Preventing Childhood Obesity in Primary Schools: A Realist Review from UK Perspective
Abstract
:1. Background
2. Methods
2.1. Development of a Programme Theory
2.2. Inclusion/Exclusion Criteria
2.3. Data Extraction (Selection and Coding)
2.4. Rigour Assessment
- Highly rigorous data (++): Arguments/data for the context-mechanism-outcomes (CMOs) are appropriate (underpinned with theory and data), and study was at a low risk of bias for our outcome.
- Rigorous data (+): Arguments/data presented are appropriate for CMOs, and study is not at a low risk of bias for our outcome.
- Unclear rigour of data (?): No or weak arguments/data presented for CMOs, irrespective of whether study is at a low risk of bias for our outcome.
- Data not rigorous (−): Contrary or unreliable arguments/data presented, irrespective of whether study is at a low risk of bias for our outcome.
2.5. Data Synthesis
2.6. Analysis of Subgroups or Subsets
3. Results
3.1. Included Study Characteristics
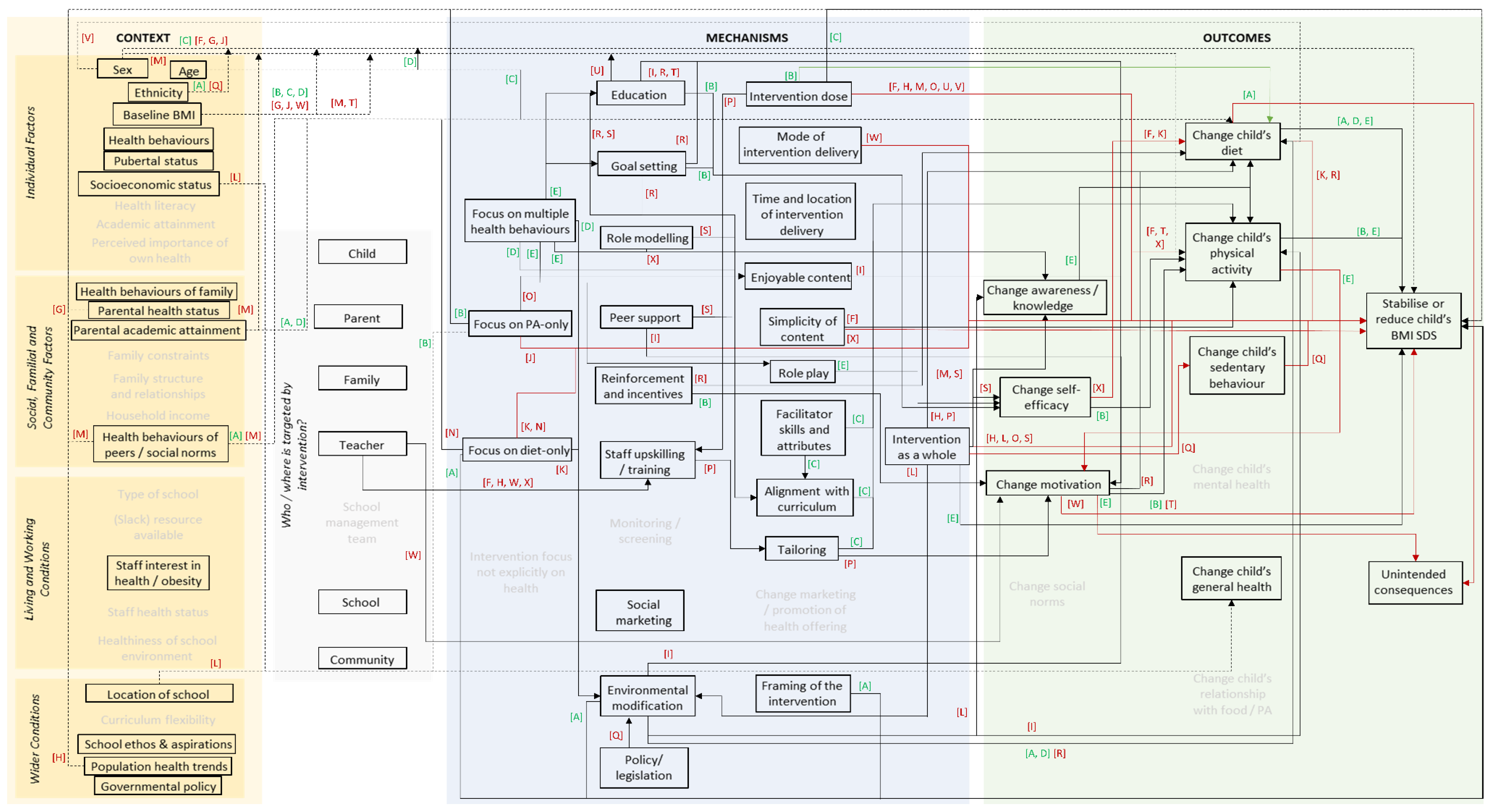
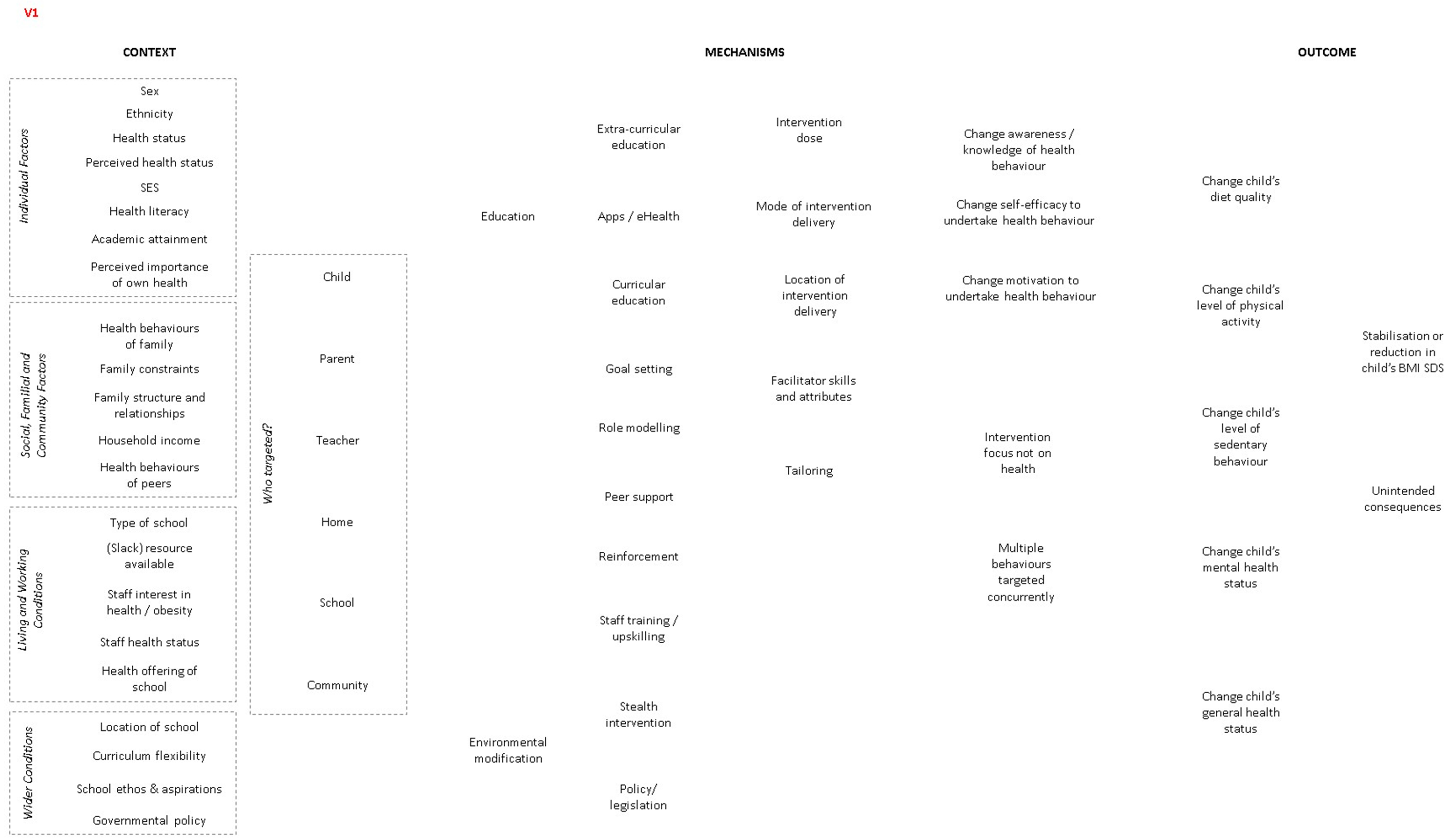
3.2. The Final Programme Theory
3.2.1. Contextual Factors
3.2.2. Mechanisms
3.3. Gaps in Evidence
3.4. Reporting of Costs
3.5. Reporting on Sustainability of Intervention
3.6. Findings of Sensitivity Analysis
4. Discussion
4.1. Comparison with Existing Literature
4.2. Strengths and Limitations of Our Realist Synthesis
4.3. Implications for UK-Based Primary Schools
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Conolly, A.; Byron, D. Health Survey for England 2017: Adult and Child Overweight and Obesity; National Centre for Social Research, NHS Digital: London, UK, 2018. [Google Scholar]
- Bagnall, A.-M.; Radley, D.; Jones, R.; Gately, P.; Nobles, J.; Van Dijk, M.; Blackshaw, J.; Montel, S.; Sahota, P. Whole systems approaches to obesity and other complex public health challenges: A systematic review. BMC Public Health 2019, 19, 1–14. [Google Scholar] [CrossRef]
- Finegood, D.T. The Complex Systems Science of Obesity. In The Oxford Handbook of the Social Science of Obesity; Cawley, J., Ed.; Oxford University Press, Inc.: New York, NY, USA, 2011. [Google Scholar]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Butland, B.; Jebb, S.; Kopelman, P.; McPherson, K.; Thomas, S.; Mardell, J.; Parry, V. Tackling Obesities: Future Choices—Project Report, 2nd ed.; Tackling Obesities: Future Choices, 164; Government Office for Science: London, UK, 2007.
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef]
- Bramante, C.T.; Thornton, R.L.; Bennett, W.L.; Zhang, A.; Wilson, R.F.; Bass, E.; Tseng, E. Systematic Review of Natural Experiments for Childhood Obesity Prevention and Control. Am. J. Prev. Med. 2019, 56, 147–158. [Google Scholar] [CrossRef]
- Waters, E.; De Silva-Sanigorski, A.; Burford, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, CD001871. [Google Scholar] [CrossRef]
- Rycroft-Malone, J.; McCormack, B.; Hutchinson, A.M.; DeCorby, K.; Bucknall, T.K.; Kent, B.; Schultz, A.; Snelgrove-Clarke, E.; Stetler, C.B.; Titler, M.; et al. Realist synthesis: Illustrating the method for implementation research. Implement. Sci. 2012, 7, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hnatiuk, J.A.; Brown, H.E.; Downing, K.L.; Hinkley, T.; Salmon, J.; Hesketh, K.D. Interventions to Increase Physical Activity in Children 0-5 Years Old: A Systematic Review, Meta-Analysis and Realist Synthesis. Obes. Rev. 2019, 20, 75–87. [Google Scholar] [CrossRef] [Green Version]
- Brown, H.E.; Atkin, A.J.; Panter, J.; Wong, G.; Chinapaw, M.J.; van Sluijs, E.M. Family-Based Interventions to Increase Physical Activity in Children: A Systematic Review, Meta-Analysis and Realist Synthesis. Obes. Rev. 2016, 17, 345–360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ijaz, S.; Nobles, J.; Johnson, L.; Moore, T.; Savović, J.; Jago, R. Preventing Childhood Obesity in the UK Primary Schools: A Realist Review. PROSPERO. 2019. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42019142192 (accessed on 14 December 2021).
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Pawson, R. Development of Methodological Guidance, Publication Standards and Training Materials for Realist and Meta-Narrative Reviews: The Rameses (Realist and Meta-Narrative Evidence Syntheses—Evolving Standards) Project. In Health Services and Delivery Research; NIHR Journals Library: Southampton, UK, 2014. [Google Scholar]
- Wong, G.; Greenhalgh, T.; Westhorp, G.; Buckingham, J.; Pawson, R. RAMESES publication standards: Realist syntheses. BMC Med. 2013, 11, 21. [Google Scholar] [CrossRef] [Green Version]
- Wong, G.; Westhorp, G.; Pawson, R.; Greenhalgh, T. Realist Synthesis: Rameses Training Materials. In RAMESES Project; Available online: https://www.ramesesproject.org/media/Realist_reviews_training_materials.pdf (accessed on 14 December 2021).
- Higgins, J.P.T.; Altman, D.G.; Sterne, J.A.C. Chapter 8: Assessing Risk of Bias in Included Studies. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011); Green, S., Ed.; The Cochrane Collaboration; Available online: www.handbook.cochrane.org. (accessed on 14 December 2021).
- Haire-Joshu, D.; Nanney, M.; Elliott, M.; Davey, C.; Caito, N.; Loman, D.; Brownson, R.C.; Kreuter, M.W. The Use of Mentoring Programs to Improve Energy Balance Behaviors in High-risk Children. Obesity 2010, 18, S75–S83. [Google Scholar] [CrossRef]
- Paineau, D.L.; Beaufils, F.; Boulier, A.; Cassuto, D.A.; Chwalow, J.; Combris, P.; Couet, C.; Jouret, B.; Lafay, L.; Laville, M.; et al. Family Dietary Coaching to Improve Nutritional Intakes and Body Weight Control: A Randomized Controlled Trial. Arch. Pediatr. Adolesc. Med. 2008, 162, 34–43. [Google Scholar] [CrossRef] [Green Version]
- Robinson, T.N.; Matheson, D.M.; Kraemer, H.C.; Wilson, D.M.; Obarzanek, E.; Thompson, N.S.; Alhassan, S.; Spencer, T.R.; Haydel, K.F.; Fujimoto, M.; et al. A Randomized Controlled Trial of Culturally Tailored Dance and Reducing Screen Time to Prevent Weight Gain in Low-Income African American Girls: Stanford Gems. Arch. Pediatr. Adolesc. Med. 2010, 164, 995–1004. [Google Scholar] [CrossRef] [Green Version]
- Amaro, S.; Viggiano, A.; Di Costanzo, A.; Madeo, I.; Viggiano, A.; Baccari, M.E.; Marchitelli, E.; Raia, M.; Viggiano, E.; Deepak, S.; et al. Kalèdo, a new educational board-game, gives nutritional rudiments and encourages healthy eating in children: A pilot cluster randomized trial. Eur. J. Nucl. Med. Mol. Imaging 2006, 165, 630–635. [Google Scholar] [CrossRef]
- Baranowski, T.; Adams, L.; Baranowski, J.; Canada, A.; Cullen, K.W.; Dobbins, M.H.; Jago, R.; Oceguera, A.; Rodriguez, A.X.; Speich, C. A School-Based Intervention for Diabetes Risk Reduction. N. Engl. J. Med. 2010, 363, 443–453. [Google Scholar]
- Cao, Z.-J.; Wang, S.-M.; Chen, Y. A Randomized Trial of Multiple Interventions for Childhood Obesity in China. Am. J. Prev. Med. 2015, 48, 552–560. [Google Scholar] [CrossRef] [Green Version]
- Damsgaard, C.T.; Dalskov, S.M.; Laursen, R.P.; Ritz, C.; Hjorth, M.F.; Lauritzen, L.; Sorensen, L.B.; Petersen, R.A.; Andersen, M.R.; Stender, S.; et al. Provision of Healthy School Meals Does Not Affect the Metabolic Syndrome Score in 8-11-Year-Old Children, but Reduces Cardiometabolic Risk Markers Despite Increasing Waist Circumference. Br. J. Nutr. 2014, 112, 1826–1836. [Google Scholar] [CrossRef] [Green Version]
- de Ruyter, J.C.; Olthof, M.R.; Kuijper, L.D.; Katan, M.B. Effect of Sugar-Sweetened Beverages on Body Weight in Children: Design and Baseline Characteristics of the Double-Blind, Randomized Intervention Study in Kids. Contemp. Clin. Trials 2012, 33, 247–257. [Google Scholar] [CrossRef]
- Fairclough, S.J.; Hackett, A.F.; Davies, I.G.; Gobbi, R.; Mackintosh, A.K.; Warburton, G.L.; Stratton, G.; Van Sluijs, E.M.; Boddy, L.M. Promoting healthy weight in primary school children through physical activity and nutrition education: A pragmatic evaluation of the CHANGE! randomised intervention study. BMC Public Health 2013, 13, 626. [Google Scholar] [CrossRef] [Green Version]
- Foster, G.D.; Sherman, S.; Borradaile, K.E.; Grundy, K.M.; Vander Veur, S.S.; Nachmani, J.; Karpyn, A.; Kumanyika, S.; Shults, J.; Healy, C.M.; et al. A Policy-Based School Intervention to Prevent Overweight and Obesity. Pediatrics 2008, 121, e794–e802. [Google Scholar] [CrossRef] [Green Version]
- Grydeland, M.; Bergh, I.H.; Bjelland, M.; Lien, N.; Andersen, L.F.; Ommundsen, Y.; Klepp, K.-I.; Anderssen, S.A. Intervention effects on physical activity: The HEIA study—a cluster randomized controlled trial. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 17. [Google Scholar] [CrossRef] [Green Version]
- Gutin, B.; Yin, Z.; Johnson, M.; Barbeau, P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: The Medical College of Georgia Fitkid Project. Pediatr. Obes. 2008, 3, 3–9. [Google Scholar] [CrossRef]
- Herscovici, C.R.; Kovalskys, I.; De Gregorio, M.J. Gender differences and a school-based obesity prevention program in Argentina: A randomized trial. Rev. Panam. Salud Publica 2013, 34. [Google Scholar]
- James, J.; Thomas, P.; Cavan, D.; Kerr, D. Preventing Childhood Obesity by Reducing Consumption of Carbonated Drinks: Cluster Randomised Controlled Trial. BMJ 2004, 328, 1237. [Google Scholar] [CrossRef] [Green Version]
- Johnston, C.A.; Moreno, J.P.; El-Mubasher, A.; Gallagher, M.; Tyler, C.; Woehler, D. Impact of a School-Based Pediatric Obesity Prevention Program Facilitated by Health Professionals. J. Sch. Health 2013, 83, 171–181. [Google Scholar] [CrossRef]
- Khan, N.A.; Raine, L.B.; Drollette, E.S.; Scudder, M.R.; Pontifex, M.B.; Castelli, D.M.; Donovan, S.M.; Evans, E.M.; Hillman, C.H. Impact of the FITKids Physical Activity Intervention on Adiposity in Prepubertal Children. Pediatrics 2014, 133, e875–e883. [Google Scholar] [CrossRef] [Green Version]
- Kipping, R.R.; Howe, L.; Jago, R.; Campbell, R.; Wells, S.; Chittleborough, C.; Mytton, J.; Noble, S.M.; Peters, T.; Lawlor, D.A. Effect of intervention aimed at increasing physical activity, reducing sedentary behaviour, and increasing fruit and vegetable consumption in children: Active for Life Year 5 (AFLY5) school based cluster randomised controlled trial. BMJ 2014, 348, g3256. [Google Scholar] [CrossRef] [Green Version]
- Lazaar, N.; Aucouturier, J.; Ratel, S.; Rance, M.; Meyer, M.; Duché, P. Effect of physical activity intervention on body composition in young children: Influence of body mass index status and gender. Acta Paediatr. 2007, 96, 1321–1325. [Google Scholar] [CrossRef]
- Li, Y.-P.; Hu, X.-Q.; Schouten, E.G.; Liu, A.-L.; DU, S.-M.; Li, L.-Z.; Cui, Z.-H.; Wang, D.; Kok, F.J.; Hu, F.B.; et al. Report on Childhood Obesity in China (8): Effects and Sustainability of Physical Activity Intervention on Body Composition of Chinese Youth. Biomed. Environ. Sci. 2010, 23, 180–187. [Google Scholar] [CrossRef]
- Marcus, C.; Nyberg, G.; Nordenfelt, A.; Karpmyr, M.; Kowalski, J.; Ekelund, U. A 4-year, cluster-randomized, controlled childhood obesity prevention study: STOPP. Int. J. Obes. 2009, 33, 408–417. [Google Scholar] [CrossRef] [Green Version]
- Meng, L.; Xu, H.; Liu, A.; Van Raaij, J.; Bemelmans, W.; Hu, X.; Zhang, Q.; Du, S.; Fang, H.; Ma, J.; et al. The Costs and Cost-Effectiveness of a School-Based Comprehensive Intervention Study on Childhood Obesity in China. PLoS ONE 2013, 8, e77971. [Google Scholar] [CrossRef] [Green Version]
- Muckelbauer, R.; Libuda, L.; Clausen, K.; Toschke, A.M.; Reinehr, T.; Kersting, M. Immigrational Background Affects the Effectiveness of a School-based Overweight Prevention Program Promoting Water Consumption. Obesity 2010, 18, 528–534. [Google Scholar] [CrossRef]
- Rosário, R.; Oliveira, B.; Araújo, A.; Lopes, O.; Padrão, P.; Moreira, A.; Teixeira, V.; Barros, R.; Pereira, B.; Moreira, P. The Impact of an Intervention Taught by Trained Teachers on Childhood Overweight. Int. J. Environ. Res. Public Health 2012, 9, 1355–1367. [Google Scholar] [CrossRef] [Green Version]
- Rush, E.; Reed, P.; McLennan, S.; Coppinger, T.; Simmons, D.; Graham, D. A School-Based Obesity Control Programme: Project Energize. Two-Year Outcomes. Br. J. Nutr. 2012, 107, 581–587. [Google Scholar] [CrossRef] [Green Version]
- Sahota, P.; Rudolf, M.C.J.; Dixey, R.; Hill, A.J.; Barth, J.H.; Cade, J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ 2001, 323, 1029. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.G.; Durksen, A.; Rabbanni, R.; Chanoine, J.P.; Lamboo Miln, A.; Mayer, T.; McGavock, J.M. Effectiveness of Peer-Based Healthy Living Lesson Plans on Anthropometric Measures and Physical Activity in Elementary School Students: A Cluster Randomized Trial. JAMA Pediatr. 2014, 168, 330–337. [Google Scholar] [CrossRef]
- Siegrist, M.; Lammel, C.; Haller, B.; Christle, J.; Halle, M. Effects of a Physical Education Program on Physical Activity, Fitness, and Health in Children: The Juventum Project. Scand. J. Med. Sci. Sports 2013, 23, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, S.A.; Foulk, D. Reducing Overweight through a Multidisciplinary School-based Intervention. Obesity 2006, 14, 88–96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williamson, D.A.; Champagne, C.M.; Harsha, D.W.; Han, H.; Martin, C.K.; Newton, R.; Sothern, M.S.; Stewart, T.M.; Webber, L.S.; Ryan, D.H.; et al. Effect of an Environmental School-Based Obesity Prevention Program on Changes in Body Fat and Body Weight: A Randomized Trial. Obesity 2012, 20, 1653–1661. [Google Scholar] [CrossRef] [Green Version]
- Breheny, K.; Passmore, S.; Adab, P.; Martin, J.; Hemming, K.; Lancashire, E.R.; Frew, E. Effectiveness and cost-effectiveness of The Daily Mile on childhood weight outcomes and wellbeing: A cluster randomised controlled trial. Int. J. Obes. 2020, 44, 812–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGill, R.; Anwar, E.; Orton, L.; Bromley, H.; Lloyd-Williams, F.; O’Flaherty, M.; Taylor-Robinson, D.; Guzman-Castillo, M.; Gillespie, D.; Moreira, P.; et al. Are interventions to promote healthy eating equally effective for all? Systematic review of socioeconomic inequalities in impact. BMC Public Health 2015, 15, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Flodgren, G.M.; Helleve, A.; Lobstein, T.; Rutter, H.; Klepp, K. Primary prevention of overweight and obesity in adolescents: An overview of systematic reviews. Obes. Rev. 2020, 21. [Google Scholar] [CrossRef]
- Carozza, S.E.; Puumala, S.E.; Chow, E.; Fox, E.E.; Horel, S.; Johnson, K.J.; McLaughlin, C.C.; Reynolds, P.; Von Behren, J.; Mueller, B.A.; et al. Parental educational attainment as an indicator of socioeconomic status and risk of childhood cancers. Br. J. Cancer 2010, 103, 136–142. [Google Scholar] [CrossRef]
- Fernández-Alvira, J.M.; Mouratidou, T.; Bammann, K.; Hebestreit, A.; Barba, G.; Sieri, S.; Reisch, L.; Eiben, G.; Hadjigeorgiou, C.; Kovacs, E.; et al. Parental education and frequency of food consumption in European children: The IDEFICS study. Public Health Nutr. 2012, 16, 487–498. [Google Scholar] [CrossRef] [Green Version]
- Heerman, W.J.; Jaka, M.M.; Berge, J.M.; Trapl, E.S.; Sommer, E.C.; Samuels, L.R.; Jackson, N.; Haapala, J.L.; Kunin-Batson, A.S.; Olson-Bullis, B.A.; et al. The dose of behavioral interventions to prevent and treat childhood obesity: A systematic review and meta-regression. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 157. [Google Scholar] [CrossRef] [Green Version]
- Driessen, C.E.; Cameron, A.J.; Thornton, L.; Lai, S.; Barnett, L. Effect of changes to the school food environment on eating behaviours and/or body weight in children: A systematic review. Obes. Rev. 2014, 15, 968–982. [Google Scholar] [CrossRef]
- Cooper, A.M.; O’Malley, L.; Elison, S.N.; Armstrong, R.; Burnside, G.; Adair, P.; Dugdill, L.; Pine, C. Primary school-based behavioural interventions for preventing caries. Cochrane Database Syst. Rev. 2013, CD009378. [Google Scholar] [CrossRef]
- Mason-Jones, A.J.; Sinclair, D.; Mathews, C.; Kagee, A.; Hillman, A.; Lombard, C. School-Based Interventions for Preventing Hiv, Sexually Transmitted Infections, and Pregnancy in Adolescents. Cochrane Database Syst. Rev. 2016, 11, CD006417. [Google Scholar] [CrossRef] [Green Version]
- Ebrahim, S.; Taylor, F.; Ward, K.; Beswick, A.; Burke, M.; Smith, G.D. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst. Rev. 2011, 19, CD001561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, J.; Mytton, O.; White, M.; Monsivais, P. Why Are Some Population Interventions for Diet and Obesity More Equitable and Effective Than Others? The Role of Individual Agency. PLOS Med. 2016, 13, e1001990. [Google Scholar]
- Psaltopoulou, T.; Tzanninis, S.; Ntanasis-Stathopoulos, I.; Panotopoulos, G.; Kostopoulou, M.; Tzanninis, I.-G.; Tsagianni, A.; Sergentanis, T.N. Prevention and treatment of childhood and adolescent obesity: A systematic review of meta-analyses. World J. Pediatr. 2019, 15, 350–381. [Google Scholar] [CrossRef] [PubMed]
- Nobles, J.; Summerbell, C.; Brown, T.; Jago, R.; Moore, T. A Secondary Analysis of the Childhood Obesity Prevention Literature through a Wider Determinants of Health Lens. Int. J. Behav. Nutr. Phys. Act. 2021, 22, 18. [Google Scholar] [CrossRef]
- Oliver, S.; Bagnall, A.; Thomas, J.; Shepherd, J.; Sowden, A.; White, I.; Dinnes, J.; Rees, R.; Colquitt, J.L.; Oliver, K.; et al. Randomised controlled trials for policy interventions: A review of reviews and meta-regression. Health Technol. Assess. 2010, 14. [Google Scholar] [CrossRef] [Green Version]
- Crane, M.; Bohn-Goldbaum, E.; Grunseit, A.; Bauman, A. Using natural experiments to improve public health evidence: A review of context and utility for obesity prevention. Health Res. Policy Syst. 2020, 18, 1–13. [Google Scholar] [CrossRef]
- Karacabeyli, D.; Allender, S.; Pinkney, S.; Amed, S. Evaluation of complex community-based childhood obesity prevention interventions. Obes. Rev. 2018, 19, 1080–1092. [Google Scholar] [CrossRef] [PubMed]
- Flynn, M.A.T.; McNeil, D.A.; Maloff, B.; Mutasingwa, D.; Wu, M.; Ford, C.; Tough, S.C. Reducing obesity and related chronic disease risk in children and youth: A synthesis of evidence with ‘best practice’ recommendations. Obes. Rev. 2006, 7, 7–66. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.; Ananthapavan, J.; Sonntag, D.; Tan, E.J.; Hayes, A.; Moodie, M. The potential for long-term cost-effectiveness of obesity prevention interventions in the early years of life. Pediatr. Obes. 2019, 14, e12517. [Google Scholar] [CrossRef] [PubMed]
| Study and Location | Intervention Content and Delivery | Contexts Identified | Mechanisms Identified | CMO Configurations | Rigour |
|---|---|---|---|---|---|
| Effective studies | |||||
| de Ruyter, 2012 [24] The Netherlands | Description: Double blind RCT, replacing sugary drinks (regularly consumed in school breaks and at home) with identical tasting sugar free drinks. Provider: Third party (researchers) Timing: N/A–drinks available at home and school; 18 months duration. Target group: Children; parents; teachers; school. |
|
|
| ++ |
| Khan 2014 [32] USA | Description: Two hours of daily PA, five days/week for nine months; 15 min of education and healthy snack. Provider: Third party (undergrads, researchers). Timing: After school hours; nine months duration. Target group: Children. |
|
|
| ++ |
| Li, 2010 [35] China | Description: Two daily 10 min MVPA sessions conducted in the break between classes with variety of safe, moderate, age- and space-appropriate activities. Provider: Teacher. Timing: During school hours; 12 months duration. Target group: Children. |
|
|
| + |
| Marcus, 2009 [36] Sweden | Description: 30 min of daily PA was integrated into the curriculum. School lunch and afternoon snack were made healthier by adding fruit and vegetables. Awareness raising intervention provided for staff and parents. Provider: Teacher. Timing: During school hours; 48 months duration. Target group: Children, parents school staff. |
|
|
| + |
| Spiegel 2006, [44] USA | Description: Seven modules of educational content for children. Modules on (1) general wellness, (2) reflective self-analysis, (3) principles of PA, (4) principles of diet and nutrition, (5) learning about the body, (6) genetics and family health and (7) practical application of acquired knowledge. Ten mins of PA each day during class time. Provider: Teacher. Timing: During school hours; nine months duration Target group: Children, family, teacher. | None identified |
|
| ? |
| Ineffective studies | |||||
| Fairclough, 2013 [25] UK | Description: One hour of content per week over 20 weeks. Intervention provided teachers with lesson plans, worksheets, homework tasks, lesson resources and a CD-ROM. Topics covered PA and diet, and aligned with the UK Healthy Schools programme. Developed with parents, children and teachers input. Provider: Teacher. Timing: During and after school hours; five months duration Target group: Children, family, teacher. |
|
|
| ? |
| Cao, 2015 [22] China | Description: Six hours of health educational content per semester. Intervention also includes regular newspapers, brochures, seminars, and morning meetings. Offer one hour of PA per school day. Lower fat content and more fruits and vegetables available at canteens. Provider: Teacher, parent. Timing: During and after school hours; 34 months duration Target group: Children, parent, teacher |
|
|
| ? |
| Sahota, 2001 [41] UK | Description: Teacher training, modifications of school meals and the development and implementation of school action plans designed to promote healthy eating and PA over one academic year. Developed with parent, teacher, and child input. Provider: Teacher, school. Timing: During school hours; nine months. Target group: Children, teacher, school. |
|
|
| ? |
| Gutin, 2008 [28] USA | Description: 40-min session of academic enrichment activities, followed by 80 min MVPA. Offered each day after school. Healthy snacks provided during break. Provider: Teacher. Timing: After school hours; 36 months duration. Target group: Children, teacher. |
|
|
| + |
| Lazaar, 2007 [34] France | Description: Two sessions of school PE per week (one hour per session). The which intensity and duration off sessions increased throughout the study with the aim that the 45 min of exercise in one hour is playful. Provider: Third party (state PE undergrads). Timing: During school hours; six months duration. Target group: Children. |
|
|
| ? |
| Damsgaard, 2014 [23] Denmark | Description: School lunch and snacks based on the New Nordic Diet, designed to cover 40–45% of the children’s daily energy intake (mid-morning snack, ad-libitum hot lunch, afternoon snack, fresh fruit or fruit-based dessert). Seasonal menus developed. Children participated in the cooking. Provider: Kitchen staff, school. Timing: Three months duration. Target group: Children, school. |
|
|
| + |
| Rush, 2012 [40] New Zealand | Description: Project staff allocated to schools to model classes around various physical activities. Study also promoted active transport, lunchtime games, bike days and training for students to be leaders of PA. Project staff assisted school with healthy eating initiatives (e.g., canteen makeovers). Nutritional information included in weekly school newsletter. Parents asked to attend three information sessions and a 45-min practical nutrition class. Project staff helped teachers, parents and the local community via a range of activities (open days, edible gardens). Provider: Third party (project staff), teacher. Timing: During school hours; 24 months duration. Target group: Children, parent, teacher, school, community. |
|
|
| ? |
| Grydeland, 2014 [27] Norway | Description: Classroom-based dietary education using personally tailored computer software. Intervention also offered fruit/vegetable and PA breaks during day. Inspirational PA courses for teachers, and fact sheets to parents. Environmental component included active transport campaigns, PA equipment and suggestions for playground improvements. Provider: Teacher. Timing: During and after school hours; 20 months duration. Target group: Children, teacher, parent. |
|
|
| ? |
| James, 2004 [30] UK | Description: Four educational components delivered to children by project staff: (1) a one-hour session delivered once per term on the balance of good health and promotion of drinking water, (2,3) one off sessions to create a rap/song about healthy diet and (4) a presentation and quiz. Provider: Third party (project staff), teacher. Timing: During school hours; 12 months duration. Target group: Children. | None identified |
|
| + |
| Meng, 2013 [37] China | Description: Classroom-based 10-min MVPA led by teachers. Sessions on nutrition and health six times for students (monthly), twice for parents and four times for teachers and health workers. Provider: Teacher Timing: During school hours; six months duration. Target group: Children, parent teacher. |
|
|
| ? |
| Rosario, 2012 [39] Portugal | Description: 12 nutritional education sessions of three hours each duration for children plus six month of teacher training. Provider: Teacher. Timing: During school hours; six months duration. Target group: Children, teacher. |
|
|
| - |
| Foster, 2008 [26] USA | Description: The School Nutrition Policy Initiative included: school self-assessment; nutritional education for parent, child and teacher; nutrition policy; social marketing campaign targeted at children; and parent outreach work via nutrition educators. Provider: Teacher, third party (nutrition educators). Timing: During and after school hours; 24 months duration. Target group: Children, parent, teacher, school. |
|
|
| - |
| Muckelbauer, 2010 [38] Germany | Description: Combined environmental and educational intervention promoting water consumption: water fountains installed in schools, provision of reusable water bottles and lessons importance of water consumption Provider: Teacher, school. Timing: During school hours; 12 months duration. Target group: Children, teacher, school. |
|
|
| - |
| Santos, 2014 [42] Canada | Description: Older students received a weekly 45-min healthy living lesson from teachers (given training for two days). Older students acted as peer mentors, teaching a 30-min lesson to younger “buddies.” Two 30-min structured aerobic fitness sessions per week with student pairs. Provider: Teacher, child. Timing: During school hours; 10 months duration. Target group: Children. |
|
|
| ++ |
| Siegrist, 2013 [43] Germany | Description: 45 min per month of additional PE during school hours. Re-arrangement of the classrooms, halls and playgrounds to promote more PA. Worksheets, assignments and newsletters sent home to support PA. Measures to improve the quality of food sold at school snack bars. Parents provided with three hours of training, and teachers given nine hours. Provider: Teacher. Timing: During and after school hours; 12 months duration. Target group: Children, parents, teachers. |
|
|
| - |
| Williamson, 2012 [45] USA | Description: Environmental modification of school setting: (1) cues related to healthy eating and activity, (2) cafeteria food service and (3) PE programs. Behavioural modification: (1) educational program delivered as a part of class work, with synchronous on-line counselling and asynchronous email communications for children and parents. Teachers trained prior to, and throughout, the trial duration. Provider: Teacher. Timing: During school hours; 28 months duration Target group: Children |
|
|
| ? |
| Herscovici, 2013 [29] Argentina | Description: Four workshops (40 min each, once a month) on diet and PA (three for children and one for parents). Modifications made to school cafeteria menu. Provider: Third party (interdisciplinary team). Timing: During school hours; six months duration. Target group: Children, parents. |
|
|
| ? |
| Johnston, 2013 [31] USA | Description: Trained health professionals visited school three times per week to meet staff and provide suggestions for how to improve health messages across school. They trained and assisted teachers (60 h training and 40 h of supervised practice) to implement healthy messages in curriculum. They also helped to improve availability of nutrient-rich food at school cafeteria. Provider: Third party (trained health professionals), teacher. Timing: During school hours; 24 months duration. Target group: Children, parents, teachers, school. |
|
|
| + |
| Kipping, 2014 [33] UK | Description: Training for teachers and teaching assistants provided by the study team. Teachers provided with 16 lesson-plans and teaching materials. Schools also provided with information that they could use in newsletters about the importance of PA, sedentary behaviour and diet. Parents provided with 10 parent–child interaction homework activities, and information on how to encourage their child’s health behaviours. Provider: Teacher, third party (multidisciplinary). Timing: During and after school hours; eight months duration. Target group: Children, parent, teacher, school. |
|
|
| ++ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ijaz, S.; Nobles, J.; Johnson, L.; Moore, T.; Savović, J.; Jago, R. Preventing Childhood Obesity in Primary Schools: A Realist Review from UK Perspective. Int. J. Environ. Res. Public Health 2021, 18, 13395. https://doi.org/10.3390/ijerph182413395
Ijaz S, Nobles J, Johnson L, Moore T, Savović J, Jago R. Preventing Childhood Obesity in Primary Schools: A Realist Review from UK Perspective. International Journal of Environmental Research and Public Health. 2021; 18(24):13395. https://doi.org/10.3390/ijerph182413395
Chicago/Turabian StyleIjaz, Sharea, James Nobles, Laura Johnson, Theresa Moore, Jelena Savović, and Russell Jago. 2021. "Preventing Childhood Obesity in Primary Schools: A Realist Review from UK Perspective" International Journal of Environmental Research and Public Health 18, no. 24: 13395. https://doi.org/10.3390/ijerph182413395
APA StyleIjaz, S., Nobles, J., Johnson, L., Moore, T., Savović, J., & Jago, R. (2021). Preventing Childhood Obesity in Primary Schools: A Realist Review from UK Perspective. International Journal of Environmental Research and Public Health, 18(24), 13395. https://doi.org/10.3390/ijerph182413395






