Analysis of Effectiveness of Individual and Group Trauma-Focused Interventions for Female Victims of Intimate Partner Violence
Abstract
1. Introduction
2. Materials and Methods
2.1. Objectives and Hypotheses
2.2. Participants
2.3. Design
2.4. Variables and Measures
2.4.1. Demographic Variables and History and Features of Violence
2.4.2. Outcome Variables
2.5. Procedure
2.6. Data Analysis
3. Results
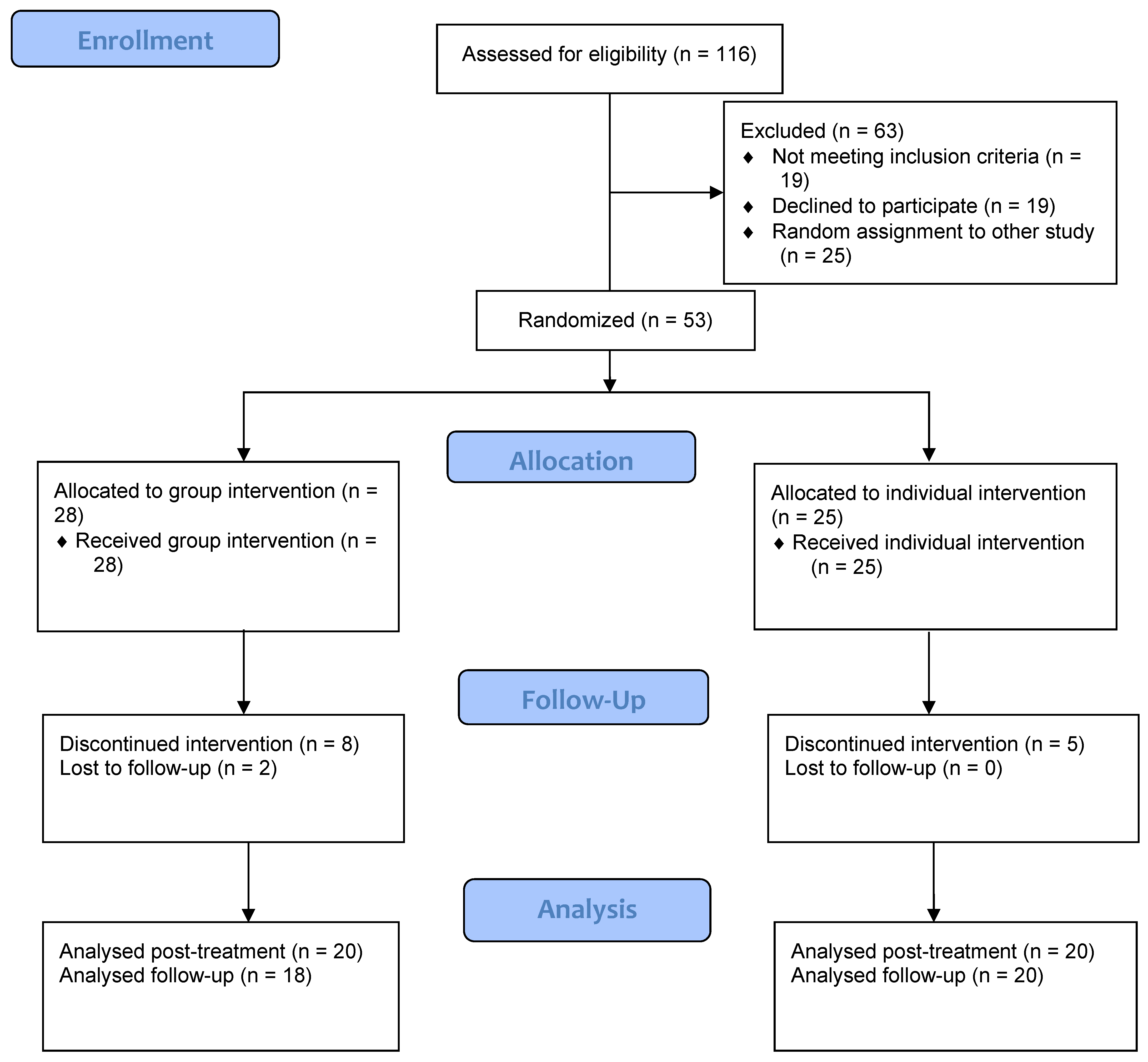
3.1. Adherence to Treatment
3.2. Sample Characteristics and Group Homogeneity
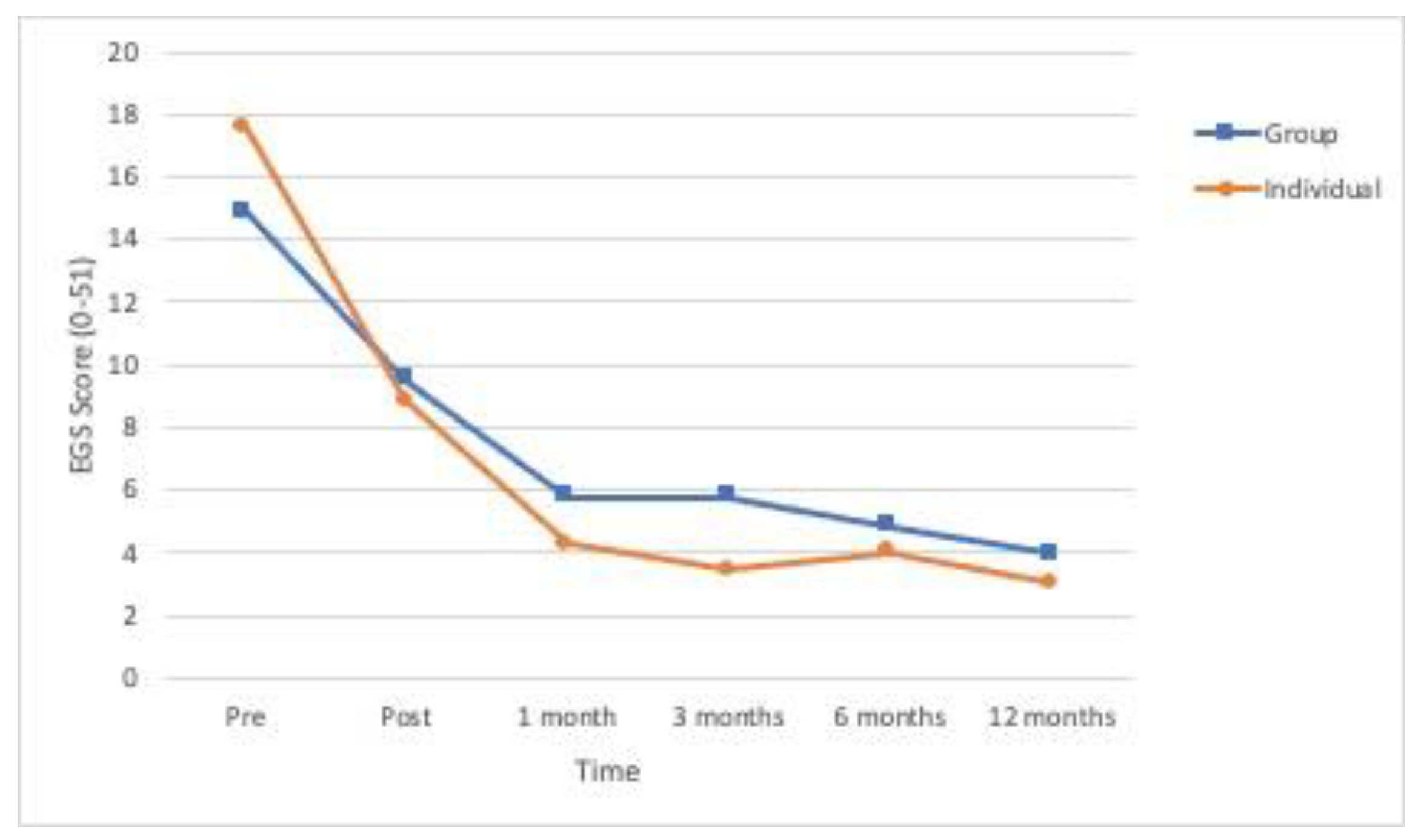
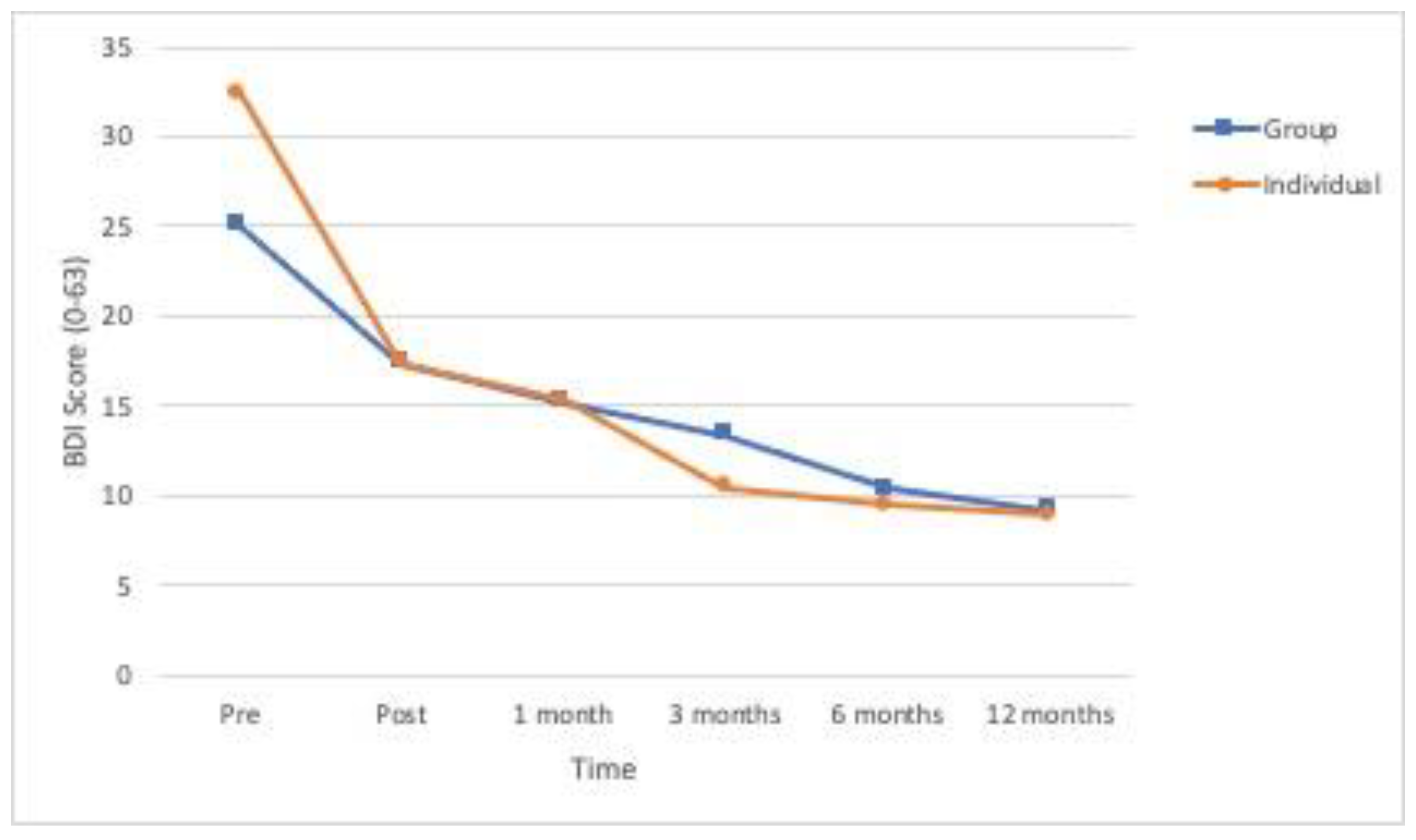
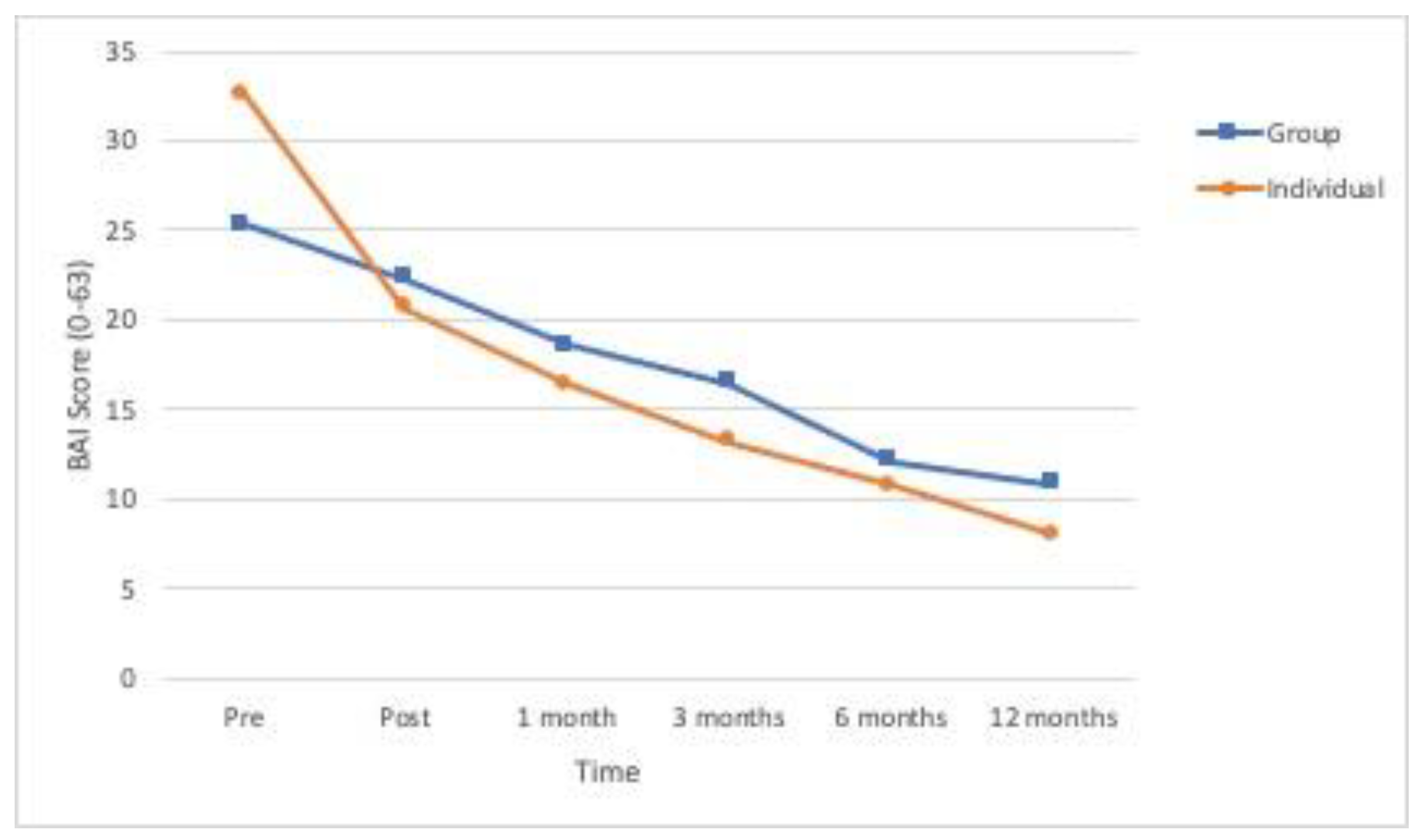
3.3. Treatment Effectiveness
3.4. Effect of Individual and Group Formats on Social Variables
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization; Department of Reproductive Health and Research; London School of Hygiene and Tropical Medicine; South African Medical Research Council. Global and Regional Estimates of Violence against Women: Prevalence and Health Effects of Intimate Partner Violence and Non-Partner Sexual Violence; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Domenech, I.; Sirvent, E. The consequences of intimate partner violence on health: A further disaggregation of psychological violence-evidence from Spain. Violence Women 2017, 23, 1771–1789. [Google Scholar] [CrossRef]
- Smith, S.G.; Zhang, X.; Basile, K.C.; Merrick, M.T.; Wang, J.; Kresnow, M.; Chen, J. The National Intimate Partner and Sexual Violence Survey (NISVS): 2015 Data Brief—Updated Release; National Center for Injury Prevention, and Control, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2018.
- Lagdon, S.; Armour, C.; Stringer, M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: A systematic review. Eur. J. Psychotraumatol. 2014, 5, 24794. [Google Scholar] [CrossRef]
- Koenen, K.C.; Ratanatharathorn, A.; Ng, L.; McLaughlin, K.A.; Bromet, E.J.; Stein, D.J.; Karam, E.G.; Ruscio, A.M.; Benjet, C.; Scott, K.; et al. Posttraumatic stress disorder in the world mental health surveys. Psychol. Med. 2017, 47, 2260–2274. [Google Scholar] [CrossRef]
- Coker, A.L.; Davis, K.E.; Arias, I.; Desai, S.; Sanderson, M.; Brandt, H.M.; Smith, P.H. Physical and mental health effects of intimate partner violence for men and women. Am. J. Prev. Med. 2002, 23, 260–268. [Google Scholar] [CrossRef]
- Pico-Alfonso, M.A.; Garcia-Linares, M.I.; Celda-Navarro, N.; Blasco-Ros, C.; Echeburúa, E.; Martinez, M. The impact of physical, psychological, and sexual intimate male partner violence on women’s mental health: Depressive symptoms, posttraumatic stress disorder, state anxiety, and suicide. J. Women’s Health 2006, 15, 599–611. [Google Scholar] [CrossRef]
- Nathanson, A.M.; Shorey, R.C.; Tirone, V.; Rhatigan, D.L. The prevalence of mental health disorders in a community sample of female victims of intimate partner violence. Partn. Abus. 2012, 3, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Helfrich, C.A.; Fujiura, G.T.; Rutkowski-Kmitta, V. Mental health disorders and functioning of women in domestic violence shelters. J. Interpers. Violence 2008, 23, 437–453. [Google Scholar] [CrossRef]
- Arroyo, K.; Lundahl, B.; Butters, R.; Vanderloo, M.; Wood, D.S. Short-term interventions for survivors of intimate partner violence: A systematic review and meta-analysis. Trauma Violence Abus. 2017, 18, 155–171. [Google Scholar] [CrossRef] [PubMed]
- Echeburúa, E.; Sarasua, B.; Zubizarreta, I. Individual versus individual and group therapy regarding a cognitive-behavioral treatment for battered women in a community setting. J. Interpers. Violence 2014, 29, 1783–1801. [Google Scholar] [CrossRef]
- Fernández-Velasco, M.R. Estrés Postraumático y Violencia de Pareja: Análisis de la Eficacia de Tratamientos Psicológicos. Ph.D. Dissertation, Universidad Complutense de Madrid, Madrid, Spain, 2014. [Google Scholar]
- Miller, L.E.; Howell, K.H.; Graham-Bermann, S.A. The effect of an evidence-based intervention on women’s exposure to intimate partner violence. Am. J. Orthopsychiatry 2014, 84, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Graham-Bermann, S.A.; Miller, L.E. Intervention to reduce traumatic stress following intimate partner violence: An efficacy trial of the moms’ empowerment program (MEP). Psychodyn. Psychiatry 2013, 41, 329–349. [Google Scholar] [CrossRef] [PubMed]
- Foy, D.W.; Glynn, S.M.; Schnurr, P.P.; Jankowski, M.K.; Wattenberg, M.S.; Weiss, D.S.; Gusman, F.D. Group therapy. In Effective Treatments for PTSD: Practice Guidelines from the International Society for Traumatic Stress Studies; Foa, E.B., Keane, T.M., Friedman, M.J., Eds.; Guilford Press: New York, NY, USA, 2000; pp. 336–338. [Google Scholar]
- Crespo, M.; Arinero, M. Assessment of the efficacy of a psychological treatment for women victims of violence by their intimate male partner. Span. J. Psychol. 2010, 13, 849–863. [Google Scholar] [CrossRef]
- Echeburúa, E.; De Corral, P.; Amor, P.J.; Zubizarreta, I.; Sarasua, B. Escala de gravedad de síntomas del trastorno de estrés postraumático: Propiedades psicométricas [Posttraumatic stress symptom severity scale: Psychometric properties]. Anál. Modif. Conducta 1997, 23, 503–526. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, C332. [Google Scholar] [CrossRef]
- Rincón, P.P.; Labrador, F.J. Transtorno de estrés postraumático en víctimas de maltrato doméstico: Evaluación de un programa de intervención [Posttraumatic stress disorder in victims of domestic violence: Assessment of an intervention program]. Anál. Modif. Conducta 2002, 28, 905–934. [Google Scholar]
- Ewing, J.A. Detecting alcoholism. The CAGE questionnaire. JAMA 1984, 252, 1905–1907. [Google Scholar] [CrossRef]
- Fonseca del Pozo, F.J.; Pérula de Torres, L.Á.; Martínez de La Iglesia, J. Detección de alcoholismo en una población general a través de la aplicación del test de Cage [The detection of alcoholism in a general population by using the CAGE test]. Aten. Primaria 1993, 11, 393–399. [Google Scholar]
- Rodríguez-Martos, A.; Navarro, R.; Vecino, C.; Pérez, R. Validación de los cuestionarios KFA (CBA) y CAGE para el diagnóstico del alcoholismo [Validation of KFA (CBA) and CAGE in the diagnosis of alcoholism]. Drogalcohol 1986, 11, 132–139. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Brown, G.K. BDI–II. Beck Depression Inventory–Second Edition Manual; The Psychological Corporation: San Antonio, TX, USA, 1996. [Google Scholar]
- Sanz, J.; Navarro, M.E.; Vázquez, C. Adaptación española del Inventario para la Depresión de Beck—II (BDI-II): 1. Propiedades psicométricas en estudiantes universitarios [Spanish adaptation of the Beck Depression Inventory-II (BDI-II): 1. Psychometric properties with university students]. Anál. Notif. Conducta 2003, 29, 239–288. [Google Scholar]
- Sanz, J.; Perdigón, A.L.; Vázquez, C. Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 2. Propiedades psicométricas en población general [The Spanish adaptation of Beck´s Depression Inventory-II (BDI-II): 2. Psychometric properties in the general population]. Clín. Salud. 2003, 14, 249–280. [Google Scholar]
- Sanz, J.; García-Vera, M.P.; Espinosa, R.; Fortún, M.; Vázquez, C. Adaptación española del Inventario para la Depresión de Beck-II (BDI-II): 3. Propiedades psicométricas en pacientes con trastornos psicológicos [Spanish adaptation of the Beck Depression Inventory-II (BDI-II): 3. Psychometric features in patients with psychological disorders]. Clín. Salud. 2005, 16, 121–142. [Google Scholar]
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psychol. 1988, 56, 893–897. [Google Scholar] [CrossRef] [PubMed]
- Sanz, J.; Navarro, M.E. Propiedades psicométricas de una versión española del inventario de ansiedad de beck (BAI) en estudiantes universitarios [The psychometric properties of a spanish version of the Beck Anxiety Inventory (BAI) in a university students’ sample]. Ansiedad Estrés 2003, 9, 59–84. [Google Scholar]
- Sanz, J. Recomendaciones para la utilización de la adaptación española del Inventario de Ansiedad de Beck (BAI) en la práctica clínica [Recommendations for the use of the Spanish adaptation of the Beck Anxiety Inventory (BAI) in clinical practice]. Clín. Salud. 2014, 25, 39–48. [Google Scholar] [CrossRef]
- Rosenberg, A. Society and the Adolescent Self-Image; Princeton University Press: Princeton, NJ, USA, 1965. [Google Scholar]
- Echeburúa, E.; Corral, P. Manual de Violencia Familiar [Family Violence Handbook]; Pirámide: Madrid, Spain, 1998. [Google Scholar]
- Larsen, D.L.; Attkisson, C.C.; Hargreaves, W.A.; Nguyen, T.D. Assessment of client/patient satisfaction: Development of a general scale. Eval. Program Plan. 1979, 2, 197–207. [Google Scholar] [CrossRef]
- Arinero, M.; Crespo, M. Evaluación de la eficacia de un programa de tratamiento psicológico para mujeres víctimas de maltrato doméstico: Estudio piloto [Assessment of the efficacy of a psychological program for female victims of domestic violence: Pilot study]. Psicol. Conduct. 2004, 12, 233–249. [Google Scholar]
- Little, R.J.A. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 1988, 83, 1198–1202. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Jacobson, N.S.; Roberts, L.J.; Berns, S.B.; McGlinchey, J.B. Methods for defining and determining the clinical significance of treatment effects: Description, application, and alternatives. J. Consult. Clin. Psychol. 1999, 67, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Hameed, M.; O’Doherty, L.; Gilchrist, G.; Tirado-Muñoz, J.; Taft, A.; Chondros, P.; Feder, G.; Tan, M.; Hegarty, K. Psychological therapies for women who experience intimate partner violence. Cochrane Database Syst. Rev. 2020, 7, CD013017. [Google Scholar] [CrossRef]
- Alonso, E.; Labrador, F.J. Eficacia de un programa de intervención para el trastorno de estrés postraumático en mujeres inmigrantes víctimas de violencia de pareja: Un estudio piloto [Effectiveness of a treatment program for immigrant women victims of partner violence, with postraumatic stress disorder: A pilot estudy]. Interam. J. Psychol. 2010, 44, 547–559. [Google Scholar]
- Cáceres, E. Tratamiento Psicológico Centrado en el Trauma en Mujeres Víctimas de Violencia de Pareja. Ph.D. Dissertation, Universidad Complutense de Madrid, Madrid, Spain, 2012. [Google Scholar]
- Labrador, F.J.; Alonso, E. Eficacia a corto plazo de un programa de intervención para el trastorno de estrés postraumático en mujeres mexicanas víctimas de violencia doméstica [Short term effectiveness of a treatment program for the posttraumatic stress disorder in Mexican women victims of domestic violence]. Rev. Psicopatol. Psicol. Clín. 2007, 12, 117–130. [Google Scholar] [CrossRef]
- Kubany, E.S.; Hill, E.E.; Owens, J.A. Cognitive trauma therapy for battered women with PTSD: Preliminary findings. J. Trauma Stress 2003, 16, 81–91. [Google Scholar] [CrossRef] [PubMed]
- Menon, B.; Stoklosa, H.; Van Dommelen, K.; Awerbuch, A.; Caddell, L.; Roberts, K.; Potter, J. Informing human trafficking clinical care through two systematic reviews on sexual assault and intimate partner violence. Trauma Violence Abus. 2020, 21, 932–945. [Google Scholar] [CrossRef] [PubMed]
- Trabold, N.; McMahon, J.; Alsobrooks, S.; Whitney, S.; Mittal, M. A systematic review of intimate partner violence interventions: State of the field and implications for practitioners. Trauma Violence Abus. 2020, 21, 311–325. [Google Scholar] [CrossRef] [PubMed]
- Warshaw, C.; Sullivan, C.M. A Systematic Review of Trauma-Focused Interventions for Domestic Violence Survivors; National Center on Domestic Violence, Trauma & Mental Health: East Lansing, MI, USA, 2013. [Google Scholar]
| Individual (n = 25) | Group (n = 28) | Statistics | p | Effect Size | |
|---|---|---|---|---|---|
| Age in years M (SD) | 38.04 (10.53) | 40.18 (9.95) | t (51) = −0.76 | 0.451 | d = 0.209 |
| Social class n (%) | Fisher exact test | 0.071 | - | ||
| Low | 6 (24.0) | 3 (10.7) | |||
| Medium-low | 4 (16.0) | 9 (32.1) | |||
| Medium | 15 (60) | 12 (42.9) | |||
| Medium-high | 0 (0.0) | 4 (14.3) | |||
| Marital status n (%) | Fisher exact test | 0.454 | - | ||
| Single | 7 (28.0) | 6 (21.4) | |||
| Living with stable partner | 3 (12.0) | 1 (3.6) | |||
| Married | 2 (8.0) | 6 (21.4) | |||
| Divorced | 13 (52.0) | 14 (50.0) | |||
| Widowed | 0 (0.0) | 1 (3.6) | |||
| Work status n (%) | Fisher exact test | 0.683 | - | ||
| Active | 5 (20.0) | 8 (28.6) | |||
| Unemployed | 7 (28.0) | 6 (21.4) | |||
| Housewife | 3 (12.0) | 6 (21.4) | |||
| Disabled | 1 (4.0) | 0 (0.0) | |||
| Educational n (%) | Fisher exact test | 0.269 | - | ||
| Incomplete primary studies | 5 (20.0) | 1 (3.6) | |||
| Complete primary studies | 9 (36.0) | 10 (35.7) | |||
| Secondary level | 9 (36.0) | 12 (42.9) | |||
| University level | 2 (8.0) | 5 (17.9) | |||
| Lives with aggressor n (%) | 7 (25.0) | 9 (32.1) | X2 (1,53) = 0.001 | 0.977 | Φ = 0.045 |
| Depends economically on aggressor n (%) | 8 (32.0) | 12 (42.9) | X2 (1,53) = 0.28 | 0.596 | Φ = 0.112 |
| Duration (years) of maltreatment M (SD) | 12.00 (10.89) | 10.61 (10.42) | t (51) = 0.48 | 0.636 | d = 0.130 |
| Frequency of maltreatment past month n (%) | Fisher exact test | 0.640 | - | ||
| Daily | 9 (36.0) | 15 (53.6) | |||
| Once a week | 3 (12.0) | 2 (7.1) | |||
| Once a month | 5 (20.0) | 5 (17.9) | |||
| Has not occurred | 8 (32.0) | 6 (21.4) | |||
| Type of maltreatment n (%) | Fisher exact test | 0.080 | - | ||
| Psychological | 11 (44) | 6 (21.4) | |||
| Physical | 0 (0.0) | 1 (3.6) | |||
| Psychological + Physical | 12 (48) | 19 (67.9) | |||
| Psychological + Sexual | 1 (4.0) | 0 (0.0) | |||
| Physical + Sexual | 1 (4.0) | 0 (0.0) | |||
| Physical + Psychological + Sexual | 0 (0.0) | 2 (7.1) | |||
| Has reported maltreatment n (%) | 17 (68.0) | 15 (53.6) | X2 (1,53) = 0.62 | 0.429 | Φ = −0.147 |
| Has had to leave home n (%) | 11 (44.0) | 17 (60.7) | X2 (1,53) = 0.89 | 0.347 | Φ = 0.167 |
| Medical attention n (%) | 9 (36.9) | 10 (35.7) | X2 (1,53) = 0.00 | 1.00 | Φ = −0.003 |
| Psychiatric/psychological attention n (%) | 7 (28.0) | 13 (46.4) | X2 (1,53) = 1.20 | 0.272 | Φ = 0.190 |
| Receives medication n (%) | 13 (52.0) | 15 (53.6) | X2 (1,53) = 0.00 | 1.00 | Φ = 0.016 |
| Legal support n (%) | 16 (64.0) | 12 (42.9) | X2 (1,53) = 1.60 | 0.206 | Φ = −0.211 |
| Family support n (%) | 20 (80) | 22 (78.6) | X2 (1,53) = 0.00 | 1.00 | Φ = −0.018 |
| Social support n (%) | 14 (56) | 18 (63.3) | X2 (1,53) = 0.11 | 0.738 | Φ = 0.085 |
| Suicidal ideation n (%) | 10 (40.0) | 17 (60.7) | X2 (1,53) = 1.51 | 0.218 | Φ = 0.207 |
| Posttraumatic symptoms (EGS) M (SD) (0–51) | 17.56 (6.44) | 14.86 (6.51) | t (51) = 1.51 | 0.136 | d = 0.041 |
| Depression (BDI) M (SD) (0–63) | 32.24 (12.61) | 24.18 (14.03) | t (51) = 2.08 | 0.042 | d = 0.596 |
| Anxiety (BAI) M (SD) (0–63) | 31.56 (11.83) | 24.48 (12.54) | t (51) = 2.05 | 0.045 | d = 0.563 |
| Self-esteem (Rosenberg’s) M (SD) (10–40) | 25.80 (4,06) | 28.00 (3.45) | t (51) = −3.20 | 0.002 | d = 0.874 |
| Alcohol consumption (CAGE) M (SD) (0–4) | 0.08 (0.27) | 0.14 (0.44) | t (51) = −0.49 | 0.042 | d = 0.136 |
| Variable | Individual (n = 25) | Group (n = 28) | ANOVA | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | Effect | F (1,51) | p | η2p | |
| PTSD (EGS) | ||||||||
| Pretreatment | 17.56 | 6.45 | 14.86 | 6.51 | Group | 0.30 | 0.584 | 0.006 |
| Posttreatment | 8.84 | 6.99 | 9.64 | 6.69 | Time | 65.15 | <0.001 | 0.561 |
| 1 month | 4.28 | 4.00 | 5.78 | 6.96 | Group × Time | 2.08 | 0.070 | 0.039 |
| 3 months | 3.44 | 3.90 | 5.78 | 6.15 | ||||
| 6 months | 4.04 | 3.72 | 4.86 | 5.83 | ||||
| 12 months | 3.04 | 3.76 | 3.96 | 5.21 | ||||
| Depression (BDI) | ||||||||
| Pretreatment | 32.44 | 12.84 | 25.03 | 13.00 | Group | 0.06 | 0.801 | 0.001 |
| Posttreatment | 17.36 | 10.82 | 17.36 | 14.48 | Time | 41.58 | <0.001 | 0.449 |
| 1 month | 15.28 | 10.49 | 15.25 | 12.13 | Group × Time | 2.45 | 0.034 | 0.046 |
| 3 months | 10.48 | 8.68 | 13.36 | 10.36 | ||||
| 6 months | 9.48 | 7.30 | 10.39 | 10.37 | ||||
| 12 months | 8.96 | 8.84 | 9.25 | 9.55 | ||||
| Anxiety (BAI) | ||||||||
| Pretreatment | 32.56 | 13.11 | 25.36 | 12.44 | Group | 0.079 | 0.780 | 0.002 |
| Posttreatment | 20.72 | 11.83 | 22.32 | 16.19 | Time | 35.13 | <0.001 | 0.408 |
| 1 month | 16.40 | 12.34 | 18.61 | 14.06 | Group × Time | 2.64 | 0.024 | 0.049 |
| 3 months | 13.24 | 10.88 | 16.50 | 14.03 | ||||
| 6 months | 10.76 | 9.21 | 12.14 | 8.43 | ||||
| 12 months | 8.00 | 7.23 | 10.82 | 9.00 | ||||
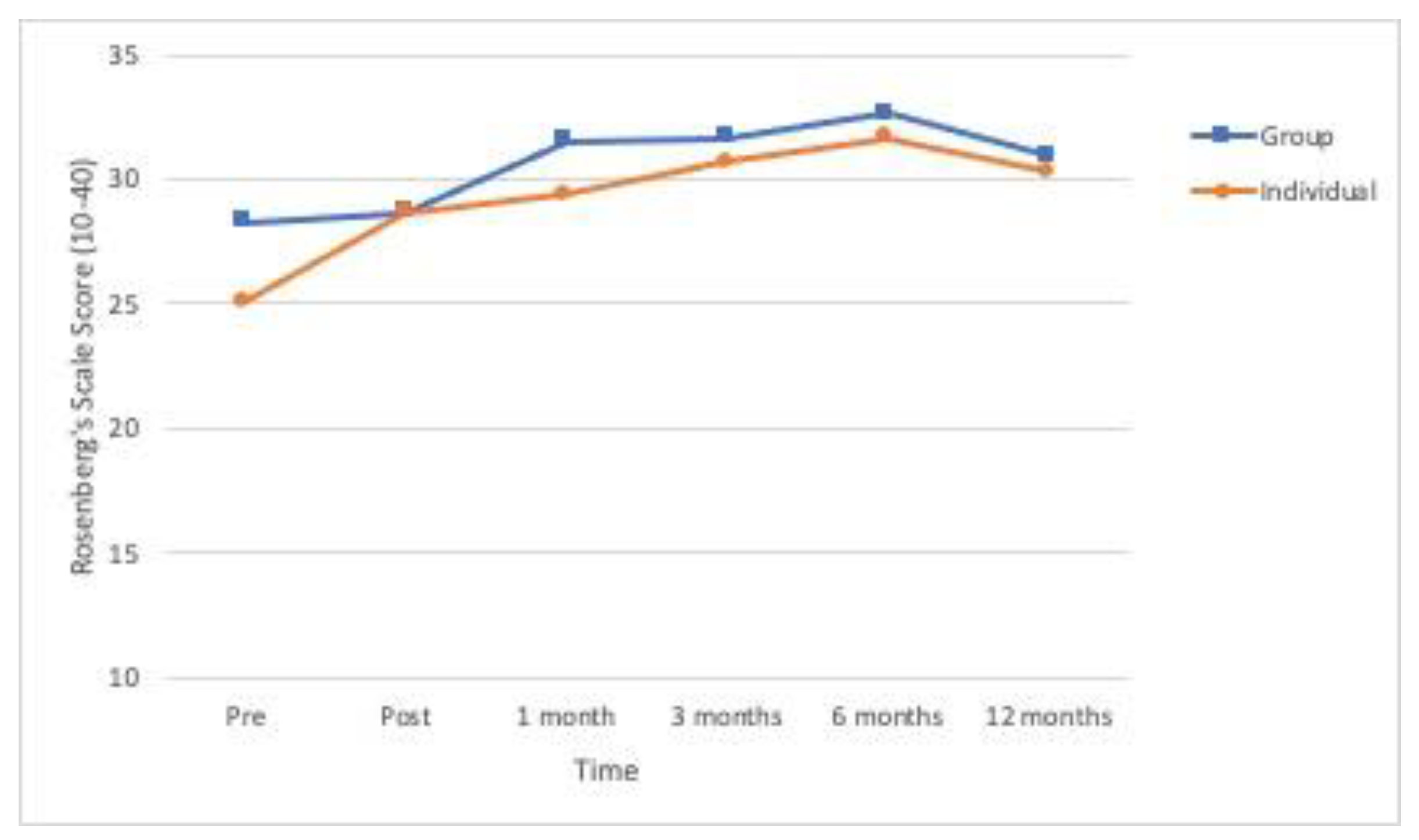
| Self-esteem (Rosenberg’s) | ||||||||
| Pretreatment | 25.12 | 4.05 | 28.28 | 3.12 | Group | 3.23 | 0.078 | 0.060 |
| Posttreatment | 28.68 | 3.21 | 28.64 | 4.18 | Time | 17.70 | <0.001 | 0.258 |
| 1 month | 29.40 | 3.01 | 31.50 | 3.40 | Group × Time | 1.52 | 0.184 | 0.029 |
| 3 months | 30.68 | 3.14 | 31.64 | 5.00 | ||||
| 6 months | 31.64 | 2.39 | 32.61 | 3.68 | ||||
| 12 months | 30.28 | 5.47 | 30.93 | 6.02 | ||||
| Individual (n = 25) | Group (n = 28) | Statistics | p | Φ | |
|---|---|---|---|---|---|
| Posttraumatic symptoms (EGS)n (%) | |||||
| Pretreatment | 15 (60) | 12 (42.9) | X2 (1,53) = 0.94 | 0.332 | −0.171 |
| Posttreatment | 6 (24.0) | 8 (28.6) | X2 (1,53) = 0.004 | 0.948 | 0.052 |
| 1 month | 1 (4.0) | 5 (17.9) | Fisher exact test | 0.196 | - |
| 3 months | 1 (4.0) | 2 (7.1) | Fisher exact test | 1.00 | - |
| 6 months | 0 (0.0) | 1 (3.6) | Fisher exact test | 1.00 | - |
| 12 months | 1 (4.0) | 2 (7.1) | Fisher exact test | 1.00 | - |
| Depression (BDI)n (%) | |||||
| Pretreatment | 24 (96.0) | 23 (82.1) | X2 (1,53) = 1.33 | 0.248 | −0.218 |
| Posttreatment | 15 (60.0) | 13 (46.4) | X2 (1,53) = 0.51 | 0.476 | −0.136 |
| 1 month | 11 (44.0) | 10 (35.7) | X2 (1,53) = 0.11 | 0.738 | −0.085 |
| 3 months | 7 (28.0) | 11 (29.3) | X2 (1,53) = 0.33 | 0.565 | 0.119 |
| 6 months | 7 (28.0) | 8 (28.6) | X2 (1,53) = 0.00 | 1.00 | 0.006 |
| 12 months | 5 (20.0) | 6 (21.4) | X2 (1,53) = 0.00 | 1.00 | 0.018 |
| Anxiety (BAI)n (%) | |||||
| Pretreatment | 24 (96.0) | 21 (75.0) | X2 (1,53) = 3.05 | 0.081 | −0.293 |
| Posttreatment | 19 (76.0) | 17 (60.7) | X2 (1,53) = 0.80 | 0.371 | −0.163 |
| 1 month | 15 (60.0) | 16 (57.1) | X2 (1,53) = 0.00 | 1.00 | −0.029 |
| 3 months | 9 (36.0) | 14 (50.0) | X2 (1,53) = 0.56 | 0.454 | 0.141 |
| 6 months | 10 (40.0) | 12 (42.9) | X2 (1,53) = 0.00 | 1.00 | 0.029 |
| 12 months | 7 (28.0) | 12 (42.9) | X2 (1,53) = 0.70 | 0.401 | 0.155 |
| Family supportn (%) | |||||
| Pretreatment | 20 (80.0) | 22 (78.6) | X2 (1,53) = 0.00 | 1.00 | −0.018 |
| Posttreatment | 18 (72.0) | 22 (78.6) | X2 (1,53) = 0.05 | 0.814 | 0.076 |
| 1 month | 18 (72.0) | 25 (89.3) | X2 (1,53) = 1.57 | 0.210 | 0.221 |
| 3 months | 21 (84.0) | 20 (71.4) | X2 (1,53) = 0.58 | 0.446 | −0.150 |
| 6 months | 18 (72.0) | 22 (78.6) | X2 (1,53) = 0.05 | 0.814 | 0.076 |
| 12 months | 17 (68.0) | 18 (64.3) | X2 (1,53) = 0.00 | 1.00 | −0.039 |
| Social supportn (%) | |||||
| Pretreatment | 14 (56.9) | 18 (64.3) | X2 (1,53) = 0.11 | 0.738 | 0.085 |
| Posttreatment | 22 (88.0) | 24 (85.7) | X2 (1,53) = 0.00 | 1.00 | −0.034 |
| 1 month | 19 (76.0) | 23 (82.1) | X2 (1,53) = 0.04 | 0.833 | 0.076 |
| 3 months | 21 (84.0) | 18 (64.3) | X2 (1,53) = 1.72 | 0.189 | −0.223 |
| 6 months | 20 (80.0) | 19 (67.9) | X2 (1,53) = 0.47 | 0.491 | −0.137 |
| 12 months | 22 (88.0) | 23 (82.1) | X2 (1,53) = 0.04 | 0.833 | −0.082 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Crespo, M.; Arinero, M.; Soberón, C. Analysis of Effectiveness of Individual and Group Trauma-Focused Interventions for Female Victims of Intimate Partner Violence. Int. J. Environ. Res. Public Health 2021, 18, 1952. https://doi.org/10.3390/ijerph18041952
Crespo M, Arinero M, Soberón C. Analysis of Effectiveness of Individual and Group Trauma-Focused Interventions for Female Victims of Intimate Partner Violence. International Journal of Environmental Research and Public Health. 2021; 18(4):1952. https://doi.org/10.3390/ijerph18041952
Chicago/Turabian StyleCrespo, María, María Arinero, and Carmen Soberón. 2021. "Analysis of Effectiveness of Individual and Group Trauma-Focused Interventions for Female Victims of Intimate Partner Violence" International Journal of Environmental Research and Public Health 18, no. 4: 1952. https://doi.org/10.3390/ijerph18041952
APA StyleCrespo, M., Arinero, M., & Soberón, C. (2021). Analysis of Effectiveness of Individual and Group Trauma-Focused Interventions for Female Victims of Intimate Partner Violence. International Journal of Environmental Research and Public Health, 18(4), 1952. https://doi.org/10.3390/ijerph18041952







