Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health
Abstract
1. Introduction: Rocket Science or Preponderance of Evidence?
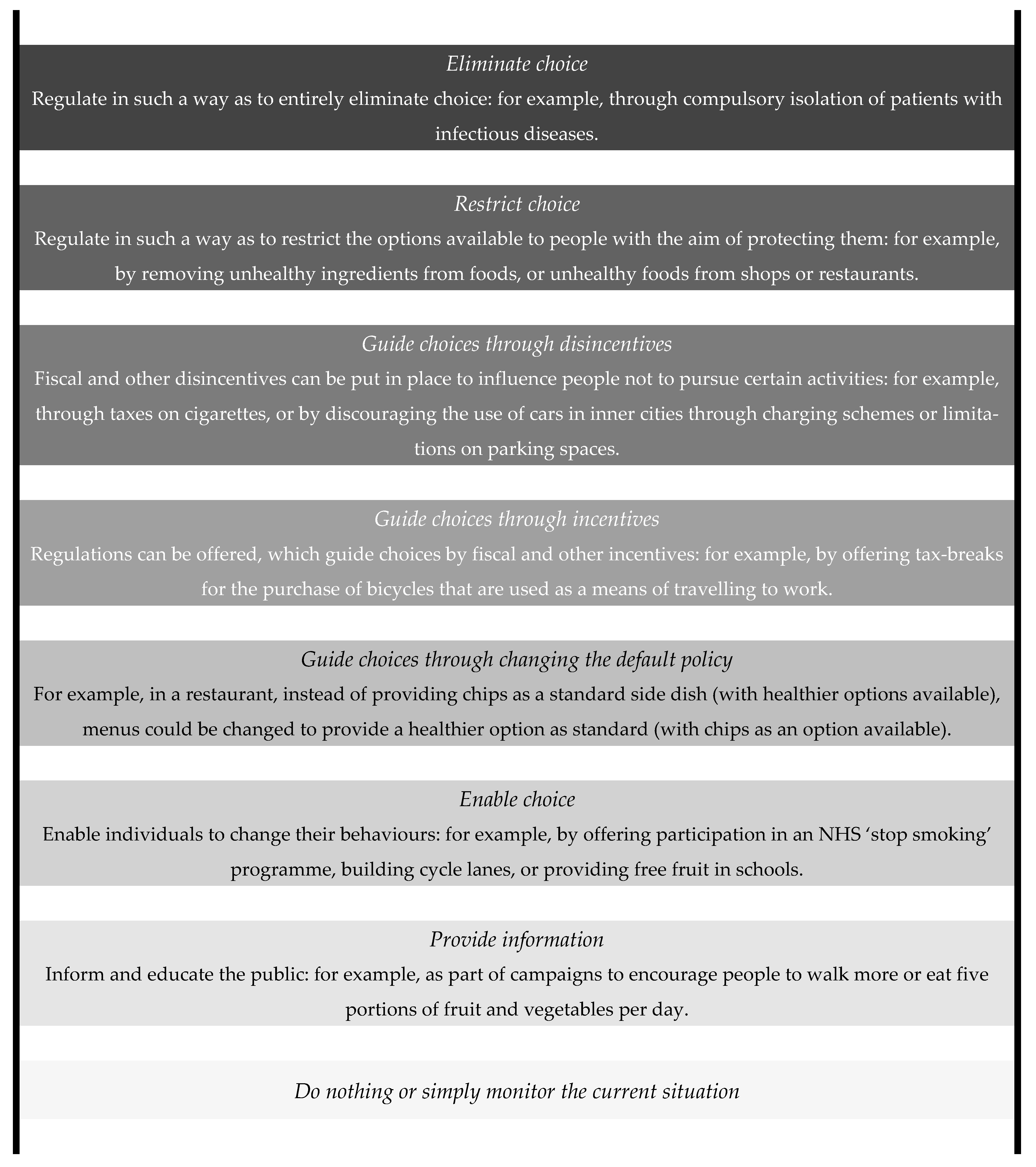
2. Can CWF Be an Issue of Public Health Ethics?
3. Slanted Rungs in the Intervention Ladder
4. Three Caveats for Ethical Considerations on Community Water Fluoridation
4.1. Procedural Justice: The End Does Not Always Justify The Means
4.2. Social Contexts: Comparing Apples and Oranges
4.3. Maintenance of Trust: Good Intentions and Good Works
5. Conclusions: You Can Lead a Horse to Water, but You Cannot Make It Drink
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Ten great public health achievements—United States, 1900–1999. MMWR Morb. Mortal Wkly. Rep. 1999, 48, 241.
- Armfield, J.; Akers, H. Risk perception and water fluoridation support and opposition in Australia. J. Public Health Dent. 2010, 70, 58–66. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, M.S.; Whiting, P.F.; Wilson, P.M.; Sutton, A.J.; Chestnutt, I.; Cooper, J.; Misso, K.; Bradley, M.; Treasure, E.; Kleijnen, J. Systematic review of water fluoridation. Br. Med. J. 2000, 321, 855–859. [Google Scholar] [CrossRef]
- Iheozor-Ejiofor, Z.; Worthington, H.V.; Walsh, T.; O’Malley, L.; Clarkson, J.E.; Macey, R.; Alam, R.; Tugwell, P.; Welch, V.; Glenny, A.M. Water fluoridation for the prevention of dental caries. Cochrane Database Syst. Rev. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- National Health and Medical Research Council. Information Paper—Water Fluoridation: Dental and Other Human Health Outcomes; National Health and Medical Research Council: Canberra, Australia, 2017. [Google Scholar]
- Choi, A.L.; Sun, G.; Zhang, Y.; Grandjean, P. Developmental fluoride neurotoxicity: A systematic review and meta-analysis. Environ. Health Perspect. 2012, 120, 1362–1368. [Google Scholar] [CrossRef]
- Green, R.; Lanphear, B.; Hornung, R.; Flora, D.; Martinez-Mier, E.A.; Neufeld, R.; Ayotte, P.; Muckle, G.; Till, C. Association Between Maternal Fluoride Exposure During Pregnancy and IQ Scores in Offspring in Canada. JAMA Pediatr. 2019. [Google Scholar] [CrossRef]
- Warren, J.J.; Levy, S.M.; Broffitt, B.; Cavanaugh, J.E.; Kanellis, M.J.; Weber-Gasparoni, K. Considerations on Optimal Fluoride Intake Using Dental Fluorosis and Dental Caries Outcomes—A Longitudinal Study. J. Public Health Dent. 2009, 69, 111–115. [Google Scholar] [CrossRef]
- Grandjean, P.; Choi, A.L.; Broadbent, J.M.; Thomson, W.M.; Moffitt, T.E.; Poulton, R. Community water fluoridation and intelligence. Am. J. Public Health 2015, 105, E3. [Google Scholar] [CrossRef] [PubMed]
- McLaren, L.; Patterson, S.; Thawer, S.; Faris, P.; McNeil, D.; Potestio, M. Fluoridation cessation: More science from Alberta. Community Dent. Oral Epidemiol. 2017, 45, 503–505. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haby, M.; Bowen, S. Making Decisions about Interventions. A Guide for Evidence-Informed Policy and Practice; Prevention and Population Health Branch, Victorian Government Department of Health: Melbourne, Australia, 2010. [Google Scholar]
- Cross, D.W.; Carton, R.J. Fluoridation: A violation of medical ethics and human rights. Int. J. Occup. Environ. Health 2003, 9, 24–29. [Google Scholar] [CrossRef]
- Awofeso, N. Ethics of Artificial Water Fluoridation in Australia. Public Health Ethics 2012, 5, 161–172. [Google Scholar] [CrossRef]
- Armfield, J.M. When public action undermines public health: A critical examination of antifluoridationist literature. Aust. New Zealand Health Policy 2007, 4, 25. [Google Scholar] [CrossRef]
- Daly, B.; Batchelor, P.; Treasure, E.; Watt, R. Essential Dental Public Health; Oxford University Press: Oxford, UK, 2013; pp. 8, 139–140, 144. [Google Scholar]
- Sheiham, A.; Watt, R. Oral health promotion and policy. In The Prevention of Oral Disease, 4th ed.; Murray, J.J., Nunn, J.H., Steele, J.G., Eds.; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Acheson, D. Public Health in England: The Report of the Committee of Inquiry into the Future Development of the Public Health Function; The Stationary Office: London, UK, 1988; pp. 23–34. [Google Scholar]
- Sanders, A.E. Social Determinants of Oral Health: Conditions Linked to Socioeconomic Inequalities in Oral Health in the Australian Population; Australian Institute of Health and Welfare (Media and Publishing Unit): Canberra, Australia, 2007. [Google Scholar]
- MacDonald, M. Introduction to Public Health Ethics: Background; National Collaborating Centre for Healthy Public Policy: Montreal, QC, Canada, 2014. [Google Scholar]
- Verweij, M.; Dawson, A. The meaning of ‘public’ in ‘public health’. Ethics Prev. Public Health 2007, 13–29. [Google Scholar]
- Beauchamp, T.L.; Childress, J.F. Principles of Biomedical Ethics; Oxford University Press: New York, NY, USA, 2001. [Google Scholar]
- Selgelid, M.J. A moderate pluralist approach to public health policy and ethics. Public Health Ethics 2009, 2, 195–205. [Google Scholar] [CrossRef]
- Childress, J.F.; Faden, R.R.; Gaare, R.D.; Gostin, L.O.; Kahn, J.; Bonnie, R.J.; Kass, N.E.; Mastroianni, A.C.; Moreno, J.D.; Nieburg, P. Public health ethics: Mapping the terrain. J. Law Med. Ethics 2002, 30, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.; Selgelid, M.J. Necessity and least infringement conditions in public health ethics. Med. Health Care Philos. 2017, 20, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Aoun, A.; Darwiche, F.; Al Hayek, S.; Doumit, J. The fluoride debate: The pros and cons of fluoridation. Prev. Nutr. Food Sci. 2018, 23, 171. [Google Scholar] [CrossRef]
- Mullane, D.; Baez, R.; Jones, S.; Lennon, M.; Petersen, P.E.; Rugg-Gunn, A.; Whelton, H.; Whitford, G.M. Fluoride and oral health. Community Dent. Health 2016, 33, 69–99. [Google Scholar]
- Bánóczy, J.; Rugg-Gunn, A.; Woodward, M. Milk fluoridation for the prevention of dental caries. Acta Med. Acad. 2013, 42, 156. [Google Scholar] [CrossRef]
- Dawson, A.J. Snakes and ladders: State interventions and the place of liberty in public health policy. J. Med. Ethics 2016, 42, 510–513. [Google Scholar] [CrossRef]
- Nuffield Council on Bioethics. Public Health: Ethical Issues; Nuffield Council on Bioethics: London, UK, 2007. [Google Scholar]
- Calman, K. Beyond the ‘nanny state’: Stewardship and public health. Public Health 2009, 123, e6–e10. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, P.; West, C. A balanced intervention ladder: Promoting autonomy through public health action. Public Health 2015, 129, 1092–1098. [Google Scholar] [CrossRef]
- Rose, G. Sick individuals and sick populations. Int. J. Epidemiol. 2001, 30, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Milio, N. Promoting Health through Public Policy; Canadian Public Health Association: Ottawa, ON, Canada, 1986. [Google Scholar]
- Baldwin, T.; Brownsword, R.; Schmidt, H. Stewardship, Paternalism and Public Health: Further Thoughts. Public Health Ethics 2009, 2, 113–116. [Google Scholar] [CrossRef]
- Upshur, R.E. Principles for the justification of public health intervention. Can. J. Public Health 2002, 101–103. [Google Scholar] [CrossRef]
- Bellefleur, O.; Keeling, M. Utilitarianism in Public Health. In Built Environment; National Collaborating Centre for Healthy Public Policy: Montréal, QC, Canada, 2016; Volume 15. [Google Scholar]
- Harrison, T.; Waite, K.; White, P. Analysis by paralysis: The pension purchase decision process. Int. J. Bank Mark. 2006, 24, 5–23. [Google Scholar] [CrossRef]
- Rawls, J. A Theory of Justice; Harvard University Press: Cambridge, MA, USA, 1971. [Google Scholar]
- Luhmann, N. Familiarity, confidence, trust: Problems and alternatives. In Trust: Making and Breaking Cooperative Relations; Gambetta, D., Ed.; University of Oxford: Oxford, UK, 2000; pp. 94–107. [Google Scholar]
- Wiser Healthcare. Community Juries. Available online: https://www.wiserhealthcare.org.au/community-juries/ (accessed on 9 February 2020).
- Daniels, N.; Sabin, J. The Ethics of Accountability in Managed Care Reform: Recent efforts at reforming managed care practices have one thing in common: A call for accountability to consumers. Health Aff. 1998, 17, 50–64. [Google Scholar] [CrossRef]
- Daniels, N.; Sabin, J. Limits to health care: Fair procedures, democratic deliberation, and the legitimacy problem for insurers. Philos. Public Aff. 1997, 26, 303–350. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.K.; Giacomini, M.; Singer, P.A. Fairness, accountability for reasonableness, and the views of priority setting decision-makers. Health Policy 2002, 61, 279–290. [Google Scholar] [CrossRef]
- Selgelid, M.J. Gain-of-function research: Ethical analysis. Sci. Eng. Ethics 2016, 22, 923–964. [Google Scholar] [CrossRef] [PubMed]
- Kikuzawa, S.; Olafsdottir, S.; Pescosolido, B.A. Similar pressures, different contexts: Public attitudes toward government intervention for health care in 21 nations. J. Health Soc. Behav. 2008, 49, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Viehbeck, S.M.; Petticrew, M.; Cummins, S. Old myths, new myths: Challenging myths in public health. Am. J. Public Health 2015, 105, 665–669. [Google Scholar] [CrossRef] [PubMed]
- Olivier, J.; Boufous, S.; Grzebieta, R. The impact of bicycle helmet legislation on cycling fatalities in Australia. Int. J. Epidemiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Busko, A.; Hubbard, Z.; Zakrison, T. Motorcycle-helmet laws and public health. N. Engl. J. Med. 2017, 376, 1208–1209. [Google Scholar] [CrossRef]
- Marx, P. About Face: Why Is South Korea the World’s Plastic-Surgery Capital? New Yorker, 23 March 2015. [Google Scholar]
- Jang, Y.E.; Kim, C.B.; Kim, N.H. Utilization of Preventive Dental Services Before and After Health Insurance Covered Dental Scaling in Korea: 2009 to 2014 Community Health Survey. Asia Pac. J. Public Health 2017, 29, 70–80. [Google Scholar] [CrossRef]
- Page, L. What Donald Trump would do with the US healthcare system. Br. Med. J. 2016, 353, i2996. [Google Scholar] [CrossRef]
- Dawson, A.; Verweij, M. Introduction: Ethics, prevention, and public health. In Ethics, Prevention, and Public Health; Dawson, A., Verweij, M., Eds.; Oxford University Press: New York, NY, USA, 2007; pp. 1–12. [Google Scholar]
- Ho, K.; Neidell, M. Equilibrium Effects of Public Goods: The Impact of Community Water Fluoridation on Dentists; National Bureau of Economic Research: Cambridge, MA, USA, 2009. [Google Scholar]
- Carstairs, C. Debating water fluoridation before Dr. Strangelove. Am. J. Public Health 2015, 105, 1559–1569. [Google Scholar] [CrossRef]
- Ward, P.R. Improving Access to, Use of, and Outcomes from Public Health Programs: The importance of Building and Maintaining Trust with Patients/Clients. Front. Public Health 2017, 5, 22. [Google Scholar] [CrossRef]
- Song, Y.; Luzzi, L.; Brennan, D.S. Trust in dentist-patient relationships: Mapping the relevant concepts. Eur. J. Oral Sci. 2020, 128, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Udow-Phillips, M.; Lantz, P.M. Trust in public health is essential amid the COVID-19 pandemic. J. Hosp. Med. 2020, 15, 431–433. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.L. Evaluating and Deploying Covid-19 Vaccines—The Importance of Transparency, Scientific Integrity, and Public Trust. N. Engl. J. Med. 2020, 383, 1703–1705. [Google Scholar] [CrossRef] [PubMed]
- Fawell, J.; Bailey, K.; Chilton, J.; Dahi, E.; Fewtrell, L.; Magara, Y. Fluoride in Drinking-Water; World Health Organization: Geneva, Switzerland, 2006; p. 79. [Google Scholar]
- Community Preventive Services Task Force. Oral Health: Preventing Dental Caries, Community Water Fluoridation. Available online: https://www.thecommunityguide.org/sites/default/files/assets/Oral-Health-Caries-Community-Water-Fluoridation_3.pdf (accessed on 13 February 2021).
- Project of the ABIM Foundation; ACP–ASIM Foundation; European Federation of Internal Medicine. Medical professionalism in the new millennium: A physician charter. Ann. Intern. Med. 2002, 136, 243–246. [CrossRef] [PubMed]
| Justificatory Condition | Meaning | Evaluation of Community Water Fluoridation (CWF) |
|---|---|---|
| Effectiveness | Interventions should protect public health effectively. | CWF has been confirmed to reduce dental caries effectively by empirical evidence [3,4,5]. |
| Proportionality | The probable public health benefits should outweigh the infringed moral considerations. | Social and psychological benefits from the decrease in dental caries outweigh the harm of infringed autonomy [26]. |
| Necessity/least infringement | The minimal infringement of moral considerations should have priority among other effective policies. | No other public health intervention can reduce dental caries of the general public as effectively as CWF. Milk fluoridation is also efficient with attached conditions [27] and salt fluoridation may induce hypertension as an adverse effect [25]. Fluoride supplementation holds a higher risk of harmful effects [26] and dental sealants are limited to individual beneficiaries. However, the amount of effects the infringement can affect may differ in accordance with the implementation of CWF. |
| Public justification | The infringement should be explained and justified to the relevant parties. | Further consideration is required for CWF. |
| Condition | Description | Application to Community Water Fluoridation (CWF) |
|---|---|---|
| Publicity | Rationales for decisions should be publicised and approachable. | Principles and evidence for CWF to be publicly accessible. |
| Relevance | Rationales to provide a reasonable construal of how to meet varied health needs of relevant parties. | Reasonable appraisal of the evidence and practice for CWF. |
| Revision | Mechanisms as a dispute resolution procedure for revisiting decisions in light of counter-arguments and further evidence. | Establishment of the procedure to re-evaluate the implementation of CWF. |
| Enforcement | Voluntary or public regulation to ensure conditions suggested are satisfied. | Developing a protocol to ensure the fulfillment of three conditions in CWF. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, Y.; Kim, J. Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health. Int. J. Environ. Res. Public Health 2021, 18, 2372. https://doi.org/10.3390/ijerph18052372
Song Y, Kim J. Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health. International Journal of Environmental Research and Public Health. 2021; 18(5):2372. https://doi.org/10.3390/ijerph18052372
Chicago/Turabian StyleSong, Youngha, and Junhewk Kim. 2021. "Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health" International Journal of Environmental Research and Public Health 18, no. 5: 2372. https://doi.org/10.3390/ijerph18052372
APA StyleSong, Y., & Kim, J. (2021). Community Water Fluoridation: Caveats to Implement Justice in Public Oral Health. International Journal of Environmental Research and Public Health, 18(5), 2372. https://doi.org/10.3390/ijerph18052372






