Effects of Dispositional Resilience and Self-Efficacy on Practice in Advanced Care Planning of Terminally Ill Patients among Taiwanese Nurses: A Study Using Path Modeling
Abstract
1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Instruments
2.2.1. Demographics and Work-Related Characteristics
2.2.2. Nurses’ Knowledge, Attitude, and Practice of ACP Inventory
2.2.3. Dispositional Resilience Scale
2.2.4. General Self-Efficacy Scale
2.3. Study Process
2.4. Statistical Analysis
3. Results
3.1. Demographics and Work-Related Characteristics
3.2. Knowledge, Attitude, and Practice toward ACP of Terminally Ill Patients, Dispositional Resilience, and Self-Efficacy among Nurses
3.3. Predictors of KAP-ACP of Terminally Ill Patients among Nurses
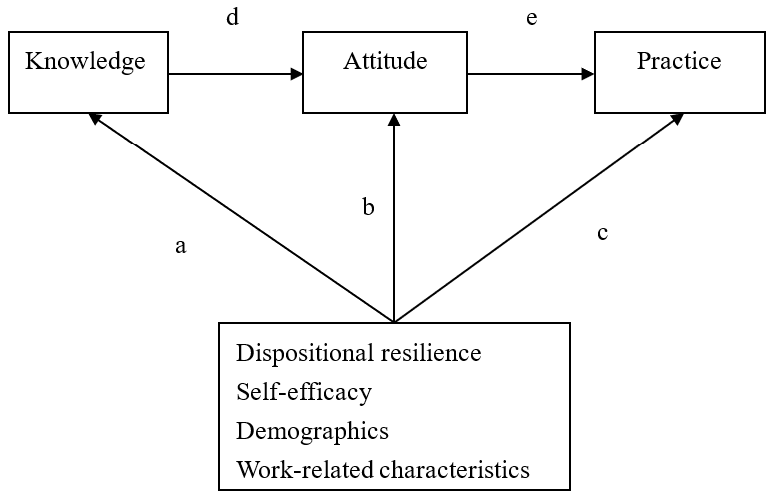
3.4. Path Modeling of KAP-ACP among Nurses
4. Discussion
4.1. Factors Affecting the KAP-ACP of Terminally Ill Patients among Nurses
4.2. Path Modeling of KAP-ACP of Terminally Ill Patients among Nurses
4.3. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hou, X.T.; Lu, Y.H.; Yang, H.; Guo, R.X.; Wang, Y.; Wen, L.H.; Zhang, Y.R.; Sun, H.Y. The knowledge and attitude towards advance care planning among Chinese patients with advanced cancer. J. Cancer Educ. 2019, 1–8. [Google Scholar] [CrossRef]
- Laws and Regulations Database of the Republic of China Hospice-Palliative Care Act. Available online: https://law.moj.gov.tw/ENG/ (accessed on 25 August 2020).
- Pereira-Salgado, A.; Philpot, S.; Schlieff, J.; O’Driscoll, L.; Mills, A. Advance care planning simulation-based learning for nurses: Mixed methods pilot study. Clin. Simul. Nurs. 2019, 29, 1–8. [Google Scholar] [CrossRef]
- Gleeson, A.; Noble, S.; Mann, M. Advance care planning for home health staff: A systematic review. BMJ Support. Palliat. Care 2019. [Google Scholar] [CrossRef]
- Martin, R.S.; Hayes, B.; Gregorevic, K.; Lim, W.K. The effects of advance care planning interventions on nursing home residents: A systematic review. J. Am. Med. Dir. Assoc. 2016, 17, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Detering, K.M.; Hancock, A.D.; Reade, M.C.; Silvester, W. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ Support. Palliat. Care 2010, 340, c1345. [Google Scholar] [CrossRef] [PubMed]
- Sung, H.C.; Wang, S.C.; Fan, S.Y.; Lin, C.Y. Advance care planning program and the knowledge and attitude concerning palliative care. Clin. Gerontol. 2019, 42, 238–246. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.C.; Huang, H.P.; Tung, T.H.; Chen, I.C.; Beaton, R.D.; Jane, S.W. The exploration of the knowledge, attitudes and practice behaviors of advanced care planning and its related predictors among Taiwanese nurses. BMC Palliat. Care 2019, 18, 99. [Google Scholar] [CrossRef]
- Jezewski, M.A.; Feng, J.-Y. Emergency nurses’ knowledge, attitudes, and experiential survey on advance directives. Appl. Nurs. Res. 2007, 20, 132–139. [Google Scholar] [CrossRef]
- Zhou, G.; Stoltzfus, J.C.; Houldin, A.D.; Parks, S.M.; Swan, B.A. Knowledge, attitudes, and practice behaviors of oncology advanced practice nurses regarding advanced care planning for patients with cancer. Oncol. Nurs. Forum 2010, 37, E400–E410. [Google Scholar] [CrossRef]
- Stage, F.K.; Carter, H.C.; Nora, A. Path analysis: An introduction and analysis of a decade of research. J. Educ. Res. 2004, 98, 5–13. [Google Scholar] [CrossRef]
- Wong, J.Y.; Fong, D.Y.; Choi, A.W.; Chan, C.K.; Tiwari, A.; Chan, K.L.; Lai, V.; Logan, T.; Bartone, P. Transcultural and psychometric validation of the Dispositional Resilience Scale (DRS-15) in Chinese adult women. Qual. Life Res. 2014, 23, 2489–2494. [Google Scholar] [CrossRef] [PubMed]
- Jerusalem, M.; Schwarzer, R. Self-efficacy as a resource factor in stress appraisal processes. In Self-Efficacy: Thought Control of Action; Hemisphere Publishing Corp: Washington, DC, USA, 1992; pp. 195–213. [Google Scholar]
- AlFayyad, I.N.; Al-Tannir, M.A.; AlEssa, W.A.; Heena, H.M.; Abu-Shaheen, A.K. Physicians and nurses’ knowledge and attitudes towards advance directives for cancer patients in Saudi Arabia. PLoS ONE 2019, 14, e0213938. [Google Scholar] [CrossRef] [PubMed]
- Van der Burgt, S.M.E.; Kusurkar, R.A.; Wilschut, J.A.; Tjin, A.T.S.; Croiset, G.; Peerdeman, S.M. Motivational profiles and motivation for lifelong learning of medical specialists. J. Contin. Educ. Health Prof. 2018, 38, 171–178. [Google Scholar] [CrossRef]
- Tjin, A.; Tsoi, S.L.N.M.; de Boer, A.; Croiset, G.; Koster, A.S.; Kusurkar, R.A. Unraveling motivational profiles of health care professionals for continuing education: The example of pharmacists in the Netherlands. J. Contin. Educ. Health Prof. 2016, 36, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Jezewski, M.A.; Brown, J.K.; Wu, Y.-W.B.; Meeker, M.A.; Feng, J.-Y.; Bu, X. Oncology nurses’ knowledge, attitudes, and experiences regarding advance directives. Oncol. Nurs. Forum 2005, 32, 319–328. [Google Scholar] [CrossRef]
- Haras, M.S.; Astroth, K.S.; Woith, W.L.; Kossman, S.P. Exploring advance care planning from the nephrology nurse perspective: A literature review. Nephrol. Nurs. J. 2015, 42, 23–35. [Google Scholar]
- Ryan, D.; Jezewski, M.A. Knowledge, attitudes, experiences, and confidence of nurses in completing advance directives: A systematic synthesis of three studies. J. Nurs. Res. 2012, 20, 131–141. [Google Scholar] [CrossRef]
- Toode, K.; Routasalo, P.; Helminen, M.; Suominen, T. Hospital nurses’ work motivation. Scand. J. Caring Sci. 2015, 29, 248–257. [Google Scholar] [CrossRef]
- Lai, Y.H.; Chen, M.L.; Tsai, L.Y.; Lo, L.H.; Wei, L.L.; Hong, M.Y.; Hsiu, L.N.; Hsiao-Sheen, S.T.; Chen, S.C.; Kao, C.C. Are nurses prepared to manage cancer pain? A national survey of nurses’ knowledge about pain control in Taiwan. J. Pain Symptom Manag. 2003, 26, 1016–1025. [Google Scholar] [CrossRef]
- Blackwood, D.H.; Walker, D.; Mythen, M.G.; Taylor, R.M.; Vindrola-Padros, C. Barriers to advance care planning with patients as perceived by nurses and other healthcare professionals: A systematic review. J. Clin. Nurs. 2019, 28, 4276–4297. [Google Scholar] [CrossRef]
- Caton, A.P.; Klemm, P. Introduction of novice oncology nurses to end-of-life care. Clin. J. Oncol. Nurs. 2006, 10, 604–608. [Google Scholar] [CrossRef] [PubMed]
- Chiang, F.M.; Hsieh, J.G.; Fan, S.Y.; Wang, Y.W.; Wang, S.C. Does the experience of caring for a severely disabled relative impact advance care planning? A qualitative study of caregivers of disabled patients. Int. J. Environ. Res. 2020, 17, 1594. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.F.; Chang, L.F.; Hung, Y.C.; Lin, C.; Tzou, S.J.; Chou, L.J.; Pan, H.H. The effect of practice toward do-not-resuscitate among Taiwanese nursing staff using path modeling. Int. J. Environ. Res. Public Health 2020, 17, 6350. [Google Scholar] [CrossRef] [PubMed]
- Brent, S.B.; Speece, M.W.; Gates, M.F.; Mood, D.; Kaul, M. The Contribution of Death-Related Experiences to Health Care Providers’ Attitudes toward Dying Patients: I. Graduate and Undergraduate Nursing Students. OMEGA J. Death Dying 1991, 23, 249–278. [Google Scholar] [CrossRef]
- Gilissen, J.; Pivodic, L.; Wendrich-van Dael, A.; Cools, W.; Vander Stichele, R.; Van den Block, L.; Deliens, L.; Gastmans, C. Nurses’ self-efficacy, rather than their knowledge, is associated with their engagement in advance care planning in nursing homes: A survey study. Palliat. Med. 2020, 34, 917–924. [Google Scholar] [CrossRef]
- Azmoude, E.; Farkhondeh, F.; Ahour, M.; Kabirian, M. Knowledge, practice and self-efficacy in evidence-based practice among midwives in East Iran. Sult. Qaboos Univ. Med. J. 2017, 17, e66. [Google Scholar] [CrossRef]
- Herliani, Y.; Harun, H.; Setyawati, A.; Ibrahim, K. Self-efficacy and the competency of nursing students toward the implementation of evidence-based practice. J. Ners. 2018, 13, 50–56. [Google Scholar] [CrossRef]
- Ludwick, R.; Baughman, K.R.; Jarjoura, D.; Kropp, D.J. CE: Original Research: Advance Care Planning: An Exploration of the Beliefs, Self-Efficacy, Education, and Practices of RNs and LPNs. Am. J. Nurs. 2018, 118, 26–32. [Google Scholar] [CrossRef]
- Manojlovich, M. Promoting nurses’ self-efficacy: A leadership strategy to improve practice. J. Nurs. Adm. 2005, 35, 271–278. [Google Scholar] [CrossRef]
- Elkady, A.A.M. Mindfulness and resilience as predictors of job burnout among nurses in public hospitals. Int. J. Psycho Educ. Sci. 2019, 8, 14–21. [Google Scholar]
- Yu, F.; Raphael, D.; Mackay, L.; Smith, M.; King, A. Personal and work-related factors associated with nurse resilience: A systematic review. Int. J. Nurs. Stud. 2019, 93, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Mirzaeirad, S.Z.; Arsalani, N.; Dalvandi, A.; Rezasoltani, P.; Hoseini, S.D. The effect of resilience skills training on nursing stress of nursing staff in hospitals of Golestan Province. J. Health Promot. Manag. 2019, 8, 41–48. [Google Scholar]
- Ko, E.; Kim, H.Y.; Bartone, P.T.; Kang, H.S. Reliability and validity of the Korean version of the 15-item Dispositional Resilience Scale. Psychol. Health Med. 2018, 23 (Suppl. 1), 1287–1298. [Google Scholar] [CrossRef] [PubMed]
- Shepherd, J.; Waller, A.; Sanson-Fisher, R.; Clark, K.; Ball, J. Knowledge of, and participation in, advance care planning: A cross-sectional study of acute and critical care nurses’ perceptions. Int. J. Nurs. Stud. 2018, 86, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Hanari, K.; Hamano, J.; Gallagher, J.; Tamiya, N. Current engagement in advance care planning in Japan and its associated factors. Gerontol. Geriatr. Med. 2019, 5. [Google Scholar] [CrossRef]
- Chow, K.M.; Tang, W.K.F.; Chan, W.H.C.; Sit, W.H.J.; Choi, K.C.; Sally, C. Resilience and well-being of university nursing students in Hong Kong: A cross-sectional study. BMC Med. Educ. 2018, 18, 1–8. [Google Scholar] [CrossRef]
- Cohen, A.; Nirenberg, A. Current practices in advance care planning. Clin. J. Oncol. Nurs. 2011, 15. [Google Scholar] [CrossRef]
- Yoo, S.H.; Lee, J.; Kang, J.H.; Maeng, C.H.; Kim, Y.J.; Song, E.K.; Koh, Y.; Yun, H.J.; Shim, H.J.; Kwon, J.H.; et al. Association of illness understanding with advance care planning and end-of-life care preferences for advanced cancer patients and their family members. Support Care Cancer 2020, 28, 2959–2967. [Google Scholar] [CrossRef]
- Berger, J.T.; Miller, D.R. Being Do Not Resuscitate. J. Palliat. Med. 2020, 23, 313. [Google Scholar] [CrossRef]
| Variable | N (%) /Mean ± SD |
|---|---|
| Demographics | |
| Age(year) | 30.1 ± 7.7 |
| Gender | |
| Female | 242 (91.0%) |
| Male | 24 (9.0%) |
| Education level | |
| Junior college | 34 (12.8%) |
| Bachelor | 211 (79.3%) |
| Master | 21 (7.9%) |
| Religious Belief | |
| No | 125 (47.0%) |
| Yes | 141 (53.0%) |
| Marital Status | |
| Single | 220 (82.7%) |
| Married | 46 (17.3%) |
| Work-related characteristics | |
| Ward | |
| HemaOnco | 31 (11.7%) |
| Medical | 53 (19.9%) |
| Surgical | 61 (22.9%) |
| ICU | 121 (45.5%) |
| Service duration in nursing (year) | 7.2 ± 6.9 |
| Caring for terminally ill friends or relatives | |
| No | 172 (64.7%) |
| Yes | 94 (35.3%) |
| Frequency of caring for terminally ill patients | 2.8 ± 1.1 |
| Participation in DNR signature | |
| No | 219 (82.3%) |
| Yes | 47 (17.7%) |
| Receiving education related to ACP | |
| No | 95 (35.7%) |
| Yes | 171 (64.3%) |
| Variable | Mean ± SD |
|---|---|
| Knowledge | 9.2 ± 0.8 |
| Proportion of correct answer (%) | 91.5 ± 8.4 |
| Attitude | 60.3 ± 7.7 |
| Practice | 34.9 ± 8.2 |
| Dispositional resilience | 27.6 ± 4.3 |
| Commitment | 8.3 ± 1.7 |
| Control | 10.0 ± 1.8 |
| Challenge | 9.3 ± 1.7 |
| Self-efficacy | 26.3 ± 5.4 |
| Knowledge | Attitude | Practice | |
|---|---|---|---|
| Variables | β (95%CI) | β (95%CI) | β (95%CI) |
| Knowledge | - | 2.32 *** (1.25~3.38) | 0.69 (−0.31~1.68) |
| Attitude | - | - | 0.21 *** (0.10~0.32) |
| Practice | - | - | - |
| Dispositional resilience | 0.01 (−0.02~0.04) | 0.11 (−0.14~0.35) | 0.36 ** (0.14~0.58) |
| Self-efficacy | −0.01 (−0.03~0.02) | −0.03 (−0.23~0.18) | 0.28 ** (0.10~0.47) |
| Demographics | |||
| Age (years) | −0.002 (−0.02~0.01) | 0.04 (−0.10~0.18) | −0.10 (−0.23~0.02) |
| Gender | |||
| Female | 0.49 ** (0.14~0.83) | −2.69 (−5.81~0.43) | 1.64 (−1.19~4.47) |
| Male | Reference | Reference | Reference |
| Education level | |||
| Junior college | −0.12 (−0.63~0.39) | −0.81 (−5.30~3.68) | −1.62 (−5.67~2.43) |
| Bachelor | −0.25 (−0.68~0.19) | −0.55 (−4.40~3.29) | −2.50 (−5.97~0.97) |
| Master | Reference | Reference | Reference |
| Religious belief | |||
| No | Reference | Reference | Reference |
| Yes | 0.02 (−0.19~0.23) | 1.50 (−0.34~3.34) | 0.40 (−1.28~2.07) |
| Marital status | |||
| Single | Reference | Reference | Reference |
| Married | −0.09 (−0.39~0.21) | −1.38 (−4.03~1.27) | −0.20 (−2.60~2.20) |
| Work-related characteristics | |||
| Ward | |||
| HemaOnco | 0.27 (−0.05~0.58) | 3.61 * (0.37~6.86) | 3.98 ** (1.21~6.74) |
| Medical | 0.46 *** (0.18~0.73) | 2.86 * (0.28~5.49) | 0.11 (−2.15~2.37) |
| Surgical | −0.06 (−0.32~0.20) | −0.10 (−2.50~2.29) | −2.85 ** (−4.92~−0.78) |
| ICU | Reference | Reference | Reference |
| Service duration in nursing | 0.001 (−0.01~0.02) | 0.02 (−0.11~0.16) | 0.02 (−0.11~0.16) |
| Caring for terminally ill friends or relatives | |||
| No | Reference | Reference | Reference |
| Yes | 0.01 (−0.23~0.25) | 2.20 * (0.11~4.29) | 0.48 (−1.43~2.39) |
| Frequency of caring for terminally ill patients | −0.01 (−0.10~0.09) | 0.26 (−0.58~1.10) | 1.91 *** (1.16~2.67) |
| Participation in DNR signature | |||
| No | Reference | Reference | Reference |
| Yes | −0.03 (−0.32~0.26) | −0.45 (−3.00~2.11) | 0.32 (−1.98~2.63) |
| Receiving education related to ACP | |||
| No | Reference | Reference | Reference |
| Yes | 0.01 (−0.29~0.30) | −0.38 (−2.98~2.22) | −1.14 (−3.50~1.21) |
| Knowledge→Attitude→Practice | Attitude→Practice | Practice | ||||
|---|---|---|---|---|---|---|
| Variables | Coefficients | p Value | Coefficients | p Value | Coefficients | p Value |
| Dispositional Resilience | 0.008 | 0.902 | 0.087 | 0.159 | 0.354 | <0.001 |
| Self-efficacy | 0.008 | 0.895 | 0.091 | 0.139 | 0.337 | <0.001 |
| Demographics | ||||||
| Age | −0.002 | 0.979 | −0.017 | 0.787 | −0.049 | 0.427 |
| Gender | ||||||
| Male/Female | −0.001 | 0.993 | −0.011 | 0.853 | −0.017 | 0.783 |
| Education level | ||||||
| Junior college/Master | 0.002 | 0.968 | 0.028 | 0.649 | 0.098 | 0.113 |
| Bachelor/Master | −0.002 | 0.975 | −0.024 | 0.693 | −0.092 | 0.136 |
| Religious Belief | ||||||
| Yes/No | 0.000 | 0.999 | 0.000 | 0.996 | 0.027 | 0.661 |
| Marital Status | ||||||
| Married/Single | −0.002 | 0.976 | −0.020 | 0.750 | −0.086 | 0.163 |
| Work-related characteristics | ||||||
| Ward | ||||||
| HemaOnco/ICU | −0.004 | 0.944 | −0.059 | 0.339 | 0.229 | <0.001 |
| Medical/ICU | 0.003 | 0.958 | 0.043 | 0.488 | 0.187 | 0.003 |
| Surgical/ICU | 0.003 | 0.966 | 0.037 | 0.553 | 0.165 | 0.008 |
| Service duration in nursing | −0.003 | 0.960 | −0.033 | 0.589 | −0.102 | 0.099 |
| Caring for terminally ill friends or relatives | ||||||
| Yes/No | 0.004 | 0.953 | 0.038 | 0.536 | 0.170 | 0.006 |
| Participation in DNR signature | ||||||
| Yes/No | 0.004 | 0.954 | 0.038 | 0.534 | 0.139 | 0.025 |
| Frequency of caring for terminally ill patients | 0.008 | 0.891 | 0.089 | 0.151 | 0.328 | <0.001 |
| Receiving education related to ACP | ||||||
| Yes/No | 0.002 | 0.969 | 0.028 | 0.651 | 0.094 | 0.128 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, H.-H.; Wu, L.-F.; Chang, L.-F.; Hung, Y.-C.; Lin, C.; Ho, C.-L. Effects of Dispositional Resilience and Self-Efficacy on Practice in Advanced Care Planning of Terminally Ill Patients among Taiwanese Nurses: A Study Using Path Modeling. Int. J. Environ. Res. Public Health 2021, 18, 1236. https://doi.org/10.3390/ijerph18031236
Pan H-H, Wu L-F, Chang L-F, Hung Y-C, Lin C, Ho C-L. Effects of Dispositional Resilience and Self-Efficacy on Practice in Advanced Care Planning of Terminally Ill Patients among Taiwanese Nurses: A Study Using Path Modeling. International Journal of Environmental Research and Public Health. 2021; 18(3):1236. https://doi.org/10.3390/ijerph18031236
Chicago/Turabian StylePan, Hsueh-Hsing, Li-Fen Wu, Li-Fang Chang, Yu-Chun Hung, Chin Lin, and Ching-Liang Ho. 2021. "Effects of Dispositional Resilience and Self-Efficacy on Practice in Advanced Care Planning of Terminally Ill Patients among Taiwanese Nurses: A Study Using Path Modeling" International Journal of Environmental Research and Public Health 18, no. 3: 1236. https://doi.org/10.3390/ijerph18031236
APA StylePan, H.-H., Wu, L.-F., Chang, L.-F., Hung, Y.-C., Lin, C., & Ho, C.-L. (2021). Effects of Dispositional Resilience and Self-Efficacy on Practice in Advanced Care Planning of Terminally Ill Patients among Taiwanese Nurses: A Study Using Path Modeling. International Journal of Environmental Research and Public Health, 18(3), 1236. https://doi.org/10.3390/ijerph18031236







