How Are We Managing Patients with Hyperuricemia and Gout: A Cross Sectional Study Assessing Knowledge and Attitudes of Primary Care Physicians?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Survey
2.3. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, L.; Zhang, Y.; Zeng, C. Update on the epidemiology, genetics, and therapeutic options of hyperuricemia. Am. J. Transl. Res. 2020, 12, 3167–3181. [Google Scholar] [PubMed]
- Halperin Kuhns, V.L.; Woodward, O.M. Sex Differences in Urate Handling. Int. J. Mol. Sci. 2020, 21, 4269. [Google Scholar] [CrossRef] [PubMed]
- Koto, R.; Nakajima, A.; Horiuchi, H.; Yamanaka, H. Real-world treatment of gout and asymptomatic hyperuricemia: A cross-sectional study of Japanese health insurance claims data. Mod. Rheumatol. 2021, 31, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Koto, R.; Nakajima, A.; Horiuchi, H.; Yamanaka, H. Factors associated with achieving target serum uric acid level and occurrence of gouty arthritis: A retrospective observational study of Japanese health insurance claims data. Pharmacoepidemiol. Drug Saf. 2020. [Google Scholar] [CrossRef]
- Abhishek, A.; Roddy, E.; Doherty, M. Gout—A guide for the general and acute physicians. Clin. Med. 2017, 17, 54–59. [Google Scholar] [CrossRef]
- Winder, M.; Owczarek, A.J.; Mossakowska, M.; Broczek, K.; Grodzicki, T.; Wierucki, Ł.; Chudek, J. Prevalence of Hyperuricemia and the Use of Allopurinol in Older Poles-Results from a Population-Based PolSenior Study. Int. J. Environ. Res. Public Health 2021, 18, 387. [Google Scholar] [CrossRef]
- Miljković, A.; Pehlić, M.; Budimir, D.; Gunjača, G.; Mudnić, I.; Pavić, A.; Jerončić, I.; Kolčić, I.; Boban, M.; Hayward, C.; et al. Can genetics aggravate the health of isolated and remote populations? The case of gout, hyperuricaemia and osteoarthritis in Dalmatia. Rural Remote Health 2013, 13, 2153. [Google Scholar]
- Vučak, J.; Katić, M.; Bielen, I.; Vrdoljak, D.; Lalić, D.I.; Kranjčević, K.; Marković, B.B. Association between hyperuricemia, prediabetes, and prehypertension in the Croatian adult population—A cross-sectional study. BMC Cardiovasc. Disord. 2012, 12, 117. [Google Scholar] [CrossRef]
- Li, Y.W.; Chen, W.L. Clinical relevance of serum uric acid and abdominal aortic-calcification in a national survey. Clin. Cardiol. 2020, 43, 1194–1201. [Google Scholar] [CrossRef]
- Heron, M.; Anderson, R.N. Changes in the Leading Cause of Death: Recent Patterns in Heart Disease and Cancer Mortality. NCHS Data Brief 2016, 254, 1–8. [Google Scholar]
- Zhao, D.; Liu, J.; Wang, M.; Zhang, X.; Zhou, M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat. Rev. Cardiol. 2019, 16, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Economic Burden of Cardiovascular Disease in Type 2 Diabetes: A Systematic Review. Value Health 2018, 21, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Luengo-Fernandez, R.; Leal, J.; Gray, A.; Petersen, S.; Rayner, M. Cost of cardiovascular diseases in the United Kingdom. Heart 2006, 92, 1384–1389. [Google Scholar] [CrossRef] [PubMed]
- Siqueira, A.S.E.; Siqueira-Filho, A.G.; Land, M.G.P. Analysis of the Economic Impact of Cardiovascular Diseases in the Last Five Years in Brazil. Arq. Bras. Cardiol. 2017, 109, 39–46. [Google Scholar] [CrossRef]
- Sample Size Calculator. Available online: https://www.surveymonkey.com/mp/sample-size-calculator/ (accessed on 20 March 2020).
- Hrvatski Zavod za Zdravstveno Osiguranje. Ugovoreni Sadržaji Zdravstvene Zaštite u RH. Available online: https://www.hzzo.hr/zdravstveni-sustav-rh/zdravstvena-zastita-pokrivena-obveznim-zdravstvenim-osiguranjem/ugovoreni-sadrzaji-zdravstvene-zastite-u-rh/ (accessed on 20 March 2020).
- Alqarni, N.A.; Hassan, A.H. Knowledge and practice in the management of asymptomatic hyperuricemia among primary health care physicians in Jeddah, Western Region of Saudi Arabia. Saudi Med. J. 2018, 39, 1218–1225. [Google Scholar] [CrossRef]
- Kostka-Jeziorny, K.; Widecka, K.; Tykarski, A. Study of epidemiological aspects of hyperuricemia in Poland. Cardiol. J. 2019, 26, 241–252. [Google Scholar] [CrossRef]
- Keenan, R.T. The biology of urate. Semin. Arthritis Rheum. 2020, 50, S2–S10. [Google Scholar] [CrossRef]
- Gois, P.H.F.; Souza, E.R.M. Pharmacotherapy for hyperuricaemia in hypertensive patients. The Cochrane database of systematic reviews. Cochrane Database Syst. Rev. 2020, 9, CD008652. [Google Scholar]
- Braga, F.; Pasqualetti, S.; Ferraro, S.; Panteghini, M. Hyperuricemia as risk factor for coronary heart disease incidence and mortality in the general population: A systematic review and meta-analysis. Clin. Chem. Lab. Med. 2016, 54, 7–15. [Google Scholar] [CrossRef]
- Kumric, M.; Borovac, J.A.; Kurir, T.T.; Bozic, J. Clinical Implications of Uric Acid in Heart Failure: A Comprehensive Review. Life 2021, 11, 53. [Google Scholar] [CrossRef]
- Kaya, M.G.; Uyarel, H.; Akpek, M.; Kalay, N.; Ergelen, M.; Ayhan, E.; Isik, T.; Cicek, G.; Elcik, D.; Sahin, O.; et al. Prognostic value of uric acid in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Am. J. Cardiol. 2012, 109, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Mandurino-Mirizzi, A.; Cornara, S.; Somaschini, A.; Demarchi, A.; Galazzi, M.; Puccio, S.; Montalto, C.; Crimi, G.; Ferlini, M.; Camporotondo, R.; et al. Elevated serum uric acid is associated with a greater inflammatory response and with short- and long-term mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Nutr. Metab. Cardiovasc. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mandurino-Mirizzi, A.; Demarchi, A.; Ruffinazzi, M.; Cornara, S.; Somaschini, A.; Crimi, G.; Ferlini, M.; Camporotondo, R.; Gnecchi, M.; Ferrario, M.; et al. Serum uric acid may modulate the inflammatory response after primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. J. Cardiovasc. Med. 2020, 21, 337–339. [Google Scholar] [CrossRef] [PubMed]
- Chia, F.L. Poorly controlled gout: Who is doing poorly? Singap. Med. J. 2016, 57, 412–414. [Google Scholar] [CrossRef]
- Day, R.; Nguyen, A.; Graham, G.; Aung, E.; Coleshill, M.; Stocker, S. Better outcomes for patients with gout. Inflammopharmacology 2020, 28, 1395–1400. [Google Scholar] [CrossRef]
- Dore, R.K. Gout: What primary care physicians want to know. J. Clin. Rheumatol. 2008, 14, S47–S54. [Google Scholar] [CrossRef]
- Skoczynska, M.; Chowaniec, M.; Szymczak, A.; Langner-Hetmanczuk, A.; Maciazek-Chyra, B.; Wiland, P. Pathophysiology of hyperuricemia and its clinical significance—A narrative review. Reumatologia 2020, 58, 312–323. [Google Scholar] [CrossRef]
- Pillinger, M.H.; Mandell, B.F. Therapeutic approaches in the treatment of gout. Semin. Arthritis Rheum. 2020, 50, S24–S30. [Google Scholar] [CrossRef]
| Total | 336 (100%) |
|---|---|
| Gender (N) | |
| Men | 61 (18.2%) |
| Women | 275 (81.8%) |
| Age (years) | |
| <30 | 46 (13.7%) |
| 31–54 | 171 (50.9%) |
| >55 | 119 (35.4%) |
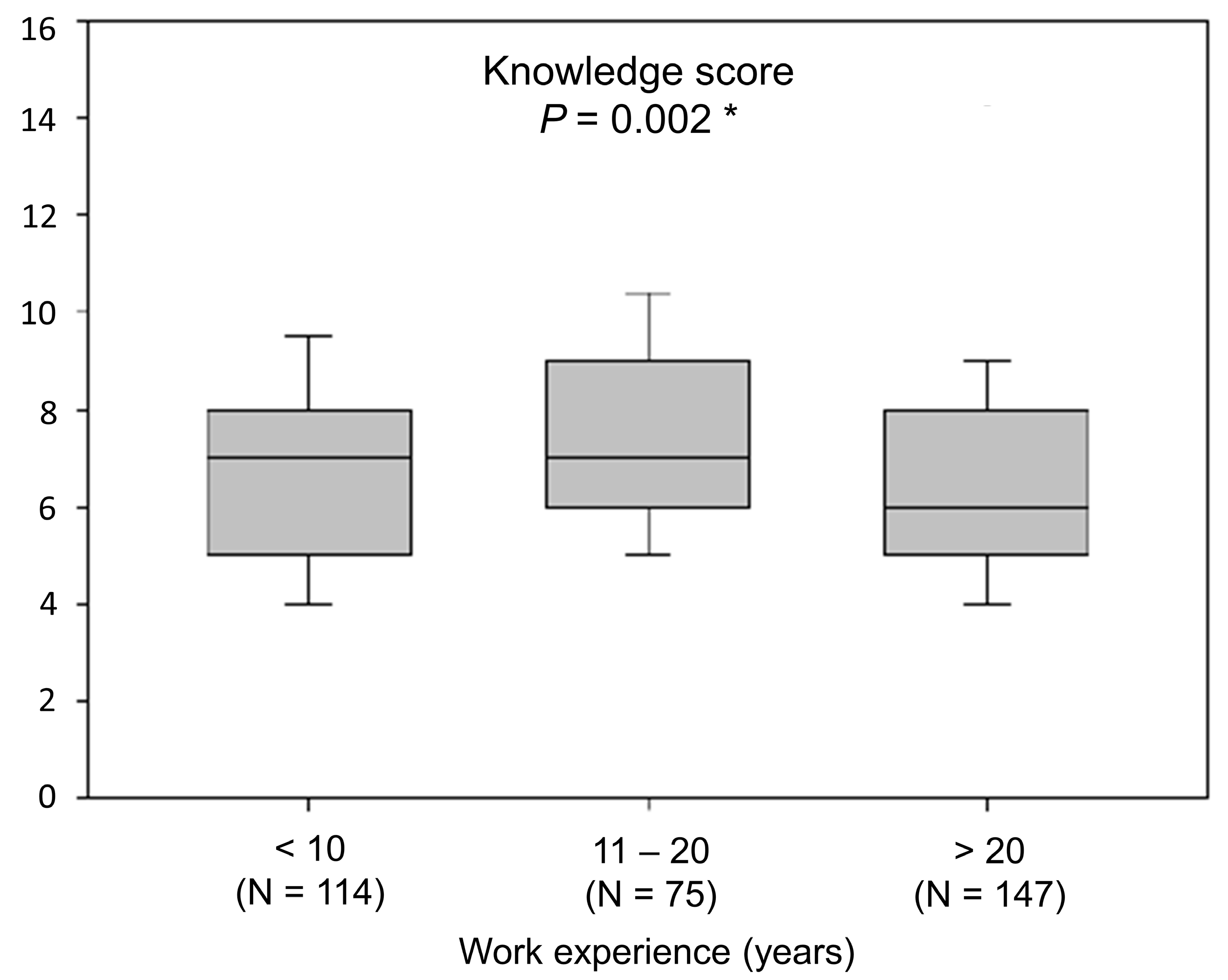
| Work experience (years) | |
| <5 | 55 (16.4%) |
| 5–10 | 59 (17.6%) |
| 11–20 | 75 (22.3%) |
| >20 | 147 (43.7%) |
| General practitioner | 106 (31.5%) |
| Family medicine specialist | 183 (54.5%) |
| Family medicine resident | 47 (14.0%) |
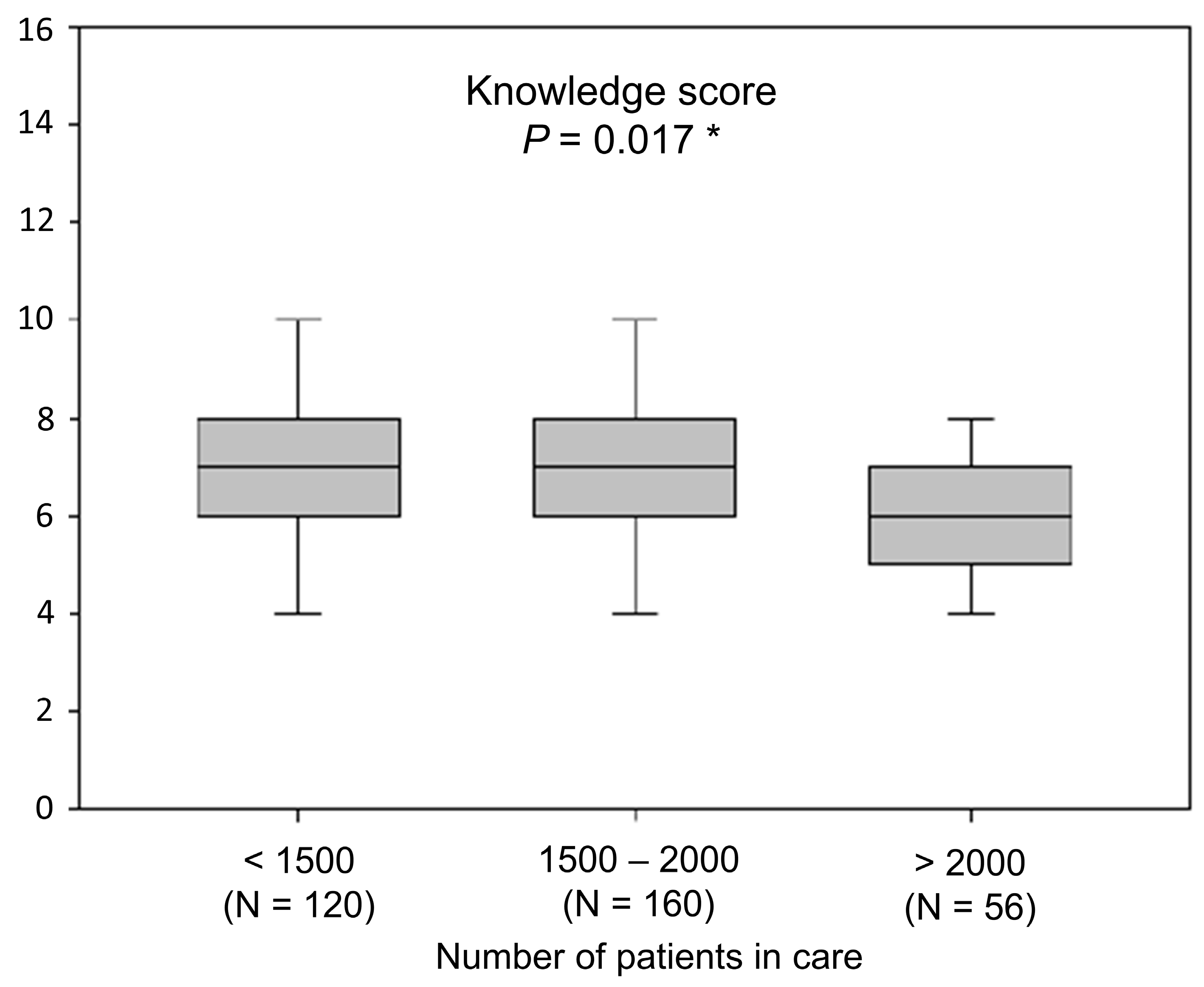
| Number of patients in care | |
| <500 | 5 (1.5%) |
| 500–1000 | 25 (7.4%) |
| 1000–1500 | 90 (26.8%) |
| 1500–2000 | 160 (47.6%) |
| >2000 | 56 (16.7%) |
| Population of work location area | |
| <5000 | 103 (30.7%) |
| 5000–50,000 | 88 (26.2%) |
| 50,000–150,000 | 36 (10.7%) |
| 150,000–300,000 | 51 (15.2%) |
| >300,000 | 58 (17.3%) |
| Patients with Hyperuricemia in Care (N) | |
|---|---|
| <100 | 227 (67.6%) |
| 100–300 | 94 (28.0%) |
| >300 | 15 (4.5%) |
| Cases of asymptomatic hyperuricemia in daily practice (N per month) | |
| 0 | 8 (2.4%) |
| 1 | 61 (18.2%) |
| 5–10 | 220 (65.5%) |
| 11–29 | 36 (10.7%) |
| ≥30 | 11 (3.3%) |
| Cases of gout in daily practice (N per month) | |
| 0 | 32 (9.5%) |
| 1 | 217 (64.6%) |
| 5–10 | 83 (24.7%) |
| 11–29 | 4 (1.2%) |
| ≥30 | 0 (0.0%) |
| Patients with hyperuricemia receiving pharmacological treatment in care | |
| ≤5% | 101 (30.1%) |
| 6%–10% | 73 (21.7%) |
| 11%–30% | 95 (28.3%) |
| 31%–60% | 51 (15.2%) |
| >60% | 16 (4.8%) |
| Scientific papers on asymptomatic hyperuricemia/gout read in the past year (N) | |
| 0 | 152 (45.2%) |
| 1 | 126 (37.5%) |
| 2 | 40 (11.9%) |
| 3 | 9 (2.7%) |
| 4 and more | 9 (2.7%) |
| How often do you refer a newly diagnosed gout patient to a rheumatologist? | |
| Never | 198 (58.9%) |
| In 10% of cases | 119 (35.4%) |
| In 11%–30% of cases | 8 (2.4%) |
| In 31%–50% of cases | 6 (1.8%) |
| Consistently | 5 (1.8%) |
| Fully Disagree | Disagree | Unsure | Agree | Fully Agree | |
|---|---|---|---|---|---|
| I am satisfied with my approach to care of patients with asymptomatic hyperuricemia. | 2 (0.6%) | 41 (12.2%) | 128 (38.1%) | 147 (43.7%) | 18 (5.4%) |
| I am satisfied with my approach to care of patients with gout. | 1 (0.3%) | 20 (6.0%) | 83 (24.7%) | 199 (59.2%) | 33 (9.8%) |
| I am satisfied with my success in changing lifestyle of patients with asymptomatic hyperuricemia/gout. | 25 (7.4%) | 110 (32.7%) | 123 (36.6%) | 74 (22.0%) | 4 (1.2%) |
| I am familiar with the EULAR evidence-based recommendations for the management of gout. | 59 (17.6%) | 83 (24.7%) | 102 (30.4%) | 81 (24.1%) | 11 (3.3%) |
| I use EULAR evidence-based recommendations for the management of gout in everyday practice. | 66 (19.6%) | 76 (22.6%) | 112 (33.3%) | 78 (23.2%) | 4 (1.2%) |
| I approach patients with asymptomatic hyperuricemia mostly based on my clinical experience. | 8 (2.4%) | 28 (8.3%) | 74 (22.0%) | 194 (57.7%) | 32 (9.5%) |
| I believe that guidelines for management of patients with asymptomatic hyperuricemia would be of great assistance in my everyday practice. | 2 (0.6%) | 3 (0.9%) | 26 (7.7%) | 105 (31.2%) | 200 (59.5%) |
| National referent values of serum uric acid levels are important cut-off values for everyday decisions about starting pharmacotherapy in patients with asymptomatic hyperuricemia. | 2 (0.6%) | 20 (6.0%) | 80 (23.8%) | 148 (44.0%) | 86 (25.6%) |
| Number (%) of Physicians Who Answered Correctly | |
|---|---|
| 1. Non-pharmacological interventions for hyperuricemia | 296 (88.1%) |
| 2. Drug classes for treatment of hyperuricemia registered in Croatia | 261 (77.7%) |
| 3. Treatment for gout flares | 260 (77.4%) |
| 4. Second line of treatment of hyperuricemia | 250 (74.4%) |
| 5. Treatment approach in asymptomatic hyperuricemia | 233 (69.3%) |
| 6. Identifying drugs that elevate serum uric acid levels | 211 (62.8%) |
| 7. Identifying drugs that lower serum uric acid levels | 158 (47.0%) |
| 8. Diagnostic procedure for confirmation of gout diagnosis | 122 (36.3%) |
| 9. Relationship of asymptomatic hyperuricemia and gout | 115 (34.2%) |
| 10. The expected effect of non-pharmacological treatment options for lowering hyperuricemia | 100 (29.8%) |
| 11. Drugs for lowering hyperuricemia registered in Croatia (with reference to the most likely cause of hyperuricemia in most patients) | 94 (28.0%) |
| 12. Cut-off value of serum uric levels for initiation of pharmacological treatment | 71 (21.1%) |
| 13. Asymptomatic hyperuricemia as a risk factor | 46 (13.7%) |
| 14. Most common reason of elevated urate levels | 44 (13.1%) |
| 15. The goal when treating hyperuricemia | 13 (3.9%) |
| 16. Definition of asymptomatic hyperuricemia | 10 (3%) |
| Factor | Β | SE | t | p * |
|---|---|---|---|---|
| Age (years) | −0.667 | 0.224 | −2.983 | 0.003 |
| Work experience (clustered) | 0.133 | 0.172 | 0.772 | 0.440 |
| Number of patients in care (clustered) | −0.293 | 0.129 | −2.261 | 0.024 |
| Gender | 0.198 | 0.293 | 0.499 | 0.499 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zuzic Furlan, S.; Rusic, D.; Bozic, J.; Rumboldt, M.; Rumboldt, Z.; Rada, M.; Tomicic, M. How Are We Managing Patients with Hyperuricemia and Gout: A Cross Sectional Study Assessing Knowledge and Attitudes of Primary Care Physicians? Int. J. Environ. Res. Public Health 2021, 18, 1234. https://doi.org/10.3390/ijerph18031234
Zuzic Furlan S, Rusic D, Bozic J, Rumboldt M, Rumboldt Z, Rada M, Tomicic M. How Are We Managing Patients with Hyperuricemia and Gout: A Cross Sectional Study Assessing Knowledge and Attitudes of Primary Care Physicians? International Journal of Environmental Research and Public Health. 2021; 18(3):1234. https://doi.org/10.3390/ijerph18031234
Chicago/Turabian StyleZuzic Furlan, Sanja, Doris Rusic, Josko Bozic, Mirjana Rumboldt, Zvonko Rumboldt, Marko Rada, and Marion Tomicic. 2021. "How Are We Managing Patients with Hyperuricemia and Gout: A Cross Sectional Study Assessing Knowledge and Attitudes of Primary Care Physicians?" International Journal of Environmental Research and Public Health 18, no. 3: 1234. https://doi.org/10.3390/ijerph18031234
APA StyleZuzic Furlan, S., Rusic, D., Bozic, J., Rumboldt, M., Rumboldt, Z., Rada, M., & Tomicic, M. (2021). How Are We Managing Patients with Hyperuricemia and Gout: A Cross Sectional Study Assessing Knowledge and Attitudes of Primary Care Physicians? International Journal of Environmental Research and Public Health, 18(3), 1234. https://doi.org/10.3390/ijerph18031234








