427–431. [Google Scholar] [CrossRef]
- Hind, S.E.; Haines-Bazrafshan, R.; Benton, C.L.; Brassington, W.; Towle, B.; Moore, D.R. Prevalence of clinical referrals having hearing thresholds within normal limits. Int. J. Audiol. 2011, 50, 708–716. [Google Scholar] [CrossRef]
- Kumar, U.A.; Ameenudin, S.; Sangamanatha, A.V. Temporal and speech processing skills in normal hearing individuals exposed to occupational noise. Noise Health 2012, 14, 100–105. [Google Scholar]
- Beach, E.F.; Williams, W.; Gilliver, M. Estimating young Australian adults’ risk of hearing damage from selected leisure activities. Ear. Hear. 2013, 34, 75–82. [Google Scholar] [CrossRef]
- Tung, C.-Y.; Chao, K.-P. Effect of recreational noise exposure on hearing impairment among teenage students. Res. Dev. Disab. 2013, 34, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Sheldrake, J.; Diehl, P.U.; Schaette, R. Audiometric characteristics of hyperacusis patients. Front. Neurol. 2015, 6, 105. [Google Scholar] [CrossRef]
- Tremblay, K.L.; Pinto, A.; Fischer, M.E.; Klein, B.E.; Klein, R.; Levy, S.; Tweed, T.S.; Cruickshanks, K.J. Self-Reported Hearing Difficulties Among Adults With Normal Audiograms: The Beaver Dam Offspring Study. Ear. Hear. 2015, 36, 290–299. [Google Scholar] [CrossRef]
- Guest, H.; Munro, K.J.; Prendergast, G.; Howe, S.; Plack, C.J. Tinnitus with a normal audiogram: Relation to noise exposure but no evidence for cochlear synaptopathy. Hear. Res. 2017, 344, 265–274. [Google Scholar] [CrossRef]
- Moore, D.R.; Zobay, O.; Mackinnon, R.C.; Whitmer, W.M.; Akeroyd, M.A. Lifetime leisure music exposure associated with increased frequency of tinnitus. Hear. Res. 2017, 347, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Parthasarathy, A.; Hancock, K.E.; Bennett, K.; DeGruttola, V.; Polley, D.B. Bottom-up and top-down neural signatures of disordered multi-talker speech perception in adults with normal hearing. Elife 2020, 9, e51419. [Google Scholar] [CrossRef]
- Clark, W.W.; Bohne, B.A.; Boettcher, F.A. Effect of periodic rest on hearing loss and cochlear damage following exposure to noise. J. Acoust. Soc. Am. 1987, 82, 1253–1264. [Google Scholar] [CrossRef]
- Subramaniam, M.; Salvi, R.J.; Spongr, V.P.; Henderson, D.; Powers, N.L. Changes in distortion product otoacoustic emissions and outer hair cells following interrupted noise exposures. Hear. Res. 1994, 74, 204–216. [Google Scholar] [CrossRef]
- Withnell, R.H. The cochlear microphonic as an indication of outer hair cell function. Ear. Hear. 2001, 22, 75–77. [Google Scholar] [CrossRef]
- Chen, G.D.; Fechter, L.D. The relationship between noise-induced hearing loss and hair cell loss in rats. Hear. Res. 2003, 177, 81–90. [Google Scholar] [CrossRef]
- Schuknecht, H.F.; Woellner, R.C. Hearing losses following partial section of the cochlear nerve. Laryngoscope 1953, 63, 441–465. [Google Scholar] [CrossRef]
- Kujawa, S.G.; Liberman, M.C. Adding insult to injury: Cochlear nerve degeneration after “temporary” noise-induced hearing loss. J. Neurosci. 2009, 29, 14077–14085. [Google Scholar] [CrossRef]
- Lin, H.W.; Furman, A.C.; Kujawa, S.G.; Liberman, M.C. Primary neural degeneration in the guinea pig cochlea after reversible noise-induced threshold shift. J. Assoc. Res. Otolaryngol. 2011, 12, 605–616. [Google Scholar] [CrossRef]
- Wang, Y.; Ren, C. Effects of repeated "benign" noise exposures in young CBA mice: Shedding light on age-related hearing loss. J. Assoc. Res. Otolaryngol. 2012, 13, 505–515. [Google Scholar] [CrossRef]
- Lobarinas, E.; Salvi, R.; Ding, D. Insensitivity of the audiogram to carboplatin induced inner hair cell loss in chinchillas. Hear Res 2013, 302, 113–120. [Google Scholar] [CrossRef]
- Chambers, A.R.; Resnik, J.; Yuan, Y.; Whitton, J.P.; Edge, A.S.; Liberman, M.C.; Polley, D.B. Central gain restores auditory processing following near-complete cochlear denervation. Neuron 2016, 89, 867–879. [Google Scholar] [CrossRef]
- Pienkowski, M. On the etiology of listening difficulties in noise despite clinically normal audiograms. Ear Hear. 2017, 38, 135–148. [Google Scholar] [CrossRef]
- Welch, D.; Fremaux, G. Why Do People Like Loud Sound? A Qualitative Study. Int. J. Environ. Res. Public Health 2017, 14, 908. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.H.; Des Roches, C.M.; Meunier, J.; Eavey, R.D. Evaluation of noise-induced hearing loss in young people using a web-based survey technique. Pediatrics 2005, 115, 861–867. [Google Scholar] [CrossRef]
- Jones, P. Tinnitus: Warning for Music Fans Attending Concerts. BBC Wales News, 12 July 2019. Available online: https://www.bbc.com/news/uk-wales-47948065?fbclid=IwAR3SLyZXar1ol2SBT-AO-usqSMCiaF_zpB5j7d3Qx8b31niLCtu8gMg-HCg (accessed on 15 April 2021).
- Neitzel, R.L.; Fligor, B.J. Risk of noise-induced hearing loss due to recreational sound: Review and recommendations. J. Acoust. Soc. Am. 2019, 146, 3911–3921. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.; Neitzel, R.L. Noise exposure limit for children in recreational settings: Review of available evidence. J. Acoust. Soc. Am. 2019, 146, 3922–3933. [Google Scholar] [CrossRef]
- Moore, B.C.J. A review of the perceptual effects of hearing loss for frequencies above 3 kHz. Int. J. Audiol. 2016, 55, 707–714. [Google Scholar] [CrossRef]
- Hunter, L.L.; Monson, B.B.; Moore, D.R.; Dhar, S.; Wright, B.A.; Munro, K.J.; Zadeh, L.M.; Blankenship, C.M.; Stiepan, S.M.; Siegel, J.H. Extended High Frequency Hearing and Speech Perception Implications in Adults and Children. Hear. Res. 2020, 397, 107922. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.; Nixon, C.; Stephenson, M. Long-duration exposure to intermittent noises. Aviat. Space Environ. Med. 1976, 47, 987–990. [Google Scholar] [PubMed]
- Ward, E.D.; Cushing, E.M.; Burns, E.M. Effective quiet and moderate TTS: Implications for noise exposure standards. J. Acoust. Soc. Am. 1976, 59, 160–165. [Google Scholar] [CrossRef]
- Nixon, C.; Johnson, D.; Stephenson, M. Asymptotic behavior of temporary threshold shift and recovery from 24 to 48 hour noise exposures. Aviat. Space Environ. Med. 1977, 48, 311–515. [Google Scholar]
- World Health Organization (WHO). Guidelines for Community Noise; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Neitzel, R.L.; Gershon, R.R.M.; McAlexander, T.P.; Magda, L.A.; Pearson, J.M. Exposures to transit and other sources of noise among New York City residents. Environ. Sci. Technol. 2012, 46, 500–508. [Google Scholar] [CrossRef]
- McAlexander, T.P.; Gershon, R.R.M.; Neitzel, R.L. Streetlevel noise in an urban setting: Assessment and contribution to personal exposure. Environ. Health 2015, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Basner, M.; Brink, M.; Bristow, A.; de Kluizenaar, Y.; Finegold, L.; Hong, J. ICBEN review of research on the biological effects of noise 2011–2014. Noise Health 2015, 17, 57–82. [Google Scholar] [CrossRef] [PubMed]
- Neitzel, R.L.; Seixas, N.; Goldman, B.; Daniell, W. Contributions of non-occupational activities to total noise exposure of construction workers. Ann. Occup. Hyg. 2004, 48, 463–473. [Google Scholar]
- Abbate, C.; Concetto, G.; Fortunato, M.; Brecciaroli, R.; Tringali, M.A.; Beninato, G.; D’Arrigo, G.; Domenico, G. Influence of environmental factors on the evolution of industrial noise-induced hearing loss. Environ. Monit. Assess. 2005, 107, 351–361. [Google Scholar] [CrossRef]
- Jokitulppo, J.; Toivonen, M.; Björk, E. Estimated leisure-time noise exposure, hearing thresholds, and hearing symptoms of Finnish conscripts. Mil. Med. 2006, 171, 112–116. [Google Scholar] [CrossRef]
- Leensen, M.C.; van Duivenbooden, J.C.; Dreschler, W.A. A retrospective analysis of noise-induced hearing loss in the Dutch construction industry. Int. Arch. Occup. Environ. Health 2011, 84, 577–590. [Google Scholar] [CrossRef]
- Feder, K.; Marro, L.; McNamee, J.; Michaud, D. Prevalence of loud leisure noise activities among a representative sample of Canadians aged 6-79 years. J. Acoust. Soc. Am. 2019, 146, 3934–3946. [Google Scholar] [CrossRef]
- International Standards Organization (ISO). ISO Standard 1999; Acoustics—determination of occupational noise exposure and estimation of noise-induced hearing impairment; International Standards Organization: Geneve, Switzerland, 1990. [Google Scholar]
- Johnson, D.L.; Papadopoulos, P.; Watfa, N.; Takala, J. Exposure criteria, occupational exposure levels. In Occupational Exposure to Noise: Evaluation, Prevention and Control; WHO: Geneva, Switzerland, 2001; pp. 79–102. [Google Scholar]
- European Union (EU). Directive 2003/10/EC of the European Parliament and of the Council of 6 February 2003 on the Minimum Health and Safety Requirements Regarding the Exposure of Workers to the Risks Arising from Physical Agents (Noise); EU: Brussels, Belgium, 2003. [Google Scholar]
- Arenas, J.P.; Suter, A.H. Comparison of occupational noise legislation in the Americas: An overview and analysis. Noise Health 2014, 16, 306–319. [Google Scholar] [CrossRef] [PubMed]
- Kerr, M.J.; Neitzel, R.L.; Hong, O.; Sataloff, R.T. Historical review of efforts to reduce noise-induced hearing loss in the United States. Am. J. Ind. Med. 2017, 60, 569–577. [Google Scholar] [CrossRef]
- Beach, E.F.; Gilliver, M.; Williams, W. Leisure noise exposure: Participation trends, symptoms of hearing damage, and perception of risk. Int. J. Audiol. 2013, 52 (Suppl. 1), 20–25. [Google Scholar] [CrossRef] [PubMed]
- Williams, W.; Beach, E.F.; Gilliver, M. Clubbing: The cumulative effect of noise exposure from attendance at dance clubs and night clubs on whole-of-life noise exposure. Noise Health 2010, 12, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Flamme, G.A.; Stephenson, M.R.; Deiters, K.; Tatro, A.; van Gessel, D.; Geda, K.; Wyllys, K.; McGregor, K. Typical noise exposure in daily life. Int. J. Audiol. 2012, 51 (Suppl. 1), 3–11. [Google Scholar] [CrossRef]
- Jokitulppo, J.S.; Björk, E.A.; Akaan-Penttilä, E. Estimated leisure noise exposure and hearing symptoms in Finnish teenagers. Scand. Audiol. 1997, 26, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Biassoni, E.C.; Serra, M.R.; Richtert, U.; Joekes, S.; Yacci, M.R.; Carignani, J.A.; Abraham, S.; Minoldo, G.; Franco, G. Recreational noise exposure and its effects on the hearing of adolescents. Part II: Development of hearing disorders. Int. J. Audiol. 2005, 44, 74–85. [Google Scholar] [CrossRef]
- Vogel, I.; Verschuure, H.; van der Ploeg, C.P.; Brug, J.; Raat, H. Estimating adolescent risk for hearing loss based on data from a large school-based survey. Am. J. Public Health 2010, 100, 1095–1100. [Google Scholar] [CrossRef]
- Henderson, E.; Testa, M.A.; Hartnick, C. Prevalence of noise-induced hearing-threshold shifts and hearing loss among US youths. Pediatrics 2011, 127, 39–46. [Google Scholar] [CrossRef]
- Gilles, A.; De Ridder, D.; Van Hal, G.; Wouters, K.; Kleine Punte, A.; Van de Heyning, P. Prevalence of leisure noise-induced tinnitus and the attitude toward noise in university students. Otol. Neurotol. 2012, 33, 899–906. [Google Scholar] [CrossRef]
- Gilles, A.; Van Hal, G.; De Ridder, D.; Wouters, K.; Van de Heyning, P. Epidemiology of noise-induced tinnitus and the attitudes and beliefs towards noise and hearing protection in adolescents. PLoS ONE 2013, 8, e70297. [Google Scholar] [CrossRef]
- Johnson, O.; Andrew, B.; Walker, D.; Morgan, S.; Aldren, A. British university students’ attitudes towards noise-induced hearing loss caused by nightclub attendance. J. Laryngol. Otol. 2014, 128, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Vogel, I.; van de Looij-Jansen, P.M.; Mieloo, C.L.; Burdorf, A.; de Waart, F. Risky music listening, permanent tinnitus and depression, anxiety, thoughts about suicide and adverse general health. PLoS ONE 2014, 9, e98912. [Google Scholar] [CrossRef]
- Dehnert, K.; Raab, U.; Perez-Alvarez, C.; Steffens, T.; Bolte, G.; Fromme, H.; Twardella, D. Total leisure noise exposure and its association with hearing loss among adolescents. Int. J. Audiol. 2015, 54, 665–673. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Hearing Loss due to Recreational Exposure to Loud Sounds; A review; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Speaks, C.; Nelson, D.; Ward, W.D. Hearing loss in rock-and-roll musicians. J. Occup. Environ. Med. 1970, 12, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Clark, W.W. Noise exposure from leisure activities: A review. J. Acoust. Soc. Am. 1991, 90, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Bisch, C. Epidemiological evaluation of hearing damage related to strongly amplified music (personal cassette players, discotheques, rock concerts)—High-definition audiometric survey on 1364 subjects. Audiology 1996, 35, 121–142. [Google Scholar] [CrossRef] [PubMed]
- Gunderson, E.; Moline, J.; Catalano, P. Risks of developing noise-induced hearing loss in employees of urban music clubs. Am. J. Ind. Med. 1997, 31, 75–79. [Google Scholar] [CrossRef]
- Opperman, D.A.; Reifman, W.; Schlauch, R.; Levine, S. Incidence of spontaneous hearing threshold shifts during modern concert performances. Otolaryngol. Head. Neck. Surg. 2006, 134, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Grose, J.H.; Buss, E.; Hall, J.W., 3rd. Loud music exposure and cochlear synaptopathy in young adults: Isolated auditory brainstem response effects but no perceptual consequences. Trends. Hear. 2017, 21, 2331216517737417. [Google Scholar]
- Le Prell, C.G.; Dell, S.; Hensley, B.N.; Hall, J.W.I.; Campbell, K.C.M.; Antonelli, P.A.; Green, G.E.; Miller, J.M.; Guire, K. Digital music exposure reliably induces temporary threshold shift (TTS) in normal hearing human subjects. Ear. Hear. 2012, 33, 44–58. [Google Scholar] [CrossRef] [PubMed]
- Bogoch, I.I.; House, R.A.; Kudla, I. Perceptions about hearing protection and noise-induced hearing loss of attendees of rock concerts. Can. J. Public Health 2005, 96, 69–72. [Google Scholar] [CrossRef]
- Axelsson, A.; Lindgren, F. Hearing in classical musicians. Acta. Otolaryngol. 1981, 91, 3–74. [Google Scholar] [CrossRef]
- Axelsson, A.; Eliasson, A.; Israelsson, B. Hearing in pop/rock musicians: A follow-up study. Ear. Hear. 1995, 16, 245–253. [Google Scholar] [CrossRef]
- Kähäri, K.R.; Zachau, G.; Eklöf, M.; Sandsjö, L.; Möller, C. Assessment of hearing and hearing disorders in rock/jazz musicians. Int. J. Audiol. 2003, 42, 279–288. [Google Scholar] [CrossRef]
- Juman, S.; Karmody, C.S.; Simeon, D. Hearing loss in steelband musicians. Otolaryngol. Head. Neck Surg. 2003, 131, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Schmuziger, N.J.; Patscheke, J.; Probst, R. Hearing in non-professional pop/rock musicians. Ear. Hear. 2006, 27, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Størmer, C.C.; Laukli, E.; Høydal, E.H.; Stenklev, N.C. Hearing loss and tinnitus in rock musicians: A Norwegian survey. Noise Health 2015, 17, 411–421. [Google Scholar] [CrossRef] [PubMed]
- McIlvaine, D.; Stewart, M.; Anderson, R. Noise exposure levels for musicians during rehearsal and performance times. Med. Probl. Perform. Art. 2012, 27, 31–36. [Google Scholar] [CrossRef]
- Jansson, E.; Karlsson, K. Sound levels recorded within the symphony orchestra and risk criteria for hearing loss. Scand. Audiol. 1983, 12, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Royster, J.D.; Royster, L.H.; Killion, M.C. Sound exposures and hearing thresholds of symphony orchestra musicians. J. Acoust. Soc. Am. 1991, 89, 2793–2803. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Behar, A.; Kunov, H.; Wong, W. Musicians’ noise exposure in orchestra pit. Appl. Acoust. 2005, 66, 919–931. [Google Scholar] [CrossRef]
- Emmerich, E.; Rudel, L.; Richter, F. Is the audiologic status of professional musicians a reflection of the noise exposure in classical orchestral music? Eur. Arch. Otorhinolaryngol. 2008, 265, 753–758. [Google Scholar] [CrossRef] [PubMed]
- Kang, T.S.; Lee, L.K.; Kang, S.C.; Yoon, C.S.; Park, D.U.; Kim, R.H. Assessment of noise measurements made with a continuous monitoring in time. J. Acoust. Soc. Am. 2010, 134, 822–831. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, I.; Driscoll, T.; Ackermann, B. Sound Exposure of Professional Orchestral Musicians during Solitary Practice. J. Acoust. Soc. Am. 2013, 134, 2748–2754. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, K.; Lundquist, P.G.; Olaussen, T. The hearing of symphony orchestra musicians. Scand. Audiol. 1983, 12, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Strasser, H.; Irle, H.; Scholz, R. Physiological cost of energy-equivalent exposures to white noise, industrial noise, heavy metal music, and classical music. Noise Control Eng. J. 1999, 47, 187–192. [Google Scholar] [CrossRef]
- Strasser, H.; Irle, H.; Legler, R. Temporary hearing threshold shifts and restitution after energy-equivalent exposures to industrial noise and classical music. Noise Health 2003, 5, 75–84. [Google Scholar]
- Swanson, S.J.; Dengerink, H.A.; Kondrick, P.; Miller, C.L. The influence of subjective factors on temporary threshold shifts after exposure to music and noise of equal energy. Ear. Hear. 1987, 8, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Lindgren, F. Does pop music cause hearing damage? Audiology 1977, 16, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Westmore, G.A.; Eversden, I.D. Noise-induced hearing loss and orchestral musicians. Arch. Otolaryngol. 1981, 107, 761–764. [Google Scholar] [CrossRef] [PubMed]
- Ostri, B.; Eller, N.; Dahlin, E.; Skylv, G. Hearing impairment in orchestral musicians. Scand. Audiol. 1989, 18, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Kähäri, K.R.; Axelsson, A.; Hellström, P.A.; Zachau, G. Hearing assessment of classical orchestral musicians. Scand. Audiol. 2001, 30, 13–23. [Google Scholar] [CrossRef]
- Kähäri, K.R.; Axelsson, A.; Hellström, P.A.; Zachau, G. Hearing development in classical orchestral musicians. A follow-up study. Scand. Audiol. 2001, 30, 141–149. [Google Scholar] [CrossRef]
- Laitinen, H.M.; Toppila, E.M.; Olkinuora, P.S.; Kuisma, K. Sound exposure among the Finnish National Opera personnel. Appl. Occup. Environ. Hyg. 2003, 18, 177–182. [Google Scholar] [CrossRef]
- Jansen, E.J.M.; Helleman, H.W.; Dreschler, W.A.; Laat, J.A.P.M. Noise induced hearing loss and other hearing complaints among musicians of symphony orchestras. Int. Arch. Occ. Environ. Health 2009, 82, 153–164. [Google Scholar] [CrossRef]
- Phillips, S.L.; Henrich, V.C.; Mace, S.T. Prevalence of noise-induced hearing loss in student musicians. Int. J. Audiol. 2010, 49, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Toppila, E.; Koskinen, H.; Pyykko, I. Hearing loss among classical-orchestra musicians. Noise Health 2011, 13, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.H.; Pedersen, E.; Paarup, H.; Christensen-Dalsgaard, J.; Andersen, T.; Poulsen, T.; Baelum, J. Hearing Loss in Relation to Sound Exposure of Professional Symphony Orchestra Musicians. Ear. Hear. 2014, 35, 448–460. [Google Scholar] [CrossRef] [PubMed]
- Halevi-Katz, D.N.; Yaakobi, E.; Putter-Katz, H. Exposure to music and noise-induced hearing loss (NIHL) among professional pop/rock/jazz musicians. Noise Health 2015, 17, 158–164. [Google Scholar] [CrossRef]
- Pawalczyk-Luszczynska, M.; Zamojska-Daniszewska, M.; Dudarewicz, A.; Zaborowski, K. Exposure to excessive sounds and hearing status in academic classical music students. Int. J. Occup. Med. Environ. Health 2017, 30, 55–75. [Google Scholar]
- Pouryaghoub, G.; Mehrdad, R.; Pourhosein, S. Noise-Induced hearing loss among professional musicians. J. Occup. Health 2017, 59, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, J.H.; Paarup, H.M.; Baelum, J. Tinnitus severity is related to the sound exposure of symphony orchestra musicians independently of hearing impairment. Ear. Hear. 2019, 40, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Kazkayasi, M.; Yetiser, S.; Ozcelik, S. Effect of musical training on musical perception and hearing sensitivity: Conventional and high-frequency audiometric comparison. J. Otolaryngol. 2006, 35, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Liberman, M.C.; Epstein, M.J.; Cleveland, S.S.; Wang, H.; Maison, S.F. Toward a Differential Diagnosis of Hidden Hearing Loss in Humans. PLoS ONE 2016, 11, e0162726. [Google Scholar] [CrossRef] [PubMed]
- Schmuziger, N.; Patscheke, J.; Probst, R. An assessment of threshold shifts in nonprofessional pop/rock musicians using conventional and extended high-frequency audiometry. Ear. Hear. 2007, 28, 643–648. [Google Scholar] [CrossRef]
- Keefe, J. Noise Exposure Associated with Marching and Pep Bands. ASA/NOISE-CON. 2005. Available online: http://acoustics.org/pressroom/httpdocs/150th/Keefe.html (accessed on 15 April 2021).
- National Institute for Occupational Safety and Health (NIOSH). Health Hazard Evaluation Report: Noise Evaluation of Elementary and High School Music Classes and Indoor Marching Band Rehearsals—Alabama; Publication No. 2011‒0129‒3160; Chen, L., Brueck, S., Eds.; NIOSH: Washington, DC, USA, 2012. [Google Scholar]
- Russell, J.A.; Yamaguchi, M. Sound Exposure of Healthcare Professionals Working With a University Marching Band. J. Am. Acad. Audiol. 2018, 29, 83–89. [Google Scholar] [CrossRef]
- Jin, S.H.; Nelson, P.B.; Schlauch, R.; Carney, E. Hearing conservation program for marching band members: A risk for noise-induced hearing loss? Am. J. Audiol. 2013, 22, 26–39. [Google Scholar] [CrossRef]
- Di Stadio, A.; Dipietro, L.; Ricci, G.; Della Volpe, A.; Minni, A.; Greco, A.; de Vincentiis, M.; Ralli, M. Hearing Loss, Tinnitus, Hyperacusis, and Diplacusis in Professional Musicians: A Systematic Review. Int. J. Environ. Res. Public. Health. 2018, 15, E2120. [Google Scholar] [CrossRef] [PubMed]
- Gundersen, E. List of Rockers with Hearing Loss Grows. 2018. Available online: https://www.aarp.org/health/conditions-treatments/info-2018/musicians-hearing-loss.html (accessed on 15 April 2021).
- Coleman, C. Royal Opera House Loses Appeal over Viola Player’s Hearing. British Broadcasting Corporation Wales News, 12 July 2019. Available online: https://www.bbc.com/news/entertainment-arts-47965734 (accessed on 15 April 2021).
- Tan, T.C.; Tsang, H.C.; Wong, T.L. Noise surveys in discotheques in Hong Kong. Ind. Health 1990, 28, 37–40. [Google Scholar] [PubMed]
- Lee, L.T. A study of the noise hazard to employees in local discotheques]. Singapore Med. J. 1999, 40, 571–574. [Google Scholar]
- Sadhra, S.; Jackson, C.A.; Ryder, T.; Brown, M.J. Noise exposure and hearing loss among student employees working in university entertainment venues. Ann. Occup. Hyg. 2002, 46, 455–463. [Google Scholar]
- Park, M.-Y. Assessment of potential noise-induced hearing loss with commercial "Karaoke" noise. Int. J. Ind. Ergonom. 2003, 31, 375–385. [Google Scholar] [CrossRef]
- Bray, A.; Szymański, M.; Mills, R. Noise induced hearing loss in dance music disc jockeys and an examination of sound levels in nightclubs. J. Laryngol. Otol. 2004, 118, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Twardella, D.; Wellhoefer, A.; Brix, J.; Fromme, H. High sound pressure levels in Bavarian discotheques remain after introduction of voluntary agreements. Noise Health 2008, 10, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.C.; Boyd, S.M.; Henehan, G.T.; Chambers, G. Occupational noise exposure of nightclub bar employees in Ireland. Noise Health 2012, 14, 148–154. [Google Scholar] [CrossRef]
- Potier, M.; Hoquet, C.; Lloyd, R.; Nicolas-Puel, C.; Uziel, A.; Puel, J.L. The risks of amplified music for disc-jockeys working in nightclubs. Ear. Hear. 2009, 30, 291–293. [Google Scholar] [CrossRef]
- Serra, M.R.; Biassoni, E.C.; Richter, U.; Minoldo, G.; Franco, G.; Abraham, S.; Carignani, J.A.; Joekes, S.; Yacci, M.R. Recreational noise exposure and its effects on the hearing of adolescents. Part I: An interdisciplinary long-term study. Int. J. Audiol. 2005, 44, 65–73. [Google Scholar] [CrossRef]
- Biassoni, E.C.; Serra, M.R.; Hinalaf, M.; Abraham, M.; Pavlik, M.; Villalobo, J.P.; Curet, C.; Joekes, S.; Yacci, M.R.; Righetti, A. Hearing and loud music exposure in a group of adolescents at the ages of 14-15 and retested at 17–18. Noise Health 2014, 16, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Serra, M.R.; Biassoni, E.C.; Hinalaf, M.; Abraham, M.; Pavlik, M.; Villalobo, J.P.; Curet, C.; Joekes, S.; Yacci, M.R.; Righetti, A. Hearing and loud music exposure in 14-15 years old adolescents. Noise Health 2014, 16, 320–330. [Google Scholar] [CrossRef] [PubMed]
- Keith, S.E.; Michaud, D.S.; Chiu, V. Evaluating the maximum playback sound levels from portable digital audio players. J. Acoust. Soc. Am. 2008, 123, 4227–4237. [Google Scholar] [CrossRef]
- Breinbauer, H.A.; Anabalón, J.L.; Gutierrez, D.; Cárcamo, R.; Olivares, C.; Caro, J. Output capabilities of personal music players and assessment of preferred listening levels of test subjects: Outlining recommendations for preventing music-induced hearing loss. Laryngoscope 2012, 122, 2549–2556. [Google Scholar] [CrossRef]
- Shim, H.; Lee, S.; Koo, M.; Kim, J. Analysis of Output Levels of an MP3 Player: Effects of Earphone Type, Music Genre, and Listening Duration. J. Audiol. Otol. 2018, 22, 140–147. [Google Scholar] [CrossRef]
- Jiang, W.; Zhao, F.; Guderley, N.; Manchaiah, V. Daily music exposure dose and hearing problems using personal listening devices in adolescents and young adults: A systematic review. Int. J. Audiol. 2016, 55, 197–205. [Google Scholar] [CrossRef]
- Fligor, B.J.; Levey, S.; Levey, T. Cultural and demographic factors influencing noise exposure estimates from use of portable listening devices in an urban environment. J. Speech Lang. Hear. Res. 2013, 57, 1535–1547. [Google Scholar] [CrossRef] [PubMed]
- Levey, S.; Levey, T.; Fligor, B.J. Noise exposure estimates of urban MP3 player users. J. Speech Lang. Hear. Res. 2011, 54, 263–277. [Google Scholar] [CrossRef]
- Gilliver, M.; Nguyen, J.; Beach, E.F.; Barr, C. Personal Listening Devices in Australia: Patterns of Use and Levels of Risk. Semin. Hear. 2017, 38, 282–297. [Google Scholar] [PubMed]
- Muchnik, C.; Amir, N.; Shabtai, E.; Kaplan-Neeman, R. Preferred listening levels of personal listening devices in young teenagers: Self reports and physical measurements. Int. J. Audiol. 2012, 51, 287–293. [Google Scholar] [CrossRef]
- Cone, B.K.; Wake, M.; Tobin, S.; Poulakis, Z.; Rickards, F.W. Slight-mild sensorineural hearing loss in children: Audiometric, clinical, and risk factor profiles. Ear. Hear. 2010, 31, 202–212. [Google Scholar] [CrossRef]
- Båsjö, S.; Möller, C.; Widén, S.; Jutengren, G.; Kähäri, K. Hearing thresholds, tinnitus, and headphone listening habits in nine-year-old children. Int. J. Audiol. 2016, 55, 587–596. [Google Scholar] [CrossRef]
- Mills, J.H. Noise and children: A review of literature. J. Acoust. Soc. Am. 1975, 58, 767–779. [Google Scholar] [CrossRef] [PubMed]
- Mahboubi, H.; Oliaei, S.; Badran, K.W. Systematic assessment of noise amplitude generated by toys intended for young children. Otolaryngol. Head Neck Surg. 2013, 148, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Peng, J.H.; Tao, Z.Z.; Huang, Z.W. Risk of damage to hearing from personal listening devices in young adults. J. Otolaryngol. 2007, 36, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Le Prell, C.G.; Spankovich, C.; Lobarinas, E.; Griffiths, S.K. Extended high-frequency thresholds in college students: Effects of music player use and other recreational noise. J. Am. Acad. Audiol. 2013, 24, 725–739. [Google Scholar] [CrossRef]
- Sulaiman, A.H.; Husain, R.; Seluakumaran, K. Evaluation of early hearing damage in personal listening device users using extended high-frequency audiometry and otoacoustic emissions. Eur. Arch. Otorhinolaryngol. 2014, 271, 1463–1470. [Google Scholar] [CrossRef] [PubMed]
- Engard, D.J.; Sandfort, D.R.; Gotshall, R.W.; Brazile, W.J. Noise exposure, characterization, and comparison of three football stadiums. J. Occup. Environ. Hyg. 2010, 7, 616–621. [Google Scholar] [CrossRef]
- Hodgetts, W.E.; Liu, R. Can hockey playoffs harm your hearing? CMAJ 2006, 175, 1541–1542. [Google Scholar] [CrossRef]
- Cranston, C.J.; Brazile, W.J.; Sandfort, D.R.; Gotshall, R.W. Occupational and recreational noise exposure from indoor arena hockey games. J. Occup. Environ. Hyg. 2013, 10, 11–16. [Google Scholar] [CrossRef] [PubMed]
- De Swanepoel, W.; Hall, J.W., 3rd. Football match spectator sound exposure and effect on hearing: A pretest-post-test study. S. Afr. Med. J. 2010, 100, 239–242. [Google Scholar] [CrossRef]
- Flamme, G.A.; Williams, N. Sports officials’ hearing status: Whistle use as a factor contributing to hearing trouble. J. Occup. Environ. Hyg. 2013, 10, 1–10. [Google Scholar] [CrossRef]
- Torre, P., 3rd; Howell, J.C. Noise levels during aerobics and the potential effects on distortion product otoacoustic emissions. J. Commun. Disord. 2008, 41, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Nassar, G. The human temporary threshold shift after exposure to 60 minutes’ noise in an aerobics class. Br. J. Audiol. 2001, 35, 99–101. [Google Scholar] [CrossRef]
- Beach, E.F.; Nie, V. Noise levels in fitness classes are still too high: Evidence from 1997–1998 and 2009–2011. Arch. Environ. Occup. Health 2014, 69, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Rose, A.S.; Ebert, C.S., Jr.; Prazma, J.; Pillsbury, H.C., 3rd. Noise exposure levels in stock car auto racing. Ear Nose Throat J. 2008, 87, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Kardous, C.; Morata, T. Occupational and recreational noise exposures at stock car racing circuits: An exploratory survey of three professional race tracks. Noise Control Eng. 2010, 58, 54–61. [Google Scholar] [CrossRef]
- Morley, J.C.; Seitz, T.; Tubbs, R. Carbon monoxide and noise exposure at a monster truck and motocross show. Appl. Occup. Environ. Hyg. 1999, 14, 645–655. [Google Scholar] [CrossRef]
- McCombe, A.W.; Binnington, J. Hearing loss in Grand Prix motorcyclists: Occupational hazard or sports injury? Br. J. Sports Med. 1994, 28, 35–37. [Google Scholar] [CrossRef]
- Ross, B.C. Noise exposure of motorcyclists. Ann. Occup. Hyg. 1989, 33, 123–127. [Google Scholar] [PubMed]
- Kennedy, J.; Carley, M.; Walker, I.; Holt, N. On-road and wind-tunnel measurement of motorcycle helmet noise. J. Acoust. Soc. Am. 2013, 134, 2004–2010. [Google Scholar] [CrossRef] [PubMed]
- McCombe, A.W.; Binington, J.; Davis, A.C.; Spencer, H. Hearing loss in motorcyclists. J. Laryngol. Otol. 1995, 109, 599–604. [Google Scholar] [CrossRef]
- Moore, K.L. Noise Exposures of Recreational Snowmobilers. University of Colorado Unpublished Thesis. 2014. Available online: https://digscholarship.unco.edu/cgi/viewcontent.cgi?article=1002&context=capstones (accessed on 15 April 2021).
- Zhao, Y.M.; Qiu, W.; Zeng, L.; Chen, S.S.; Cheng, X.R.; Davis, R.I.; Hamernik, R.P. Application of the kurtosis statistic to the evaluation of the risk of hearing loss in workers exposed to high-level complex noise. Ear. Hear. 2010, 31, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.D.; Williams, E. Acoustic trauma in the sports hunter. Laryngoscope 1966, 76, 863–879. [Google Scholar] [CrossRef]
- Stewart, M.; Borer, S.E.; Lehman, M. Shooting habits of U.S. waterfowl hunters. Noise Health 2009, 11, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Meinke, D.K.; Snyders, J.K.; Howerton, K. Shooting habits of youth recreational firearm users. Int. J. Audiol. 2014, 53, 26–34. [Google Scholar] [CrossRef]
- Zadeh, L.M.; Silbert, N.H.; Sternasty, K.; Swanepoel, D.W.; Hunter, L.L.; Moore, D.R. Extended high-frequency hearing enhances speech perception in noise. PNAS 2019, 116, 23753–23759. [Google Scholar] [CrossRef] [PubMed]
- Shargorodsky, J.; Curhan, S.G.; Curhan, G.C.; Eavey, R. Change in prevalence of hearing loss in US adolescents. JAMA 2010, 304, 772–778. [Google Scholar] [CrossRef]
- Rhee, J.; Lee, D.; Lim, H.J.; Park, M.K.; Suh, M.W.; Lee, J.H.; Hong, Y.C.; Oh, S.H. Hearing loss in Korean adolescents: The prevalence thereof and its association with leisure noise exposure. PLoS ONE 2019, 14, e0209254. [Google Scholar] [CrossRef] [PubMed]
- Schlauch, R.S.; Carney, E. The challenge of detecting minimal hearing loss in audiometric surveys. Am. J. Audiol. 2012, 21, 106–119. [Google Scholar] [CrossRef]
- Ward, W.D. The concept of susceptibility to hearing loss. J. Occup. Med. 1965, 7, 595–607. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.; Subramaniam, M.; Boettcher, F.A. Individual susceptibility to noise-induced hearing loss: An old topic revisited. Ear. Hear. 1993, 14, 152–168. [Google Scholar] [CrossRef] [PubMed]
- Shuster, B.Z.; Depireux, D.A.; Mong, J.A.; Hertzano, R. Sex differences in hearing: Probing the role of estrogen signaling. J. Acoust. Soc. Am. 2019, 145, 3656–3663. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, E.A.; Castro, J.C.; Macedo, M.E. Iris pigmentation and susceptibility to noise-induced hearing loss. Int. J. Audiol. 2008, 47, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Flamme, G.A.; Deiters, K.; Needham, T. Distributions of pure-tone hearing threshold levels among adolescents and adults in the United States by gender, ethnicity, and age: Results from the US National Health and Nutrition Examination Survey. Int. J. Audiol. 2011, 50, S11–S20. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Maas, P.; Chien, W.; Carey, J.P.; Ferrucci, L.; Thorpe, R. Association of skin color, race/ethnicity, and hearing loss among adults in the USA. J. Assoc. Res. Otolaryngol. 2012, 13, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Spankovich, C.; Le Prell, C.G.; Lobarinas, E.; Hood, L.J. Noise History and Auditory Function in Young Adults With and Without Type 1 Diabetes Mellitus. Ear. Hear. 2017, 38, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Zakrisson, J.E.; Borg, E.; Lidén, G.; Nilsson, R. Stapedius reflex in industrial impact noise: Fatigability and role for temporary threshold shift (TTS). Scand. Audiol. Suppl. 1980, 12, 326–334. [Google Scholar]
- Shotland, L.I. Dosimetry measurements using a probe tube microphone in the ear canal. J. Acoust. Soc. Am. 1996, 99, 979–984. [Google Scholar] [CrossRef]
- Grinn, S.K.; Le Prell, C.G. Noise-dose estimated with and without pre-cochlear amplification. J. Acoust. Soc. Am. 2019, 146, 3967. [Google Scholar] [CrossRef] [PubMed]
- Henderson, D.; Bielefeld, E.C.; Harris, K.C. The role of oxidative stress in noise-induced hearing loss. Ear. Hear. 2006, 27, 1–19. [Google Scholar] [CrossRef]
- Liu, Y.-M.; Li, X.-D.; Guo, X.; Liu, B.; Lin, A.-H.; Ding, Y.-L.; Rao, S.-Q. SOD2 V16A SNP in the mitochondrial targeting sequence is associated with noise induced hearing loss in Chinese workers. Dis. Markers 2010, 28, 137–147. [Google Scholar] [CrossRef]
- Sliwinska-Kowalska, M.; Pawelczyk, M. Contribution of genetic factors to noise-induced hearing loss: A human studies review. Mutat. Res. 2013, 752, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, A.S.; Bohne, B.A.; Harding, G.W. Histopathological differences between temporary and permanent threshold shift. Hear. Res. 2000, 139, 13–30. [Google Scholar] [CrossRef]
- Fernandez, K.A.; Jeffers, P.W.; Lall, K.; Liberman, M.C.; Kujawa, S.G. Aging after noise exposure: Acceleration of cochlear synaptopathy in “recovered” ears. J. Neurosci. 2015, 35, 7509–7520. [Google Scholar] [CrossRef] [PubMed]
- Beach, E.; Williams, W.; Gilliver, M. Hearing protection for clubbers is music to their ears. Health Promot. J. Aust. 2010, 21, 215–221. [Google Scholar] [CrossRef]
- Themann, C.L.; Suter, A.H.; Stephenson, M.R. National research agenda for the prevention of occupational hearing loss—Part 1. Sem. Hear. 2013, 34, 145–207. [Google Scholar] [CrossRef]
- Hickey, K. Musician Earplugs: Knowledge, Attitudes, Beliefs, Behaviors, and Experiences among Small Music Venue Workers; Capstones & Scholarly Projects. 67. 2019. Available online: https://digscholarship.unco.edu/capstones/67 (accessed on 15 April 2021).
- Brown, C.H.; Gordon, M.S. Motorcycle Helmet Noise and Active Noise Reduction. Open Acoust. J. 2011, 4, 14–24. [Google Scholar] [CrossRef]
- Henry, P.; Foots, A. Comparison of user volume control settings for portable music players with three earphone configurations in quiet and noisy environments. J. Am. Acad. Audiol. 2012, 23, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Liang, M.J.; Zhao, F.; French, D.; Zheng, Y.Q. Characteristics of noise-canceling headphones to reduce the hearing hazard for MP3 users. J. Acoust. Soc. Am. 2012, 131, 4526–4534. [Google Scholar] [CrossRef]
- Chasin, M. Musicians and the Prevention of Hearing Loss; Singular Press: San Diego, CA, USA, 2010. [Google Scholar]
- Murphy, W.J.; Byrne, D.C.; Franks, J.R. Firearms and hearing protection. Hear. Rev. 2007, 14, 36–38. [Google Scholar]
- Widén, S.E.; Erlandsson, S.I. The influence of socio-economic status on adolescent attitude to social noise and hearing protection. Noise Health 2004, 7, 59–70. [Google Scholar] [PubMed]
- Laitinen, H.M. Factors affecting the use of hearing protectors among classical music players. Noise Health 2005, 7, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Nondahl, D.M.; Cruickshanks, K.J.; Dalton, D.S.; Klein, B.E.; Klein, R.; Tweed, T.S.; Wiley, T.L. The use of hearing protection devices by older adults during recreational noise exposure. Noise Health 2006, 8, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, K.; Sivonen, V.; Poykko, V. Symphony orchestra musicians’ use of hearing protection and attenuation of custom-made hearing protectors as measured with two different real-ear attenuation at threshold methods. Noise Health 2011, 13, 176–188. [Google Scholar] [CrossRef] [PubMed]
- Beach, E.F.; Williams, W.; Gilliver, M. A qualitative study of earplug use as a health behavior: The role of noise injury symptoms, self-efficacy and an affinity for music. J. Health Psych. 2012, 17, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Beach, E.F.; O’Brien, I. In Their Own Words: Interviews with Musicians Reveal the Advantages and Disadvantages of Wearing Earplugs. Med. Probl. Perform. Art. 2017, 32, 101–110. [Google Scholar] [CrossRef]
- Hunter, A. Attitudes, risk behavior, and noise exposure among young adults with hearing problems: Identifying a typology. Semin. Hear. 2017, 38, 332–347. [Google Scholar] [CrossRef] [PubMed]
- Cozad, R.L.; Marston, L.; Joseph, D. Some implications regarding high frequency hearing loss in school-age children. J. School Health 1974, 44, 92–96. [Google Scholar] [CrossRef]
- Lass, N.J.; Woodford, C.M.; Lundeen, C.; Lundeen, D.J.; Everly-Myer, D.S. A survey of high school students’ knowledge and awareness of hearing, hearing loss, and hearing health. Hear. J. 1987, 40, 15–19. [Google Scholar]
- Lass, N.J.; Woodford, C.M.; Lundeen, C.; Lundeen, D.J.; Everly-Myer, D.S.; McGuire, K.; Mason, D.S.; Paknik, L.; Phillips, R.P. A hearing-conservation program for a junior high school. Hear. J. 1987, 40, 32–40. [Google Scholar]
- Lewis, D.A. A hearing conservation program for high school-level students. Hear. J. 1989, 42, 19–24. [Google Scholar]
- Chermak, G.D.; Peters-McCarthy, E. The effectiveness of an educational hearing conservation program for elementary school children. Lang. Speech Hear. Serv. Sch. 1991, 22, 308–312. [Google Scholar] [CrossRef]
- Blair, J.C.; Hardegree, D.; Benson, P.V. Necessity and effectiveness of a hearing conservation program for elementary students. J. Edu. Audiol. 1996, 4, 12–16. [Google Scholar]
- Chermak, G.D.; Curtis, L.; Seikel, J.A. The effectiveness of an interactive hearing conservation program for elementary school children. Lang. Speech Hear. Serv. Sch. 1996, 27, 29–39. [Google Scholar] [CrossRef]
- Knobloch, M.J.; Broste, S.K. A hearing conservation program for Wisconsin youth working in agriculture. J. Sch. Health 1998, 68, 313–318. [Google Scholar] [CrossRef]
- Lukes, E.; Johnson, M. Hearing conservation: Community outreach programs for high school students. Am. Assoc. Occ. Health Nurses J. 1998, 46, 340–343. [Google Scholar] [CrossRef]
- Anderson, K.L. Hearing conservation in the public schools revisited. Sem. Hear. 1999, 12, 340–364. [Google Scholar] [CrossRef]
- Bennett, J.A.; English, K. Teaching hearing conservation to school children: Comparing the outcomes and efficacy of two pedagogical approaches. J. Edu. Audiol. 1999, 7, 29–33. [Google Scholar]
- Folmer, R.L.; Griest, S.E.; Martin, W.H. Hearing conservation education programs for children: A review. J. Sch. Health 2002, 72, 51–57. [Google Scholar] [CrossRef]
- Folmer, R.L. The importance of hearing conservation instruction. J. Sch. Nurs. 2003, 19, 140–148. [Google Scholar] [CrossRef] [PubMed]
- Fausti, S.A.; Wilmington, D.J.; Helt, P.V.; Helt, W.J.; Konrad-Martin, D. Hearing health and care: The need for improved hearing loss prevention and hearing conservation practices. J. Rehabil. Res. Dev. 2005, 42, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Marlenga, B.; Linneman, J.G.; Pickett, W.; Wood, D.J.; Kirkhorn, S.R.; Broste, S.K. Randomized trial of a hearing conservation intervention for rural students: Long-term outcomes. Pediatrics 2011, 128, 1139–1146. [Google Scholar] [CrossRef] [PubMed]
- Auchter, M.; Le Prell, C.G. Hearing loss prevention education using adopt-a-band: Changes in self-reported earplug use in two high school marching bands. Am. J. Audiol. 2014, 23, 211–226. [Google Scholar] [CrossRef] [PubMed]
- Gilles, A.; Paul Vde, H. Effectiveness of a preventive campaign for noise-induced hearing damage in adolescents. Int. J. Pediatr. Otorhinolaryngol. 2014, 78, 604–609. [Google Scholar] [CrossRef]
- Sha, S.H.; Schacht, J. Emerging therapeutic interventions against noise-induced hearing loss. Expert Opin. Investig. Drugs 2017, 26, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Bielefeld, E.C.; Harrison, R.T.; Riley DeBacker, J. Pharmaceutical otoprotection strategies to prevent impulse noise-induced hearing loss. J. Acoust. Soc. Am. 2019, 146, 3790. [Google Scholar] [CrossRef]
- McFerran, D.J.; Stockdale, D.; Holme, R.; Large, C.H.; Baguley, D.M. Why Is There No Cure for Tinnitus? Front. Neurosci. 2019, 13, 802. [Google Scholar] [CrossRef] [PubMed]
- Bielefeld, E.C.; Kobel, M.J. Advances and Challenges in Pharmaceutical Therapies to Prevent and Repair Cochlear Injuries From Noise. Front. Cell Neurosci. 2019, 13, 285. [Google Scholar] [CrossRef] [PubMed]
- Kujawa, S.G.; Liberman, M.C. Translating animal models to human therapeutics in noise-induced and age-related hearing loss. Hear. Res. 2019, 377, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Schilder, A.G.M.; Su, M.P.; Mandavia, R.; Anderson, C.R.; Landry, E.; Ferdous, T.; Blackshaw, H. Early phase trials of novel hearing therapeutics: Avenues and opportunities. Hear. Res. 2019, 380, 175–186. [Google Scholar] [CrossRef]
- Kraus, K.S.; Mitra, S.; Jimenez, Z.; Hinduja, S.; Ding, D.; Jiang, H.; Gray, L.; Lobarinas, E.; Sun, W.; Salvi, R.J. Noise trauma impairs neurogenesis in the rat hippocampus. Neuroscience 2010, 167, 1216–1226. [Google Scholar] [CrossRef] [PubMed]
- Li, C.M.; Zhang, X.; Hoffman, H.J.; Cotch, M.F.; Themann, C.L.; Wilson, M.R. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005-2010. JAMA Otolaryngol. Head. Neck Surg. 2014, 140, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Martini, A.; Castiglione, A.; Bovo, R.; Vallesi, A.; Gabelli, C. Aging, cognitive load, dementia and hearing loss. Audiol. Neurotol. 2014, 19, 2–5. [Google Scholar] [CrossRef]
- Dawes, P.; Emsley, R.; Cruickshanks, K.J.; Moore, D.R.; Fortnum, H.; Edmondson-Jones, M.; McCormack, A.; Munro, K.J. Hearing loss and cognition: The role of hearing aids, social isolation and depression. PLoS ONE 2015, 10, e0119616. [Google Scholar] [CrossRef]
- Fortunato, S.; Forli, F.; Guglielmi, V.; De Corso, E.; Paludetti, G.; Berrettini, S.; Fetoni, A.R. A review of new insights on the association between hearing loss and cognitive decline in ageing. Acta. Otorhinolaryngol. Ital. 2016, 36, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Shen, P.; He, T.; Chang, Y.; Shi, L.; Tao, S.; Li, X.; Xun, Q.; Guo, X.; Yu, Z.; et al. Noise induced hearing loss impairs spatial learning/memory and hippocampal neurogenesis in mice. Sci. Rep. 2016, 6, 20374. [Google Scholar] [CrossRef] [PubMed]
- Cosh, S.; Carriere, I.; Daien, V.; Amieva, H.; Tzourio, C.; Delcourt, C.; Helmer, C. The relationship between hearing loss in older adults and depression over 12 years: Findings from the three-year prospective cohort study. Int. J. Geriatr. Psychiat. 2018, 33, 1654–1661. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Metter, E.J.; O’Brien, R.J.; Resnick, S.M.; Zonderman, A.B.; Ferrucci, L. Hearing loss and incident dementia. Arch. Neurol. 2011, 68, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Thomson, R.S.; Auduong, P.; Miller, A.T.; Gurgel, R.K. Hearing loss as a risk factor for dementia: A systematic review. Laryngoscope Investig. Otolaryngol. 2017, 2, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Aazh, H.; Moore, B.C.J. Thoughts about Suicide and Self-Harm in Patients with Tinnitus and Hyperacusis. J. Am. Acad. Adiol. 2018, 29, 255–261. [Google Scholar] [CrossRef] [PubMed]
| Name of Organization Advocating for Hearing Conservation | Web Address |
|---|---|
| Academy of Doctors of Audiology | audiologist.org * |
| Action on Hearing Loss | actiononhearingloss.org.uk * |
| American Academy of Audiology | audiology.org * |
| American Academy of Otolaryngology—Head and Neck Surgery | entnet.org * |
| American Speech-Language-Hearing Association | asha.org * |
| American Tinnitus Association | ata.org * |
| Center for Hearing and Communication | chchearing.org * |
| Dangerous Decibels | dangerousdecibels.org * |
| Hearing Education and Awareness for Rockers | hearnet.com * |
| Hearing Industries Association | hearing.org * |
| Hearing Loss Association of America | hearingloss.org * |
| Howard Leight | howardleight.com * |
| National Hearing Conservation Association | hearingconservation.org * |
| National Institute for Occupational Safety and Health | cdc.gov/niosh/topics/noise/ * |
| National Institute on Deafness and Other Communication Disorders | nidcd.nih.gov * |
| Sight & Hearing Association | sightandhearing.org * |
| The Hearing Conservation Workshop | heartomorrow.org * |
| The Noise Pollution Clearinghouse | nonoise.org * |
| The Quiet Coalition | thequietcoalition.org * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pienkowski, M. Loud Music and Leisure Noise Is a Common Cause of Chronic Hearing Loss, Tinnitus and Hyperacusis. Int. J. Environ. Res. Public Health 2021, 18, 4236. https://doi.org/10.3390/ijerph18084236
Pienkowski M. Loud Music and Leisure Noise Is a Common Cause of Chronic Hearing Loss, Tinnitus and Hyperacusis. International Journal of Environmental Research and Public Health. 2021; 18(8):4236. https://doi.org/10.3390/ijerph18084236
Chicago/Turabian StylePienkowski, Martin. 2021. "Loud Music and Leisure Noise Is a Common Cause of Chronic Hearing Loss, Tinnitus and Hyperacusis" International Journal of Environmental Research and Public Health 18, no. 8: 4236. https://doi.org/10.3390/ijerph18084236
APA StylePienkowski, M. (2021). Loud Music and Leisure Noise Is a Common Cause of Chronic Hearing Loss, Tinnitus and Hyperacusis. International Journal of Environmental Research and Public Health, 18(8), 4236. https://doi.org/10.3390/ijerph18084236





