The Effects of E-Cigarette Use on Alcohol and Marijuana Abuse Symptoms in an Ethnically Diverse Sample of Young Adults
Abstract
:1. Introduction
2. Materials and Methods
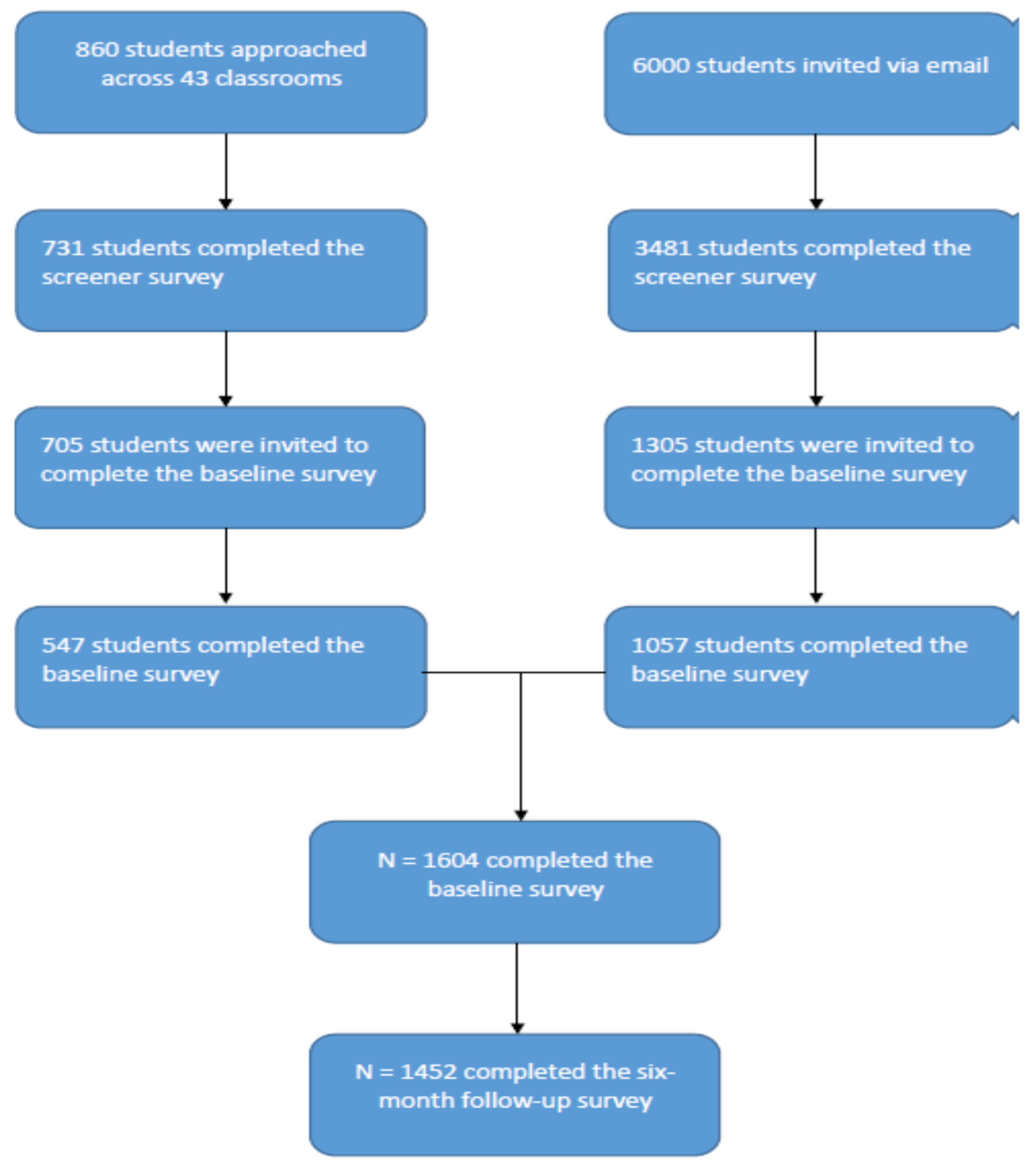
2.1. Procedures
2.2. Measures
2.2.1. Demographics
2.2.2. Sensation Seeking
2.2.3. Current Cigarette, E-Cigarette, and Marijuana Use
2.2.4. Alcohol Abuse Symptoms
2.2.5. Marijuana Abuse Symptoms
2.3. Data Analysis
3. Results
3.1. Participants
3.2. Associations of Baseline E-Cigarette Use with Future Problem Alcohol and Marijuana Use
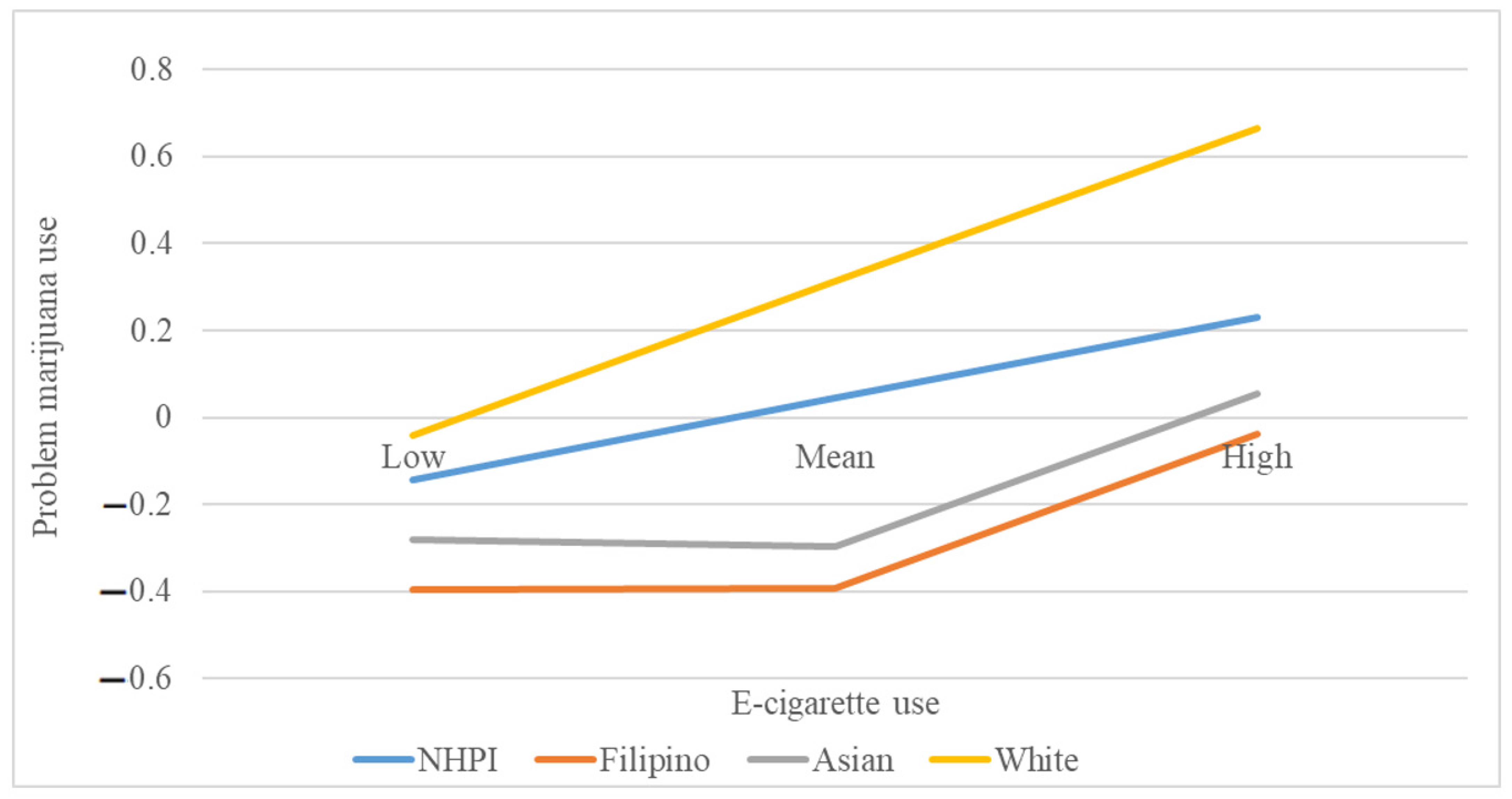
3.3. Moderation by Ethnicity
4. Discussion
5. Conclusions
6. Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gentzke, A.S.; Creamer, M.; Cullen, K.A.; Ambrose, B.K.; Willis, G.; Jamal, A.; King, B.A. Vital Signs: Tobacco Product Use Among Middle and High School Students—United States, 2011–2018. MMWR Morb. Mortal. Wkly. Rep. 2019, 68, 157–164. [Google Scholar] [CrossRef] [Green Version]
- Gentzke, A.S.; Wang, T.W.; Jamal, A.; Park-Lee, E.; Ren, C.; Cullen, K.A.; Neff, L. Tobacco Product Use Among Middle and High School Students—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1881–1888. [Google Scholar] [CrossRef]
- Cornelius, M.E.; Wang, T.W.; Jamal, A.; Loretan, C.G.; Neff, L.J. Tobacco Product Use among Adults—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1736–1742. [Google Scholar] [CrossRef]
- Wills, T.A.; Soneji, S.S.; Choi, K.; Jaspers, I.; Tam, E.K. E-cigarette use and respiratory disorders: An integrative review of converging evidence from epidemiological and laboratory studies. Eur. Respir. J. 2021, 57, 1901815. [Google Scholar] [CrossRef]
- Audrain-McGovern, J.; Stone, M.D.; Barrington-Trimis, J.; Unger, J.B.; Leventhal, A.M. Adolescent E-Cigarette, Hookah, and Conventional Cigarette Use and Subsequent Marijuana Use. Pediatrics 2018, 142, e20173616. [Google Scholar] [CrossRef] [Green Version]
- Bluestein, M.; Kelder, S.; Perry, C.L.; Pérez, A. Exploring associations between the use of alcohol and marijuana with e-cigarette use in a U.S.A. nationally representative sample of young adults. Int. J. Health Sci. 2019, 13, 30–39. [Google Scholar]
- Boccio, C.M.; Jackson, D.B. Adolescent nicotine and marijuana vaping activity and the use of other illicit substances. Drug Alcohol Depend. 2021, 219, 108469. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, A.H.; Platt, J.; Zhu, J.; Levin, J.; Ganz, O.; Goodwin, R.D. Cigarette Use and Cannabis Use Disorder Onset, Persistence, and Relapse: Longitudinal Data from a Representative Sample of US Adults. J. Clin. Psychiatry 2021, 82, 20m13713. [Google Scholar] [CrossRef] [PubMed]
- Dierker, L.; Braymiller, J.; Rose, J.; Goodwin, R.; Selya, A. Nicotine dependence predicts cannabis use disorder symptoms among adolescents and young adults. Drug Alcohol Depend. 2018, 187, 212–220. [Google Scholar] [CrossRef]
- McKee, S.A.; Falba, T.; O’Malley, S.S.; Sindelar, J.; O’Connor, P.G. Smoking status as a clinical indicator for alcohol misuse in US adults. Arch. Intern. Med. 2007, 167, 716–721. [Google Scholar] [CrossRef]
- Rose, J.E.; Brauer, L.H.; Behm, F.M.; Cramblett, M.; Calkins, K.; Lawhon, D. Psychopharmacological interactions between nicotine and ethanol. Nicotine Tob. Res. 2004, 6, 133–144. [Google Scholar] [CrossRef]
- Kalman, D.; Morissette, S.B.; George, T.P. Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am. J. Addict. 2005, 14, 106–123. [Google Scholar] [CrossRef]
- Weinberger, A.H.; Sofuoglu, M. The impact of cigarette smoking on stimulant addiction. Am. J. Drug Alcohol Abuse. 2009, 35, 12–17. [Google Scholar] [CrossRef]
- Hartmann-Boyce, J.; McRobbie, H.; Lindson, N.; Bullen, C.; Begh, R.; Theodoulou, A.; Notley, C.; Rigotti, N.A.; Turner, T.; Fanshawe, T.R.; et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 2020, 10, Cd010216. [Google Scholar] [CrossRef]
- Collins, L.; Glasser, A.M.; Abudayyeh, H.; Pearson, J.L.; Villanti, A.C. E-Cigarette Marketing and Communication: How E-Cigarette Companies Market E-Cigarettes and the Public Engages with E-cigarette Information. Nicotine Tob. Res. 2019, 21, 14–24. [Google Scholar] [CrossRef]
- Roberts, W.; Moore, K.E.; Peltier, M.R.; Verplaetse, T.L.; Oberleitner, L.; Hacker, R.; McKee, S.A. Electronic Cigarette Use and Risk of Harmful Alcohol Consumption in the U.S. Population. Alcohol Clin. Exp. Res. 2018, 42, 2385–2393. [Google Scholar] [CrossRef]
- Grant, J.E.; Lust, K.; Fridberg, D.J.; King, A.C.; Chamberlain, S.R. E-cigarette use (vaping) is associated with illicit drug use, mental health problems, and impulsivity in university students. Ann. Clin. Psychiatr. 2019, 31, 27–35. [Google Scholar]
- Temple, J.R.; Shorey, R.C.; Lu, Y.; Torres, E.; Stuart, G.L.; Le, V.D. E-cigarette use of young adults motivations and associations with combustible cigarette alcohol, marijuana, and other illicit drugs. Am. J. Addict. 2017, 26, 343–348. [Google Scholar] [CrossRef]
- Baldassarri, S.R.; Camenga, D.R.; Fiellin, D.A.; Friedman, A.S. Marijuana Vaping in U.S. Adults: Evidence from the Behavioral Risk Factor Surveillance System. Am. J. Prev. Med. 2020, 59, 449–454. [Google Scholar] [CrossRef]
- Harrell, M.B.; Chen, B.; Clendennen, S.L.; Sumbe, A.; Case, K.R.; Wilkinson, A.V.; Perry, C.L. Longitudinal trajectories of E-cigarette use among adolescents: A 5-year, multiple cohort study of vaping with and without marijuana. Prev. Med. 2021, 150, 106670. [Google Scholar] [CrossRef]
- Pokhrel, P.; Fagan, P.; Kawamoto, C.T.; Okamoto, S.K.; Herzog, T.A. Predictors of marijuana vaping onset and escalation among young adults. Drug Alcohol Depend. 2020, 216, 108320. [Google Scholar] [CrossRef] [PubMed]
- Kaholokula, J.K.; Saito, E.; Shikuma, C.; Look, M.; Spencer-Tolentino, K.; Mau, M.K. Native and Pacific health disparities research. Hawaii Med. J. 2008, 67, 218–219, 222. [Google Scholar]
- Andrade, N.N.; Bell, C.K. The Hawaiians. In People and Cultures of Hawaii; McDermott, J.F., Jr., Andrade, N.N., Eds.; University of Hawaii Press: Honolulu, HI, USA, 2011. [Google Scholar]
- Kaholokula, J.K.; Grandinetti, A.; Keller, S.; Nacapoy, A.H.; Kingi, T.K.; Mau, M.K. Association between perceived racism and physiological stress indices in Native Hawaiians. J. Behav. Med. 2012, 35, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Kaholokula, J.K.; Iwane, M.K.; Nacapoy, A.H. Effects of perceived racism and acculturation on hypertension in Native Hawaiians. Hawaii Med. J. 2010, 69 (Suppl. S2), 11–15. [Google Scholar]
- Hixson, L.K.; Hepler, B.B.; Kim, M.O. The Native Hawaiian and Other Pacific Islander Population: 2010; United States Census Bureau, U.S. Department of Commerce: Washington, DC, USA, 2010.
- Look, M.; Trask-Batti, M.; Agres, R.; Mau, M.; Kaholokula, J. Assessment and Priorities for Health & Well-Being in Native Hawaiians & Other Pacific Peoples; Center for Native and Pacific Health Disparities Research, University of Hawaii: Honolulu, HI, USA, 2013. [Google Scholar]
- Hawaii State Department of Health. HAWAII Behavioral Risk Factor Surveillance System (BRFSS). 2018. Available online: http://hhdw.org/health-reports-data/data-source/brfss-reports/ (accessed on 25 July 2020).
- Guerrero, A.P.S.; Bayola, R.; Ona, C. The Filipinos. In People and Cultures of Hawaii; McDermott, J.F., Jr., Andrade, N.N., Eds.; The University of Hawaii Press: Honolulu, HI, USA, 2011; pp. 201–219. [Google Scholar]
- Pokhrel, P.; Little, M.A.; Herzog, T.A. Current Methods in Health Behavior Research Among, U.S. Community College Students: A Review of the Literature. Eval. Health Prof. 2014, 37, 178–202. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoyle, R.H.; Stephenson, M.T.; Palmgreen, P.; Lorch, E.P.; Donohew, R.L. Reliability and validity of a brief measure of sensation seeking. Personal. Individ. Differ. 2002, 32, 401–414. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; de la Fuente, J.R.; Grant, M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction 1993, 88, 791–804. [Google Scholar] [CrossRef]
- Legleye, S. The Cannabis Abuse Screening Test and the DSM-5 in the general population: Optimal thresholds and underlying common structure using multiple factor analysis. Int. J. Methods Psychiatr. Res. 2018, 27, e1597. [Google Scholar] [CrossRef] [Green Version]
- Legleye, S.; Piontek, D.; Kraus, L.; Morand, E.; Falissard, B. A validation of the Cannabis Abuse Screening Test (CAST) using a latent class analysis of the DSM-IV among adolescents. Int. J. Methods Psychiatr. Res. 2013, 22, 16–26. [Google Scholar] [CrossRef]
- Legleye, S.; Guignard, R.; Richard, J.B.; Ludwig, K.; Pabst, A.; Beck, F. Properties of the Cannabis Abuse Screening Test (CAST) in the general population. Int. J. Methods Psychiatr. Res. 2015, 24, 170–183. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G. Multiple Regression: Testing and Interpreting Interactions; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1991. [Google Scholar]
- Schulenberg, J.E.; Patrick, M.E.; Johnston, L.D.; O’Malley, P.M.; Bachman, J.G.; Miech, R.A. Monitoring the Future National Survey Results on Drug Use, 1975–2020: Volume II, College Students and Adults Ages 19–60; Institute for Social Research, The University of Michigan: Ann Arbor, MI, USA, 2021. [Google Scholar]
- Haass-Koffler, C.L.; Bartlett, S.E. Stress and addiction: Contribution of the corticotropin releasing factor (CRF) system in neuroplasticity. Front Mol. Neurosci. 2012, 5, 91. [Google Scholar] [CrossRef] [Green Version]
| All (N = 1463) | NHPI (n = 290) | Filipino (n = 423) | Asian (n = 382) | White (n = 368) | |||
|---|---|---|---|---|---|---|---|
| Mean (SD)/% | Range | ||||||
| Age *** | 22.2 (3.2) | 22.3 (3.2) | 21.4 (3.0) | 22.2 (3.1) | 23.0 (3.3) | 18–30 | |
| Sex | |||||||
| Men | 40.5% | 39.7% | 42.5% | 43.2% | 36.1% | ||
| Women | 59.5% | 60.3% | 57.5% | 56.8% | 63.9% | ||
| Household income *** | |||||||
| USD 0–19 K | 22.8% | 31.2% | 18.7% | 20.7% | 22.7% | ||
| USD 20–39 K | 23.3% | 24.8% | 20.0% | 20.7% | 27.8% | ||
| USD 40–69 K | 23.6% | 23.1% | 24.1% | 23.8% | 23.3% | ||
| USD 70–99 K | 11.9% | 9.8% | 14.6% | 13.7% | 9.2% | ||
| USD 100–119 K | 10.5% | 6.4% | 13.7% | 12.0% | 8.8% | ||
| USD 120 K or Over | 7.9% | 4.7% | 8.9% | 9.0% | 8.2% | ||
| Hours/week worked for pay *** | |||||||
| 0 h | 24.1% | 26.9% | 24.2% | 24.2% | 21.9% | ||
| 1–9 h | 8.9% | 6.6% | 8.3% | 9.7% | 10.7% | ||
| 10–19 h | 20.6% | 17.9% | 23.3% | 24.7% | 15.3% | ||
| 20–29 h | 21.2% | 19.7% | 21.6% | 20.7% | 22.4% | ||
| 30–39 h | 10.7% | 13.8% | 10.0% | 7.6% | 12.3% | ||
| 40 h | 9.9% | 6.6% | 9.0% | 9.5% | 13.9% | ||
| Over 40 h | 4.6% | 8.6% | 3.6% | 3.7% | 3.6% | ||
| Current substance use | |||||||
| E-cigarette ** | 30.3% | 34.8% | 29.5% | 23.8% | 39.3% | ||
| Cigarette | 10.0% | 10.7% | 9.2% | 9.7% | 14.4% | ||
| Marijuana *** | 23.5% | 23.4% | 15.1% | 7.0% | 39.1% | ||
| Binge drinking *** | 28.6% | 31.4% | 24.6% | 23.3% | 36.4% | ||
| Problem use | |||||||
| Alcohol *** | 4.2 (4.8) | 4.8 (5.4) | 3.6 (4.3) | 3.5 (4.1) | 5.1 (5.3) | 0–25 | |
| Marijuana *** | 3.2 (4.9) | 4.0 (5.2) | 1.9 (3.7) | 2.2 (3.9) | 5.1 (5.9) | 0–24 | |
| Independent Variables | B (SE) |
|---|---|
| Age | 0.05 (0.05) |
| Sex (men: 0, women: 1) | −0.02 (0.02) |
| Hours/week worked for pay | −0.01 (0.04) |
| NHPI | 0.03 (0.02) |
| Filipino | −0.09 (0.06) |
| Asian | −0.04 (0.06) |
| T1 Sensation seeking | 0.04 (0.02) |
| T1 current cigarette smoking | 0.01 (0.02) |
| T1 problem alcohol use | 0.65 (0.02) *** |
| T1 current e-cigarette use | 0.06 (0.02) ** |
| Independent Variables | B (SE) |
|---|---|
| Age | 0.05 (0.02) * |
| Sex (men: 0, women: 1) | 0.12 (0.04) ** |
| Hours/week worked for pay | −0.001 (0.02) |
| NHPI | −0.12 (0.06) * |
| Filipino | −0.09 (0.05) |
| Asian | −0.03 (0.05) |
| T1 Sensation seeking | 0.06 (0.02) ** |
| T1 current cigarette smoking | −0.04 (0.02) |
| T1 current marijuana vaping | 0.01 (0.02) |
| T1 problem marijuana use | 0.66 (0.02) *** |
| T1 current e-cigarette use | 0.06 (0.02) ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pokhrel, P.; Elwir, T.; Mettias, H.; Kawamoto, C.T.; Oli, N.; Okamoto, S.K. The Effects of E-Cigarette Use on Alcohol and Marijuana Abuse Symptoms in an Ethnically Diverse Sample of Young Adults. Int. J. Environ. Res. Public Health 2021, 18, 13159. https://doi.org/10.3390/ijerph182413159
Pokhrel P, Elwir T, Mettias H, Kawamoto CT, Oli N, Okamoto SK. The Effects of E-Cigarette Use on Alcohol and Marijuana Abuse Symptoms in an Ethnically Diverse Sample of Young Adults. International Journal of Environmental Research and Public Health. 2021; 18(24):13159. https://doi.org/10.3390/ijerph182413159
Chicago/Turabian StylePokhrel, Pallav, Taha Elwir, Hannah Mettias, Crissy T. Kawamoto, Nabin Oli, and Scott K. Okamoto. 2021. "The Effects of E-Cigarette Use on Alcohol and Marijuana Abuse Symptoms in an Ethnically Diverse Sample of Young Adults" International Journal of Environmental Research and Public Health 18, no. 24: 13159. https://doi.org/10.3390/ijerph182413159
APA StylePokhrel, P., Elwir, T., Mettias, H., Kawamoto, C. T., Oli, N., & Okamoto, S. K. (2021). The Effects of E-Cigarette Use on Alcohol and Marijuana Abuse Symptoms in an Ethnically Diverse Sample of Young Adults. International Journal of Environmental Research and Public Health, 18(24), 13159. https://doi.org/10.3390/ijerph182413159







