Sleep Indices and Cardiac Autonomic Activity Responses during an International Tournament in a Youth National Soccer Team
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
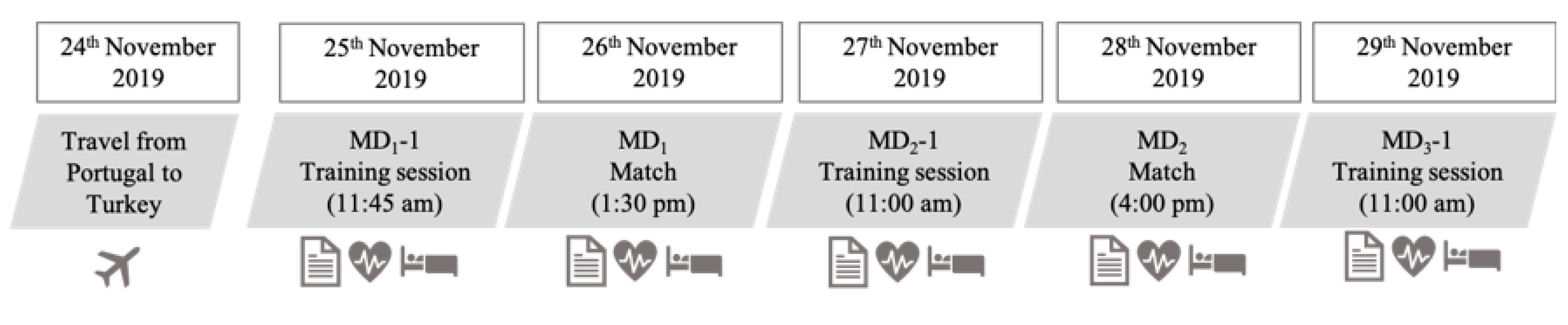
2.2. Procedures
2.3. Statistical Methods
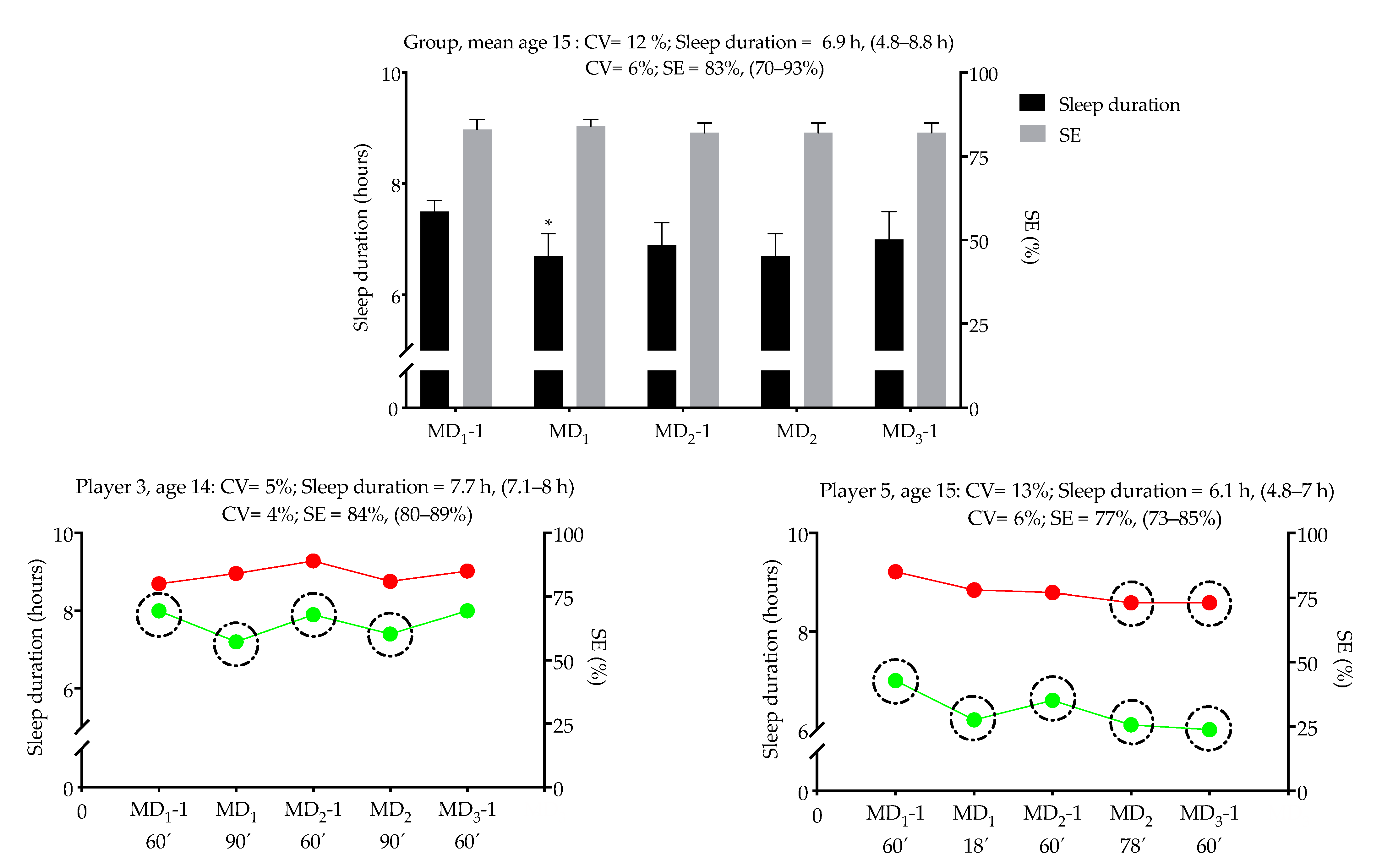
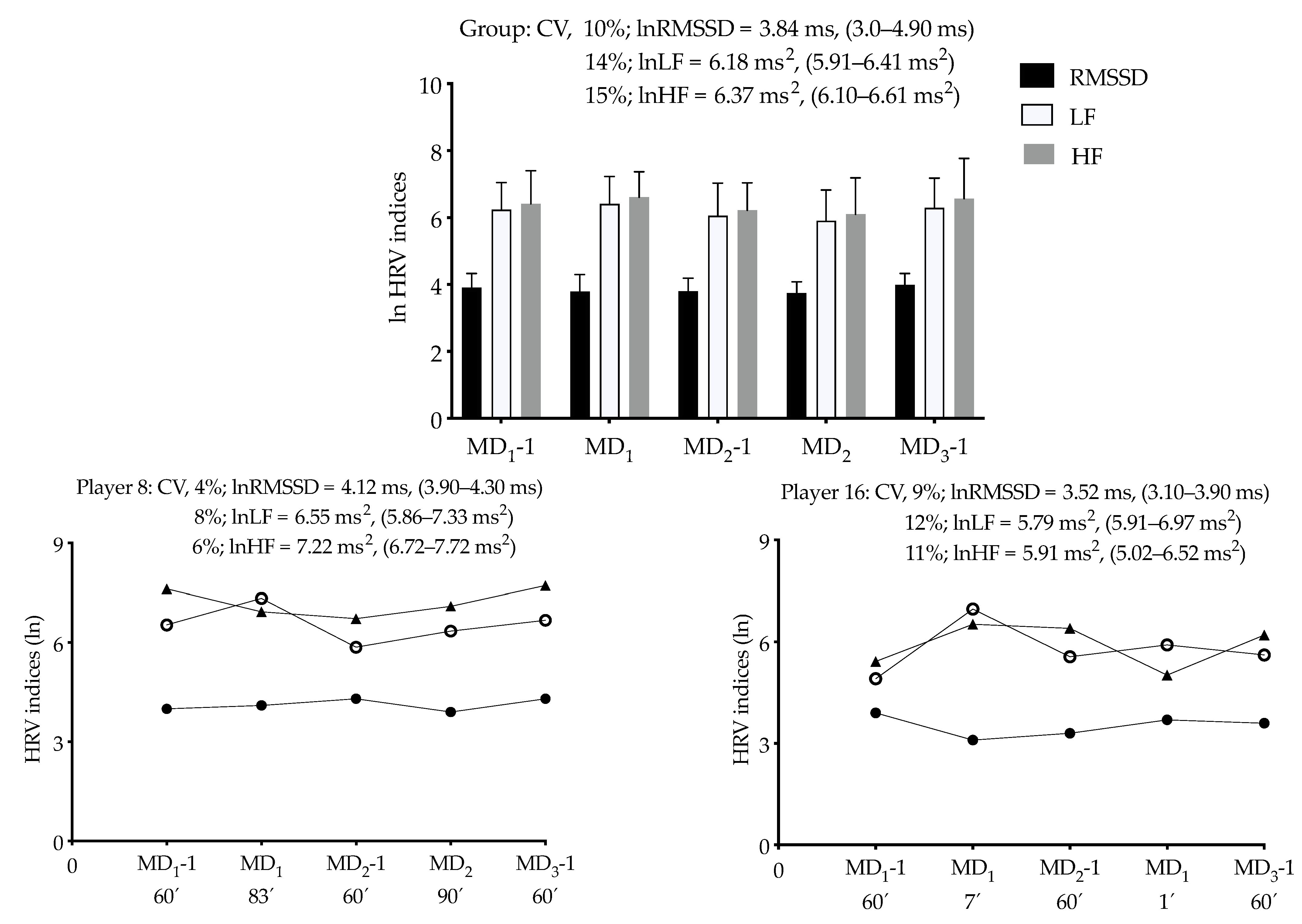
3. Results
3.1. Within-Subject Correlation between Sleep Indices and Nocturnal HRV
3.2. Within-Subject Correlation between Sleep Indices and Nocturnal HRV with Training/Match Load
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Halson, S.L. Sleep Monitoring in Athletes: Motivation, Methods, Miscalculations and Why it Matters. Sports Med. 2019, 49, 1487–1497. [Google Scholar] [CrossRef] [PubMed]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Healyh 2017, 3, 6–19. [Google Scholar] [CrossRef] [PubMed]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef] [PubMed]
- Sawczuk, T.; Jones, B.; Scantlebury, S.; Till, K. Influence of Perceptions of Sleep on Well-Being in Youth Athletes. J. Strength Cond. Res. 2018. [Google Scholar] [CrossRef]
- Fullagar, H.H.K.; Skorski, S.; Duffield, R.; Hammes, D.; Coutts, A.J.; Meyer, T. Sleep and Athletic Performance: The Effects of Sleep Loss on Exercise Performance, and Physiological and Cognitive Responses to Exercise. Sports Med. 2015, 45, 161–186. [Google Scholar] [CrossRef] [PubMed]
- Claudino, J.G.; Gabbett, T.J.; Souza, H.D.S.; Simim, M.; Fowler, P.; Borba, D.D.A.; Melo, M.; Bottino, A.; LoTurco, I.; D’Almeida, V.; et al. Which parameters to use for sleep quality monitoring in team sport athletes? A systematic review and meta-analysis. BMJ Open Sport Exerc. Med. 2019, 5, e000475. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.S.H.; Teo, W.-P.; Warmington, S.A. Effects of training and competition on the sleep of elite athletes: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 513–522. [Google Scholar] [CrossRef]
- Staunton, C.; Gordon, B.; Custovic, E.; Stanger, J.; Kingsley, M. Sleep patterns and match performance in elite Australian basketball athletes. J. Sci. Med. Sport 2017, 20, 786–789. [Google Scholar] [CrossRef]
- Chennaoui, M.; Arnal, P.J.; Sauvet, F.; Léger, D. Sleep and exercise: A reciprocal issue? Sleep Med. Rev. 2015, 20, 59–72. [Google Scholar] [CrossRef]
- Plews, D.J.; Laursen, P.B.; Buchheit, M. Day-to-Day Heart-Rate Variability Recordings in World-Champion Rowers: Appreciating Unique Athlete Characteristics. Int. J. Sports Physiol. Perform. 2017, 12, 697–703. [Google Scholar] [CrossRef]
- Pichot, V.; Busso, T.; Roche, F.; Garet, M.; Costes, F.; Duverney, D.; Lacour, J.-R.; Barthélémy, J.-C. Autonomic adaptations to intensive and overload training periods: A laboratory study. Med. Sci. Sports Exerc. 2002, 34, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Ebuchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef]
- De Freitas, V.H.; Pereira, L.A.; De Souza, E.A.; Leicht, A.S.; Bertollo, M.; Nakamura, F.Y. Sensitivity of the Yo-Yo Intermittent Recovery Test and Cardiac Autonomic Responses to Training in Futsal Players. Int. J. Sports Physiol. Perform. 2015, 10, 553–558. [Google Scholar] [CrossRef]
- Pichot, V.; Roche, F.; Gaspoz, J.M.; Enjolras, F.; Antoniadis, A.; Minini, P.; Costes, F.; Busso, T.; Lacour, J.R.; Barthélémy, J.C. Relation between heart rate variability and training load in middle-distance runners. Med. Sci. Sports Exerc. 2000, 32, 1729–1736. [Google Scholar] [CrossRef]
- Hynynen, E.; Uusitalo, A.; Konttinen, N.; Rusko, H. Heart Rate Variability during Night Sleep and after Awakening in Overtrained Athletes. Med. Sci. Sports Exerc. 2006, 38, 313–317. [Google Scholar] [CrossRef]
- Buchheit, M.; Simon, C.; Piquard, F.; Ehrhart, J.; Brandenberger, G. Effects of increased training load on vagal-related indexes of heart rate variability: A novel sleep approach. Am. J. Physiol. Circ. Physiol. 2004, 287, H2813–H2818. [Google Scholar] [CrossRef] [PubMed]
- Hausswirth, C.; Louis, J.; Aubry, A.; Bonnet, G.; Duffield, R.; Le Meur, Y. Evidence of Disturbed Sleep and Increased Illness in Overreached Endurance Athletes. Med. Sci. Sports Exerc. 2014, 46, 1036–1045. [Google Scholar] [CrossRef] [PubMed]
- Sekiguchi, Y.; Adams, W.M.; Benjamin, C.L.; Curtis, R.M.; Giersch, G.E.; Casa, D.J. Relationships between resting heart rate, heart rate variability and sleep characteristics among female collegiate cross-country athletes. J. Sleep Res. 2019, 28, e12836. [Google Scholar] [CrossRef]
- Furlan, R.; Piazza, S.; Dell’Orto, S.; Gentile, E.; Cerutti, S.; Pagani, M.; Malliani, A. Early and late effects of exercise and athletic training on neural mechanisms controlling heart rate. Cardiovasc. Res. 1993, 27, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.; Figueiredo, P.; Nakamura, F.; Rago, V.; Rebelo, A.; Brito, J. Intra-individual variability of sleep and nocturnal cardiac autonomic activity in elite female soccer players during an international tournament. PLoS ONE 2019, 14, e0218635. [Google Scholar] [CrossRef]
- Costa, J.A.; Brito, J.; Nakamura, F.Y.; Figueiredo, P.; Oliveira, E.; Rebelo, A. Sleep patterns and nocturnal cardiac autonomic activity in female athletes are affected by the timing of exercise and match location. Chrono- Int. 2018, 36, 360–373. [Google Scholar] [CrossRef]
- Costa, J.A.; Brito, J.; Nakamura, F.Y.; Oliveira, E.M.; Costa, O.P.; Rebelo, A.N. Does Night Training Load Affect Sleep Patterns and Nocturnal Cardiac Autonomic Activity in High-Level Female Soccer Players? Int. J. Sports Physiol. Perform. 2019, 14, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.A.; Brito, J.; Nakamura, F.Y.; Oliveira, E.M.; Rebelo, A.N. Effects of Late-Night Training on “Slow-Wave Sleep Episode” and Hour-by-Hour-Derived Nocturnal Cardiac Autonomic Activity in Female Soccer Players. Int. J. Sports Physiol. Perform. 2018, 13, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Lastella, M.; Roach, G.D.; Halson, S.L.; Sargent, C. Sleep/wake behaviours of elite athletes from individual and team sports. Eur. J. Sport Sci. 2015, 15, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Sargent, C.; Lastella, M.; Halson, S.L.; Roach, G.D. The impact of training schedules on the sleep and fatigue of elite athletes. Chrono- Int. 2014, 31, 1160–1168. [Google Scholar] [CrossRef]
- Muñoz-López, A.; Naranjo-Orellana, J. Individual versus team heart rate variability responsiveness analyses in a national soccer team during training camps. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Alsaadi, S.M.; McAuley, J.H.; Hush, J.M.; Bartlett, D.J.; McKeough, Z.M.; Grunstein, R.R.; Ii, G.C.D.; Maher, C.G. Assessing Sleep Disturbance in Low Back Pain: The Validity of Portable Instruments. PLoS ONE 2014, 9, e95824. [Google Scholar] [CrossRef]
- Sadeh, A.; Sharkey, K.M.; Carskadon, M.A. Activity-Based Sleep-Wake Identification: An Empirical Test of Methodological Issues. Sleep 1994, 17, 201–207. [Google Scholar] [CrossRef]
- Brandenberger, G.; Buchheit, M.; Ehrhart, J.; Simon, C.; Piquard, F. Is slow wave sleep an appropriate recording condition for heart rate variability analysis? Auton. Neurosci. 2005, 121, 81–86. [Google Scholar] [CrossRef] [PubMed]
- TaskForce. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Al Haddad, H.; Laursen, P.B.; Chollet, D.; Ahmaidi, S.; Buchheit, M. Reliability of Resting and Postexercise Heart Rate Measures. Int. J. Sports Med. 2011, 32, 598–605. [Google Scholar] [CrossRef]
- Foster, C.; Florhaug, J.A.; Franklin, J.; Gottschall, L.; Hrovatin, L.A.; Parker, S.; Doleshal, P.; Dodge, C. A new approach to monitoring exercise training. J. Strength Cond. Res. 2001, 15, 109–115. [Google Scholar] [PubMed]
- Bland, J.M.; Altman, D.G. Statistics notes: Calculating correlation coefficients with repeated observations: Part 1--correlation within subjects. BMJ 1995, 310, 446. [Google Scholar] [CrossRef]
- Makowski, D.; Ben-Shachar, M.S.; Patil, I.; Lüdecke, D. Methods and Algorithms for Correlation Analysis in R. J. Open Source Softw. 2020, 5, 2306. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef]
- Van Dongen, H.P.; Maislin, G.; Mullington, J.M.; Dinges, D.F. The Cumulative Cost of Additional Wakefulness: Dose-Response Effects on Neurobehavioral Functions and Sleep Physiology from Chronic Sleep Restriction and Total Sleep Deprivation. Sleep 2003, 26, 117–126. [Google Scholar] [CrossRef]
- Walsh, N.P.; Halson, S.L.; Sargent, C.; Roach, G.D.; Nédélec, M.; Gupta, L.; Leeder, J.; Fullagar, H.H.; Coutts, A.J.; Edwards, B.J.; et al. Sleep and the athlete: Narrative review and 2021 expert consensus recommendations. Br. J. Sports Med. 2020, 10, 1136. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef] [PubMed]
- Whitworth-Turner, C.M.; Di Michele, R.; Muir, I.; Gregson, W.; Drust, B. Training load and schedule are important determinants of sleep behaviours in youth-soccer players. Eur. J. Sport Sci. 2018, 19, 576–584. [Google Scholar] [CrossRef]
- Nédélec, M.; Dawson, B.; Dupont, G. Influence of Night Soccer Matches on Sleep in Elite Players. J. Strength Cond. Res. 2019, 33, 174–179. [Google Scholar] [CrossRef]
- Venter, R.E. Perceptions of team athletes on the importance of recovery modalities. Eur. J. Sport Sci. 2011, 14, S69–S76. [Google Scholar] [CrossRef]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Mohr, M.; Draganidis, D.; Chatzinikolaou, A.; Barbero-Álvarez, J.C.; Castagna, C.; Douroudos, I.; Avloniti, A.; Margeli, A.; Papassotiriou, I.; Flouris, A.D.; et al. Muscle damage, inflammatory, immune and performance responses to three football games in 1 week in competitive male players. Graefe’s Arch. Clin. Exp. Ophthalmol. 2015, 116, 179–193. [Google Scholar] [CrossRef]
- Buchheit, M.; Mendez-Villanueva, A.; Quod, M.J.; Poulos, N.; Bourdon, P. Determinants of the variability of heart rate measures during a competitive period in young soccer players. Graefe’s Arch. Clin. Exp. Ophthalmol. 2010, 109, 869–878. [Google Scholar] [CrossRef]
- Esco, M.R.; Snarr, R.L.; Flatt, A.; Leatherwood, M.; Whittaker, A. Tracking Changes in Maximal Oxygen Consumption with the Heart Rate Index in Female Collegiate Soccer Players. J. Hum. Kinet. 2014, 42, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Fantozzi, M.T.; Artoni, F.; Faraguna, U. Heart rate variability at bedtime predicts subsequent sleep features. In Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; Volume 2019, pp. 6784–6788. [Google Scholar]
- Sargent, C.; Lastella, M.; Halson, S.L.; Roach, G.D. The validity of activity monitors for measuring sleep in elite athletes. J. Sci. Med. Sport 2016, 19, 848–853. [Google Scholar] [CrossRef] [PubMed]
- Parak, J.; Korhonen, I. Accuracy of Firstbeat BodyGuard 2 Beat-to-Beat Heart Rate Monitor. Available online: https://www.firstbeat.com/app/uploads/2015/10/white_paper_bodyguard2_final.pdf (accessed on 8 May 2017).
| Variables | MD1-1 | MD1 | MD2-1 | MD2 | MD3-1 |
|---|---|---|---|---|---|
| Sleep duration (h) | 7.5 (7.0; 7.7) | 6.7 (6.3; 7.1) * | 6.9 (6.5; 7.3) | 6.8 (6.3; 7.1) | 7.0 (6.6; 7.5) |
| Sleep efficiency (%) | 83 (81; 86) | 84 (81; 86) | 82 (79; 85) | 82 (79; 85) | 82 (79; 85) |
| lnRMSSD (ms) | 3.9 (3.7; 4.1) | 3.8 (3.6; 4.0) | 3.9 (3.7; 4.1) | 3.8 (3.6; 4.0) | 4.1 (3.9; 4.3) |
| lnLF (ms2) | 6.2 (5.8; 6.7) | 6.4 (6.1; 7.0) | 6.1 (5.7; 6.6) | 5.9 (5.6; 6.5) | 6.3 (6.0; 7.0) |
| lnHF (ms2) | 6.4 (5.9; 6.9) | 6.6 (6.2; 7.2) | 6.2 (5.9; 6.8) | 6.1 (5.8; 6.7) | 6.6 (6.3; 7.4) |
| LF/HF | 0.9 (0.9; 1.1) | 0.9 (0.9; 1.1) | 0.9 (0.9; 1.0) | 0.9 (0.9; 1.1) | 0.9 (0.9; 1.0) |
| s-RPE (AU) | 233 (170; 320) | 388 (275; 548) * | 225 (161; 314) # | 469 (319; 689) *† | 251 (168; 375) ‡ |
| Sleep Duration | Sleep Efficiency | |||||
|---|---|---|---|---|---|---|
| r (95% CI) | p | Description | r (95% CI) | p | Description | |
| lnRMSSD | 0.22 (−0.05; 0.47) | 0.11 | Unclear | −0.12 (−0.38; 0.16) | 0.38 | Unclear |
| lnLF | 0.14 (−0.14; 0.40) | 0.32 | Unclear | −0.02 (−0.29; 0.26) | 0.91 | Unclear |
| lnHF | 0.22 (−0.06; 0.46) | 0.12 | Unclear | −0.04 (−0.31; 0.24) | 0.78 | Unclear |
| LF/HF | −0.002 (−0.38; 0.15) | −0.12 | Unclear | −0.002 (−0.27; 0.27) | 0.98 | Unclear |
| s-RPE | |||
|---|---|---|---|
| r (95% Confidence Interval) | p | Description | |
| Sleep duration | −0.41 (−0.62; −0.14) | 0.003 | Moderate |
| Sleep efficiency | −0.08 (−0.35; 0.21) | 0.59 | Unclear |
| lnRMSSD | −0.24 (−0.48; 0.04) | 0.08 | Unclear |
| lnLF | −0.12 (−0.38; 0.16) | 0.34 | Unclear |
| lnHF | −0.16 (−0.41; 0.12) | 0.27 | Unclear |
| LF/HF | −0.03 (−0.30; 0.25) | 0.82 | Unclear |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Figueiredo, P.; Costa, J.; Lastella, M.; Morais, J.; Brito, J. Sleep Indices and Cardiac Autonomic Activity Responses during an International Tournament in a Youth National Soccer Team. Int. J. Environ. Res. Public Health 2021, 18, 2076. https://doi.org/10.3390/ijerph18042076
Figueiredo P, Costa J, Lastella M, Morais J, Brito J. Sleep Indices and Cardiac Autonomic Activity Responses during an International Tournament in a Youth National Soccer Team. International Journal of Environmental Research and Public Health. 2021; 18(4):2076. https://doi.org/10.3390/ijerph18042076
Chicago/Turabian StyleFigueiredo, Pedro, Júlio Costa, Michele Lastella, João Morais, and João Brito. 2021. "Sleep Indices and Cardiac Autonomic Activity Responses during an International Tournament in a Youth National Soccer Team" International Journal of Environmental Research and Public Health 18, no. 4: 2076. https://doi.org/10.3390/ijerph18042076
APA StyleFigueiredo, P., Costa, J., Lastella, M., Morais, J., & Brito, J. (2021). Sleep Indices and Cardiac Autonomic Activity Responses during an International Tournament in a Youth National Soccer Team. International Journal of Environmental Research and Public Health, 18(4), 2076. https://doi.org/10.3390/ijerph18042076









