Trends of Substance Use among Individuals with Cardiovascular Disease in the United States, 2015–2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Descriptive Statistics
3.2. Trends in Substance Use
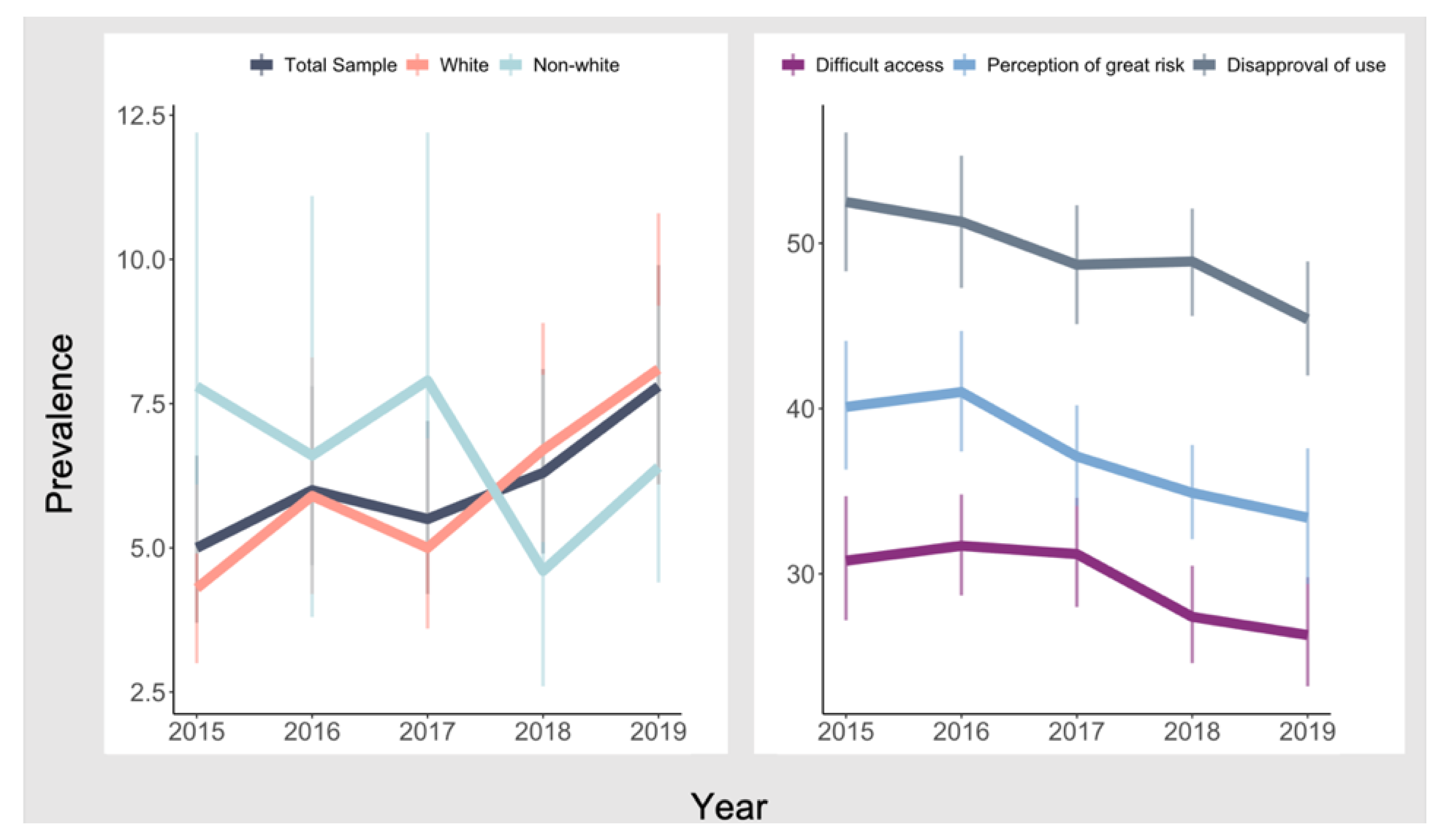
3.3. Trends in Cannabis-Specific Contexts
3.4. Associations between Cannabis-Specific Contexts and Cannabis Use Trends
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Individuals with a Heart Disease | All Individuals without a Heart Disease | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | Change Rate from 2015 to 2019 | 2015 | 2016 | 2017 | 2018 | 2019 | Change Rate from 2015 to 2019 | |
| Tobacco Use | ||||||||||||
| Total Sample | 20.1 | 19.8 | 18.4 | 19.8 | 18.1 | −10.0% | 26.1 | 25.8 | 24.4 | 23.4 | 23.2 | −11.1% |
| White | 19.5 | 19.0 | 18.0 | 19.4 | 17.1 | −12.3% | 28.1 | 28.3 | 26.6 | 25.8 | 25.5 | −9.3% |
| Non-White | 22.5 | 23.0 | 20.7 | 21.7 | 22.0 | −2.2% | 22.5 | 21.4 | 20.7 | 19.4 | 19.4 | −13.8% |
| Alcohol Use | ||||||||||||
| Total Sample | 46.1 | 45.9 | 46.2 | 46.2 | 46.2 | 0.2% | 56.5 | 55.9 | 56.7 | 55.8 | 55.5 | −1.8% |
| White | 48.1 | 46.9 | 47.8 | 48.1 | 48.4 | 0.6% | 61.7 | 61.5 | 61.8 | 61.2 | 60.8 | −1.5% |
| Non-White | 37.2 | 41.7 | 38.5 | 37.7 | 37.4 | 0.5% | 47.3 | 45.9 | 48.0 | 46.8 | 46.9 | −0.8% |
| Cannabis Use | ||||||||||||
| Total Sample | 5.0 | 6.0 | 5.5 | 6.3 | 7.8 | 56.0% | 8.7 | 9.2 | 10.0 | 10.7 | 12.1 | 39.1% |
| White | 4.3 | 5.9 | 5.0 | 6.7 | 8.2 | 90.7% | 8.8 | 9.3 | 10.4 | 10.8 | 12.7 | 44.3% |
| Non-White | 7.8 | 6.6 | 7.9 | 4.6 | 6.4 | −17.9% | 8.4 | 9.1 | 9.4 | 10.6 | 11.3 | 34.5% |
| Tobacco Use | Alcohol Use | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted Model | Adjusted Model | Unadjusted Model | Adjusted Model | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Survey Year | 0.97 | 0.92–1.03 | 0.99 | 0.93–1.06 | 1.00 | 0.96–1.05 | 1.00 | 0.96–1.04 |
| Gender | ||||||||
| Men | … | … | ||||||
| Women | 0.56 | 0.48–0.64 | 0.70 | 0.63–0.79 | ||||
| Age | ||||||||
| 18–25 | 1.74 | 1.31–2.31 | 0.75 | 0.53–1.05 | ||||
| 26–34 | 1.19 | 0.90–1.57 | 0.51 | 0.37–0.71 | ||||
| 35–64 | 0.31 | 0.22–0.45 | 0.43 | 0.30–0.61 | ||||
| 65+ | … | … | ||||||
| Race/ethnicity | ||||||||
| Black | 0.80 | 0.62–1.03 | 0.90 | 0.72–1.14 | ||||
| Hispanic | 0.53 | 0.36–0.78 | 0.71 | 0.51–0.99 | ||||
| Other | 1.04 | 0.76–1.40 | 0.65 | 0.49–0.85 | ||||
| White | … | … | ||||||
| Education | ||||||||
| Less than high school | 3.11 | 2.31–4.20 | 0.35 | 0.28–0.45 | ||||
| High school graduate | 2.18 | 1.71–2.78 | 0.50 | 0.41–0.62 | ||||
| Some college | 1.85 | 1.43–2.40 | 0.79 | 0.66–0.94 | ||||
| College graduate | … | … | ||||||
| Employment | ||||||||
| Employed | … | … | ||||||
| Unemployed | 1.79 | 0.89–3.58 | 0.95 | 0.59–1.53 | ||||
| Not in labor force | 0.93 | 0.71–1.21 | 0.67 | 0.58–0.77 | ||||
| Household income | ||||||||
| <$20,000 | 2.36 | 1.72–3.25 | 0.41 | 0.32–0.52 | ||||
| $20,000–39,999 | 1.93 | 1.47–2.54 | 0.44 | 0.38–0.51 | ||||
| $40,000–74,999 | 1.61 | 1.25–2.09 | 0.63 | 0.53–0.75 | ||||
| $75,000+ | … | … | ||||||
| Marital status | ||||||||
| Married | … | … | ||||||
| Widowed/divorced/separated | 1.53 | 1.27–1.85 | 0.96 | 0.84–1.10 | ||||
| Never married | 1.22 | 0.95–1.58 | 0.81 | 0.62–1.05 | ||||
| Health insurance coverage | ||||||||
| Yes | … | … | ||||||
| No | 1.23 | 0.90–1.70 | 1.37 | 0.96–1.94 | ||||
| Severe psychological distress | ||||||||
| Yes | 1.47 | 1.20–1.79 | 0.99 | 0.83–1.19 | ||||
| No | … | … | ||||||
| Urbanicity of residence | ||||||||
| Rural | 1.18 | 0.91–1.54 | 0.91 | 0.74–1.12 | ||||
| Urban | … | … | ||||||
| Model 1(Unadjusted) | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Survey Year | 1.11 | 1.01–1.26 | 1.13 | 1.02–1.25 | 1.10 | 1.00–1.22 | 1.10 | 0.99–1.21 | 1.09 | 0.99–1.20 | 1.06 | 0.96–1.16 |
| Gender | ||||||||||||
| Men | … | … | … | … | … | |||||||
| Women | 0.57 | 0.45–0.73 | 0.61 | 0.47–0.78 | 0.64 | 0.50–0.83 | 0.61 | 0.47–0.78 | 0.69 | 0.52–0.92 | ||
| Age | ||||||||||||
| 18–25 | 1.16 | 0.80–1.68 | 1.19 | 0.83–1.70 | 1.13 | 0.78–1.63 | 1.00 | 0.68–1.47 | 1.02 | 0.70–1.49 | ||
| 26–34 | 0.55 | 0.37–0.81 | 0.61 | 0.41–0.90 | 0.62 | 0.42–0.91 | 0.57 | 0.38–0.85 | 0.67 | 0.45–0.99 | ||
| 35–64 | 0.18 | 0.10–0.31 | 0.26 | 0.15–0.43 | 0.26 | 0.15–0.43 | 0.27 | 0.16–0.47 | 0.43 | 0.26–0.73 | ||
| 65+ | … | … | … | … | … | |||||||
| Race/ethnicity | ||||||||||||
| Black | 0.83 | 0.53–1.28 | 0.83 | 0.53–1.29 | 0.94 | 0.61–1.46 | 0.88 | 0.55–1.42 | 0.95 | 0.59–1.52 | ||
| Hispanic | 0.60 | 0.38–0.95 | 0.70 | 0.44–1.12 | 0.75 | 0.47–1.21 | 0.68 | 0.41–1.13 | 0.92 | 0.56–1.51 | ||
| Other | 0.81 | 0.56–1.16 | 0.94 | 0.63–1.39 | 0.86 | 0.59–1.25 | 0.92 | 0.60–1.41 | 1.12 | 0.70–1.78 | ||
| White | … | … | … | … | … | |||||||
| Education | ||||||||||||
| Less than high school | 0.66 | 0.39–1.12 | 0.76 | 0.44–1.29 | 0.80 | 0.46–1.40 | 0.74 | 0.42–1.31 | 0.95 | 0.53–1.69 | ||
| High school graduate | 0.81 | 0.55–1.19 | 0.87 | 0.59–1.26 | 0.90 | 0.60–1.34 | 0.83 | 0.56–1.24 | 0.95 | 0.65–1.38 | ||
| Some college | 0.99 | 0.67–1.48 | 0.99 | 0.67–1.46 | 1.05 | 0.70–1.57 | 1.02 | 0.67–1.55 | 1.06 | 0.70–1.61 | ||
| College graduate | … | … | … | … | … | |||||||
| Employment | ||||||||||||
| Employed | … | … | … | … | … | |||||||
| Unemployed | 2.17 | 1.07–4.41 | 2.41 | 1.23–4.73 | 1.94 | 1.00–3.77 | 2.22 | 1.05–4.72 | 2.21 | 1.15–4.26 | ||
| Not in labor force | 1.01 | 0.74–1.37 | 1.06 | 0.79–1.41 | 1.03 | 0.75–1.42 | 1.02 | 0.74–1.41 | 1.10 | 0.80–1.52 | ||
| Household income | ||||||||||||
| <$20,000 | 1.49 | 0.86–2.58 | 1.59 | 0.90–2.83 | 1.60 | 0.91–2.80 | 1.65 | 0.94–2.87 | 1.70 | 0.93–3.10 | ||
| $20,000–39,99 | 1.22 | 0.86–1.74 | 1.29 | 0.91–1.84 | 1.33 | 0.94–1.90 | 1.39 | 0.95–2.03 | 1.48 | 1.01–2.16 | ||
| $40,000–74,999 | 1.04 | 0.71–1.52 | 1.07 | 0.74–1.55 | 1.05 | 0.72–1.53 | 1.13 | 0.77–1.65 | 1.13 | 0.78–1.64 | ||
| $75,000+ | … | … | … | … | … | |||||||
| Marital status | ||||||||||||
| Married | … | … | … | … | … | |||||||
| Widowed/divorced/separated | 1.58 | 1.12–2.25 | 1.57 | 1.10–2.25 | 1.54 | 1.08–2.20 | 1.42 | 0.99–2.04 | 1.47 | 1.01–2.14 | ||
| Never married | 1.69 | 1.14–2.52 | 1.61 | 1.07–2.41 | 1.62 | 1.07–2.45 | 1.56 | 1.02–2.39 | 1.49 | 0.96–2.32 | ||
| Health insurance coverage | ||||||||||||
| Yes | … | … | … | … | … | |||||||
| No | 1.56 | 0.93–2.60 | 1.58 | 0.93–2.66 | 1.50 | 0.91–2.46 | 1.58 | 0.95–2.63 | 1.68 | 1.00–2.83 | ||
| Severe psychological distress | ||||||||||||
| Yes | 1.79 | 1.37–2.33 | 1.69 | 1.29–2.20 | 1.61 | 1.21–2.14 | 1.56 | 1.19–2.03 | 1.47 | 1.11–1.94 | ||
| No | … | … | … | … | … | |||||||
| Urbanicity of residence | ||||||||||||
| Rural | 0.60 | 0.38–0.94 | 0.54 | 0.35–0.86 | 0.61 | 0.39–0.94 | 0.62 | 0.39–0.99 | 0.58 | 0.37–0.91 | ||
| Urban | … | … | … | … | … | |||||||
| Difficult access to cannabis | ||||||||||||
| Yes | 0.06 | 0.02–0.14 | 0.14 | 0.06–0.35 | ||||||||
| No | … | … | ||||||||||
| Perception of risk of cannabis | ||||||||||||
| Yes | 0.06 | 0.02–1.14 | 0.12 | 0.06–0.21 | ||||||||
| No | … | … | ||||||||||
| Disapproval of cannabis use | ||||||||||||
| Yes | 0.07 | 0.04–0.12 | 0.08 | 0.03–0.21 | ||||||||
| No | … | … | ||||||||||
| Model 1 (Unadjusted) | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Survey Year | 1.16 | 1.04–1.30 | 1.17 | 1.05–1.32 | 1.15 | 1.03–1.29 | 1.14 | 1.02–1.28 | 1.14 | 1.02–1.28 | 1.1 | 0.98–1.23 |
| Gender | ||||||||||||
| Men | … | … | … | … | … | |||||||
| Women | 0.57 | 0.45–0.74 | 0.62 | 0.48–0.81 | 0.65 | 0.50–0.84 | 0.60 | 0.46–0.78 | 0.69 | 0.51–0.93 | ||
| Age | ||||||||||||
| 18–25 | 1.22 | 0.77–1.91 | 1.27 | 0.81–2.00 | 1.22 | 0.77–1.94 | 1.07 | 0.66–1.72 | 1.14 | 0.70–1.84 | ||
| 26–34 | 0.57 | 0.36–0.88 | 0.63 | 0.41–0.98 | 0.65 | 0.41–1.01 | 0.58 | 0.36–0.94 | 0.68 | 0.43–1.08 | ||
| 35–64 | 0.19 | 0.10–0.34 | 0.27 | 0.15–0.47 | 0.27 | 0.15–0.49 | 0.29 | 0.15–0.54 | 0.44 | 0.24–0.80 | ||
| 65+ | … | … | … | … | … | |||||||
| Education | ||||||||||||
| Less than high school | 0.68 | 0.37–1.24 | 0.79 | 0.44–1.42 | 0.83 | 0.44–1.54 | 0.79 | 0.42–1.48 | 1.01 | 0.54–1.89 | ||
| High school graduate | 0.78 | 0.49–1.22 | 0.84 | 0.54–1.30 | 0.86 | 0.54–1.37 | 0.79 | 0.49–1.26 | 0.93 | 0.59–1.44 | ||
| Some college | 0.96 | 0.62–1.50 | 0.97 | 0.62–1.51 | 1.01 | 0.65–1.58 | 0.98 | 0.61–1.56 | 1.05 | 0.66–1.68 | ||
| College graduate | … | … | … | … | … | |||||||
| Employment | ||||||||||||
| Employed | … | … | … | … | … | |||||||
| Unemployed | 2.03 | 0.80–5.19 | 2.15 | 0.91–5.09 | 1.78 | 0.72–4.41 | 2.04 | 0.72–5.75 | 1.92 | 0.75–4.97 | ||
| Not in labor force | 1.03 | 0.72–1.47 | 1.10 | 0.79–1.55 | 1.05 | 0.74–1.50 | 1.06 | 0.72–1.55 | 1.18 | 0.81–1.71 | ||
| Household income | ||||||||||||
| <$20,000 | 1.33 | 0.70–2.52 | 1.43 | 0.74–2.75 | 1.46 | 0.76–2.80 | 1.53 | 0.79–2.95 | 1.54 | 0.78–3.06 | ||
| $20,000–39,99 | 1.28 | 0.84–1.95 | 1.35 | 0.88–2.07 | 1.41 | 0.92–2.16 | 1.45 | 0.92–2.28 | 1.55 | 0.99–2.43 | ||
| $40,000–74,999 | 1.04 | 0.69–1.58 | 1.06 | 0.71–1.60 | 1.07 | 0.71–1.60 | 1.14 | 0.74–1.73 | 1.13 | 0.75–1.71 | ||
| $75,000+ | … | … | … | … | … | |||||||
| Marital status | ||||||||||||
| Married | … | … | … | … | … | |||||||
| Widowed/divorced/ separated | 1.60 | 1.15–2.23 | 1.59 | 1.14–2.22 | 1.56 | 1.11–2.19 | 1.43 | 1.02–1.99 | 1.43 | 1.01–2.03 | ||
| Never married | 1.57 | 1.03–2.41 | 1.53 | 1.00–2.34 | 1.55 | 1.00–2.39 | 1.48 | 0.93–2.34 | 1.46 | 0.91–2.33 | ||
| Health insurance coverage | ||||||||||||
| Yes | … | … | … | … | … | |||||||
| No | 1.89 | 0.98–3.62 | 1.92 | 0.98–3.76 | 1.79 | 0.94–3.40 | 2.00 | 1.06–3.79 | 2.18 | 1.11–4.28 | ||
| Severe psychological distress | ||||||||||||
| Yes | 1.80 | 1.28–2.54 | 1.71 | 1.21–2.41 | 1.63 | 1.12–2.39 | 1.57 | 1.09–2.26 | 1.49 | 1.02–2.17 | ||
| No | … | … | … | … | … | |||||||
| Urbanicity of residence | ||||||||||||
| Rural | 0.64 | 0.40–1.03 | 0.59 | 0.36–0.96 | 0.66 | 0.41–1.05 | 0.68 | 0.42–1.11 | 0.64 | 0.39–1.04 | ||
| Urban | … | … | … | … | … | |||||||
| Difficult access to cannabis | ||||||||||||
| Yes | 0.07 | 0.02–0.19 | 0.19 | 0.07–0.51 | ||||||||
| No | … | … | ||||||||||
| Perception of risk of cannabis | ||||||||||||
| Yes | 0.07 | 0.02–0.19 | 0.10 | 0.05–0.21 | ||||||||
| No | … | … | ||||||||||
| Disapproval of cannabis use | ||||||||||||
| Yes | 0.06 | 0.03–0.13 | 0.10 | 0.04–0.29 | ||||||||
| No | … | … | ||||||||||
References
- Breslow, R.A.; Castle, I.J.P.; Chen, C.M.; Graubard, B.I. Trends in alcohol consumption among older Americans: National Health Interview Surveys, 1997 to 2014. Alcohol. Clin. Exp. Res. 2017, 41, 976–986. [Google Scholar] [CrossRef] [PubMed]
- Dawson, D.A.; Goldstein, R.B.; Saha, T.D.; Grant, B.F. Changes in alcohol consumption: United States, 2001–2002 to 2012–2013. Drug Alcohol Depend. 2015, 148, 56–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanton, C.A.; Keith, D.R.; Gaalema, D.E.; Bunn, J.Y.; Doogan, N.J.; Redner, R.; Kurti, A.N.; Roberts, M.E.; Higgins, S.T. Trends in tobacco use among US adults with chronic health conditions: National Survey on Drug Use and Health 2005–2013. Prev. Med. 2016, 92, 160–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salas-Wright, C.P.; Vaughn, M.G.; Cummings-Vaughn, L.A.; Holzer, K.J.; Nelson, E.J.; AbiNader, M.; Oh, S. Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002–2014. Drug Alcohol Depend. 2017, 171, 97–106. [Google Scholar] [CrossRef] [Green Version]
- McCarthy, J. One in eight US adults say they smoke marijuana. Gallup Website, 8 August 2016. [Google Scholar]
- Grucza, R.A.; Agrawal, A.; Krauss, M.J.; Cavazos-Rehg, P.A.; Bierut, L.J. Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA Psychiatry 2016, 73, 300–301. [Google Scholar] [CrossRef] [PubMed]
- Tramèr, M.R.; Carroll, D.; Campbell, F.A.; Reynolds, D.J.M.; Moore, R.A.; McQuay, H.J. Cannabinoids for control of chemotherapy induced nausea and vomiting: Quantitative systematic review. BMJ 2001, 323, 16. [Google Scholar] [CrossRef] [Green Version]
- Musty, R.E.; Rossi, R. Effects of smoked cannabis and oral Δ9-tetrahydrocannabinol on nausea and emesis after cancer chemotherapy: A review of state clinical trials. J. Cannabis Ther. 2001, 1, 29–56. [Google Scholar] [CrossRef]
- Nova, E.; Baccan, G.; Veses, A.; Zapatera, B.; Marcos, A. Potential health benefits of moderate alcohol consumption: Current perspectives in research. Proc. Nutr. Soc. 2012, 71, 307–315. [Google Scholar] [CrossRef] [Green Version]
- Frati, G.; Forte, M.; di Nonno, F.; Bordin, A.; Chimenti, I.; Picchio, V.; Cavarretta, E.; Stanzione, R.; Bianchi, F.; Carnevale, R. inhibition of miR-155 attenuates detrimental vascular effects of tobacco cigarette smoking. J. Am. Heart Assoc. 2020, 9, e017000. [Google Scholar] [CrossRef]
- Scolaro, J.A.; Schenker, M.L.; Yannascoli, S.; Baldwin, K.; Mehta, S.; Ahn, J. Cigarette smoking increases complications following fracture: A systematic review. JBJS J. Bone Jt. Surg. 2014, 96, 674–681. [Google Scholar] [CrossRef]
- Turati, F.; Galeone, C.; Rota, M.; Pelucchi, C.; Negri, E.; Bagnardi, V.; Corrao, G.; Boffetta, P.; La Vecchia, C. Alcohol and liver cancer: A systematic review and meta-analysis of prospective studies. Ann. Oncol. 2014, 25, 1526–1535. [Google Scholar] [CrossRef]
- Rehm, J.; Taylor, B.; Mohapatra, S.; Irving, H.; Baliunas, D.; Patra, J.; Roerecke, M. Alcohol as a risk factor for liver cirrhosis: A systematic review and meta-analysis. Drug Alcohol Rev. 2010, 29, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Calabria, B.; Degenhardt, L.; Hall, W.; Lynskey, M. Does cannabis use increase the risk of death? Systematic review of epidemiological evidence on adverse effects of cannabis use. Drug Alcohol Rev. 2010, 29, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Campeny, E.; López-Pelayo, H.; Nutt, D.; Blithikioti, C.; Oliveras, C.; Nuño, L.; Maldonado, R.; Florez, G.; Arias, F.; Fernández-Artamendi, S. The blind men and the elephant: Systematic review of systematic reviews of cannabis use related health harms. Eur. Neuropsychopharmacol. 2020, 33, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Gurm, H.; Bartholomew, J.R. Smokeless tobacco and cardiovascular risk. Arch. Intern. Med. 2004, 164, 1845–1849. [Google Scholar] [CrossRef] [Green Version]
- Bullen, C. Impact of tobacco smoking and smoking cessation on cardiovascular risk and disease. Expert Rev. Cardiovasc. Ther. 2008, 6, 883–895. [Google Scholar] [CrossRef] [PubMed]
- Foerster, M.; Marques-Vidal, P.; Gmel, G.; Daeppen, J.-B.; Cornuz, J.; Hayoz, D.; Pécoud, A.; Mooser, V.; Waeber, G.; Vollenweider, P. Alcohol drinking and cardiovascular risk in a population with high mean alcohol consumption. Am. J. Cardiol. 2009, 103, 361–368. [Google Scholar] [CrossRef] [Green Version]
- Mostofsky, E.; Chahal, H.S.; Mukamal, K.J.; Rimm, E.B.; Mittleman, M.A. Alcohol and immediate risk of cardiovascular events: A systematic review and dose–response meta-analysis. Circulation 2016, 133, 979–987. [Google Scholar] [CrossRef] [Green Version]
- Jouanjus, E.; Raymond, V.; Lapeyre-Mestre, M.; Wolff, V. What is the current knowledge about the cardiovascular risk for users of cannabis-based products? A systematic review. Curr. Atheroscler. Rep. 2017, 19, 26. [Google Scholar] [CrossRef]
- DeFilippis, E.M.; Bajaj, N.S.; Singh, A.; Malloy, R.; Givertz, M.M.; Blankstein, R.; Bhatt, D.L.; Vaduganathan, M. Marijuana use in patients with cardiovascular disease: JACC review topic of the week. J. Am. Coll. Cardiol. 2020, 75, 320–332. [Google Scholar] [CrossRef]
- Page, R.L.; Allen, L.A.; Kloner, R.A.; Carriker, C.R.; Martel, C.; Morris, A.A.; Piano, M.R.; Rana, J.S.; Saucedo, J.F. Medical marijuana, recreational cannabis, and cardiovascular health: A scientific statement from the American Heart Association. Circulation 2020, 142, e131–e152. [Google Scholar] [CrossRef]
- Havakuk, O.; Rezkalla, S.H.; Kloner, R.A. The cardiovascular effects of cocaine. J. Am. Coll. Cardiol. 2017, 70, 101–113. [Google Scholar] [CrossRef]
- Mladěnka, P.; Applová, L.; Patočka, J.; Costa, V.M.; Remiao, F.; Pourová, J.; Mladěnka, A.; Karlíčková, J.; Jahodář, L.; Vopršalová, M. Comprehensive review of cardiovascular toxicity of drugs and related agents. Med. Res. Rev. 2018, 38, 1332–1403. [Google Scholar] [CrossRef] [PubMed]
- Mirijello, A.; Tarli, C.; Vassallo, G.A.; Sestito, L.; Antonelli, M.; d’Angelo, C.; Ferrulli, A.; De Cosmo, S.; Gasbarrini, A.; Addolorato, G. Alcoholic cardiomyopathy: What is known and what is not known. Eur. J. Intern. Med. 2017, 43, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Auger, N.; Paradis, G.; Low, N.; Ayoub, A.; He, S.; Potter, B.J. Cannabis use disorder and the future risk of cardiovascular disease in parous women: A longitudinal cohort study. BMC Med. 2020, 18, 328. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Bhatia, H.; Ma, J.; Dickson, S.D.; Alshawabkeh, L.; Adler, E.; Maisel, A.; Criqui, M.H.; Greenberg, B.; Thomas, I.C. The impact of substance abuse on heart failure hospitalizations. Am. J. Med. 2020, 133, 207–213.e1. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Salas-Wright, C.P.; Vaughn, M.G.; DiNitto, D.M. Marijuana use during pregnancy: A comparison of trends and correlates among married and unmarried pregnant women. Drug Alcohol Depend. 2017, 181, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Salas-Wright, C.P.; Vaughn, M.G.; Reingle Gonzalez, J.M.; Fu, Q.; Clark Goings, T. Attacks intended to seriously harm and co-occurring drug use among youth in the United States. Subst. Use Misuse 2016, 51, 1681–1692. [Google Scholar] [CrossRef]
- Schuermeyer, J.; Salomonsen-Sautel, S.; Price, R.K.; Balan, S.; Thurstone, C.; Min, S.-J.; Sakai, J.T. Temporal trends in marijuana attitudes, availability and use in Colorado compared to non-medical marijuana states: 2003–11. Drug Alcohol Depend. 2014, 140, 145–155. [Google Scholar] [CrossRef] [Green Version]
- Moore, A.A.; Karno, M.P.; Grella, C.E.; Lin, J.C.; Warda, U.; Liao, D.H.; Hu, P. Alcohol, tobacco, and nonmedical drug use in older US adults: Data from the 2001/02 National Epidemiologic Survey of Alcohol and Related Conditions. J. Am. Geriatr. Soc. 2009, 57, 2275–2281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonomo, Y.; Proimos, J. Substance misuse: Alcohol, tobacco, inhalants, and other drugs. BMJ 2005, 330, 777–780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keyes, K.M.; Vo, T.; Wall, M.M.; Caetano, R.; Suglia, S.F.; Martins, S.S.; Galea, S.; Hasin, D. Racial/ethnic differences in use of alcohol, tobacco, and marijuana: Is there a cross-over from adolescence to adulthood? Soc. Sci. Med. 2015, 124, 132–141. [Google Scholar] [CrossRef] [Green Version]
- Han, B.H.; Palamar, J.J. Trends in cannabis use among older adults in the United States, 2015–2018. JAMA Intern. Med. 2020, 180, 609–611. [Google Scholar] [CrossRef] [PubMed]
- Center for Behavioral Health Statistics and Quality. 2019 National Survey on Drug Use and Health Public Use File Codebook; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2020. [Google Scholar]
- Kim, J.H.; Martins, S.S.; Shmulewitz, D.; Santaella, J.; Wall, M.M.; Keyes, K.M.; Eaton, N.R.; Krueger, R.; Grant, B.F.; Hasin, D.S. Childhood maltreatment, stressful life events, and alcohol craving in adult drinkers. Alcohol. Clin. Exp. Res. 2014, 38, 2048–2055. [Google Scholar] [CrossRef]
- Myers, B.; McLaughlin, K.A.; Wang, S.; Blanco, C.; Stein, D.J. Associations between childhood adversity, adult stressful life events, and past-year drug use disorders in the National Epidemiological Study of Alcohol and Related Conditions (NESARC). Psychol. Addict. Behav. 2014, 28, 1117–1126. [Google Scholar] [CrossRef] [Green Version]
- Storr, C.L.; Reboussin, B.A.; Green, K.M.; Mojtabai, R.; Susukida, R.; Young, A.S.; Cullen, B.A.; Alvanzo, A.A.; Crum, R.M. Stressful life events and transitions in problematic alcohol use involvement among US adults. Subst. Use Misuse 2021, 56, 2171–2180. [Google Scholar] [CrossRef]
- Tamers, S.L.; Okechukwu, C.; Marino, M.; Gueguen, A.; Goldberg, M.; Zins, M. Effect of stressful life events on changes in smoking among the French: Longitudinal findings from GAZEL. Eur. J. Public Health 2015, 25, 711–715. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control Prevention. Conducting Trend Analyses of YRBS Data; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2016. [Google Scholar]
- Substance Abuse & Mentla Health Data Archive National Survey of Drug Use and Health (NSDUH-2019). Available online: https://www.datafiles.samhsa.gov/study/national-survey-drug-use-and-health-nsduh-2019-nid19014 (accessed on 14 April 2021).
| Characteristics | Unweighted Frequency (%) | Weighted % (95% Confidence Interval) | ||
|---|---|---|---|---|
| Tobacco | Alcohol | Cannabis | ||
| Total Sample | 7339 (100.0) | 19.2 (18.0–20.5) | 46.1 (44.5–47.7) | 6.2 (5.5–6.9) |
| Gender | ||||
| Men | 3403 (46.4) | 21.2 (19.7–22.7) | 51.8 (49.7–53.9) | 7.0 (6.1–8.0) |
| Women | 3936 (53.6) | 17.1 (15.6–18.8) | 40.1 (38.0–42.2) | 5.3 (4.4–6.4) |
| Age | ||||
| 18–25 | 843 (11.5) | 30.9 (27.0–35.1) | 58.4 (53.3–63.3) | 20.4 (16.6–24.9) |
| 26–34 | 579 (7.9) | 36.8 (31.9–42.1) | 57.1 (52.8–61.4) | 19.9 (15.9–24.5) |
| 35–64 | 3114 (42.4) | 29.0 (26.8–31.3) | 49.9 (47.4–52.5) | 8.6 (7.5–9.8) |
| 65+ | 2803 (38.2) | 10.2 (8.8–11.9) | 41.9 (39.6–44.2) | 2.8 (2.0–3.8) |
| Race/ethnicity | ||||
| Black | 663 (9.0) | 23.9 (20.3–28.0) | 39.6 (34.9–44.6) | 7.3 (5.2–10.3) |
| Hispanic | 516 (7.0) | 18.8 (14.3–24.4) | 36.6 (29.9–43.8) | 5.9 (4.0–8.6) |
| Other | 492 (6.7) | 22.9 (18.3–28.2) | 39.2 (33.0–45.7) | 6.3 (4.5–8.8) |
| White | 5668 (77.2) | 18.9 (17.2–20.0) | 47.9 (46.2–49.6) | 6.1 (5.3–7.0) |
| Education | ||||
| Less than high school | 948 (12.9) | 30.2 (26.3–34.3) | 24.3 (21.1–27.7) | 5.1 (3.8–6.9) |
| High school graduate | 1989 (27.1) | 23.2 (20.9–25.7) | 35.5 (32.5–38.6) | 6.0 (4.8–7.4) |
| Some college | 2446 (33.3) | 20.4 (18.4–22.6) | 49.6 (46.8–52.4) | 7.3 (5.9–8.9) |
| College graduate | 1956 (26.7) | 9.6 (8.1–11.4) | 61.3 (58.1–64.4) | 5.7 (4.4–7.3) |
| Employment | ||||
| Employed | 3918 (43.6) | 20.8 (18.5–23.2) | 59.3 (57.1–61.5) | 7.6 (6.4–9.1) |
| Unemployed | 215 (2.9) | 43.1 (32.4–54.5) | 49.0 (39.2–58.8) | 21.4 (12.8–33.7) |
| Not in labor force | 3926 (53.5) | 17.6 (16.0–19.3) | 38.5 (36.6–40.5) | 4.9 (4.2–5.8) |
| Household income | ||||
| <$20,000 | 1544 (21.0) | 30.9 (27.7–24.3) | 28.1 (25.1–31.4) | 8.8 (6.7–11.4) |
| $20,000–39,999 | 1722 (23.5) | 22.9 (20.6–25.3) | 33.5 (30.3–36.7) | 6.3 (5.0–7.9) |
| $40,000–74,999 | 1927 (26.3) | 17.7 (15.4–20.2) | 47.0 (44.1–49.9) | 5.3 (4.3–6.7) |
| $75,000+ | 2146 (29.2) | 11.6 (9.9–13.5) | 63.8 (61.2–66.3) | 5.4 (4.2–6.9) |
| Marital status | ||||
| Married | 3655 (49.8) | 14.9 (13.4–16.5) | 51.5 (49.4–53.6) | 4.4 (3.6–5.5) |
| Widowed/divorced/separated | 2145 (29.2) | 22.9 (21.1–24.9) | 37.1 (34.6–39.8) | 6.3 (5.2–7.6) |
| Never married | 1539 (21.0) | 30.0 (26.5–33.8) | 45.0 (41.0–49.1) | 14.5 (12.1–17.3) |
| Health insurance coverage | ||||
| Yes | 6991 (95.3) | 18.5 (17.3–19.7) | 46.1 (44.4–47.7) | 5.8 (5.1–6.6) |
| No | 348 (10.7) | 41.5 (33.4–50.2) | 47.4 (38.9–56.0) | 16.6 (10.9–24.5) |
| Urbanicity of residence | ||||
| Rural | 782 (10.7) | 24.8 (20.7–29.3) | 38.0 (33.7–42.6) | 4.0 (2.7–5.8) |
| Urban | 6557 (89.3) | 18.7 (17.5–20.1) | 46.8 (45.0–48.5) | 6.4 (5.6–7.2) |
| Survey Year | ||||
| 2015 | 1420 (19.4) | 20.1 (17.2–23.3) | 46.1 (42.7–49.5) | 5.0 (3.7–6.6) |
| 2016 | 1397 (19.0) | 19.8 (17.0–22.9) | 45.9 (42.3–49.5) | 6.0 (4.7–7.8) |
| 2017 | 1462 (19.9) | 18.4 (16.0–21.1) | 46.2 (42.3–50.1) | 5.5 (4.2–7.2) |
| 2018 | 1564 (21.3) | 19.8 (17.1–22.8) | 46.2 (42.1–50.3) | 6.3 (4.9–8.1) |
| 2019 | 1496 (20.4) | 18.1 (16.0–20.3) | 46.2 (43.0–49.4) | 7.8 (6.1–9.9) |
| All Individuals with a Heart Disease | Racial/Ethnic Subgroups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Black | Hispanic | Other | White | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Tobacco Use | ||||||||||
| Unadjusted (Bivariate) | 0.97 | 0.92–1.03 | 1.05 | 0.90–1.22 | 1.01 | 0.83–1.24 | 0.87 | 0.68–1.10 | 0.97 | 0.91–1.04 |
| Adjusted for Covariates | 0.99 | 0.93–1.06 | 1.12 | 0.94–1.32 | 1.04 | 0.86–1.26 | 0.91 | 0.70–1.18 | 0.97 | 0.90–1.05 |
| Alcohol Use | ||||||||||
| Unadjusted (Bivariate) | 1.00 | 0.96–1.05 | 1.01 | 0.89–1.16 | 0.89 | 0.74–1.07 | 1.08 | 0.84–1.39 | 1.01 | 0.95–1.06 |
| Adjusted for Covariates | 1.00 | 0.96–1.04 | 1.01 | 0.89–1.15 | 0.87 | 0.73–1.05 | 1.18 | 0.91–1.54 | 1.00 | 0.95–1.05 |
| Cannabis Use | ||||||||||
| Unadjusted (Bivariate) | 1.11 | 1.01–1.23 | 0.99 | 0.77–1.26 | 0.83 | 0.61–1.13 | 0.96 | 0.76–1.22 | 1.16 | 1.04–1.30 |
| Adjusted for Covariates | 1.13 | 1.02–1.25 | 1.01 | 0.75–1.37 | 0.84 | 0.63–1.11 | 1.08 | 0.81–1.43 | 1.17 | 1.05–1.31 |
| All Individuals with a Heart Disease | Racial/Ethnic Subgroups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Black | Hispanic | Other | White | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Cannabis-Specific Factors | ||||||||||
| Difficult Access 1 | ||||||||||
| Unadjusted (Bivariate) | 0.94 | 0.89–0.99 | 0.95 | 0.80–1.13 | 1.14 | 0.92–1.41 | 0.85 | 0.66–1.08 | 0.92 | 0.87–0.98 |
| Adjusted for Sociodemographic Factors | 0.93 | 0.87–0.98 | 0.96 | 0.80–1.14 | 1.14 | 0.90–1.44 | 0.70 | 0.54–0.91 | 0.92 | 0.86–0.98 |
| Perception of Great Risk 2 | ||||||||||
| Unadjusted (Bivariate) | 0.92 | 0.87–0.97 | 0.97 | 0.83–1.13 | 0.91 | 0.77–1.08 | 0.88 | 0.69–1.12 | 0.92 | 0.87–0.97 |
| Adjusted for Sociodemographic Factors | 0.91 | 0.86–0.96 | 0.96 | 0.80–1.15 | 0.86 | 0.72–1.02 | 0.80 | 0.63–1.03 | 0.91 | 0.86–0.96 |
| Disapproval 3 | ||||||||||
| Unadjusted (Bivariate) | 0.94 | 0.89–0.99 | 0.94 | 0.80–1.10 | 1.00 | 0.81–1.25 | 0.96 | 0.81–1.14 | 0.93 | 0.88–0.98 |
| Adjusted for Sociodemographic Factors | 0.93 | 0.88–0.98 | 0.93 | 0.79–1.10 | 1.00 | 0.82–1.21 | 0.85 | 0.68–1.06 | 0.93 | 0.88–0.98 |
| All Individuals with a Heart Disease | Racial/Ethnic Subgroups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Black | Hispanic | Other | White | |||||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Cannabis Use | ||||||||||
| Adjusted for Covariates | 1.13 | 1.02–1.25 | 1.01 | 0.74–1.38 | 0.84 | 0.63–1.11 | 1.08 | 0.81–1.44 | 1.17 | 1.05–1.32 |
| Additional Adjustments for Risk Factors | ||||||||||
| Difficult Access 1 | 1.10 | 1.00–1.22 | 1.00 | 0.73–1.38 | 0.89 | 0.68–1.17 | 0.99 | 0.72–1.35 | 1.15 | 1.03–1.29 |
| Perception of Great Risk 2 | 1.10 | 0.99–1.21 | 1.03 | 0.74–1.42 | 0.78 | 0.59–1.04 | 1.07 | 0.80–1.44 | 1.14 | 1.02–1.28 |
| Disapproval of Use 3 | 1.09 | 0.99–1.20 | 0.93 | 0.68–1.27 | 0.85 | 0.60–1.20 | 1.01 | 0.73–1.39 | 1.14 | 1.02–1.28 |
| Full Modell 4 | 1.06 | 0.96–1.16 | 0.97 | 0.70–1.34 | 0.78 | 0.55–1.12 | 0.99 | 0.70–1.39 | 1.10 | 0.98–1.23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Oh, S.; Fadel, P.J.; Salas-Wright, C.P.; Vaughn, M.G. Trends of Substance Use among Individuals with Cardiovascular Disease in the United States, 2015–2019. Int. J. Environ. Res. Public Health 2022, 19, 577. https://doi.org/10.3390/ijerph19010577
Kim Y, Oh S, Fadel PJ, Salas-Wright CP, Vaughn MG. Trends of Substance Use among Individuals with Cardiovascular Disease in the United States, 2015–2019. International Journal of Environmental Research and Public Health. 2022; 19(1):577. https://doi.org/10.3390/ijerph19010577
Chicago/Turabian StyleKim, Yeonwoo, Sehun Oh, Paul J. Fadel, Christopher P. Salas-Wright, and Michael G. Vaughn. 2022. "Trends of Substance Use among Individuals with Cardiovascular Disease in the United States, 2015–2019" International Journal of Environmental Research and Public Health 19, no. 1: 577. https://doi.org/10.3390/ijerph19010577
APA StyleKim, Y., Oh, S., Fadel, P. J., Salas-Wright, C. P., & Vaughn, M. G. (2022). Trends of Substance Use among Individuals with Cardiovascular Disease in the United States, 2015–2019. International Journal of Environmental Research and Public Health, 19(1), 577. https://doi.org/10.3390/ijerph19010577







